Abstract
The focus on urogenital mycoplasmas as the possible etiologic agents of urogenital infections and syndromes, has increased in the last decade. Of these, Mycoplasma genitalium is proven to be pathogenic and sexually transmitted. We compared five commercially available assays for the detection of these organisms in urogenital mycoplasma culture specimen remnants. Stored specimen remnants were tested on Aptima Mycoplasma genitalium, Allplex™ STI Essential and CGMT, ResitancePlus®MG and Allplex™ MG & AziR Assays. All positive M. genitalium specimens and culture negative, nucleic acid positive Ureaplasmas were sent to the National Microbiology Laboratory for confirmation. The Aptima Mycoplasma genitalium assay detected 7 M. genitalium infections, the Allplex™ STI-EA and the Allplex™ CGMT detected 6 M. genitalium positives, and the Allplex™MG and AziR and SpeeDx ResistancePlus® MG detected 5 M. genitalium positives, four with macrolide resistant genes. The Allplex™ STI Essential assay was 100% sensitive and specific for Mycoplasma hominis and Ureaplasma targets. As seen in other studies, the Aptima Mycoplasma genitalium assay was 100% sensitive and specific for the detection of M. genitalium. The multiplex assays had lower sensitivities for M. genitalium detection (Allplex™ STI Essential and CGMT sensitivity of 85.71%; Allplex™ MG & AziR and SpeeDx ResistancePlus® MG sensitivity of 71.43%) with high specificities of 100%. Assays tested have high sensitivities and specificities for the detection of urogenital mycoplasmas especially M. genitalium macrolide resistance markers. All labs wanting to perform onsite detection of these organisms will find an assay to easily fit into their workflow.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The focus on urogenital mycoplasmas as the possible etiologic agents of urogenital infections and syndromes, has increased in the last decade. These intracellular, cell wall deficient organisms present many difficulties in regards to specimen transportation, culture and antimicrobial susceptibility testing in clinical laboratories. The rapid evolution of molecular detection assays has thus been instrumental in the recent increased focus on this family of organisms.
Mycoplasma genitalium has so far been the only organism in this group proven to be a “true” sexually transmitted pathogen. The organism was first isolated from the urine of two males with non-gonococcal urethritis (NGU) and was thus first associated with male NGU, and, was subsequently shown to have an even stronger association with non-chlamydial NGU; with some evidence that it can cause proctitis [1]. Although often asymptomatic in females, M. genitalium is associated with cervicitis, endometritis and pelvic inflammatory disease [2]. A meta-analysis has also associated M. genitalium with preterm birth, spontaneous abortion and female infertility [3]. With reported global prevalence rates of 1–6% rising as high as 38% in high risk populations [2], the burden of this sexually transmitted infection lies between that of Neiserria gonorrhoeae and Chlamydia trachomatis. In addition, M. genitalium stimulates HIV replication [4], has been shown to convey a twofold increased risk of HIV infection among infected individuals [5], and M. genitalium infection likely increases HIV transmission to uninfected partners [6].
The American [7], European [8], Australian [9], United Kingdom [10] and Canadian [11] Sexually Transmitted Infections (STI) guidelines all recommend testing for and treating M. genitalium infection. Highly sensitive nucleic acid testing is the test of choice for detection since culture is less sensitive and M. genitalium grows slowly with cultures taking six weeks to six months. In contrast, there are no recommendations for the routine detection and treatment of Mycoplasma hominis, Ureaplasma urealyticum or Ureaplasma parvum. The American [7], European [8] and Canadian STI Guidelines [11] state that there is insufficient evidence to make any recommendations regarding these organisms as genitourinary pathogens. Our laboratory, a provincial referral and public health facility, continues to culture urogenital specimens for Mycoplasma and Ureaplasma species, a process that was implemented decades ago when the role of these organisms was less clear. There is no evidence that by reporting these organisms, we are doing more good than harm and a recent position statement by the European STI Guidelines Editorial Board recommended against routine testing and treatment for asymptomatic or symptomatic men and women for M. hominis, U. urealyticum and U. parvum [12]. The European statement only recommends testing for U. urealyticum in males with symptomatic urethritis after N. gonorrhoeae, C. trachomatis, M. genitalium and Trichomonas vaginalis (in settings with high prevalence) have been excluded and treatment only for males with high U. urealyticum loads.
We undertook this single site quality improvement study primarily to assess the sensitivity of culture of urogenital specimens for urogenital mycoplasmas, compared to that of five commercial molecular assays. We also sought to assess the ease of use, labor required and ease of introduction into the current work flow of our laboratory for each of the assays.
Materials and methods
Biological specimens
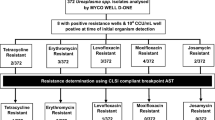
One hundred stored remnants of all genital and sterility specimens (30 culture positive and 70 culture negative) submitted to our laboratory from June to August 2018 for Mycoplasma culture were tested (Table 1). These specimens were submitted from province wide communities.
Laboratory testing
The commercial assays for M. genitalium evaluated were the Aptima Mycoplasma genitalium Assay (Hologic®, Massachusetts, USA), Allplex™ STI Essential Assay, Allplex™ CGMT (Seegene Technologies Inc., Seoul, South Korea), ResitancePlus®MG (SpeeDx, Sydney, Australia) (MgPa, A2058T, A2058C, A2058G, A2059C, A2059G,) and Allplex™ MG & AziR (Seegene Technologies Inc., Seoul, South Korea) (MgPa, A2058T, A2058C, A2058G, A2059C, A2059G, A2059T). The characteristics of each assay is outlined in Table 2.
One positive M. genitalium sample was serially diluted and tested to compare the relative limit of detection of the assays since culture isolates were not available. In addition, blinded panels from the National Microbiology Laboratory (NML) were used; a 10 sample panel consisting of 2 M. genitalium, one M. hominis, one U. urealyticum and 3 U. parvum positive and 3 negative specimens, were tested on all assays and a panel of five M. genitalium positive samples with known mutations was tested on the two assays that detected macrolide resistance mutations.
All clinical samples were extracted using the EasyMag system (Biomerieux, North Carolina, USA). Samples received from NML were extracted using the EasyMag or manually with the Qiagen QIAamp DNA mini kit if in Aptima (Hologic®, Massachusetts, USA) media. The DNA extracts of all positive M. genitalium specimens were sent to NML for confirmation by MgPa and to determine the presence of antimicrobial resistance mutations by sequencing the 23S rRNA, gyrA and parC genes [13]. Culture negative, nucleic acid positive U. urealyticum and U. parvum on the Allplex™ were confirmed by sequencing the Ureaplasma spp. EF-Tu and Ureaplasma 16S rRNA genes [14].
Statistical methods
Calculations of the relative limit of detection (LOD) and sensitivity and specificity were performed for each commercial assay for the detection of their respective targets in the specimens.
Ethics approval for the study was obtained from the Human Research Ethics Board at the University of Alberta.
Results
The 22 culture negative sterility specimens tested negative on all assays for all targets. Of the 100 remnant specimens tested, results for the 78 clinical specimens are summarized in Table 3.
The Aptima Mycoplasma genitalium assay detected 7 M. genitalium infections, the Allplex™ STI-EA and the Allplex™ CGMT detected 6 M. genitalium positives, and the Allplex™MG and AziR and SpeeDx ResistancePlus® MG detected 5 M. genitalium positives. The M. genitalium prevalence in this study was thus 8.97%, comparable to that of previous studies in our province [15, 16]. All 7 M. genitalium positives were confirmed by NML. The assays detected all of the Ureasplasma culture positive samples as either U. urealyticum or U. parvum or both. Nine of the 22 (40.9%) culture positives reported as U. urealyticum were reported correctly; the other isolates were U. parvum. Culture cannot distinguish U. urealyticum from U. parvum and historic reporting of all culture positive, urea positive organisms on the Mycoplasma culture bench as U. urealyticum, was maintained. All of the culture positive M. hominis were detected. As is common when comparing molecular assays to culture, the assays detected two M. hominis and 6 U. parvum that did not grow in culture. The two M. hominis that were missed in culture were detected in specimens from which U. urealyticum were cultured.
Macrolide resistance gene detection was similar on Seegene and SpeeDx assays with the Seegene assay results providing the specific single nucleotide polymorphism (SNP) responsible for resistance (Table 4). The A2058G mutation was found in 3 of the 4 specimens with macrolide resistance markers. The two M. genitalium positive specimens that were not detected on the resistance assays had the A2059G mutation when tested at NML.
The sensitivity and specificity of the assays are listed in Table 5. The NML result was used to resolve discrepant results between culture and the assays. The Allplex™ STI Essential assay was highly sensitive (100%) and specific (100) for M. hominis, U. urealyticum and U. parvum targets. As seen in other studies, the Aptima Mycoplasma genitalium assay is highly sensitive (100%) and specific (100%) for the detection of M. genitalium. The multiplex assays had lower sensitivities for M. genitalium detection (Allplex™ STI Essential and CGMT had the same sensitivity of 85.71%; Allplex™ MG & AziR and SpeeDx ResistancePlus® MG both had sensitivities of 71.43%) while they all maintained high specificities of 100%.
Testing of the blinded panels produced 100% concordance on all assays.
The relative LOD and end point variability of the assays were tested by performing ten-fold serial dilutions on one specimen and testing these in triplicate over two days. All assays detected M. genitalium in the 10–3 dilution. The number of cycles for target detection (ct) increased as expected by three cycles for each dilution. The Allplex™ STI-EA is almost a log more sensitive that the Allplex™ MG & AziR assay, as was observed with one M. genitalium positive specimen (ct of 37.5 on the Allplex™ STI-EA and 39.8 on the Allplex™ CGMT) that was not detected on this assay. End point variation began at a ct of 37 for the Allplex™ STI Essential and the Allplex™ CGMT assays, at a ct of 40 for the Allplex™ MG & AziR assay and at a ct of > 30 for the SpeeDx ResistancePlus® MG assay (Tables 6, 7). Since quantified M. genitalium organisms were not available for this study, similar testing of the Hologic assay was not performed.
The workflow (Table 8) for the Seegene and SpeeDx assays were the same requiring all the same steps and hands-on time (75 min) with the Hologic assay requiring only 15 min for a larger specimen volume (250 versus 96). The assay run time was fastest for the SpeeDx assay (40 min), slowest for the Hologic assay (180 min) with 120 min for the Seegene assays.
Discussion
The results of our study confirm that the molecular assays we tested were more sensitive than culture. As anticipated, the use of more sensitive nucleic acid amplification (NAA) tests also detected previously undiagnosed M. genitalium infections that could not be detected using culture. We suspect that most clinicians are unaware that the routinely offered culture for urogenital mycoplasmas does not identify M. genitalium due to its fastidious and very slow growth. The Hologic assay emerged as the most sensitive (100%) for M. genitalium detection and is consistent with other studies which have reported sensitives ranging from 99.1 to 100% in the Nordic countries [17] and 100% in a French study [18]. The M. genitalium detection rate in this small convenience sample was 8.9%, which is similar to our previous studies reporting prevalence rates of 7.4% and 6.2% among female and male STI clinic attendees in Alberta [15, 16]. Despite this assay’s high sensitivity, it is at a disadvantage due to the lack of macrolide resistance gene detection. Mutations that confer antibiotic resistance to macrolides for M. genitalium are concentrated in nucleotide positions 2058 and 2059 in region V of the 23S rRNA gene [19]. Jensen et al. first reported azithromycin failure in patients with M. genitalium associated with induced macrolide resistance and mutations in the 23S rRNA gene [19]. Since then multiple studies have confirmed the rapid emergence of mutations conferring resistance to macrolides [20,21,22,23,24,25,26]. Many guidelines now recommend that all positive M. genitalium assays be reflex tested to determine mutations for macrolide resistance to guide treatment [8,9,10,11]. The majority of specimens identified with 23S rRNA macrolide resistance conferring mutations in this study were A2058G, which is similar to other Canadian studies [27].
To the best of our knowledge, ours is the first study to directly compare the performance of the two commercially available assays that detect M. genitalium and macrolide resistance markers. Both assays had the same sensitivity and specificity (Table 5) with the Allplex™ MG & AziR assay detecting six macrolide resistance mutation SNPs and providing the detected SNP in the result. This is useful for surveillance purposes. The ResitancePlus®MG detects five macrolide resistance mutation SNPs reporting the results as either mutant type or wild type (Table 4). Macrolide resistance mutations were detected in 6 of the 7 samples that tested positive for M. genitalium. While these numbers are too small to infer a macrolide resistance rate for this study, it is consistent with the high the rates (53.3% and 56.5%) of macrolide resistance of M. genitalium in our province [15, 16]. With one multi-center Canadian study reporting an overall macrolide resistance of 40% in Canada [15], real-time macrolide resistance gene detection is necessary to guide appropriate patient management.
Interestingly, U. urealyticum, U. parvum and M. hominis were identified in 53.8% of the tested specimens (8.9%, 29.5% and 15.4% respectively). These organisms are frequently found in the urogenital tract in both healthy and symptomatic individuals [28]. The role of these organisms as pathogens in the human urogenital tract has been controversial for many years but a recent position statement from the European STI Guidelines Editorial Board argues against the routine testing for these organisms [12]. The rationale for this recommendation is that U. urealyticum in high bacterial loads might cause a small proportion of NGU but the majority of men infected with U. urealyticum do not develop disease and, antibiotic treatment which results in clearance of infection is difficult [12]. Unfortunately, this will be challenging since many commercially available assays for urogenital mycoplasmas offer testing for multiple organisms including U. urealyticum, U. parvum and M. hominis. The European guidelines recommend testing for U. urealyticum only in symptomatic males when other traditional STI organisms (N. gonorrhoeae, C. trachomatis, M. genitalium and T. vaginalis) have been excluded. Unfortunately, since our study was laboratory based, we were unable to determine if the samples were submitted from symptomatic persons. Horner et al. also recommend against testing for M. hominis and U. parvum and instead that other STIs and bacterial vaginosis be diagnosed and treated. The US and Canadian STI guidelines make no specific recommendation for or against screening for non M. genitalium mycoplasmas citing insufficient data to make specific recommendations [7, 11].
It is well known that multiplex assays compromise on sensitivity to provide simultaneous detection of numerous targets. It was thus not surprising that the multiplex assays had lower sensitivities (sensitivity of M. genitalium detection of the Allplex STI EA and the Allplex™ CGMT = 85.71%). M. genitalium plus macrolide resistance gene detection assays had the lowest M. genitalium detection sensitivities of all the assays tested as they missed the detection of M. genitalium in two specimens; giving both of these assays a sensitivity of 71.4%. However, when compared to an inability of culture to detect M. genitalium in a clinical laboratory, these sensitivities provide a vast improvement. The lower sensitivities obtained in this study may be attributed to the use of frozen specimen remnants. Le Roy et al. and Tabrizi et al. found higher sensitivities of 98. 9 and 98.5% respectively, using the SpeeDx ResistancePlus® MG [29, 30]. It is reassuring in our study that these assays maintained a high specificity of 100%.
The relative limit of detection for the Seegene and SpeeDex assays were the same. For the Allplex™ STI Essential and Allplex™ CGMT panel assays, the manufacturer recommends a ct cutoff of < 40 for positive results. Since the observed end point variation for these assays in this study began at around a ct of 37, the cutoff for routine testing may need to be adjusted during validation and verification of the assay. A similar finding with the Allplex™ MG & AziR where end point variation was seen around a ct of 40 and the manufacturer recommends a ct cutoff of ≤ 45 for positive results. On the SpeeDx ResistancePlus® MG assay, end point variation occurred around a ct of 30. This assay has no interpretive recommendations as the assay software (Fastfinder by UgenTec, Hasselt, Belgium) performs the interpretation and provides the result.
There are a few limitations to our study. Firstly, it is a single center study evaluating a small convenience sample of frozen stored urogenital specimens thus making it difficult to accurately assess prevalence of infection and macrolide resistance. Since the specimens were submitted without accompanying clinical information, we were unable to determine if these were from symptomatic persons and/or if they had received previous treatment but we suspect that the samples were likely from patients with recurrent/repeated symptoms and those who had failed empiric therapy as recommended in the Canadian STI Guidelines [11]. Since only a small proportion of specimens were vaginal swabs (7.7%), we were unable to assess the difference in test performance by urogenital specimen type. Finally, the lack of quantified cultured organisms of each species, prevented the determination of true limits of detection for each assay.
Conclusion
Our study demonstrated that the evaluated commercial assays have high sensitivities and specificities for the detection of urogenital mycoplasmas and in particular, the detection of M. genitalium macrolide resistance markers. We also confirmed the high prevalence of organisms (M. hominis, U. parvum, U. urealyticum) now considered to be primarily non-pathogenic in most clinical situations. Selection of assay will depend on the specimen volume and workflow of different clinical laboratories. Consideration should be given to suppressing the results for non M. genitalium mycoplasma species from multiplex assays except in select situations (e.g., positive results for U. urealyticum in symptomatic males with NGU where other STI pathogens have been excluded) as a positive result may result in inappropriate treatment. Future research should investigate the unresolved issues regarding non M. genitalium mycoplasmas.
Data availability
The anonymized data is available and can be provided upon request.
References
Taylor-Robinson D, Jensen JS (2011) Mycoplasma genitalium: from Chrysalis to multicolored butterfly. Clin Microbiol Rev 24(3):498–514
Manhart LE, Broad JM, Golden MR (2011) Mycoplasma genitalium: should we treat and how? Clin Infect Dis 53(Suppl 3):S129–S142
Lis R, Rowhani-Rahbar A, Manhart LE (2015) Mycoplasma genitalium infection and female reproductive tract disease: a meta-analysis. Clin Infect Dis 61(3):418–426
Sasaki Y, Honda M, Makino M, Sasaki T (1993) Mycoplasmas stimulate replication of human immunodeficiency virus type 1 through selective activation of CD4+ T lymphocytes. AIDS Res Hum Retroviruses 9(8):775–780
Napierala MS, Weiss HA (2009) Association of Mycoplasma genitalium and HIV infection: a systematic review and meta-analysis. AIDS 23(5):611–620
Martin DH, Manhart LE, Workowski KA (2017) Mycoplasma genitalium from basic science to public health: summary of the results from a national institute of allergy and infectious diseases technical consultation and consensus recommendations for future research priorities. J Infect Dis 216(S2):S427–S430
Workowski KA, Bolan GA (2015) Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep 64(3):1–136
Jensen JS, Cusini M, Gomberg M, Moi H (2016) European guideline on Mycoplasma genitalium. JEADV 30(10):1650–1656
The Australasian STI Management Guidelines. http://www.sti.guidelines.org.au/. Accessed March 12, 2020
Soni S, Horner P, Rayment M, Pinto-Sander N, Naous N, Parkhouse A, Bancroft D, Patterson C, Fifer H (2019) British association for sexual health and HIV national guideline for the management of infection with Mycoplasma genitalium (2018). Int J STD AIDS 30(10):938–950
Canadian Guidelines on Sexually Transmitted Infections—Management and treatment of specific infections—Mycoplasma genitalium Infections. https://www.canada.ca/en/public-health/services/infectious-diseases/sexual-health-sexually-transmitted-infections/canadian-guidelines/sexually-transmitted-infections/canadian-guidelines-sexually-transmitted-infections-49.html. Accessed March 12, 2020
Horner P, Donders G, Cusini M, Gomberg M, Jensen JS, Unemo M (2018) Should we be testing for urogenital Mycoplasma hominis, Ureaplasma parvum and Ureaplasma urealyticum in men and women? A position statement from the European STI Guidelines Editorial Board. J Eur Acad Dermatol Venereol 32(11):1845–1851
Jensen JS (2012) Protocol for the detection of Mycoplasma genitalium by PCR from clinical specimens and subsequent detection of macrolide resistance-mediating mutations in region V of the 23S rRNA gene. Methods Mol Biol 903:129–139
Daxboeck F, Zitta S, Stadler S, Iro E, Krause R (2005) Mycoplasma hominis and Ureaplasma urealyticum in patients with sterile pyuria. J Infect 51:54–58
Chernesky M, Jang D, Martin I, Hoang LMN, Naidu P, Levett PN, Wylie J, Rebbapragada A, Ratnam S, Smieja M, Weinbaum B, Getman D, Canadian MG Study Group (2017) Mycoplasma genitalium antibiotic resistance-mediating mutations in Canadian women with or without Chlamydia trachomatis infection. Sex Transm Dis 44(7):433–435
Gratrix J, Plitt S, Turnbull L, Smyczek P, Brandley J, Scarrott P, Naidu P, Parker P, Blore B, Bull A, Shokoples S, Bertholet L, Martin I, Chernesky M, Read R, Singh A (2017) Prevalence and antibiotic resistance of Mycoplasma genitalium among STI clinic attendees in Western Canada: a cross-sectional analysis. BMJ Open (Online) 7:e016300. https://bmjopen.bmj.com/content/7/7/e016300.citation-tools. Accessed March 12, 2020
Unemo M, Salado-Rasmussen K, Hansen M, Olsen O, Falk M, Golparian D, Aasterød M, Ringlander J, Stezckó Nilsson C, Sundqvist M, Schønning K, Moi H, Westh H, Jensen JS (2018) Clinical and analytical evaluation of the new Aptima Mycoplasma genitalium assay, with data on M. genitalium prevalence and antimicrobial resistance in M. genitalium in Denmark, Norway and Sweden in 2016. Clin Microbiol Infect 24(5):533–539
Le Roy C, Pereyre S, Hénin N, Bébéar C (2017) French prospective clinical evaluation of the Aptima Mycoplasma genitalium CE-IVD assay and macrolide resistance detection using three distinct assays. J Clin Microbiol 55(11):3194–3200
Jensen JS, Bradshaw CS, Tabrizi SN, Fairley CK, Hamasuna R (2008) Azithromycin treatment failure in Mycoplasma genitalium positive patients with non-gonococcal urethritis is associated with induced macrolide resistance. Clin Infect Dis 47:1546–1553
Manhart LE (2014) Diagnostic and resistance testing for Mycoplasma genitalium: what will it take? Clin Infect Dis 59:31–33
Tagg KA, Jeoffreys NJ, Couldwell DL, Donald JA, Gilbert GL (2013) Fluoroquinolone and macrolide resistance-associated mutations in Mycoplasma genitalium. J Clin Microbiol 51:2245–2249
Nijhuis RH, Severs TT, Van der Vegt DS, Van Zwet AA, Kusters JG (2015) High levels of macrolide resistance-associated mutations in Mycoplasma genitalium warrant antibiotic susceptibility-guided treatment. J Antimicrob Chemother 70:2515–2518
Lau A, Bradshaw CS, Lewis D, Fairley CK, Chen MY, Kong FY, Hocking JS (2015) The efficacy of azithromycin for the treatment of genital Mycoplasma genitalium: a systematic review and meta-analysis. Clin Infect Dis 61:1389–1399
Walker J, Fairley CK, Bradshaw CS et al (2013) Mycoplasma genitalium incidence, organism load, and treatment failure in a cohort of young Australian women. Clin Infect Dis 56:1094–1100
Deguchi T, Yasuda M, Horie K et al (2015) Drug resistance-associated mutations in Mycoplasma genitalium in female sex workers. Japan Emerg Infect Dis 21:1062–1064
Salado-Rasmussen K, Jensen JS (2014) Mycoplasma genitalium testing pattern and macrolide resistance: a Danish nationwide retrospective survey. Clin Infect Dis 59:24–30
Chernesky M, Jang D, Martin I, Arias M, Shah A, Smieja M, Ratnam S, Getman D, Schachter J (2019) Mycoplasma genitalium, Chlamydia trachomatis, and Neisseria gonorrhoeae detected with Aptima Assays performed on self-obtained vaginal swabs and urine collected at home and in a clinic. Sex Transm Dis 46(9):e87-89
Taylor-Robinson D (2017) Mollicutes in vaginal microbiology: Mycoplasma hominis, Ureaplasma urealyticum, Ureaplasma parvum and Mycoplasma genitalium. Res Microbiol 168:875–881
Le Roy C, Hénin N, Bébéar C, Pereyre S (2017) Evaluation of a commercial multiplex quantitative PCR (qPCR) assay for simultaneous detection of Mycoplasma genitalium and macrolide resistance-associated mutations in clinical specimens. J Clin Microbiol 55(3):978–979
Tabrizi SN, Su J, Bradshaw CS, Fairley CK, Walker S, Tan LY, Mokany E, Garland SM (2017) Prospective evaluation of ResistancePlus MG, a new multiplex quantitative PCR assay for detection of Mycoplasma genitalium and macrolide resistance. J Clin Microbiol 55(6):1915–1919
Funding
This project had no external funding. The labor was provided in kind by the laboratories and test kits were provided by the manufacturers at no charge. Seegene Inc. provided the CFX96 as a loan for the duration of the study.
Author information
Authors and Affiliations
Contributions
PN conceived the study, developed the study methodology with NZ and SS, reviewed the study results and authored the manuscript together with AS. SS performed all the testing and collated the results. Irene Martin performed the confirmatory testing. All authors participated in the review and editing of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Prenilla Naidu received honoraria for speaking engagements from Hologic® (2016) and Seegene Inc. (2019). The other authors have no conflicts of interest to declare.
Ethical approval
Ethics approval for the study was obtained from the Human Research Ethics Board at the University of Alberta. The authors confirm that this manuscript reports on results of their original research. This manuscript is not under consideration for publication by any other journal. A small portion of the data (the Seegene assay results) was presented at a workshop at the STI & HIV 2019 World Congress in Vancouver, Canada.
Consent to participate
Remnant specimens submitted for testing of the same organisms by culture were anonymized and used for this study. Consent to participate in this study was thus not required.
Consent for publication
All authors have approved this manuscript for submission for publication.
Additional information
Edited by Volkhard A. J. Kempf.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Naidu, P., Shokoples, S., Martin, I. et al. Evaluation of 5 commercial assays for the detection of Mycoplasma genitalium and other Urogenital Mycoplasmas. Med Microbiol Immunol 210, 73–80 (2021). https://doi.org/10.1007/s00430-021-00699-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00430-021-00699-1