Abstract
A histological grading system of chromophobe renal cell carcinoma (chRCC) is highly desirable to identify approximately 5–10% of tumors at risk for progression. Validation studies failed to demonstrate a correlation between the four-tiered WHO/ISUP grade and outcome. Previous proposals with three-tiered chromophobe grading systems could not be validated. In this study, the presence of sarcomatoid differentiation, necrosis, and mitosis was analyzed in a Swiss cohort (n = 42), an Italian cohort (n = 103), a German cohort (n = 54), a Japanese cohort (n = 119), and The Cancer Genome Atlas cohort (n = 64). All 3 histological parameters were significantly associated with shorter time to tumor progression and overall survival in univariate analysis. Interobserver variability for identification of these parameters was measured by Krippendorff’s alpha coefficient and showed high concordance for the identification of sarcomatoid differentiation and tumor necrosis, but only low to medium concordance for the identification of mitosis. Therefore, we tested a two-tiered tumor grading system (low versus high grade) based only on the presence of sarcomatoid differentiation and/or necrosis finding in the combined cohorts (n = 382). pT stage, patient’s age (> 65 vs ≤ 65), lymph node and/or distant metastasis, and the two-tiered grading system (low versus high grade) were significantly associated with overall survival and were independent prognostic parameters in multivariate analysis (Cox proportional hazard). This multi-institutional evaluation of prognostic parameters suggests tumor necrosis and sarcomatoid differentiation as reproducible components of a two-tiered chromophobe tumor grading system.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chromophobe renal cell carcinoma (chRCC) is a histological subtype of renal cell carcinoma (RCC) with a unique molecular background [1]. Large studies published on chRCC have shown that death occurred in only 6% of patients [2].
Tumor grade is one of the most important prognostic parameters of renal cancer. The nuclear grading system proposed by Fuhrman et al. [3] is now replaced by the International Society of Urological Pathology (ISUP) grading system [4], which was subsequently adopted by the World Health Organization (WHO) [5]. Whereas the WHO/ISUP system was validated for clear cell RCC and papillary RCC [4,5,6,7,8,9], it could not be validated for chRCC. Therefore, it was recommended that chRCC should not be graded [5, 10].
It has been described in earlier studies that chRCC has an innate constitutive atypia including prominent nucleoli, nuclear irregularities, and bi-nucleation [11]. Due to the frequent presence of nuclear atypia, chRCC displays a higher nuclear grade compared with clear cell RCC [12]. There have been several attempts to develop a grading system for chRCC [13], discounting this innate constitutive atypia of chRCC. In contrast to nuclear or nucleolar features used by the four-tiered Fuhrman or WHO/ISUP systems [5], grading proposals for chRCC included geographic nuclear crowding and presence of anaplasia. Paner et al. suggested a three-tiered chromophobe tumor grading (CTG) scheme and supplemented nuclear grading with additional variables including geographic nuclear crowding and objective nuclear size. With this approach, the majority of chRCCs are of a lower grade [13]. Lohse et al. applied a four-tiered standardized grading for chRCC and demonstrated a significant overlap in grades 3, 2, and 1 chRCC [14].
Given the situation that a small but significant group of chRCC is at greater risk of disease progression, it is highly desirable that chRCC is graded. Given poor reproducibility of grading schemes based on nuclear grade, nuclear crowding, and anaplasia, we performed a multi-institutional re-evaluation of the prognostic parameters, tumor necrosis, sarcomatoid differentiation, and mitosis for the following reasons: (i) Recently, incorporation of tumor necrosis into RCC grading was proposed [15]. (ii) Mitosis is a component of grading systems in different tumor types [15, 16]. (iii) In contrast to geographic nuclear crowding, nuclear size, and the presence of frank anaplasia, sarcomatoid differentiation is an accepted parameter of poor outcome in many grading proposals for chRCC [15].
Materials and methods
Multi-institutional collection of chromophobe renal cell carcinomas
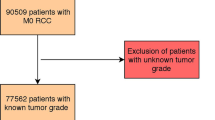
To set up a collection of chRCC from different geographic areas, we collected tumors from Switzerland, Germany, Italy, and Japan. The Swiss and Japanese cohorts have been recently described [17]. There were 2 chRCCs diagnosed with neuroendocrine differentiation [18,19,20] in Japan. As chRCC with neuroendocrine differentiation shows a specific histology, these 2 tumors were excluded from further analysis.
Italian chRCCs were retrieved from the archives of the Department of Pathology of the University of Verona and Pederzoli Hospital of Peschiera del Garda, Verona (diagnosed from 1999 to 2018). All chRCCs of the Italian cohort were reviewed by GM.
The German chRCCs were retrieved from the archives of the Department of Pathology, University of Erlangen-Nürnberg (diagnosed from 1994 to 2017) and the Department of Pathology, University of Munich. All chRCCs in the German cohort were reviewed by AH and RO.
The study protocol was approved by Institutional Review Boards (IRBs) at all participating institutions. The study did not include consultation cases.
Pathological Parameters
Tumor classification was done according to the WHO classification [5]. Tumors were staged according to the UICC TNM staging system [21]. At least 1 large tumor section per tumor diameter was available for evaluation. All tumor slides were analyzed for the presence or absence of the following parameters: (1) sarcomatoid differentiation, (2) histological coagulative tumor necrosis, and (3) presence of mitosis. No tissue microarray was used for this study. Sarcomatoid differentiation was defined as groups of clearly identifiable spindle shaped cells in at least one HPF as previously reported [22, 23] (Fig. 1a, b). To determine mitosis, 20 high-power fields (HPFs) at × 200 magnification (20× objective lens and 10× eyepiece with field number 20, 23, or 25) were screened. Subsequently, the morphology of mitosis was confirmed by high power field observation. A three-tiered chromophobe tumor grading (CTG) was performed according to a proposal by Paner et al. [13].
a ChRCC composed of epithelial, polygonal pale cells and eosinophilic cells (right) with sarcomatoid differentiation (left), composed of spindle cells. Vimentin was positive only in the sarcomatoid differentiation area (left). Epithelial cells were negative for vimentin (right). b, c chRCC with sarcomatoid differentiation in TCGA cohort (TCGA-KO-8404). Mitoses was easily found in sarcomatoid differentiation area (c, left) and the epithelial area with anaplasia (c, right) in this case. d Microscopic tumor necrosis comprised of eosinophilic, flocculent cell ghosts with granular nuclear and cytoplasmic debris in the central area. There is loss of underlying architecture (TCGA-KN-8428). Bar = 100µm
Interobserver variability
There is a different degree of interobserver variability for the identification of mitosis, necrosis, and sarcomatoid differentiation. This influences the usefulness of these morphological parameters as components of a grading system. Therefore, we organized a meeting in Zurich (Switzerland) for anonymous and independent scoring of 71 consecutive chRCCs (Swiss and German cohort) by 4 specialized uropathologists (HM, RO, GM, and AH). All cases were seen by all four pathologists and interobserver variability was calculated according to Krippendorff's alpha (KA) test (see below) [24]. In addition, 103 Italian chRCCs were evaluated by three pathologists (GM, AC, and DS).
TCGA cohort
A cohort of 64 chRCCs was identified in the Cancer Genome Atlas (TCGA) [1]. The corresponding clinical information of TCGA-KICH was obtained from TCGA Data Portal (https://portal.gdc.cancer.gov/). Two patients with missing or too short a follow-up (i.e., less than 30 days) were excluded. Digital whole slide images of TCGA-KICH cases were reviewed by RO using the Cancer Digital Slide Archive (http://cancer.digitalslidearchive.net/). TCGA-KO-8404 (TCGA Case ID) had an apparent sarcomatoid differentiation area, whereas TCGA-KM-8438 had no sarcomatoid differentiation area in registered digital images. According to the pathology report of TCGA-KM-8438 obtained from the archive, the existence of high-grade sarcomatoid differentiation had been mentioned. Therefore, we included this case as chRCC with sarcomatoid differentiation in this study. To examine mitosis, at least 100 of moderate power magnification fields of the digital slides were observed and then confirmed at high power magnification.
Statistics
All statistical analysis was done using R version 3.4.1 (R Foundation for Statistical Computing, Vienna, Austria) and EZR, version 1.37 (Saitama Medical Center, Jichi Medical University, Saitama, Japan) [25]. Statistical evaluation of the associations between the morphological grading parameters and pathologic stage was based on the Fisher’s exact test as applied to categorical variables with two or more levels. Medical records were reviewed and cross-referenced with the tumor registry for extended follow-up. Patients with missing or short (less than 30 days) follow-up were excluded from this study. For overall survival (OS) analysis, outcome was defined as the time from surgery to death. Time to progression (TTP) data was available in the Japanese and Italian cohorts from medical records. TTP was defined as the time from surgery to the first occurrence of metastasis, local recurrence, or death due to primary cancer; deaths from unrelated causes were censored. Overall survival data, mainly based on tumor registry data were available for all cohorts. Univariate associations between morphological parameters and times to event were evaluated through log rank tests and a multivariable analysis was undertaken through cox regression with Firth’s penalized likelihood [26]. Prognostic variables previously found to be univariate significant predictors of adverse outcomes were included. All statistical tests were two-sided; a p value < 0.05 was regarded as statistically significant.
Krippendorff's alpha (KA) [24] for nominal data with a 95% confidence interval (CI) based on 10,000 bootstrap resamples [27] was calculated to assess the overall inter-pathologist variability for each histopathological parameter using the “irr” and “boot” package in R.
Results
Correlation of sarcomatoid differentiation, tumor necrosis, and mitosis with patient survival
Sarcomatoid differentiation was seen in only 0 to 5% of the different cohorts, whereas microscopic tumor necrosis was present in 10 to 20% (Table 1). Mitosis was identified mainly in areas with anaplasia, nuclear crowding or sarcomatoid differentiation (Fig. 1c). In the Swiss cohort, mitoses were identified in only 10 cases. In these 10 cases, the mean + SD number of mitoses in 100 HPFs was 3.1 ± 1.4 except for one case with an extensive sarcomatoid differentiation area with more than 10 of many mitoses per 100 HPF. Most mitoses were atypical [28]. In the Japanese cohort, mitoses were found in 19 of 119 chRCC. In these tumors, the mean + SD number of mitoses in 100 HPFs was 2.3 ± 2.3, except for one case with broad sarcomatoid differentiation and more than 1000 mitoses per 100 HPF. Given the low number of mitoses in 100 HPF, we decided to categorize this parameter in the presence/absence of mitosis in 20 HPF (details see above) for further statistical analysis. With this approach, mitosis was found in 16 to 33% of chRCCs (Table 1).
All 3 histological parameters, sarcomatoid differentiation, necrosis, and mitosis, were significantly associated with TTP in the Japanese and Italian cohort (p < 0.001, each; Supplementary Figure 1 and 2). In the combined cohorts, the presence of sarcomatoid differentiation (p < 0.05), necrosis (p < 0.01), and mitosis (p < 0.01) was significantly associated with short OS in univariate analysis.
Interobserver variability
In 72 consecutive chRCC (from Swiss and German cohort) independently analyzed by 4 uropathologists, Krippendorff’s alpha (KA) was highest for sarcomatoid differentiation [0.660, 95% confidence interval (CI) − 0.0131–1.000] (Table 2). KA was moderate for the presence of necrosis (0.466, 95% CI 0.250–0.646). KA was also low for the presence of mitosis (0.371, 95% CI 0.176–0.537), indicating poor concordance. Similarly, in 103 Italian chRCCs, independently analyzed by 3 uropathologists, KA was high for sarcomatoid differentiation (0.938, 95% CI 0.787–1.000) and presence of necrosis (0.918, 95% CI 0.828–0.982). KA was moderate for the presence of mitosis (0.656, 95% CI 0.484–0.796) (Table 3).
Proposal of a two-tiered chromophobe renal cancer grading
We tested a two-tiered tumor grading system (low versus high grade) based on the presence of sarcomatoid differentiation and/or tumor necrosis in the combined cohorts. Mitosis was not included in this grading, because there was only low to medium concordance for identification of mitosis (0.37–0.66; Krippendorff’s alpha coefficient). Using this grading system, there was a statistically significant difference in OS between low- and high-grade chRCC (p < 0.01, Fig. 2a). We have also performed Paner’s chromophobe tumor grading (CTG) [13], but this CTG resulted in a lower statistical significance (p < 0.05) and showed a poor separation of grade 1 and grade 2 tumors (Fig. 2b). pT stage or T stage (T3-4 vs T1-2; p < 0.01), age (> 65 vs ≤ 65), lymph node, and/or distant metastasis (pN/N1-2 and/or cM1 vs pN/N0 and cM0) and the two-tiered grading system (low versus high grade; p < 0.01) were associated with overall survival and were independent prognostic parameters (p < 0.01 for each variables) (Fig. 2a, c, d, e and Table 3). In addition, using this grading system, there was a statistical significant different TTP between low- and high-grade chRCC in the Japanese and the Italian cohort (p < 0.001, each; Fig. 3a, b).
Prognostic impact of the two-tiered chRCC grading system (low versus high grade) based on the presence of tumor necrosis and sarcomatoid differentiation. Overall survival in all 382 chRCC patients combined from the Swiss, TCGA-KICH, Japanese, Italian, and German cohorts according to proposed two-tiered chRCC grading system (a), chromophobe tumor grade (CTG) (b), pT or T stage (c), age (y.o: years old) (d), and pN/N and/or M category (e)
Discussion
This multi-institutional re-evaluation of prognostic parameters suggests that a novel two-tiered chromophobe renal cancer grading based on the presence of sarcomatoid differentiation and/or necrosis is able to identify chRCC with increased risk of tumor progression after surgery.
Survival analyses in chRCC require large cohorts because there are only few patients with tumor-specific “events” or dead of disease (DOD). Due to the good prognosis of chRCC, many patients have dead of other causes (DOOC). For example, there were only 5.6% DOD and 9.3% DOOC in the German patient cohort. In the Japanese cohort, there were only 3.4% DOD and 4.2% DOOC. Therefore, identification of biomarkers to predict time to progression after tumorectomy is the most important parameter for chRCC from a clinical viewpoint. Chromophobe renal cell carcinomas consist of mixtures of cells with pale cytoplasm and cells with more-or-less eosinophilic cytoplasm. The “eosinophilic variant” is one extreme of a continuum from all cells with pale cytoplasm to all cells which resemble the cells of renal oncocytoma. Recently, we have shown that patients with the “eosinophilic variant” of chRCC have the same prognosis as classic chRCC. Therefore, this histological feature cannot be used as a grading component [17]. However, Trpkov et al. proposed low-grade oncocytic tumors (LOT) with CD117 negativity and CK7 positivity as an emerging renal tumor entity with indolent clinical behavior [29]. Further studies are warranted to proof that LOT potentially represents a distinct type of tumor or if they should be regarded as variant of eosinophilic chRCC.
Importantly, we have observed a significant association of all 3 histological biomarker (sarcomatoid differentiation, microscopic tumor necrosis, and presence of mitoses) with shorter time to tumor progression in a Japanese patient cohort. This finding was validated in the Italian cohort.
Different histological parameters have been previously tested as components of a potential chRCC grading system. The presence of prominent nucleoli is the basis of the novel WHO/ISUP grading system [5], but prominent nucleoli are not frequent in chRCC. In contrast, nuclear pleomorphism is inherently present in chRCC. Paner et al. introduced nuclear crowding and tumor cell anaplasia for a three-tiered chromophobe tumor grading (CTG) system [13]. In our analysis, the three-tiered Paner grading showed poor separation of grade 1 and grade 2 tumors. In addition, in our and others’ experience, inter- and intra-observer variability of nuclear crowding and nuclear pleomorphism is high [30]. We have demonstrated that there is a high to very high concordance in the identification of sarcomatoid differentiation, although sarcomatoid differentiation was seen in only 3.1% of chRCC. This prevalence of sarcomatoid differentiation was lower than data from older studies with cases diagnosed before 1990 (5–8.8%) [2, 31, 32], but was similar to recent studies reporting a prevalence of sarcomatoid differentiation in 1.8–2.0% of all chRCCs [33, 34, 35]. This discrepancy could be due to a lower T stage at detection because of recent advances in medical imaging technology. Numerous studies have confirmed that the presence of sarcomatoid morphology indicates poor prognosis for most renal cancer subtypes [2, 4, 6, 13, 15, 23, 30,31,32,33,34,35,36]. The Paner system [13] for chRCC assigned a grade 3 to tumors with frank anaplasia and/or sarcomatoid transformation, but most adverse events were observed in grade 3 tumors with sarcomatoid differentiation. Due to the overriding effect of tumors with sarcomatoid differentiation, Paner et al. decided to exclude this tumor subset from most analyses. Practically, this approach reduced the three-tiered grading system to a two-tiered system. For the predominant non-sarcomatoid cohort, Paner et al. observed a statistically significant association between grade and pT stage as well as an independent association of grade with adverse outcome [13].
In our study, overall survival data from tumor registries and patient records were available for all tumors in all patient cohorts, allowing a multivariate statistical analysis. Whereas sarcomatoid differentiation is rare, our data demonstrate that the presence of tumor necrosis is an excellent parameter for a novel grading system of chRCC, because of independent prognostic value in multivariate analysis. This confirms data from Cheville et al., who also reported necrosis as a prognostic parameter for chRCC in a univariate analysis [31]. This form of necrosis must be differentiated from thromboembolic coagulative necrosis, which is usually macroscopic and extensive. Tumor-related necrosis is characterized by aggregates of nuclear debris. In several studies, the prognostic significance of tumor-related necrosis has been investigated as a feature of tumor grading [2, 4, 6, 15]. It is well accepted that the presence of tumor-related necrosis is associated with an unfavorable prognosis in clear cell RCC [4, 6, 32].
Interestingly, detection of mitotic figures had a significant prognostic impact but there was only low to moderate concordance in identification of mitosis in our inter-observer variability study. Normally, the presence or absence of mitosis is a clearly defined feature and mitotic count is a reliable and reproducible component of grading for breast cancer [37], gastrointestinal stromal tumor [38] and pancreatic neuroendocrine tumor [39]. In renal cancer, mitotic rate was already included in early grading systems [15, 16]. We have seen mitoses in 20 to 30% of chRCC, but the mitotic count was very low with a mean number of 2.3 (Swiss tumors) to 3.1 (Japanese tumors) per 100 HPF. Therefore, we categorized this parameter in presence versus absence of any mitosis. Importantly, we noted “karyorrhexis” as a frequent phenomenon in chRCC, which is difficult to separate from “true” mitosis. The low mitotic count together with misinterpretation of “karyorrhexis” can explain the high inter-observer variability with only low to medium concordance among three to four specialized pathologists. In routine pathology, mitosis is difficult to implement because of poor reproducibility.
There are several advantages of a two-tiered grading system over previous proposals of chromophobe tumor grading and the WHO/ISUP grading. (1) WHO/ISUP grading uses four tiers, of which grade 1 is rarely used. Furthermore, WHO/ISUP grade 4 is defined by sarcomatoid or rhabdoid differentiation, which is also rare in chRCC. (2) The presence of necrosis can reliably identified in routine pathology. In contrast, pleomorphic nuclei, anaplasia, and geographic nuclear crowding are difficult to standardize and grading systems based on such parameters are poorly reproducible. (3) Our novel grading system shows a high accuracy to predict overall survival, even in tumor cohorts with a very low proportion of sarcomatoid chRCC.
In conclusion, we propose a reproducible two-tiered grading model as an independent predictor of aggressive chRCC. Our grading system will help to stratify patients with chRCC, because low-grade tumors have an extremely low risk of tumor progression after surgery.
Data availability
The data set generated and/or analyzed during the current study are not publicly available due to medical confidentiality but are available from the first author or the corresponding author on reasonable request summarized form pending the approval of the institutional review board.
Change history
10 March 2020
The legends of Figs. 1 and 3 in the published original version of the above article are incorrect.
References
Davis CF, Ricketts CJ, Wang M et al (2014) The somatic genomic landscape of chromophobe renal cell carcinoma. Cancer Cell 26:319–330
Amin MB, Paner GP, Alvarado-Cabrero I, Young AN, Stricker HJ, Lyles RH, Moch H (2008) Chromophobe renal cell carcinoma: histomorphologic characteristics and evaluation of conventional pathologic prognostic parameters in 145 cases. Am J Surg Pathol 32:1822–1834
Fuhrman SA, Lasky LC, Limas C (1982) Prognostic significance of morphologic parameters in renal cell carcinoma. Am J Surg Pathol 6:655–663
Delahunt B, Cheville JC, Martignoni G, Humphrey PA, Magi-Galluzzi C, McKenney J, Egevad L, Algaba F, Moch H, Grignon DJ, Montironi R, Srigley JR, Members of the ISUP Renal Tumor Panel (2013) The International Society of Urological Pathology (ISUP) grading system for renal cell carcinoma and other prognostic parameters. Am J Surg Pathol 37:1490–1504
Paner G, Amin MB, Moch H, Störkel S. Chromophobe renal cell carcinoma. In: Moch H, Humphrey PA, Ulbright TM, Reuter VE, editors (2016) WHO Classification of Tumours of the Urinary System and Male Genital Organs 4th edition. International Agency for Research on Cancer: Lyon, pp 27-28
Delahunt B, Srigley JR, Judge MJ, Amin MB, Billis A, Camparo P, Evans AJ, Fleming S, Griffiths DF, Lopez-Beltran A, Martignoni G, Moch H, Nacey JN, Zhou M (2019) Data set for the reporting of carcinoma of renal tubular origin: recommendations from the International Collaboration on Cancer Reporting (ICCR). Histopathology 74:377–390
Sika-Paotonu D, Bethwaite PB, McCredie MR, William Jordan T, Delahunt B (2006) Nucleolar grade but not Fuhrman grade is applicable to papillary renal cell carcinoma. Am J Surg Pathol 30:1091–1096
Delahunt B, Sika-Paotonu D, Bethwaite PB et al (2011) Grading of clear cell renal cell carcinoma should be based on nucleolar prominence. Am J Surg Pathol 135:134–1139
Dagher J, Delahunt B, Rioux-Leclercq N, Egevad L, Srigley JR, Coughlin G, Dunglinson N, Gianduzzo T, Kua B, Malone G, Martin B, Preston J, Pokorny M, Wood S, Yaxley J, Samaratunga H (2017) Clear cell renal cell carcinoma: validation of World Health Organization/International Society of Urological Pathology grading. Histopathology 71:918–925
Delahunt B, Sika-Paotonu D, Bethwaite PB et al (2007) Fuhrman grading is not appropriate for chromophobe renal cell carcinoma. Am J Surg Pathol 31:957–960
Tickoo SK, Amin MB (1998) Discriminant nuclear features of renal oncocytoma and chromophobe renal cell carcinoma. Analysis of their potential utility in the differential diagnosis. Am J Clin Pathol 110:782–787
Amin MB, Amin MB, Tamboli P, Javidan J, Stricker H, de-Peralta Venturina M, Deshpande A, Menon M (2002) Prognostic impact of histologic subtyping of adult renal epithelial neoplasms: an experience of 405 cases. Am J Surg Pathol 26:281–291
Paner GP, Amin MB, Alvarado-Cabrero I et al (2010) A novel tumor grading scheme for chromophobe renal cell carcinoma: prognostic utility and comparison with Fuhrman nuclear grade. Am J Surg Pathol 34:1233–1240
Lohse CM, Blute ML, Zincke H, Weaver AL, Cheville JC (2002) Comparison of standardized and nonstandardized nuclear grade of renal cell carcinoma to predict outcome among 2,042 patients. Am J Clin Pathol 118:877–886
Delahunt B, Eble JN, Egevad L, Samaratunga H (2019) Grading of renal cell carcinoma. Histopathology 74:4–17
Griffiths IH, Thackray AC (1949) Parenchymal carcinoma of the kidney. Br J Urol 21:128–151
Ohashi R, Schraml P, Angori S et al (2019) Classic chromophobe renal cell carcinoma incur a larger number of chromosomal losses than seen in the eosinophilic subtype. Cancers 11:1492
Ohe C, Kuroda N, Matsuura K et al (2014) Chromophobe renal cell carcinoma with neuroendocrine differentiation/morphology: a clinicopathological and genetic study of three cases. Hum Pathol Case Reports 1:31–39
Mokhtar GA, Al-Zahrani R (2015) Chromophobe renal cell carcinoma of the kidney with neuroendocrine differentiation: a case report with review of literature. Urol Ann 7:383–386
Peckova K, Martinek P, Ohe C, Kuroda N, Bulimbasic S, Condom Mundo E, Perez Montiel D, Lopez JI, Daum O, Rotterova P, Kokoskova B, Dubova M, Pivovarcikova K, Bauleth K, Grossmann P, Hora M, Kalusova K, Davidson W, Slouka D, Miroslav S, Buzrla P, Hynek M, Michal M, Hes O (2015) Chromophobe renal cell carcinoma with neuroendocrine and neuroendocrine-like features. Morphologic, immunohistochemical, ultrastructural, and array comparative genomic hybridization analysis of 18 cases and review of the literature. Ann Diagn Pathol 19:261–268
Brierley J, Gospodarowicz M, Wittekind C (2017) UICC TNM classification of malignant tumours, 8th edn. Wiley, Chichester
Akhtar M, Tulbah A, Kardar AH, Ali MA (1997) Sarcomatoid renal cell carcinoma: the chromophobe connection. Am J Surg Pathol 21:1188–1195
de Peralta-Venturina M, Moch H, Amin M, Tamboli P, Hailemariam S, Mihatsch M, Javidan J, Stricker H, Ro JY, Amin MB (2001) Sarcomatoid differentiation in renal cell carcinoma: a study of 101 cases. Am J Surg Pathol 25:275–284
Hayes AF, Krippendorff K (2007) Answering the call for a standard reliability measure for coding data. Commun Methods Meas 1:77–89
Kanda Y (2013) Investigation of the freely-available easy-to-use software “EZR” (Easy R) for medical statistics. Bone Marrow Transplant 48:452–458
Firth D (1993) Bias reduction of maximum likelihood estimates. Biometrika 80:27–38
Efron B, Tibshirani RJ (1986) Bootstrap methods for standard errors, confidence intervals, and other measures of statistical accuracy. Stat Sci 1:54–77
Matsuda Y, Yoshimura H, Ishiwata T, Sumiyoshi H, Matsushita A, Nakamura Y, Aida J, Uchida E, Takubo K, Arai T (2016) Mitotic index and multipolar mitosis in routine histologic sections as prognostic markers of pancreatic cancers: a clinicopathological study. Pancreatology 16:127–132
Trpkov K, Williamson SR, Gao Y, Martinek P, Cheng L, Sangoi AR, Yilmaz A, Wang C, San Miguel Fraile P, Perez Montiel DM, Bulimbasić S, Rogala J, Hes O (2019) Low-grade oncocytic tumour of kidney (CD117-negative, cytokeratin 7-positive): a distinct entity? Histopathology 75:174–184
Przybycin CG, Cronin AM, Darvishian F, Gopalan A, al-Ahmadie HA, Fine SW, Chen YB, Bernstein M, Russo P, Reuter VE, Tickoo SK (2011) Chromophobe renal cell carcinoma: a clinicopathologic study of 203 tumors in 200 patients with primary resection at a single institution. Am J Surg Pathol 35:962–970
Cheville JC, Lohse CM, Zincke H, Weaver AL, Blute ML (2003) Comparisons of outcome and prognostic features among histologic subtypes of renal cell carcinoma. Am J Surg Pathol 27:612–624
Leibovich BC, Lohse CM, Cheville JC et al (2018) Predicting oncologic outcomes in renal cell carcinoma after surgery. Eur Urol 73:772–780
Volpe A, Novara G, Antonelli A et al (2012) Chromophobe renal cell carcinoma (RCC): oncological outcomes and prognostic factors in a large multicentre series. BJU Int 110:76–83
Casuscelli J, Weinhold N, Gundem G et al (2017) Genomic landscape and evolution of metastatic chromophobe renal cell carcinoma. JCI Insight 2
Casuscelli J, Becerra MF, Seier K et al (2019) Chromophobe renal cell carcinoma: results from a large single-institution series. Clin Genitourin Cancer
Ged Y, Chen YB, Knezevic A, Casuscelli J, Redzematovic A, DiNatale R, Carlo MI, Lee CH, Feldman DR, Patil S, Hakimi AA, Russo P, Motzer RJ, Voss MH (2019) Metastatic chromophobe renal cell carcinoma: presence or absence of sarcomatoid differentiation determines clinical course and treatment outcomes. Clin Genitourin Cancer 17:e678–e688
Lakhani SR, Ellis IO, Schnitt SJ et al (2012) WHO classification of tumours of the breast. World Health Organization, Lyon
Rutkowski P, Bylina E, Wozniak A, Nowecki ZI, Osuch C, Matlok M, Switaj T, Michej W, Wroński M, Głuszek S, Kroc J, Nasierowska-Guttmejer A, Joensuu H (2011) Validation of the Joensuu risk criteria for primary resectable gastrointestinal stromal tumour - the impact of tumour rupture on patient outcomes. Eur J Surg Oncol 37:890–896
Lloyd RV, Osamura RY, Kloppel G et al (2017) WHO Classification of tumours of endocrine organs (World Health Organization Classification of Tumors), 4th edn. IARC Press, Lyons
Acknowledgments
The authors thank the following individuals: Susanne Dettwiler and Fabiola Prutek (Department of Pathology and Molecular Pathology, University Hospital Zurich), Kazue Kobayashi, Ayako Maruyama, Naoyuki Yamaguchi (Division of Molecular and Diagnostic Pathology, Niigata University Graduate School of Medical and Dental Sciences), Chikashi Ikegame, Kanae Takahashi, Yukie Kawaguchi and Chiaki Yokoyama (Division of Pathology, Niigata University Medical & Dental Hospital) for their outstanding technical assistance; Aashil Batavia for critical manuscript reading (Department of Pathology and Molecular Pathology, University Hospital Zurich); Takahiro Tanaka, Nobutaka Kitamura (Clinical and Translational Research Center, Niigata University Medical & Dental Hospital) and Daisuke Tokita (Clinical and Academic Research Promotion center, Tokyo Women’s Medical University) for assistance with the statistical analysis; Toshio Takagi (Department of Urology, Tokyo Women's Medical University) for insightful discussions on clinical aspects.
Funding
This work was supported in part by Niigata Foundation for the Promotion of Medicine (2015) to RO and the Swiss National Science Foundation grant to HM (No. S-87701-03-01).
Author information
Authors and Affiliations
Contributions
RO and HM designed the research and wrote the paper. All authors acquired the data. RO, GM, AH, AC, DS, and HM analyzed and interpreted the pathological data. RO performed statistical analysis. All authors critically reviewed, edited, and approved the manuscript. RO and HM provided funding. HM supervised the study and is the guarantor of the study.
Corresponding author
Ethics declarations
This study was approved by the institutional review board of each contributing institutions.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised: The legends of Figures 1 and 3 in the published original version of the above article are incorrect. The original article has been corrected.
Electronic supplementary material
ESM 1
Supplementary Figure 1 pT stage (A), sarcomatoid differentiation (B) presence of necrosis (C) and presence of mitosis (D) and time to progression in the Japanese cohort (Kaplan-Meier survival analysis). Supplementary Figure 2 pT stage (A), sarcomatoid differentiation (B), presence of necrosis (C), presence of mitosis (D) and time to progression in the Italian cohort (Kaplan-Meier survival analysis). (PDF 591 kb)
Rights and permissions
About this article
Cite this article
Ohashi, R., Martignoni, G., Hartmann, A. et al. Multi-institutional re-evaluation of prognostic factors in chromophobe renal cell carcinoma: proposal of a novel two-tiered grading scheme. Virchows Arch 476, 409–418 (2020). https://doi.org/10.1007/s00428-019-02710-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-019-02710-w