Abstract
Acute liver failure (ALF) in children is a rare condition that is often fatal without liver transplantation. The diagnostic work-up is complex, and the etiology is unidentified in up to half of patients, making decisions like therapeutic transplantation extremely difficult. We collected clinical, laboratory, and outcome data on all patients under 5 years of age who were admitted between January 2001 and December 2011 to King’s College Hospital with ALF secondary to an inherited metabolic disease (IMD), a common cause of pediatric acute liver failure. Thirty-six of 127 children with ALF had a metabolic etiology: galactosemia (17); mitochondrial respiratory chain disorder (MRCD, 7); ornithine transcarbamylase (OTC) deficiency (4); tyrosinemia type 1 (4); Niemann-Pick disease type C (NPC, 3); and congenital disorder of glycosylation type 1b (1). Seven children died: MRCD (4) and NPC (3). Four children were transplanted: OTC deficiency (1) and MRCD (3). Fifteen of 25 children followed up showed evidence of developmental delay.
Conclusion: IMD is the most common group of disorders in this age group; indeterminate cases may yet include undiagnosed metabolic disorders; the overall survival rate is good but largely depends on diagnosis, while developmental outcome of the surviving patients is less favorable.
What is Known: • Up to half of children with ALF may be undiagnosed. • IMD is a common cause of pediatric acute liver failure. |
What is New: • Initial diagnostic clues may be gathered from the child’s age and laboratory parameters. • Survival of children with IMD-related ALF is good, but developmental outcome is less favorable. • In the future, novel sequencing methods will aid in the diagnosis of disorders in which therapeutic decisions depend upon. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
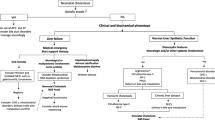
Acute liver failure (ALF) is a rare condition that is often fatal without liver transplantation [4, 5, 12]. The management and outcome depends on the underlying etiology. Given the rapidity in which the disease can progress, the family and treating professionals are under tremendous pressure to make therapeutic decisions like liver transplantation. It is not uncommon for these patients to be listed for liver transplantation while waiting for investigations to be completed. However, diagnostic difficulties pose a challenge [10]: turnaround time of diagnostic tests can take several weeks; additionally, neurological involvement at presentation can be difficult to establish whether it is due to hepatic encephalopathy (HE), part of the underlying, multi-system disease, or both. Current literature reports about half of children with ALF fall under the indeterminate category while inherited metabolic disease (IMD) is a common cause [1, 6, 17]. To date, no studies have evaluated IMD-related ALF in isolation.
The aim of this study was to describe the characteristics of newborns and young children under 5 years of age with ALF secondary to an IMD with regard to their presentation, management, and outcome.
Materials and methods
Medical records of 127 children under 5 years of age who were admitted between January 2001 and December 2011 to King’s College Hospital with ALF were reviewed. The definition of ALF was as follows: (1) children with no known evidence of chronic liver disease, (2) biochemical evidence of acute liver injury, and (3) hepatic-based coagulopathy defined as a prothrombin time (PT) ≥ 15 s or international normalized ratio (INR) ≥ 1.5 not corrected by Vitamin K in the presence of clinical HE or a PT ≥ 20 s or INR ≥ 2.0 regardless of the presence or absence of clinical HE [2, 16, 17].
Thirty-six children had an underlying IMD, and details on their demographics, medical history, and physical examination findings were obtained. Peak levels of white blood cell (WBC) count, aspartate aminotransferase (AST), bilirubin, INR, and creatinine as well as trough levels of albumin were recorded. Metabolic investigations were carried out depending on the clinical presentation of each individual patient [15]. It included analyzing levels of the following: ammonia, lactate, acylcarnitine profile, urine reducing substances and organic acids, amino acids (urine and plasma), succinylacetone (urine and plasma), galactose-1-phosphate uridyl transferase, very long chain fatty acids, chitotriosidase, alpha-1-antitrypsin phenotype, alphafetoprotein, 24-h urinary copper, serum ceruloplasmin, urinary bile acids, and glycogen branching enzyme from leucocytes. Urinary sugars and polyols were tested in the last 5 years of the study.
The diagnosis of neonatal hemochromatosis when suggested by serum ferritin and total iron binding capacity was confirmed by excess iron deposition seen on buccal mucosa (or liver, heart, or pancreas at autopsy).
Screening for viral hepatitis included serological testing for the following: hepatitis A to E virus, cytomegalovirus, Epstein-Barr virus, adenovirus, herpes simplex virus, parvovirus, and human immunodeficiency virus.
Liver ultrasound scan was performed in all children and neuroimaging in ten children.
Liver histology was available in nine children, bone marrow aspiration in seven children, skin biopsy in six children, and muscle biopsy in five children.
All children diagnosed with tyrosinemia were started on treatment with nitisinone and a protein-controlled diet. Patients suspected of having galactosemia were placed on a galactose-free diet.
Decision for orthotopic liver transplantation (OLT) was based on the National Health Service Blood and Transplant Liver Advisory Group policy, although an INR greater than four was the main parameter used [5, 11].
Information on the presence or absence of developmental delay was obtained by retrospective case note review or questionnaires directed to their respective pediatrician. Developmental data was available for 25 of 29 surviving children.
Statistics
IBM SPSS V22 was used for the statistical analysis. Mann-Whitney U test was used for the comparison of laboratory values from one diagnostic group against the other groups combined. P values were considered to be statistically significant when <0.05.
Results
Etiology
A total of 127 newborns and young children were identified from the database. The etiologies were as follows: indeterminate in 40 patients (32 %), IMD in 36 (28 %), infectious in 15 (12 %), gestational alloimmune liver disease in 11 (9 %), hemophagocytic syndrome in 8 (6 %), drug toxicity in 5 (4 %), and other in 10 (8 %). Out of the 127 patients, 41 received OLT.
Among the 36 patients (17 boys) with an underlying IMD, the diagnoses were as follows: galactosemia in 17, mitochondrial respiratory chain disorder (MRCD; complex IV deficiency in 5, complex III and IV deficiency in 1, and complex I, III, and IV deficiency in 1) in 7, ornithine transcarbamylase (OTC) deficiency in 4, tyrosinemia type 1 in 4, Niemann-Pick disease type C (NPC) in 3, and congenital disorder of glycosylation (CDG) type 1b in 1.
Demographic and clinical data
The median presenting age of the patients with an IMD was 6 weeks (1 day–41 months). Age distribution at presentation was as follows: 20 newborns less than 1 month (56 %), 9 infants between 1 month and 1 year (25 %), and 7 children between 1 and 5 years (23 %). The median ages of presentation according to diagnosis were as follows: 1 week for galactosemia, 1 week for NPC, 2 weeks for CDG type 1b, 1 month for tyrosinemia type 1, 5 months 3 weeks for MRCD, and 1 year 5 months for OTC deficiency. History of parental consanguinity was present in 16 cases. The following clinical features were identified at presentation: jaundice in 29 (80 %), hepatomegaly in 27 (75 %), splenomegaly in 8 (22 %), and HE in 7 (19 %).
The demographic and clinical data according to etiology are listed in Table 1.
Laboratory data and further investigations
The median peak INR was 4.8 (range, 1.8–15), AST 334 μmol/L (range, 39–10,710), bilirubin 227 μmol/L (range, 13–692), and median trough albumin 26 g/dL (range, 18–39). Box plots of peak laboratory values according to etiology are listed in Fig. 1. Some characteristics were found when laboratory values from one group were compared to the rest combined. In galactosemia, the median peak bilirubin was higher and AST lower compared to the rest of the groups combined (p < 0.05); in OTC deficiency, the median peak bilirubin was lower and AST higher (p < 0.05); in tyrosinemia, the median peak bilirubin, AST and albumin were all lower (p < 0.05); in NPC, the median peak bilirubin was higher (p < 0.05). The median peak INR, WBC count, and creatinine were similar between groups. The time it took for the INR to normalize was available for galactosemia (median of 3 days).
Liver histology was available in 9 children. Five of these children had MRCD, 1 had OTC deficiency, 1 had galactosemia, 1 had CDG type 1b, and 1 had NPC. Seven children had bone marrow analysis which led to the diagnosis of NPC in 3. Five children had muscle mitochondrial respiratory chain enzymology which led to the diagnosis of MRCD in 4. Six children had skin biopsy and fibroblast culture which contributed to the diagnosis of NPC in 1. Ten children had neuroimaging (computed tomography or magnetic resonance imaging). Abnormal neuroimaging was reported in 6 children (5 with MRCD and 1 with NPC).
Outcome
Twenty-nine of 36 children (81 %) with an IMD survived. The diagnoses of the 7 deceased children were MRCD in 4 and NPC in 3. Among the 4 infants with MRCD, 2 received OLT, both of whom did not have a diagnosis at the time of transplantation. The causes of death in these 4 infants were the following: disease progression in 3; multi-organ failure in the post operative period after OLT in 1.
Of the surviving children, 2 (1 OTC deficiency, 1 MRCD) underwent OLT. Follow-up data was available for 25 children with a mean follow-up period of 4 years 3 months. Fifteen (60 %) were identified as having evidence of developmental delay (DD). Patient outcomes according to etiology are listed in Table 2. All patients with galactosemia survived, and 6 out of 14 patients followed up do not have any evidence of DD. Three out of 7 patients with MRCD survived, all of whom have evidence of DD. All patients with OTC deficiency survived, and 2 out of 4 patients followed up do not have any evidence of DD. All 3 patients with tyrosinemia type 1 survived, and 2 patients followed up do not have any evidence of DD. All patients with NPC died, and 1 patient with CDG1b is alive with evidence of DD.
Discussion
The purpose of this study was to characterize newborns and young children with ALF with an underlying metabolic etiology—the largest group of disorders found in this study. The most common diagnosis within this category was galactosemia. MRCD were the second most common and above tyrosinemia and OTC deficiency. This pattern of diagnosis was consistent with the findings in the Pediatric Acute Liver Failure Study Group data of infants under 1 year of age [18].
Galactosemia was the most common metabolic diagnosis, and together with tyrosinemia, type 1 comprised over half of the study cohort. While mass screening for galactosemia does not seem to reduce the long-term complications [8], it has been shown to reduce acute mortality and morbidity to some extent [14]. The Newborn Blood Spot Screening in the UK currently does not test for galactosemia and tyrosinemia. However, given the relative frequency of these conditions seen in our study, mass screening for galactosemia and tyrosinemia will help in early identification and treatment of these conditions.
With MRCD being the second most common metabolic cause, it is important to correctly establish its diagnosis. This is even more significant when there is multi-system disease involvement which may contraindicate OLT. Two patients in our series with MRCD received OLT before muscle biopsy was undertaken due to rapidly deteriorating clinical condition. We later identified a mutation in DGUOK in one patient. In the acute setting where there is a short time period between presentation of the patient and decision to perform OLT, muscle biopsy enzymology for MRCD may not be the most convenient mean of ruling out mitochondrial DNA depletion. Furthermore, mitochondrial DNA depletion detected only in liver biopsy without confirmation on genetic mutation analysis may be secondary to liver failure itself. Therefore, genetic mutation analysis for mitochondrial disease may be the most efficient and convenient way in this setting to rule out MRCD and avoid futile OLT [9]. Rapid genetic diagnosis in MRCD should soon become a reality with the introduction of novel sequencing methods into clinical practice. However, on benefit of doubt grounds, liver transplantation continues to be offered rightly to these children in the absence of gross neurological abnormalities.
On the contrary, we did not identify any cases of fatty acid oxidation defect (FAOD) which had been reported previously as a relatively frequent metabolic cause of ALF [17]. Presenting features in some patients in the indeterminate group were very strongly suggestive of a metabolic etiology. For example, two children in this group presented with recurrent transaminitis, HE, and nonketotic hypoglycemia, but despite extensive investigation for FAODs including genetic studies for Acyl-CoA dehydrogenase 9 deficiency (ACAD9), no underlying cause was found [7]. Following negative tests, they were assigned to the indeterminate group when a diagnosis could not be established. It is possible that further more detailed investigations could have assigned a diagnosis of IMD in some of the indeterminate cases particularly in those who died or were transplanted; the latter of which would have provided cure to the defect. Nonetheless, the rate of indeterminate cases in this study was similar compared to previous studies, and improving diagnostic yield still remains a challenge [1, 6, 17].
We also sought to identify biochemical characteristics that may be attributable to the diagnoses. Combined with the age of the patient, these may provide some useful diagnostic clues. In the neonatal period, the differential diagnosis may include the following: galactosemia, MRCD, tyrosinemia type 1, NPC, and CDG type 1b. Galactosemia characteristically exhibited relatively high levels of bilirubin and low levels of AST; the time it took for the INR to normalize was relative quick. In tyrosinemia type 1, bilirubin and AST were relatively low. While in NPC, bilirubin levels were characteristically high. In older infants and young children, MRCD and OTC deficiency must be considered. In OTC deficiency, AST levels were characteristically high and bilirubin levels low. We did not find the extent of coagulopathy, WBC, and creatinine was associated with a particular diagnosis.
Overall, 29 of 36 (81 %) children with an IMD survived. This is higher when compared to studies looking at all causes of ALF in infants [6, 18] and all children [1, 17]. All children with galactosemia, OTC deficiency, tyrosinemia, and CDG type 1b survived. However, survival is notably lower in MRCD (29 %), and no patients with NPC survived. OLT was conducted in four patients with MRCD and two patients with OTC deficiency. Among the 29 surviving patients, follow-up data was available for 25. Evidence of DD was seen across all conditions. In OTC deficiency, evidence of DD was seen in half (one of whom received OLT) compared to a rate of cognitive impairment and/or DD of 44 % in a cross sectional, observational study of children and adults with OTC deficiency [13]. Data from patients with a urea cycle defect who were transplanted showed that the average developmental quotient was 69, although this improved with age and favored those that received early OLT [3].
In summary, we observed that IMD is the most common group of disorders that cause ALF in newborns and young children. Diagnostic clues may be gained from the presence of consanguinity, presenting age and biochemical characteristics. Galactosemia was the most common etiology, and together with tyrosinemia, newborn screening will help reduce the acute morbidity from these disorders. MRCD was found to be the second most common metabolic disorder following galactosemia, and its diagnosis must be established with priority and accuracy to avoid futile OLT. It is possible that indeterminate cases may include children with undiagnosed or novel FAOD or other metabolic disorders. These challenges associated with the diagnosis of MRCD or novel disorders must be met by: contemporaneous integration with molecular genetics laboratories; advanced diagnostic techniques, particularly next generation sequencing, if timely results can be obtained. The overall survival rate of newborns and young children with metabolic ALF is good but largely depends on the diagnosis; developmental outcome of the surviving patients is less favorable.
Abbreviations
- ACAD9:
-
Acyl-CoA dehydrogenase 9 deficiency
- ALF:
-
Acute liver failure
- AST:
-
Aspartate aminotransferase
- CDG:
-
Congenital disorder of glycosylation
- DD:
-
Developmental delay
- FAOD:
-
Fatty acid oxidation defect
- HE:
-
Hepatic encephalopathy
- IMD:
-
Inherited metabolic disease
- INR:
-
International normalized ratio
- MRCD:
-
Mitochondrial respiratory chain disorder
- NPC:
-
Niemann-Pick disease type C
- OLT:
-
Orthotopic liver transplantation
- OTC:
-
Ornithine transcarbamylase
- PT:
-
Prothrombin time
- WBC:
-
White blood cell
References
Bariş Z, Saltik Temızel IN, Uslu N, Usta Y, Demır H, Gürakan F, Ozen H, Yüce A (2012) Acute liver failure in children: 20-year experience. Turk J Gastroenterol 23:127–134
Bhaduri BR, Mieli-Vergani G (1996) Fulminant hepatic failure: pediatric aspects. Semin Liver Dis 16:349–355
Campeau PM, Pivalizza PJ, Miller G, McBride K, Karpen S, Goss J, Lee BH (2010) Early orthotopic liver transplantation in urea cycle defects: follow up of a developmental outcome study. Mol Genet Metab 1:S84–S87
Dhawan A, Cheesman P, Mieli-Vergani G (2004) Approaches to acute liver failure in children. Pediatr Transplant 8:584–588
Dhawan A, Mieli-Vergani G (2005) Acute liver failure in neonates. Early Hum Dev 81:1005–1010
Durand P, Debray D, Mandel R, Baujard C, Branchereau S, Gauthier F, Jacquemin E, Devictor D (2001) Acute liver failure in infancy: a 14-year experience of a pediatric liver transplantation center. J Pediatr 139:871–876
He M, Rutledge SL, Kelly DR, Palmer CA, Murdoch G, Majumder N, Nicholls RD, Pei Z, Watkins PA, Vockley J (2007) A new genetic disorder in mitochondrial fatty acid beta-oxidation: ACAD9 deficiency. Am J Hum Genet 81:87–103
Jumbo-Lucioni P et al (2012) Diversity of approaches to classic galactosemia around the world: a comparison of diagnosis, intervention, and outcomes. J Inherit Metab Dis 35:1037–1049
McKiernan PJ, Ball S, Santra S, Gupte G, Sharif K, Hickman K, McFarland R, Fratter C, Poulton J, Rahman S, Taylor RW (2013) Incidence of mitochondrial disease in children presenting with acute liver failure under 2 years of age. J Pediatr Gastroenterol Nutr 56S2:62
Narkewicz MR, Dell Olio D, Karpen SJ, Murray KF, Schwarz K, Yazigi N, Zhang S, Belle SH, Squires RH (2009) Pattern of diagnostic evaluation for the causes of pediatric acute liver failure: an opportunity for quality improvement. J Pediatr 155:801–806
National Health Service Blood and Transplant (2013) Liver transplantation; selection criteria and recipient registration. [PDF] Available via http://www.odt.nhs.uk/pdf/liver_selection_policy.pdf [Accessed 12 September 2014]
Psacharopoulos HT, Mowat AP, Davies M, Portmann B, Silk DB, Williams R (1980) Fulminant hepatic failure in childhood: an analysis of 31 cases. Arch Dis Child 55:252–258
Rüegger CM, Lindner M, Ballhausen D et al (2014) Cross-sectional observational study of 208 patients with non-classical urea cycle disorders. J Inherit Metab Dis 37:21–30
Schweitzer-Krantz S (2003) Early diagnosis of inherited metabolic disorders towards improving outcome: the controversial issue of galactosemia. Eur J Pediatr 162:S50–S53
Shanmugam NP, Bansal S, Dhawan A (2012) Acute liver failure in children and adolescents. In: Dhawan A (ed) Concise pediatric and adolescent hepatology. Karger, Basel, Chapter 2
Squires RH Jr (2008) Acute liver failure in children. Semin Liver Dis 28:153–166
Squires RH Jr, Shneider BL, Bucuvalas J et al (2006) Acute liver failure in children: the first 348 patients in the pediatric acute liver failure study group. J Pediatr 148:652–658
Sundaram SS, Alonso EM, Narkewicz MR, Zhang S, Squires RH, Pediatric Acute Liver Failure Study Group (2011) Characterization and outcomes of young infants with acute liver failure. J Pediatr 159:813–818
Acknowledgments
We thank Ashish Dhawan, an honorary research assistant, for his help in collecting data.
Conflict of interest
The authors declare that they have no conflict of interest.
Authors’ contributions
AD came up with the idea of the article. RH collected the data and drafted the manuscript. NH, PG, and AD were involved in critically revising it. All authors approved the final version of the manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Peter de Winter
Rights and permissions
About this article
Cite this article
Hegarty, R., Hadzic, N., Gissen, P. et al. Inherited metabolic disorders presenting as acute liver failure in newborns and young children: King’s College Hospital experience. Eur J Pediatr 174, 1387–1392 (2015). https://doi.org/10.1007/s00431-015-2540-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-015-2540-6