Abstract
The existence of a true mixed germ cell-sex cord stromal tumor (MGSCT) of the testis remains controversial. Based on our experience with rare testicular tumors in this spectrum, we sought to perform a detailed clinicopathologic and molecular study of MGCSCT. Eight cases of testicular MGSCT were morphologically reviewed, screened for chromosomal aberrations (using array comparative genomic hybridization (aCGH) and low pass genomic sequencing), and analyzed by next generation sequencing (The Illumina TruSight Tumor 170). Immunohistochemistry for OCT3/4, Nanog, SALL4, DMRT1, and inhibin was performed on the cohort. Clinical data and follow-up were assessed by medical record review. All patients were karyotypically normal men aged 27–74 years (median 41). All tumors had a similar biphasic morphology characterized by various proportions of the sex cord component resembling granulosa cell tumor of adult type and the germ cell component cytomorphologically akin to spermatocytic tumor. Germ cells were haphazardly scattered throughout the tumor or arranged in larger groups, without tubular formation. In 4 cases, atypical mitoses were found within the germ cells. Additionally, in 2 cases there was invasion into the spermatic cord, adjacent hilar soft tissue and into the tumor capsule, which contained both tumor components. Immunohistochemically, focal nuclear expression of DMRT1 was found in the germ cell component in 7/7 analyzable tumors, while SALL4 was positive in 6 cases and negative in one case. All tumors were negative with OCT3/4 and Nanog. The sex cord stromal component had immunoreactivity for inhibin in 7/7 analyzable cases. Four of 8 cases were cytogenetically analyzable: 4/8 by low pass genomic sequencing and 2/8 by aCGH. The results of both methods correlated well, revealing mostly multiple chromosomal losses and gains. One case revealed loss of chromosome 21; 1 case had loss of chromosomes 21 and 22 and partial gain of 22; 1 case had loss of chromosomes 22 and Y, partial loss of X, and gain of chromosomes 20, 5, 8, 9, 12, and 13; and the remaining one gain of chromosomes 20, 3, 6, 8, 2x(9), 11, 2x(12), 13, 14, 18, and 19. Three cases were analyzable by NGS; clinically significant activating mutations of either FGFR3 or HRAS were not detected in any case. Follow-up was available for 4 patients (12, 24, 84, and 288 months) and was uneventful in all 4 cases. The identification of extratesticular invasion of both the germ cell and sex cord stromal components, the DMRT1 expression, and the presence of atypical mitoses in germ cells argue for the neoplastic nature of the germ cell component. The molecular genetic study revealing multiple chromosomal losses and gains in a subset of the cases provides the first evidence that molecular abnormalities occur in testicular MGSCT. Multiple chromosomal aneuploidies, namely, recurrent losses of chromosomes 21 and 22 and gains of 8, 9, 12, 13, and 20, indicate that the germ cell component might be related to the morphologically similar spermatocytic tumor, which is characterized by extensive aneuploidies including recurrent gains of chromosomes 9 and 20 and loss of chromosome 7. In summary, our data support that rare examples of true MGSCT of the testis do exist and they represent a distinct tumor entity with admixed adult-type granulosa cell tumor and spermatocytic tumor components.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
While ovarian MGSCT without features of gonadoblastoma is generally accepted as an extraordinarily rare entity, the existence of a true testicular MGSCT is more controversial. Morphologically, they differ in the appearance of both the germ cell and sex cord component. The germ cell component in testicular MGSCT is characterized by abundant cells with clear cytoplasm and rounded variably sized nuclei, intimately admixed with the sex cord stromal component resembling adult-type granulosa cell tumor [1]. The germ cells in ovarian tumors resemble those of dysgerminoma/seminoma having typical “squared off” nuclei and brisk mitotic activity. The sex cord component in ovarian tumors is more variable, as adult-type granulosa cell tumor and Sertoli cell tumor-like components are well described [1,2,3,4,5,6]. Immunohistochemically, the sex cord component in both testicular and ovarian tumors show immunoreactivity with conventional sex cord markers. However, the immunophenotype of the germ cell component is different. In the ovary, the germ cell component has a dysgerminoma/seminoma pattern and is positive with OCT3/4, PLAP, c-kit (CD117), and PAS, while these markers are reportedly negative in testicular MGSCT [1]. The same discrepancy has been found in molecular genetic features. While the amplification of chromosome 12 has been observed in ovarian MGSCT, no such aberration was detected in testicular MGSCT. In the only molecular genetic study of testicular MGSCT to date, the PDGFRA and c-kit mutational status was also investigated, both with a negative result [1].
These reported differences between testicular and ovarian MGSCT, together with the overall bland cytologic appearance of the germ cell component and lack of characteristic immunophenotype and molecular abnormalities in testicular MGSCT, have led some authorities to conclude that true MGSCT does not exist and that all reported examples likely represent sex cord stromal tumors with entrapped non-neoplastic germ cells [7]. However, it is a widely accepted theory that genetic and epigenetic factors may induce clinicopathological differences between similar tumors of both ovarian and testicular origin [8, 9]. Based on our experience with such tumors, we sought to study a series of what we have regarded to be true testicular MGSCTs to determine their full histologic spectrum, immunophenotype, chromosomal aneuploidy status, FGFR3 and HRAS mutational status, clinical outcome, and relationship to spermatocytic tumor.
Materials and methods
Cases cross-matching the keywords “testis,” “mixed germ cell-sex cord stromal tumor,” and “Talerman’s tumor” were retrieved from the files of the authors. The search yielded altogether 8 specimens which were included in the study. The clinical information was extracted from the electronic medical records, and follow-up data were obtained from attending clinicians. The cases were collected over the period 1994–2019. Cases 1, 2, and 8 have been reported previously [1, 10]. Paraffin tissue blocks were available for 6 cases, unstained reserve slides for the remaining 2. When possible, the same tissue block from each case was used for the immunohistochemical and molecular genetic analysis.
Immunohistochemistry
The IHC analysis was performed using a Ventana BenchMark ULTRA (Ventana Medical System, Inc., Tucson, Arizona). The following primary antibodies were used: OCT3/4 (N1NK, RTU, Novocastra, Newcastle, UK), Nanog (polyclonal, 1:100, Abcam, Cambridge, UK), SALL4 (6E3, 1:800, Sigma-Aldrich, St. Luis, Missouri, USA), DMRT1 (polyclonal, 1:200, Sigma-Aldrich), and inhibin (R1, RTU, Ventana Medical System, Inc.). The primary antibodies were visualized employing the enzymes alkaline phosphatase or peroxidase as detecting systems (both purchased from Ventana Medical System, Inc.).
Molecular genetic studies
DNA extraction
Tumor areas of the formalin-fixed paraffin-embedded (FFPE) samples were determined using H&E stained slides and macro-dissected. DNA from FFPE tumor tissue was extracted using QIAsymphony DNA Mini Kit (Qiagen, Hilden, Germany) on an automated extraction system (QIAsymphony SP; Qiagen) according to manufacturer’s supplementary protocol for FFPE samples. Concentration and purity of isolated DNA were measured using NanoDrop ND-1000, and DNA integrity was examined by amplification of control genes in a multiplex polymerase chain reaction (PCR).
Array comparative genomic hybridization (aCGH) and low pass genomic sequencing
SurePlex DNA amplification system (Illumina, San Diego, CA) was used to generate DNA template from tumor samples. Amplification is highly representative, which makes the resulting product suitable for copy number variation (CNV) detection. The library of all samples was prepared using Nextera DNA Sample Prep Kit (Illumina) and sequenced on MiSeq sequencer. CNV analysis was performed using BlueFuse Multi software with the low pass genomic sequencing plugin (Illumina). Following quality control, filters for valid samples were set: minimum 1 million reads per sample, average quality score and average alignment score > 30, and overall noise < 0.3. Thresholds for CNV calling were set based on a group of samples with known CNVs that were validated using array comparative genomic hybridization (aCGH) and fluorescence in situ hybridization (FISH). The percentage of tumor in the DNA sample was considered when calling the lower frequency CNVs. Thresholds for CNVs were set individually for each case; typically the copy number was 1.5 for loss and 2.5 for gain. CNVs spanning less than the whole length of a chromosome arm were not called. FISH, as described previously [11], was used for confirmation of the results. Given the low quality of FFPE material, it was possible to confirm only some of the aberrations in three cases. Loss of chromosome 21 was confirmed in case 3; losses of chromosomes 21 and 22 were confirmed in case 4; and gain of chromosomes 9, 12, and 20 and loss of chromosome 22 were confirmed in case 5. Aberrations on gonosomes were excluded from the results. CNV detection using low pass whole genome sequencing was proven to produce similar results as in fresh frozen tissue [12].
Illumina TruSight Tumor 170 assay
The commercially available TruSight Tumor 170 assay from Illumina was performed according to the manufacturer’s instructions, and the library was sequenced on an Illumina platform as described previously [13].
Results
Clinical presentation
The clinicopathological features are listed in Table 1. All patients were normally developed men with descended testes and karyotype 46XY. The age ranged from 27 to 74 years (mean 49.2, median 41). The patients presented with unilateral testicular mass affecting left testis in 3 cases and the right in 3 cases; in the remaining 2 cases, the side was unknown. The contralateral testes were always unremarkable. All tumors were treated by unilateral orchiectomy. Follow-up duration of 1, 2, 7, and 24 years was available for 4 patients. One patient died from an unrelated cause; the remaining 3 have no signs of recurrence, metastatic spread, or an otherwise aggressive clinical course caused by the tumor.
Pathological features
Grossly, the tumors were well circumscribed and of homogenous soft structure. The tumor size ranged from 1.5 to 5 cm in the largest dimension (mean 3.9, median 4.5).
Histologically, all investigated tumors were composed of two components consisting of the sex cord stromal component and germ cell component. The sex cord stromal component was characterized by bland spindle cells with occasional nuclear grooves resembling adult-type granulosa cell tumor. The germ cell component featured plump rounded cells with abundant clear cell cytoplasm and rounded nuclei with slightly variable size. In all studied cases, the germ cell component showed low but unequivocal mitotic activity, which in 4 cases included atypical mitotic figures (Fig. 1). These two components were irregularly admixed together: in some parts of the tumor, either the sex cord or the germ cell component predominated; in others, there was an even admixture of the two (Fig. 2a–c). In some areas, germ cells predominated over the stromal cells (Fig. 2b). Of note, no areas of a tubular arrangement of the germ cell component suggesting entrapped cells within testicular tubules were apparent. The sex cord stromal component was arranged in diffuse sheets, while the germ cells grew in irregular clusters or as solitary cells. In two cases (cases 3 and 4), there was an invasion into the spermatic cord and adjacent hilar soft tissue (case 3, Fig. 3a) and into the tumor capsule (case 4, Fig. 3c). In both cases, the invasive structures contained both tumor components (Fig. 3b, d).
Both tumor components irregularly admixed together: in some parts of the tumor, either the sex cord (a) or the germ cell (b) component predominated; in others, there was an even admixture of the two (c). The sex cord stromal component was arranged in diffuse sheets, while the germ cells grew in irregular clusters or solitary units. No tubular formations were observed. H&E, × 40
Case 3 (a, b): Invasion into the spermatic cord and hilar soft tissue (A, the area of invasion encircled); H&E, × 2. Higher magnification of the same image enables to discern presence of the both germ cell and sex cord stromal component in an invasive focus (B, arrow points to germ cells); H&E, × 40. Case 4 (c, d): Invasion into the tumor capsule (C, top left); H&E, × 5. Germ cells intermingled with sex cord stromal cells in the invasive area (D); H&E, × 20
Immunohistochemistry
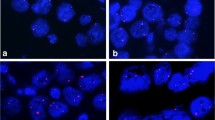
The immunohistochemical results are summarized in Table 2. Focal nuclear expression of DMRT1 was found in the germ cell component in 7/7 analyzed tumors. The sex cord stromal component was diffusely positive with inhibin in 7/7 analyzed cases (Fig. 4). Germ cell component was positive with SALL4 in 6 cases and negative in 1 case; in the remaining cases, the staining was not performed. Seven of 7 tested tumors were negative with OCT3/4, and 5/5 were negative with Nanog.
Chromosomal aneuploidy study
The results are summarized in Table 3. The results of low pass genomic sequencing and aCGH correlated well. Four of 8 cases were analyzable by low pass genomic sequencing. Case 3 revealed loss of chromosome 21 and case 4 losses of chromosomes 21 and 22. In case 5, multiple chromosomal gains were detected, including chromosomes 5, 8, 9, 12, 13, and 20 as well as losses of chromosomes 22 and Xq21.1, Y. Gains of chromosomes 3, 6, 8, 2x(9), 11, 2x(12), 13, 14, 18, 19, and 20 were seen in case 6. Two of 8 cases were analyzable by aCGH. Case 4 revealed gain of 22q11.1–q11.22 and losses of chromosomes 21 and 22q11.23–q13.33 and case 5 chromosomal gains of 8, 9, 12, 13, and 20 and loss of chromosome 22.
Illumina TruSight Tumor 170 assay
Three cases were analyzable, and all were negative.
Discussion
In 2000, Ulbright et al. reported 9 testicular sex cord stromal tumors that suggested the possibility of MGSCTs but differed in that the germ cells were entrapped and non-neoplastic [7]. The authors reported that the cases in their series had differences compared with the testicular MGSCTs published previously [1, 10, 14,15,16] and they questioned the neoplastic nature of the germ cell component in that report as well as the entire concept of testicular MGSCT. To date, this entity has been excluded from the WHO classification of testicular tumors [17]. The arguments against the neoplastic nature of the germ cell component were based on tubular arrangement, peripheral location, bland cytologic appearance, and negativity with germ cell markers in their series. While sex cord stromal tumors with entrapped non-neoplastic germ cells certainly occur, as discussed previously [18], we maintain that rare examples of true testicular MGSCT do exist. Our belief in genuine cases of MGSCT is based on several observations: (1) the germ cells form no tubules but grow in small irregular groups or singly; (2) both tumor components are intimately and irregularly admixed with no predilection of germ cells to the peripheral parts of the tumor; (3) the germ cells occasionally contain tripolar, quadripolar, or bizarre mitoses; and (4) in some tumor areas, the germ cell component dominates the tumor [19]. We have considered the morphology, immunoprofile, and molecular genetic findings of the germ cell component similar to those of spermatocytic tumor [19].
The herein presented series provides further evidence for the neoplastic nature of the germ cell component. The germ cells in 4/8 cases featured occasional atypical mitotic figures, which further supports our earlier observation [1, 19]. More importantly, in case 3 there was an invasion into the spermatic cord and hilar soft tissue and in case 4 into the tumor capsule. In each case, the invasive structures contained both the germ cell and sex cord stromal components, which we consider as a strong supportive evidence for the neoplastic nature of the germ cell component.
To date, the nature of the germ cell component in MGSCT of the testis has not been sufficiently elucidated. Nevertheless, one of the first detailed studies of MGSCT pointed to its resemblance to the spermatocytic tumor, analogically as the ovarian MGSCT corresponds to dysgerminoma [1]. This hypothesis was based on morphology (variably sized rounded nuclei), immunohistochemistry (negativity with dysgerminoma/seminoma markers), and molecular features (absence of chromosomal 12p abnormalities) of testicular MGSCTs [1]. However, several differences have emerged. As for morphology, spermatocytic tumor lacks a prominent sex cord stromal component characterizing MGSCT and exhibits greater variability of nuclear size than MGSCT [20]. Ultrastructurally, spermatocytic tumor contains more mature transformed germ cells than testicular MGSCT [7, 21]. Recently, Roth et al. immunohistochemically compared the protein expression of the transcription factors DMRT1 and TCLF5 in the germ cell component of testicular MGSCT to expression in spermatocytic tumor [20]. DMRT1 is reportedly positive in spermatogonia and negative in all more differentiated germ cells, whereas TCLF5 is immunoreactive in more mature germ cells (such as primary and secondary spermatocytes and spermatids) [22]. In their study, they found a nuclear positivity of DMRT1 and absent TCLF5 staining in both MGSCT and spermatocytic tumor [20]. The first study performing the whole-genome sequencing of spermatocytic tumors showed multiple aneuploidies of whole chromosomes [23], which was in concordance with previous studies publishing recurrent gains of chromosomes 9 and 20 as well as loss of chromosome 7 and, to a lesser extent, of chromosomes 13, 15, and 22 [24, 25]. Besides, activating mutations of FGFR3 and HRAS genes appear to occur in approximately 20% of spermatocytic tumors [23, 26].
The molecular genetic analysis performed in the current study focused on detecting abnormalities occurring in spermatocytic tumor: Chromosomal aneuploidy study and NGS study detecting among others FGFR3 and HRAS gene mutations were employed. The chromosomal study was independently performed by both aCGH and low pass genomic sequencing. Low pass genomic sequencing is a preimplantation screening method originally designed for selecting euploid embryos before in vitro fertilization. This method enables the assessment of the numerical and structural chromosomal aberrations by exploiting the NGS technology. It sequences data from thousands of loci across each chromosome enabling evaluation of multiple genomic loci and multiple samples on one chip [27, 28]. Theoretically, only a single viable, well-preserved cell should suffice for a successful analysis. We therefore hypothesized that the main advantage of this method for the purposes of our study might be its lower material input requirements as compared with aCGH, a feature very useful considering the mostly archival nature of our cases. In the current study, the results obtained by low pass genomic sequencing correlated well with aCGH. Furthermore, low pass genomic sequencing appeared to be more utilizable as 4/8 cases were successfully analyzed as compared with 2/8 cases analyzable by aCGH. Mostly multiple chromosomal losses and gains were detected, among which losses of chromosomes 21 and 22 and gains of chromosomes 8, 9, 12, 13, and 20 were recorded recurrently. None of the analyzable case revealed any molecular abnormality detectable by NGS (including FGFR3 and HRAS activating mutations). However, as FGFR3 and HRAS mutations occur only in subset of spermatocytic tumors [26], they rather represent random mutational events in spermatogonia than a fundamental pathogenetic process. Thus, their absence does not exclude diagnosis of spermatocytic tumor.
Despite the lack of a perfect molecular overlap, our results further support a potential relationship between the germ cell component of MGSCT and spermatocytic tumor, as suggested previously [1, 20]. The germ cells in both MGSCT and spermatocytic tumor are likely of premeiotic origin, as suggested by Roth et al. [20]. However, the abovementioned slight histological, ultrastructural, and molecular differences indicate that the cells in spermatocytic tumor are probably more differentiated toward primary spermatocytes, in contrast to immature spermatogonia in MGSCT.
It is worth mentioning that we repeatedly attempted microdissection which would enable the separate analysis of the germ cell and sex cord stromal component. We failed to accurately isolate germ cells from the material. As the germ cells in this particular tumor occur either as single cells or in a form of small irregular clusters, there were always present contaminating fragments of the adjacent sex cord stromal component. Ultimately, this method proved unfeasible, and both components had to be analyzed together. Thus, we cannot confidently determine which of the two, or whether both components, is/are aneuploid. However, since other testicular germ cell tumors usually feature chromosomal numerical aberrations [17, 29] whereas sex cord stromal tumors more frequently show various gene mutations [17, 30, 31], we would argue that the chromosomal aneuploidies of the current 4 cases more likely stemmed from the germ cell component.
The main differential diagnosis of MGSCT is gonadoblastoma, a tumor similarly containing both germ cell and sex cord stromal elements [32]. Gonadoblastoma typically occurs in patients with 46XY disorders with dysgenetic gonads, while MGSCT occurs in karyotypically normal men with a normal gonadal development. Furthermore, MGSCT lacks abundant mulberry-like calcifications and Leydig-like or lutein-like cells typical of gonadoblastoma [33]. Germ cell component of gonadoblastoma is similar to seminoma both morphologically and immunohistochemically and, when invasive, also genetically.
In summary, identification of extratesticular invasion of both components of MGSCT and the presence of atypical mitoses in the germ cells serve as a strong argument for the neoplastic nature of the germ cell component. In addition, the comprehensive chromosomal aneuploidy study revealed losses of chromosomes 21 and 22 and gains of 8, 9, 12, 13, and 20 in 4 cases. Although the studied sample was relatively small, it provided the first and unequivocal evidence that chromosomal abnormalities do occur in testicular MGSCT and further suggest relatedness to spermatocytic tumor. Therefore, we argue that although rare, true MGSCT of the testis do exist and should be accepted as a distinct entity.
References
Michal M, Vanecek T, Sima R, Mukensnabl P, Hes O, Kazakov DV, Matoska J, Zuntova A, Dvorak V, Talerman A (2006) Mixed germ cell sex cord-stromal tumors of the testis and ovary. Morphological, immunohistochemical, and molecular genetic study of seven cases. Virchows Archiv 448:612–622
Arroyo JG, Harris W, Laden SA (1998) Recurrent mixed germ cell-sex cord-stromal tumor of the ovary in an adult. Int J Gynecol Pathol 17:281–283
Talerman A, Roth LM (2007) Recent advances in the pathology and classification of gonadal neoplasms composed of germ cells and sex cord derivatives. Int J Gynecol Pathol 26:313–321
Talerman A (1972) A distinctive gonadal neoplasm related to gonadoblastoma. Cancer. 30:1219–1224
Zuntova A, Motlik K, Horejsi J et al (1992) Mixed germ cell-sex cord stromal tumor with heterologous structures. Int J Gynecol Pathol 11:227–233
Talerman A, van der Harten JJ (1977) Mixed germ cell-sex cord stroma tumor of the ovary associated with isosexual precocious puberty in a normal girl. Cancer. 40:889–894
Ulbright TM, Srigley JR, Reuter VE, Wojno K, Roth LM, Young RH (2000) Sex cord-stromal tumors of the testis with entrapped germ cells: a lesion mimicking unclassified mixed germ cell sex cord-stromal tumors. Am J Surg Pathol 24:535–542
Conlon N, Schultheis AM, Piscuoglio S, Silva A, Guerra E, Tornos C, Reuter VE, Soslow RA, Young RH, Oliva E, Weigelt B (2015) A survey of DICER1 hotspot mutations in ovarian and testicular sex cord-stromal tumors. Mod Pathol 28:1603–1612
Roth LM, Lyu B, Cheng L (2017) Perspectives on testicular sex cord-stromal tumors and those composed of both germ cells and sex cord-stromal derivatives with a comparison to corresponding ovarian neoplasms. Hum Pathol 65:1–14
Matoska J, Talerman A (1989) Mixed germ cell-sex cord stroma tumor of the testis. A report with ultrastructural findings. Cancer. 64:2146–2153
Sperga M, Martinek P, Vanecek T, Grossmann P, Bauleth K, Perez-Montiel D, Alvarado-Cabrero I, Nevidovska K, Lietuvietis V, Hora M, Michal M, Petersson F, Kuroda N, Suster S, Branzovsky J, Hes O (2013) Chromophobe renal cell carcinoma--chromosomal aberration variability and its relation to Paner grading system: an array CGH and FISH analysis of 37 cases. Virchows Archiv 463:563–573
Munchel S, Hoang Y, Zhao Y, Cottrell J, Klotzle B, Godwin AK, Koestler D, Beyerlein P, Fan JB, Bibikova M, Chien J (2015) Targeted or whole genome sequencing of formalin fixed tissue samples: potential applications in cancer genomics. Oncotarget. 6:25943–25961
Donati M, Kastnerova L, Martinek P, Grossmann P, Sticová E, Hadravský L, Torday T, Kyclova J, Michal M, Kazakov DV (2020) Spitz tumors with ROS1 fusions: a clinicopathological study of 6 cases, including FISH for chromosomal copy number alterations and mutation analysis using next-generation sequencing. Am J Dermatopathol 42:92–102
Bolen JW (1981) Mixed germ cell-sex cord stromal tumor. A gonadal tumor distinct from gonadoblastoma. Am J Clin Pathol 75:565–573
Talerman A (1980) The pathology of gonadal neoplasms composed of germ cells and sex cord stroma derivatives. Pathol Res Pract 170:24–38
Rames RA, Richardson M, Swiger F, Kaczmarek A (1995) Mixed germ cell-sex cord stromal tumor of the testis: the incidental finding of a rare testicular neoplasm. J Urol 154:1479
Moch H, Cubilla AL, Humphrey PA, Reuter VE, Ulbright TM (2016) The 2016 WHO classification of tumours of the urinary system and male genital organs-part a: renal, penile, and testicular tumours. Eur Urol 70:93–105
Ulbright TM, Young RH (2007) Reply: mixed germ cell sex cord-stromal tumors of the testis and ovary. Virchows Archiv 450:131–132
Michal M, Hes O, Mukensnabl P, Kazakov DV (2007) Mixed germ cell sex cord-stromal tumours of the testis. Virchows Archiv 451:1095–1096
Roth LM, Michal M, Michal M Jr, Cheng L (2018) Protein expression of the transcription factors DMRT1, TCLF5, and OCT4 in selected germ cell neoplasms of the testis. Hum Pathol 82:68–75
Rosai J, Khodadoust K, Silber I (1969) Spermatocytic seminoma. II Ultrastructural study. Cancer 24:103–116
Jorgensen A, Nielsen JE, Blomberg Jensen M, Graem N, Rajpert-de Meyts E (2012) Analysis of meiosis regulators in human gonads: a sexually dimorphic spatio-temporal expression pattern suggests involvement of DMRT1 in meiotic entry. Mol Hum Reprod 18:523–534
Giannoulatou E, Maher GJ, Ding Z, Gillis AJM, Dorssers LCJ, Hoischen A, Rajpert-de Meyts E, WGS500 Consortium, McVean G, Wilkie AOM, Looijenga LHJ, Goriely A (2017) Whole-genome sequencing of spermatocytic tumors provides insights into the mutational processes operating in the male germline. PLoS One 12:e0178169
Looijenga LH, Hersmus R, Gillis AJ et al (2006) Genomic and expression profiling of human spermatocytic seminomas: primary spermatocyte as tumorigenic precursor and DMRT1 as candidate chromosome 9 gene. Cancer Res 66:290–302
Verdorfer I, Rogatsch H, Tzankov A, Steiner H, Mikuz G (2004) Molecular cytogenetic analysis of human spermatocytic seminomas. J Pathol 204:277–281
Goriely A, Hansen RM, Taylor IB et al (2009) Activating mutations in FGFR3 and HRAS reveal a shared genetic origin for congenital disorders and testicular tumors. Nat Genet 41:1247–1252
Knapp M, Stiller M, Meyer M (2012) Generating barcoded libraries for multiplex high-throughput sequencing. Methods Mol Biol (Clifton) 840:155–170
Zheng H, Jin H, Liu L, Liu J, Wang WH (2015) Application of next-generation sequencing for 24-chromosome aneuploidy screening of human preimplantation embryos. Mol Cytogenet 8:38
Sheikine Y, Genega E, Melamed J, Lee P, Reuter VE, Ye H (2012) Molecular genetics of testicular germ cell tumors. Am J Cancer Res 2:153–167
Perrone F, Bertolotti A, Montemurro G, Paolini B, Pierotti MA, Colecchia M (2014) Frequent mutation and nuclear localization of beta-catenin in sertoli cell tumors of the testis. Am J Surg Pathol 38:66–71
Colecchia M (2014) Observations on the paper "sclerosing Sertoli cell tumor of the testis: a clinicopathologic study of 20 cases" by Kao et al. Am J Surg Pathol 38:1160
Roth LM, Cheng L (2018) Classical gonadoblastoma: its relationship to the 'dissecting' variant and undifferentiated gonadal tissue. Histopathology. 72:545–555
Scully RE (1970) Gonadoblastoma. A review of 74 cases. Cancer. 25:1340–1356
Funding
Supported by the National Sustainability Program I (NPU I) Nr. LO1503 provided by the Ministry of Education Youth and Sports of the Czech Republic and by Charles University Fund SVV 2019-260391.
Author information
Authors and Affiliations
Contributions
Kvetoslava Michalova:, case selection, results evaluation, manuscript, and figures. Jesse K. McKenney: case contribution, and discussion. Glen Kristiansen: case contribution. Petr Steiner: genetic analyses. Petr Grossmann: genetic analyses. Martina Putzova: genetic analyses. Petr Martinek: genetic analyses. Magdalena Chottova-Dvorakova: microdissection analysis. Michael Michal: results’ evaluation and discussion. Ondrej Hes: discussion. Michal Michal: study design, discussion, and figures.
Corresponding author
Ethics declarations
This study has been approved by the ethics committee of both Faculty of Medicine and Faculty Hospital in Pilsen, Czech Republic. Informed consent was not required for the study.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Quality in Pathology
Rights and permissions
About this article
Cite this article
Michalova, K., McKenney, J.K., Kristiansen, G. et al. Novel insights into the mixed germ cell-sex cord stromal tumor of the testis: detection of chromosomal aneuploidy and further morphological evidence supporting the neoplastic nature of the germ cell component. Virchows Arch 477, 615–623 (2020). https://doi.org/10.1007/s00428-020-02843-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-020-02843-3