Abstract
Formalin-fixed paraffin-embedded (FFPE) tissue blocks are widely used to identify clinically actionable molecular alterations or perform retrospective molecular studies. Our goal was to quantify degradation of DNA occurring during mid to long-term storage of samples in usual conditions. We selected 46 FFPE samples of surgically resected carcinomas of lung, colon, and urothelial tract, of which DNA had been previously extracted. We performed a second DNA extraction on the same blocks under identical conditions after a median period of storage of 5.5 years. Quantitation of DNA by fluorimetry showed a 53% decrease in DNA quantity after storage. Quantitative PCR (qPCR) targeting KRAS exon 2 showed delayed amplification of DNA extracted after storage in all samples but one. The qPCR/fluorimetry quantification ratio decreased from 56 to 15% after storage (p < 0.001). Overall, remaining proportion of DNA analyzable by qPCR represented only 11% of the amount obtained at first extraction. Maximal length of amplifiable DNA fragments assessed with a multiplex PCR was reduced in DNA extracted from stored tissue, indicating that DNA fragmentation had increased in the paraffin blocks during storage. Next-generation sequencing was performed on 12 samples and showed a mean 3.3-fold decrease in library yield and a mean 4.5-fold increase in the number of single-nucleotide variants detected after storage. In conclusion, we observed significant degradation of DNA extracted from the same FFPE block after 4 to 6 years of storage. Better preservation strategies should be considered for storage of FFPE biopsy specimens.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Preservation of tumor DNA is a major issue in molecular oncology. In clinical care, the development of targeted treatments often requires molecular analyses of tumor tissue samples several years after diagnosis. For research purposes, new molecular targets may be studied in retrospective cohorts including tissue samples. Routine histopathological samples are mostly stored as formalin-fixed paraffin-embedded (FFPE) specimens, and rarely as fresh-frozen (FF) samples. However, DNA degradation is more substantial in FFPE samples than in FF samples [1, 2], due to fragmentation and chemical modification of DNA resulting from formalin fixation and paraffin embedding. Molecular analysis by next-generation sequencing (NGS) fails more often when DNA extracted from old FFPE samples is used [2].
Two studies [3, 4], using a spectrophotometric method of quantification (UV absorbance at 260 nm), reported that the quantity and quality of DNA, extracted from different FFPE blocks of surgically resected tissue after periods of storage between less than a year up to 12 years, was similar. However, spectrophotometry has low specificity because the presence of single-strand DNA, RNA, nucleotides, or contaminants such as proteins and phenols may significantly affect the results [5], resulting in overestimation of DNA concentration [6]. In partially degraded DNA from FFPE samples, fluorimetry (which relies on the specific binding of a fluorochrome to double-strand DNA) is considered more accurate. Adema et al. observed that PCR amplifiable DNA fragments extracted from tissue blocks in 2002 were longer than the fragments extracted from the same blocks in 2010, indicating some degradation during storage [7].
To the best of our knowledge, proper quantification of degradation of DNA during storage of FFPE tissue blocks has not been reported. The aim of our study was to compare the quantity and quality of DNA extracted from the same FFPE samples stored for several years under usual conditions, using fluorimetry and quantitative PCR.
Methods
Sample selection
To compare quantity and quality of DNA extracted from the same FFPE blocks after prolonged storage, we selected surgically resected tissue samples from colon, lung, and urothelial tract cancer, of which in the past DNA had been extracted for molecular diagnosis. Colon and urothelial cancer tissue blocks had been prepared and stored in the Department of Pathology of Hospital Henri-Mondor (Créteil, Assistance Publique–Hôpitaux de Paris, France), whereas lung cancer tissue blocks had been prepared and stored in the Pathology laboratory of Dr Georges (rue de Wattignies, Paris 12ème, France). All samples had been fixed in buffered neutral 4% formaldehyde. FFPE blocks were stored without monitoring of uncontrolled ambient temperature and humidity.
DNA extraction and quantification with fluorimetry
Technical parameters, including area to be macrodissected (when necessary), number and thickness of FFPE sections (usually 7 sections of 5 μm), and elution volume (50 to 200 μl), had been recorded during initial extraction (sample A). For each tissue block, a new DNA extraction (sample B) was performed, under strictly identical conditions (macrodissection area, number and thickness of FFPE sections, and elution volume). DNA extraction was performed using BioRobot® EZ1™ (Qiagen, Milan, Italy) and the EZ1® DNA Tissue Kit (Qiagen) according to the manufacturer’s instructions. All extractions were performed in the pathology laboratory of hospital Henri Mondor, and DNA samples were stored at −20 °C.
DNA concentration of sample A and sample B was quantified at the same time by fluorimetry using Qubit dsDNA BR Assay Kit for Qubit® 2.0 Fluorometer (Life Technologies, Carlsbad, CA, USA).
Quantification of DNA by quantitative PCR
Amplifiable DNA was quantified by quantitative PCR (qPCR) targeting exon 2 of KRAS (NM_004985) using LightCycler® 480 (Roche, Basel, Switzerland). The primer sequences were as follows: forward 5′-TTATAAGGCCTGCTGAAAATG-3′, reverse 5′-CAAGATTTACCTCTATTGTTGGATCA-3′. Amplicon size was 137 bp. The final volume of the qPCR reaction was 20 μL, containing 10 μL of LightCycler 480 HRM MasterMix (Roche), 3.125 mM MgCl2, 0.1 μM each primer, 0.5 U of Uracil-N-Glycosylase, and 10 ng of DNA, as measured by fluorimetry. DNA samples were treated with uracil glycosylase before amplification to avoid artifacts due to cytosine deamination. The concentration of the stock solution of four samples was lower than 10 ng/μL, and these were added to the PCR reaction without dilution. The cycling protocol was as follows: incubation at 37 °C for 10 min, denaturation at 95 °C for 5 min, 50 cycles of amplification (30 s at 94 °C, 30 s at 58 °C, and 45 s at 72 °C), followed by a melting curve (denaturation at 95 °C, hybridization at 40 °C, and melting from 70 to 95 °C). DNA of sample A and sample B was amplified on the same PCR plate, and all samples were tested in duplicate.
Using the linear correlation between initial DNA amount and the crossing point (Cp) measured with the second derivative model, and a standard curve established with serial dilutions of a commercial DNA sample from 40.0 to 1.25 ng, we calculated the amount of amplifiable DNA for each sample. Post-amplification high-resolution melting (HRM) analysis was used to detect the presence of mutations in the amplified KRAS fragment including codon 12 and 13 hotspots.
Qualitative evaluation of the size of amplifiable fragments by PCR
The length of amplifiable DNA fragments was assessed using the multiplex PCR of the BIOMED2 European collaborative study [8]. Briefly, 20 ng DNA was amplified in a final volume of 20 μL containing 2 μL of GenAmp PCR Buffer II (Life technologies), 2 mM MgCl2, 0.05 μM of each primer (Supplementary Table 1), 0.2 mM dNTP, and 0.5 U of Taq Gold DNA Polymerase (Life technologies). The cycling protocol was as follows: denaturation at 95 °C for 7 min, 38 cycles of amplification (30 s at 94 °C, 40 s at 60 °C, and 45 s at 72 °C), followed by a final extension step at 72 °C for 10 min. PCR reaction products (8 μL) were separated in a 2% agarose gel in Tris-Borate-EDTA Buffer at 130 V.
Quantitative evaluation of the size of amplifiable fragments by multiplexed probe-based qPCR
A new multiplexed probe-based qPCR assay (ProNex™ DNA QC Assay, Promega) was used according to the manufacturer’s instructions to assess quantity and quality of genomic DNA extracted initially (sample A) and after storage (sample B). This multiplex assay detects and quantifies 75, 150, and 300 bp human genomic targets and includes an internal positive control (IPC). Serial dilution of the DNA QC Assay gDNA Standard, included in the kit, was done to obtain a scale from 0.0032 to 50 ng/μL. To perform quantification, 2 μL of each DNA was amplified in a final volume of 20 μL, containing 10 μL of DNA QC MasterMix and 1 μL of DNA QC Primer/Probe/IPC Mix. All PCR reactions were performed in duplicate. The cycling protocol was as follows: denaturation at 98 °C for 2 min followed by 40 cycles of amplification (15 s at 98 °C, 60 s at 60 °C). Standard curves derived from the gDNA standard dilutions were used to quantify the mean quantity of the three sized targets for each sample, using the Applied Biosystems® 7500 Software (ThermoFisher Scientific), and to calculate the percentage of DNA samples A and B amplified with the 150 bp relative to the 75 bp target and with the 300 bp relative to the 75 bp target.
Next-generation sequencing
For NGS, 10 ng of DNA (as measured by fluorimetry) was amplified using the Ion AmpliSeq™Colon and Lung Cancer Panel. Amplicons were then digested, barcoded, and amplified by using the Ion Oncomine™ Solid Tumor DNA Kit and Ion Select barcode adapter kit (ThermoFisher) according to the manufacturer’s instructions. After quantification of DNA, 25 pM of each library was multiplexed and clonally amplified on ion sphere particles (ISP) by emulsion PCR performed on Ion Chef (ThermoFisher) according to the manufacturer’s instructions. The ISP templates were loaded onto an Ion 316 chip and sequenced on a PGM sequencer with the Ion PGM Hi-Q Sequencing Kit according to the manufacturer’s instructions. Single-nucleotide variants and small indels were detected using the Variant Caller plug-in version 5.0.0.7 with low stringency settings (threshold of 2%).
Statistical analysis
All analyses were performed using GraphPad Prism software version 5.04. Wilcoxon and Kruskall-Wallis tests were used. A p value inferior to 0.05 was considered significant.
Results
Tissue sample characteristics
Of the 50 samples initially selected, four were excluded because the surface occupied by tumor tissue had changed between initial and later extraction, as evaluated by hematoxylin-eosin staining of control sections. The 46 tumors were obtained from partial colectomy (n = 21), transurethral tumor resection (n = 14), nephro-ureterectomy (n = 3), pulmonary lobectomy or segmental resection (n = 8). The delay between initial and later extractions was 5 to 6.3 years for samples of colon and urothelial tract cancer (median 5.6 and 5.4 years, respectively) and 4.3 to 4.8 years for samples of lung cancer (median 4.4 years) (Fig. 1). Table 1 lists the analysis results for each sample, including the period of storage, total amount of extracted DNA measured by fluorimetry, qPCR/fluorimetry ratio, percentage of DNA remaining after storage, and length of amplifiable DNA fragments. Elution volume, DNA concentration measured by fluorimetry and qPCR, Cp, and HRM results obtained with KRAS PCR are shown in supplementary data (Supplementary Table 2).
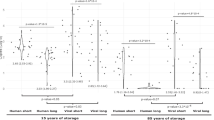
DNA amount measured by fluorimetry decreases after storage
With four exceptions (U1, U2, U3, and L8), all samples extracted from blocks after storage showed a decrease in DNA quantity (median concentration for samples A 71 ng/μL and for samples B 32 ng/μL, p < 0.0001). For colon samples, this was 105 and 38 ng/μL (p < 0.001), for urothelial tract samples 61 and 27 ng/μL (p < 0.01), and for lung samples 44 and 32 ng/μL (p < 0.05, all by Wilcoxon test) (Fig. 2a). Fold changes for total amount of DNA extracted from the blocks after storage are similar to those for DNA concentration, as the elution volume was kept constant (Supplementary Fig. 1). The median percentage of DNA extracted from stored blocks relative to that extracted initially (sample B concentration × 100/sample A concentration) was 47% for all samples. Significant differences existed between colon, urothelial tract, and lung samples (34, 62, and 72%, respectively, p 0.024, Kruskall-Wallis test) (Fig. 2b).
Fluorimetric analysis. a Fluorimetric quantification of DNA. A: First extraction. B: Second extraction; p-values: *< 0.05, **< 0.01, ***< 0.0001. Box plots indicating median, interquartile, and extreme values are shown. b Percentage of remaining DNA in samples extracted after storage evaluated by fluorimetry (Bx100/A). Individual values and median (bars) are shown
The fraction of amplifiable DNA decreases after storage
To further analyze the effect of storage time, the amount of amplifiable DNA was evaluated by qPCR, targeting an amplicon of 137 base pairs. Ten nanograms of DNA, as measured by fluorimetry, was amplified. For all samples (except C18), the amplification curve of sample B was delayed compared to that of sample A, indicating a decrease in the number of amplifiable DNA fragments (Supplementary Table 2). Figure 3a shows amplification curves of a representative sample (C4 from colon).
qPCR analysis. a Amplification curves of KRAS exon 2 (colon sample C4). DNA was diluted to a concentration of 10 ng/μL (measured by fluorimetry). A: First extraction, Cp (crossing point) = 29.8. B: Second extraction, Cp = 31.9. b qPCR/fluorimetry ratio (amplifiable DNA percentage); p values: **< 0.01, ***< 0.0001. Box plots indicating median, interquartile, and extreme values are shown. c Percentage of remaining DNA in B extraction, evaluated by qPCR, for each sample (Bx100/A). Individual values and median (bars) are shown
Amplifiable DNA quantities were calculated for all samples using a standard curve, established with a high quality reference DNA. The qPCR/fluorimetry quantification ratio represents the percentage of DNA that can be amplified by qPCR (Table 1), and its median value was 56% for all samples A and 15% for all samples B 15% (p < 0.0001). For colon samples A, this was 56% and for colon samples B 15% (p < 0.0001), for urothelial tract samples A the median value was 75% and for samples B 18% (p < 0.01) and for lung samples A 26% and for samples B 4% (p < 0.01, all by Wilcoxon test) (Fig. 3b). In summary, of samples A, 56% of DNA measured by fluorimetry was amplified by qPCR, and this was reduced to 15% for samples B.
Combining the amount of extracted DNA and the amplifiable fraction (sample B concentration × 100/sample A concentration), we found a median percentage of remaining DNA of 11% for all samples and of 9, 13, and 11% for colon, urothelial tract, and lung samples, respectively (Fig. 3c; differences not significant).
The length of amplifiable DNA fragments decreases during storage
To test whether sample B DNA is more fragmented than sample A DNA, we performed qualitative multiplex PCR of three samples per organ. Consistently, the maximum size of amplified fragments was lower in samples B than in samples A. In samples A, DNA fragments up to 300, 400, or 600 bp were amplified. The amplified fragments in samples B were consistently shorter (200 to 300 bp). Moreover, the intensity of the bands was lower in samples B, indicating that amplification was less efficient (Fig. 4a).
Evaluation of the length of amplifiable fragments. a DNA fragments amplifiable by multiplex PCR of the BIOMED2 European study were assessed: three samples each for each of the three different primary tumor types. A: First extraction. B: Second extraction. b and c Quantification of 75, 150, and 300 bp targets with a multiplex qPCR assay was used, to calculate the proportion of DNA that was amplified with the 150 bp relative to the 75 bp amplicon and with the 300 bp relative to the 75 bp amplicon, in extractions A and B, ***< 0.0001. Colon tumors (diamond symbols), urothelial tumors (round symbols), lung tumors (triangle symbols)
In order to further quantify DNA degradation, we used a DNA Quality Control Assay developed by Promega which is based on qPCR quantification of 75, 150, and 300 bp human genomic targets. Table 1 and Fig. 4b show that the mean percentage of 150 bp amplifiable DNA (relative to 75 bp DNA) decreased from 58% in samples A to 16% in samples B (p < 0.0001), and for a 300 bp amplicon, this fraction dropped from 31 to 2% (p < 0.0001).
Consistency of mutational assessment by HRM analysis
We took advantage of the qPCR-HRM experiment to search for KRAS exon 2 mutations. DNA from samples A and B of all three organs showed melting curves with a similar profile, either wild type or mutated (Supplementary Table 2). A mutated profile was observed for six out of 21 (29%) colon tumors, none of the 17 urothelial tumors and two of the eight (25%) lung tumors.
DNA extracted from stored tissue samples shows a loss of performance in NGS
In order to measure the effect of DNA degradation on mutation analysis by NGS, we analyzed DNA samples from four specimens each of colon, urothelial, and lung tumors. We observed a 3.3 [min 0.7–max 17.6] fold decrease in library yield (p = 0.0108) and a 4.5 [min 1–max 22.8] fold increase in single-nucleotide variant (SNV) rate (p = 0.006) (Fig. 5a, b), indicating a decrease in quantity and quality of DNA extracted after storage. The increased SNV rate is likely due to cytosine deamination due to formalin fixation, which results in C > T or G > A sequencing artifacts which we observed at low frequencies (< 5%) in samples B (Supplementary Fig. 2).
NGS analysis. a The concentration of library obtained after amplification with Oncomine Solid Tumor DNA (Thermo Fisher) using DNA from A (first) or B (second) extraction, measured with qPCR, *< 0.05. b SNV were detected by the Ion Reporter ™ (Thermo Fisher) bioinformatic pipeline after Personal Genome Machine ((Thermo Fisher) sequencing using DNA from A (first) or B (second) extraction, **< 0.01. Colon tumors (diamond symbols), urothelial tumors (round symbols), lung tumors (triangle symbols)
Discussion
The aim of our study was to quantify degradation of DNA due to prolonged storage of FFPE tissue blocks (up to 6 years) under non-controlled conditions. We chose surgically resected specimens rather than biopsy specimens in order not to exhaust tissue samples and to limit bias. In addition, the in-between section variability of serial sections from FFPE blocks of surgically resected specimens is less than that from biopsies, and from surgical specimens, a larger amount of tissue could be extracted. We show that after 4 to 6 years of storage of FFPE blocks (mean 5.4 years), the amount of DNA measured by fluorimetry is reduced to 47%, and only 11% of DNA is amplifiable. The strong decrease in the percentage of 150 or 300 bp target DNA that can be successfully amplified relative to 75 bp target indicates that it is due to fragmentation of DNA. Colon samples showed an increased loss of DNA compared to lung and urothelial tract tumors. We hypothesize that in these blocks, DNA was already fragmented early on, along with loss of very short fragments during storage. In addition, intrinsic physiological characteristics, such as a high microorganism content in colon samples, might be considered. For all but four samples (U1, U2, U3, and L8), the DNA concentration measured by fluorimetry was lower in sample B than in sample A. For these four samples, the slightly higher (3 to 10 ng/μL, mean 7 ng/μL) DNA concentration found might be explained by differences in the amount of tissue available. Conceivably, sections used for initial extraction were relatively superficial in the block, while later extraction was from deeper sections which are often larger.
We use the Cp value obtained during PCR amplification of exon 2 of KRAS as a surrogate marker for the amount of amplified DNA, considering HRM results to be reliable when the sample Cp is lower than 35. All 46 samples A had a Cp less than 35 while of samples B, 43 also had a Cp less than 35 and 3 between 35 and 38. This signifies that based on these Cp values, most cases remain sufficient for interpretation, which is also reflected in concordant fusion profiles in HRM analysis. While this is true for DNA extracted from surgically resected samples, with a huge amount of tissue resulting in a large amount of DNA, of biopsy samples, the amount of tissue is much more limited and loss of DNA may be much more detrimental.
NGS is a descriptive term for sensitive sequencing techniques which allow sequencing of small amounts of DNA, even up to DNA of a single cell [9, 10]. Through NGS, DNA obtained from prehistoric human tissue from Egyptian mummies [11] or from Denisova individuals [12] has been sequenced. Ancient DNA is highly modified, post-mortem damages including artefactual sequences due to cytosine deamination which results in uracil, similar to what is found in FFPE samples [13]. Schweiger et al. successfully performed massive parallel short-read sequencing (Illumina Genome Analyzer) on samples of FFPE breast cancer tissue stored for 14 and 18 years [14]. Several publications emphasize that for NGS on FFPE samples, quality thresholds need to be defined. Algorithms have been proposed, which include DNA quantity [15, 16]. Choudhary et al. showed that there is little increase in background mutations when the quantity of high-quality DNA used in NGS is reduced, but that the background mutation rate strongly increases when the same experiment is performed with lower quality FFPE DNA, notably of G > A and C > T due to cytosine to uracil deamination as a result of formalin fixation [15]. Sie et al. set quality criteria of DNA for NGS, including a minimal sequence library yield of 1 nmole, a minimum number of 100,000 reads and a minimum of 90% of amplicons with more than 100× coverage, which are not reached on samples with very low (< 30 ng) DNA content [16]. In a prospective series of FFPE samples in patients with non-small cell lung cancer sequenced by NGS, 8% of the samples had to be excluded because of insufficient quality or quantity of extracted DNA [17]. This rose to 19 and 24% for fine needle aspiration samples and core biopsies of the primary tumor and up to 50% in fine needle aspiration samples of metastatic lesions. The failure rate therefore appears to be rather elevated in recently procured FFPE samples, and conceivably might be much higher in samples stored for prolonged periods of time. Our NGS experiments support these notions, as library yield decreased and mutation background increased on DNA samples extracted from FFPE tissue after prolonged periods of storage.
Populations of tumor cells are in permanent evolution due to genome instability which results in intra-tumoral heterogeneity. Heterogeneity is an inherent part of tumor evolution and is increased by treatment, conventional chemotherapy, as well as targeted therapy [18]. To better understand tumor evolution, technologies allowing analysis of the tumor genome during clinical evolution are being developed. Serial follow-up biopsies are indicated in relapsed lung cancer to assess development of mutations which confer resistance and to adapt treatment accordingly [19, 20]. Analysis of circulating tumor DNA is increasingly explored, as sample collection is non-invasive and plasma DNA conceivably contains of all genomic alterations of primary and metastatic sites of a tumor [21]. FFPE biopsy samples might be no longer used for follow-up purposes in the future, but they will continue to provide a valuable source of tissue samples for research, for example for rare diseases or infrequent tumor subtypes. In clinical care as well as in research projects, comparing the genome of metastatic lesions to that of the primary tumor will remain important to assess if mutations in recurrent lesions existed already in the primary tumor or were newly acquired.
In summary, it is essential to be aware of the extent of DNA degradation in FFPE samples after several years of storage. We suggest that DNA degradation during storage of FFPE samples can be limited, when effective preservation strategies are developed. These might include storage at + 4 °C [22, 23], or vacuum storage [22], as has been proposed for FFPE tissue sections. Alternatively, for each case, DNA could be systematically extracted. Such approaches might not be necessary in daily practice for all cases and might be applied only to biopsy samples from patients of whom a secondary lesion will not be treated by surgical resection.
References
Ferrer I, Armstrong J, Capellari S, Parchi P, Arzberger T, Bell J, Budka H, Strobel T, Giaccone G, Rossi G, Bogdanovic N, Fakai P, Schmitt A, Riederers P, Al-Sarraj S, Ravid R, Kretzschmar H (2007) Effects of formalin fixation, paraffin embedding, and time of storage on DNA preservation in brain tissue: a BrainNet Europe study. Brain Pathol 17(3):297–303. doi:10.1111/j.1750-3639.2007.00073.x
Hedegaard J, Thorsen K, Lund MK, Hein AM, Hamilton-Dutoit SJ, Vang S, Nordentoft I, Birkenkamp-Demtroder K, Kruhoffer M, Hager H, Knudsen B, Andersen CL, Sorensen KD, Pedersen JS, Orntoft TF, Dyrskjot L (2014) Next-generation sequencing of RNA and DNA isolated from paired fresh-frozen and formalin-fixed paraffin-embedded samples of human cancer and normal tissue. PLoS One 9(5):e98187. doi:10.1371/journal.pone.0098187
Kokkat TJ, Patel MS, McGarvey D, LiVolsi VA, Baloch ZW (2013) Archived formalin-fixed paraffin-embedded (FFPE) blocks: a valuable underexploited resource for extraction of DNA, RNA, and protein. Biopreserv Biobank 11(2):101–106. doi:10.1089/bio.2012.0052
Nam SK, Im J, Kwak Y, Han N, Nam KH, Seo AN, Lee HS (2014) Effects of fixation and storage of human tissue samples on nucleic acid preservation. Korean J Pathol 48(1):36–42. doi:10.4132/KoreanJPathol.2014.48.1.36
Bhat S, Curach N, Mostyn T, Bains GS, Griffiths KR, Emslie KR (2010) Comparison of methods for accurate quantification of DNA mass concentration with traceability to the international system of units. Anal Chem 82(17):7185–7192. doi:10.1021/ac100845m
Simbolo M, Gottardi M, Corbo V, Fassan M, Mafficini A, Malpeli G, Lawlor RT, Scarpa A (2013) DNA qualification workflow for next generation sequencing of histopathological samples. PLoS One 8(6):e62692. doi:10.1371/journal.pone.0062692
Adema V, Torres E, Sole F, Serrano S, Bellosillo B (2014) Paraffin treasures: do they last forever? Biopreserv Biobank 12(4):281–283. doi:10.1089/bio.2014.0010
van Dongen JJ, Langerak AW, Bruggemann M, Evans PA, Hummel M, Lavender FL, Delabesse E, Davi F, Schuuring E, Garcia-Sanz R, van Krieken JH, Droese J, Gonzalez D, Bastard C, White HE, Spaargaren M, Gonzalez M, Parreira A, Smith JL, Morgan GJ, Kneba M, Macintyre EA (2003) Design and standardization of PCR primers and protocols for detection of clonal immunoglobulin and T-cell receptor gene recombinations in suspect lymphoproliferations: report of the BIOMED-2 concerted action BMH4-CT98-3936. Leukemia 17(12):2257–2317. doi:10.1038/sj.leu.2403202
Navin N, Kendall J, Troge J, Andrews P, Rodgers L, McIndoo J, Cook K, Stepansky A, Levy D, Esposito D, Muthuswamy L, Krasnitz A, McCombie WR, Hicks J, Wigler M (2011) Tumour evolution inferred by single-cell sequencing. Nature 472(7341):90–94. doi:10.1038/nature09807
Zong C, Lu S, Chapman AR, Xie XS (2012) Genome-wide detection of single-nucleotide and copy-number variations of a single human cell. Science 338(6114):1622–1626. doi:10.1126/science.1229164
Khairat R, Ball M, Chang CC, Bianucci R, Nerlich AG, Trautmann M, Ismail S, Shanab GM, Karim AM, Gad YZ, Pusch CM (2013) First insights into the metagenome of Egyptian mummies using next-generation sequencing. J Appl Genet 54(3):309–325. doi:10.1007/s13353-013-0145-1
Reich D, Green RE, Kircher M, Krause J, Patterson N, Durand EY, Viola B, Briggs AW, Stenzel U, Johnson PL, Maricic T, Good JM, Marques-Bonet T, Alkan C, Fu Q, Mallick S, Li H, Meyer M, Eichler EE, Stoneking M, Richards M, Talamo S, Shunkov MV, Derevianko AP, Hublin JJ, Kelso J, Slatkin M, Paabo S (2010) Genetic history of an archaic hominin group from Denisova cave in Siberia. Nature 468(7327):1053–1060. doi:10.1038/nature09710
Brotherton P, Endicott P, Sanchez JJ, Beaumont M, Barnett R, Austin J, Cooper A (2007) Novel high-resolution characterization of ancient DNA reveals C > U-type base modification events as the sole cause of post mortem miscoding lesions. Nucleic Acids Res 35(17):5717–5728. doi:10.1093/nar/gkm588
Schweiger MR, Kerick M, Timmermann B, Albrecht MW, Borodina T, Parkhomchuk D, Zatloukal K, Lehrach H (2009) Genome-wide massively parallel sequencing of formaldehyde fixed-paraffin embedded (FFPE) tumor tissues for copy-number- and mutation-analysis. PLoS One 4(5):e5548. doi:10.1371/journal.pone.0005548
Choudhary A, Mambo E, Sanford T, Boedigheimer M, Twomey B, Califano J, Hadd A, Oliner KS, Beaudenon S, Latham GJ, Adai AT (2014) Evaluation of an integrated clinical workflow for targeted next-generation sequencing of low-quality tumor DNA using a 51-gene enrichment panel. BMC Med Genet 7:62. doi:10.1186/s12920-014-0062-0
Sie D, Snijders PJ, Meijer GA, Doeleman MW, van Moorsel MI, van Essen HF, Eijk PP, Grunberg K, van Grieken NC, Thunnissen E, Verheul HM, Smit EF, Ylstra B, Heideman DA (2014) Performance of amplicon-based next generation DNA sequencing for diagnostic gene mutation profiling in oncopathology. Cell Oncol (Dordr) 37(5):353–361. doi:10.1007/s13402-014-0196-2
Hagemann IS, Devarakonda S, Lockwood CM, Spencer DH, Guebert K, Bredemeyer AJ, Al-Kateb H, Nguyen TT, Duncavage EJ, Cottrell CE, Kulkarni S, Nagarajan R, Seibert K, Baggstrom M, Waqar SN, Pfeifer JD, Morgensztern D, Govindan R (2015) Clinical next-generation sequencing in patients with non-small cell lung cancer. Cancer 121(4):631–639. doi:10.1002/cncr.29089
McGranahan N, Swanton C (2015) Biological and therapeutic impact of intratumor heterogeneity in cancer evolution. Cancer Cell 27(1):15–26. doi:10.1016/j.ccell.2014.12.001
Jekunen AP (2015) Role of rebiopsy in relapsed non-small cell lung cancer for directing oncology treatments. J Oncol 2015:809835. doi:10.1155/2015/809835
Kuiper JL, Heideman DA, Thunnissen E, Paul MA, van Wijk AW, Postmus PE, Smit EF (2014) Incidence of T790M mutation in (sequential) rebiopsies in EGFR-mutated NSCLC-patients. Lung Cancer 85(1):19–24. doi:10.1016/j.lungcan.2014.03.016
Murtaza M, Dawson SJ, Tsui DW, Gale D, Forshew T, Piskorz AM, Parkinson C, Chin SF, Kingsbury Z, Wong AS, Marass F, Humphray S, Hadfield J, Bentley D, Chin TM, Brenton JD, Caldas C, Rosenfeld N (2013) Non-invasive analysis of acquired resistance to cancer therapy by sequencing of plasma DNA. Nature 497(7447):108–112. doi:10.1038/nature12065
Xie R, Chung JY, Ylaya K, Williams RL, Guerrero N, Nakatsuka N, Badie C, Hewitt SM (2011) Factors influencing the degradation of archival formalin-fixed paraffin-embedded tissue sections. J Histochem Cytochem 59(4):356–365. doi:10.1369/0022155411398488
Grillo F, Pigozzi S, Ceriolo P, Calamaro P, Fiocca R, Mastracci L (2015) Factors affecting immunoreactivity in long-term storage of formalin-fixed paraffin-embedded tissue sections. Histochem Cell Biol. doi:10.1007/s00418-015-1316-4
Acknowledgements
We thank the technicians of molecular biology and tissue bank from the department of pathology for their technical participation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
DNA was extracted from FFPE tissue blocks for medical diagnosis in compliance with French regulations.
Funding
This study was supported by institutional funding (AP-HP, hospital Henri Mondor, departement de Pathologie).
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
ESM 1
(DOCX 222 kb)
Rights and permissions
About this article
Cite this article
Guyard, A., Boyez, A., Pujals, A. et al. DNA degrades during storage in formalin-fixed and paraffin-embedded tissue blocks. Virchows Arch 471, 491–500 (2017). https://doi.org/10.1007/s00428-017-2213-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-017-2213-0