Abstract
Cancer registries are essential in health care, since they allow more accurate planning of necessary health services and evaluation of programs for cancer prevention and control. The Hellenic Society of Pathology (HSP) having recognized the lack of such information in Greece has undertaken the task of a 5-year pathology-based cancer registry in Greece (2009–2013). In this study, > 95% of all pathology laboratories in the national health system hospitals and 100% of pathology laboratories in private hospitals, as well as > 80% of private pathology laboratories have contributed their data. The most common cancer types overall were as follows: breast cancer (18.26%), colorectal cancer (15.49%), prostate cancer (13.49%), and lung cancer (10.24% of all registered cancers). In men, the most common neoplasms were as follows: prostate cancer, colorectal cancer, lung cancer, and gastric cancer. In women, the most common neoplasms were as follows: breast cancer, colorectal cancer, thyroid cancer, and lung cancer. The data on cancer burden in Greece, presented herein, fill the void of cancer information in Greece that affects health care not only nationally but Europe-wise.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The importance of cancer registries has been recognized already from the early twentieth century, in Europe (Hamburg 1926, Mecklenbourg 1937, Denmark 1942) as well as in North America (Massachusetts 1927, Connecticut 1935) [1, 2]. In the 1950s, the World Health Organization formed a Subcommittee on the Registration of Cases of Cancer, while in the early 1960s, the USA launched the Surveillance, Epidemiology and End Results (SEER) [1,2,3]. In Europe, the International Association of Cancer Registries (IACR) (founded in 1966) collaborates with WHO on disease classification and the global burden of disease, is a partner of the International Union Against Cancer (UICC), and supports the activities of the European Network of Cancer Registries (ENCR) [2]. IACR collaborates with the International Agency for Research on Cancer (IARC) and publishes the valuable series of volumes in “The Cancer Incidence in Five Continents” [1,2,3].
It is disappointing that in Greece, despite the high level of medical care, there are no complete data on cancer registries, and in the IACR maps, Greece is colored as “registration activity” [4, 5], although official but incomplete efforts have started as early as 1967 [6, 7].
The three major types of cancer registries are hospital-based, pathology-based, and population-based. The Hellenic Society of Pathology (HSP) has long recognized the need for an official cancer registry in Greece. Thus, adhering to the principles of its statutes and bylaws, namely commitment to the improvement of public health and to consolidation of the role of the pathologists as health care providers, HSP has undertaken the task of a 5-year pathology-based cancer registry in Greece (2009–2013). In this study, almost all pathology laboratories from the public and private hospitals, as well as the vast majority of small private pathology laboratories, have contributed their data. A global view of the final results is presented herein.
Materials and methods
For the study, an official permission was granted by a constitutionally consolidated independent authority, the Hellenic Data Protection Authority (HDPA). The collection of data started in November 2010 and was concluded in December 2016. All actions were carried based on internationally accepted methods and standards [4, 8].
“Cancer Registrars” visited the participating pathology laboratories, which are listed in Supplement 1. The “Cancer Registrars” were either registrars hired for this purpose or pathology residents and all were specially trained by the HSP. All registrars signed a confidentiality contract. A special permission was granted to access and collect all necessary and essential information from the archival pathology reports. Special forms were completed on site containing the following: the pathology laboratory, the name of the patient, date of birth, sex, incidence date, primary tumor site, laterality (in paired organs), tumor macroscopic data (e.g., size), histological diagnosis, grade, co-existence of dysplasia or in situ neoplasm, prognostic and predictive markers, and pTNM staging, when information was applicable and available. The name of the patient was encrypted in arithmetical code. With the encryption method of registry, there is no possibility to register the same patient more than one time, even if they were biopsied or underwent surgery in different hospitals/regions for primary or recurrent/metastatic disease.
All written forms were collected in the offices of HSP and were accessed by a single registrar designated for this task. All data were electronically entered in a single system (ACCESS). We have recorded cancer sites/diagnoses as follows: breast, colorectum, gastric, liver, lung, pancreas, prostate gland, cervix uteri, ovaries, melanoma (skin only), thyroid gland, kidney, bone marrow/lymphomas (Hodgkin and non-Hodgkin lymphomas, myelodysplastic/myeloproliferative neoplasms, leukemias, plasma cell neoplasms), bone (only giant cell tumors), central nervous system (only glial neoplasms), neuroendocrine neoplasms (except in lung), and GISTs in all sites.
To calculate the age-standardized incidence rate (ASIR), we calculated the age-specific (incidence) rates for each age group by dividing the number of incidence by the respective population and then by multiplying the resulting number by 100,000. Age groups for the different cancer types were 0–49, 50–59, 60–69, and 70+. Thereinafter, we multiplied each of the age-specific rates by the proportion of the 2011 population belonging to the particular age group (called the standard population weight). The age-standardized rates have been obtained by adding the resulting numbers of each age group per cancer type. The rates are standardized to the 2011 population, since 2011 is the only year where official data of the Hellenic Statistical Authority are available.
Results
During the 5 years of our registry (2009–2013), we have registered 183,398 cancers in pathology laboratories. Today, in Greece, 335 pathologists are members of the HSP. Pathology departments are established in all seven medical schools and in national health system hospitals, as well as in private hospitals and also in private practice.
The pathology laboratories that participated in this study (Supplement 1) comprise the 97.4% of all pathology laboratories in the national health system, 6 out of 7 university hospital laboratories (85.7%), 21 out of 21 (100%) major private hospitals, and the vast majority of private pathology laboratories in Greece (more than 80%).
Based on the official data of the Hellenic Statistical Authority for 2011, the population in Greece was 10,816,286 people (http://www.statistics.gr/). By calculating the geographical areas covered by the pathology laboratories that participated in the registry and the very high percentage of the pathology laboratories registered, we conclude that in our pathology registry, we have covered more than 95% of the population in Greece in all regions/prefectures.
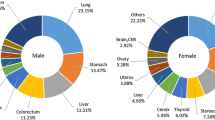
Of the 183,398 registered cancers during the 5-year period, 50.06% (91,317 cases) occurred in men and 49.94% (91,081) in women (Table 1). The most common cancer types overall were as follows: breast cancer (18.26% of all registered cancers, 33,304 cases), colorectal cancer (15.49% of all registered cancers, 28,254 cases), prostate cancer (13.49% of all registered cancers, 24,599 cases), and lung cancer (10.24% of all registered cancers, 18,681 cases). These represent more than half (57.48%) of the cancer burden in Greece. In men, the most common neoplasms were as follows: prostate cancer (24,599 cases), colorectal cancer (15,993 cases), lung cancer (15,151 cases), and gastric cancer (5044 cases) (Tables 1 and 2). In women, the most common neoplasms were as follows: breast cancer (32,959 cases), colorectal cancer (12,261 cases), thyroid cancer (8865 cases), and lung cancer (3530 cases) (Tables 1 and 2). The crude incidence rates of the four most common neoplasms in both sexes are presented in Table 3. The age-standardized incidence rates for the four most common neoplasms are presented in Table 4.
Regarding cervical cancer, during the 5-year period, a total of 1637 invasive and micro-invasive carcinomas were recorded (of all histological types) and 6180 cases of high-grade SIL and in situ adenocarcinomas.
There were no statistical differences in yearly incidence over this 5-year period, overall or in males and females. The total number of registered cancers was 37,234 for the year 2009 (20.41%), 35,753 for the year 2010 (19.60%), 35,624 for the year 2011 (19.53%), 36,316 for the year 2012 (19.91%), and 37,471 for the year 2013 (20.54%). The incidence of the more common cancers in males and females over the period 2009–2013 per year is depicted in Fig. 1.
Greece consisted traditionally of 54 prefectures. Since 2011, Greece has been subdivided into 13 regions (Kallikratis program). In our registry, we have included the vast majority of pathology laboratories in all 13 regions. In our registered cancer cases, there are no statistically significant differences in cancer incidence between regions.
Discussion
Despite the recognition of the importance of cancer registries for public health today in Greece, there are no complete data on cancer registries. In the IACR maps, Greece is colored as “registration activity,” just above the “no data/status unknown” [4, 5]. In Greece, official efforts for cancer registration have commenced as early as 1967 under the Hellenic Statistical Authority and later (1990) by the Department of Hygiene of the Hellenic Ministry for Health and Social Solidarity. Today, the Hellenic Cancer Registry runs under the Hellenic Center for Disease Control and Prevention (HCDCP), since 2008 (by law since 2005) [6, 7]. Despite this long history, when cancer incidence and mortality patterns in Europe are reported, there are either no data or only estimated data, extracted from cancer registries in neighboring countries (e.g., Bulgaria, Cyprus, central Serbia) [9,10,11].
There are three major types of cancer registries: the hospital-based which collects information from hospitals on all cases of cancer treated there, the pathology-based which collects information from pathology laboratories on cancers that have been histologically diagnosed, and the population-based which collects information from multiple sources, hospital and pathology records, community records, public sources, etc. on all neoplasms in patients within a certain geographic area [4, 5]. Population-based cancer registries are considered the gold standard as a source of information on cancer incidence in a certain population. The aim of cancer registries is not only the estimation of the frequency of the disease, its patterns, and trends, but also the understanding of its natural history, possible etiological cause, and pathogenesis. Based on these, governmental cancer-related strategies can be drawn [1,2,3,4].
In pathology-based registries, patients with diagnosed overt cancer are recorded. The final diagnosis of neoplastic disease has always been in the hand microscope of the pathologist. It is true that cancer registries are not as strong epidemiological tools as the population-based registries. Thus, as already stated, a pathology-based cancer registry is justified in the proper framework of a certain society [1]. It is also true that a pathology-based registry cannot be used for cancer surveillance purposes.
Greece is a relatively small country, in southeastern Europe, of approximately 11 million people with pathology laboratories covering all 13 regions. With the inclusion of the vast majority of pathology laboratories in this study, the number of missing reports is minimal. Based on our data, the cancer incidence in Greece is comparable with that in Europe [11]. The four most common are the same (breast, colorectal, prostate, and lung cancers), and as in Europe, they comprise more than 50% of registered cancers.
According to the GLOBOCAN 2012 estimated cancer incidence in Greece, the four most common cancers in both sexes are lung, breast, colorectal, and prostate, in male are lung, prostate, bladder, and colorectal, and in female are breast, colorectum, lung, and leukemia (Table 1) (http://globocan.iarc.fr/Pages/summary_table_pop_sel.aspx). There are indeed some differences between these data and the reported herein. A weak point in our study is that in Greece, the medical specialties of pathology and cytology are two different ones. Thus, in most hospitals, there is a department of pathology and a closely affiliated, but separate, department of cytology. This is not a problem, since in Greece, for diagnosis and treatment of any neoplasia, a biopsy and/or surgical excision is necessary, all diagnosed and registered in a pathology laboratory. There are the cases (stages IIIB and IV) of lung cancer where the cytology is positive, but the bronchial biopsy is not performed and surgical excision is not recommended. These patients are only registered in the departments of cytology and thus are not included in our cancer registry. This population is estimated approximately to 10% of lung cancer patients; thus, it does not significantly affect our study, although there is a possibility that the incidence of lung cancer is somewhat higher than the one registered. A proof of the accuracy of our results is that the ratio men/women regarding lung cancer is comparable to published European studies [9,10,11]. It is important however to underline the low incidence of lung cancer among women compared to that of men population (15–20% of the total lung cancer cases) which is attributed to the very low smoking rate among women in the previous generation.
Furthermore, our study is based on the real incidence as registered in the pathology laboratories in Greece and the GLOBOCAN data are an estimate; thus, some differences may reflect actual different incidences, since the GLOBOCAN estimation is based on the registered numbers of neighboring countries, with which Greece may have significant differences in environmental, lifestyle, and genetically related cancer risk factors. For example, leukemia is not among the four most common cancers in women; however, we believe that this estimate in GLOBOCAN incidence refers to a broad category which most probably also includes lymphomas, myelodysplastic syndromes, etc. Instead, in a female Greek population, thyroid cancer is quite common, a registered fact, and quite different from the estimated low GLOBOCAN incidence. This high incidence might reflect known environmental catastrophes in the vicinity of Greece a few decades ago. In fact, this is one of the strengths in our study, which can draw attention on certain cancers with actual incidence quite different from the estimated one.
It appears from our registry that in Greece, the burden of cervical neoplasia is quite high; however, 79% of cases are not invasive. This is a powerful indication that the national health system policy regarding the organized screening for cervical cancer is successful.
Another weak point in our study is that some neoplasms are missing from the registry. The original planning in 2008 did not include some rare neoplasms, such as head and neck; so now, we do not have data on them. Bladder neoplasms were not included since then, it was estimated that most were superficial papillary carcinomas, without serious consequences.
In conclusion, we present herein the first official cancer registry in Greece for a 5-year period (2009–2013). We would like to support that this cancer registry is as powerful as a population registry for cancer incidence, particularly in the absence of official population registry data. This is because it includes data from the vast majority of Hellenic Pathology Laboratories, where all malignant neoplasms are diagnosed and recorded, and which are estimated to cover an area of more than 95% of population in Greece.
References
Terracini B, Zanetti R (2003) A short history of pathology registries, with emphasis on cancer registries. Soz- Präventivmed 48:3–10
Saracci R, Wild CP (2015) International Agency for Research on Cancer: the first 50 years, 1965–2015. WHO Press ISBN 978-92-832-0441-1
Whelan SL (2010) International Association of Cancer Registries—a history. Asian Pacific Journal of Cancer Prevention Vol 11, IACR Supplement ISSN 1513–7368
Bray F, Znaor A, Cueva P, Korir A, Swaminathan R, Ullrich A, Wang SA, Parkin DM (2014) Planning and developing population-based cancer registration in low- and middle-income settings IARC Technical Publication No 43, Chapter 2, Chapter 6
UICC Cancer registries—why, what and how? www.uicc.org
Hellenic Cancer Registry (HCR): two years after. HCR Office, HCDCF, 8 April 2015. www2.keelpno.gr
Tzala L (2011) The development of the Hellenic Cancer Registry, HCDCP Newsletter 2011 Vol 11/year 1st ISSN 1792-9016
Bray F, Parkin DM (2009) Evaluation of data quality in the cancer registry: principles and methods. Eur J Cancer 45(5):747–755. https://doi.org/10.1016/j.ejca.2008.11.032
Karim-Kos HE, de Vries E, Soerjomatarama I, Lemmens V, Siesling S, Coebergh JWW (2008) Recent trends of cancer in Europe: a combined approach of incidence, survival and mortality for 17 cancer sites since the1990s. EJC 44:1345–1389
Ferlay J, Parkin DM, Steliarova-Foucher E (2010) Estimates of cancer incidence and mortality in Europe in 2008. EJC 46:765–781
Ferlay J, Steliarova-Foucher E, Lortet-Tieulent J, Rosso S, Coebergh JWW, Comber H, Forman D, Bray F (2013) Cancer incidence and mortality patterns in Europe: estimates for 40 countries in 2012. EJC 49:1374–1403
Acknowledgements
We are grateful to all pathologists (directors and staff pathologists) of the participating pathology laboratories, for enabling and facilitating in every possible way the HSP cancer registry. Without their work and support, this registry would not have been possible. We are also grateful to the past presidents of HSP, Professors E. Vrettou and E.N. Stathopoulos, for overseeing this project. Prof. E. Vrettou, in particular, was pivotal in the initiation and the establishment of the registry.
Funding
The work was funded by funds of the Hellenic Society of Pathology (www.pathology.gr).
Author information
Authors and Affiliations
Consortia
Contributions
All authors qualify for every one of the four criteria listed below:
• Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work
• Drafting the work or revising it critically for important intellectual content
• Final approval of the version to be published
• Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved
Corresponding author
Ethics declarations
The authors confirm that the work presented complies with ethical standards.
Conflict of interest
All authors declare that they have no conflict of interest.
Electronic supplementary material
ESM 1
(DOCX 17 kb)
Rights and permissions
About this article
Cite this article
Patsea, E., Kaklamanis, L., Batistatou, A. et al. The first report of a 5-year period cancer registry in Greece (2009–2013): a pathology-based cancer registry. Virchows Arch 472, 677–682 (2018). https://doi.org/10.1007/s00428-017-2287-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-017-2287-8