Abstract
Neuronatin (NNAT) is a proteolipid involved in cation homeostasis especially in the developing brain. Its expression has been associated with the progression of lung cancer, glioblastoma, and neuroblastoma as well as glucose induced apoptosis in pancreatic cells. We performed a retrospective study of 148 breast cancer specimens for NNAT expression by immunohistochemistry to evaluate this protein as a prognostic marker for breast cancer. We found a high NNAT immunoreactivity score (by multivariate cox regression) to be an independent prognostic marker for relapse-free (hazard ratio HR = 3.55, p = 0.002) and overall survival (HR = 6.29, p < 0.001). However, NNAT expression was not associated with classical parameters such as hormone receptor expression (p = 0.86) or lymph node metastasis (p = 0.83). Additional independent risk factors in this study population were tumor size (≤2 cm; overall survival: HR = 0.36, p = 0.023; relapse-free survival: HR = 0.26, p < 0.01) and blood vessel infiltration (overall survival: HR = 0.34 p < 0.01). NNAT expression determined by immunohistochemistry might therefore become a helpful additional biomarker to identify high-risk breast cancer patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neuronatin (NNAT) is a paternally imprinted gene and expressed during the development of the neuronal system [1, 2]. Based on its expression pattern, NNAT functions in the developing hindbrain [3] but a function in retina development has also been suggested [4]. In adult humans, NNAT mRNA is mainly expressed in the cerebral cortex, endocrine tissues, placenta, and adipose tissue [5, 6].
The NNAT gene encodes two proteolipids translated from differentially spliced mRNAs. Such proteolipids typically contain one membrane spanning hydrophobic alpha helix and a hydrophilic domain [7]. The function of the NNAT proteolipid is suspected to be similar to the function of the structurally related proteins phospholamban and plasma membrane ATPase-associated proteolipid 1 (PMP1), which are both involved in the regulation of ion channels [9]. NNAT seems to be particularly involved in the regulation of Ca-channels. Thereby, it controls protein folding as well as glycogen synthesis via the phosphatidylinositol-3-kinase. NNAT has also been found in neurological disorders such as Lafora disease where it forms cytotoxic aggregates [7]. It is also expressed in pancreatic β-islet cells where it can contribute to glucose induced apoptosis [10, 11].
In mice, NNAT is an inflammation and obesity-related gene and activates several signaling pathways such as p38 MAPK, Jun NH(2)-terminal kinase, extracellular signal-related kinase (ERK), and AKT but not NF-kB [12]. This link to obesity was further underlined by the finding that NNAT potentiates adipogenesis in rats by increased phosphorylation of CREB [13].
For several cancer entities, overexpression of NNAT was observed and correlated with loss of methylation of the maternal allele [7]. In glioblastoma multiforme [14], medulloblastoma [8], myxoid liposarcoma [15], and lung cancer [16, 17] high NNAT expression is associated with unfavorable outcome. In contrast, increased promoter methylation and downregulation of NNAT expression was found in childhood leukemia [18]. In the anterior pituitary gland, NNAT is expressed in all secretory cell types. In adenomas derived from these cells, low NNAT expression is associated with benign behavior [19].
In addition to promoter methylation, microRNA 708 has been found to downregulate NNAT expression, which decreases intracellular calcium ions in breast cancer resulting in reduced migration and metastasis [20]. Further evidence for a function of NNAT for calcium regulation comes from embryonal stem cells. In such cells, NNAT promotes the neuronal lineage via calcium signaling [21].
As NNAT is upregulated in several cancer entities and its regulatory miRNA has an effect on breast cancer metastatic potential, we studied whether NNAT expression by immunohistochemistry has prognostic potential for breast cancer patients.
Methods
Study population
For this retrospective analysis, 148 patients with primary invasive mamma carcinoma from the Department of Gynecology of the Otto von Guericke University Magdeburg were selected form a larger study population described earlier [22]. Selection criterion was availability of sufficient paraffin embedded material. These patients were diagnosed with breast cancer between 1999 and 2006 and had a median age of 64.2 years and follow-up for up to 155 months (mean 59 months). This study was approved by the Research and Ethics Committee of Otto von Guericke University, Magdeburg, Germany (AKZ 114/13).
Immunohistochemistry
Paraffin embedded tissue was sectioned (3 μm) and deparaffinized. Epitope retrieval was performed by heat treatment in a pressure cooker for 3 min at 121 °C in citrate buffer (pH 6). The primary antibody used (ab27266, Abcam, Cambridge, UK) was raised against amino acids 51 up to the C-terminus and therefore detects both isoforms of NNAT. Incubation with the primary antibody, diluted 1:100 in antibody dilution buffer (Ventana Medical Systems, Tucson, AZ, USA), was 30 min at room temperature. After three washes with TBST (TRIS/Cl 50 mM, NaCl 150 mM, Tween-20 0.05%, pH 7.4), the sections were incubated with secondary peroxidase conjugated goat-anti-rabbit antibody (DAKO, Hamburg, Germany) for 30 min at room temperature. After another three washes, bound antibody was visualized using diaminobenzindine (DAB, DAKO, Hamburg, Germany) as chromogen. Antibody dilution and incubation conditions were optimized using brain tissue, which also served as positive control. As negative control, the primary antiserum was omitted. Staining of the tumor samples was classified according to intensity (0 = no staining; 1 = weak staining; 2 = intermediate staining, and 3 = intense staining) and the percentage of positive cancer cells. To obtain an immunoreactivity score (IRS), these two parameters were multiplied and the resulting number divided by 10, to result in a score ranging from 0 to 30. For Ki-67 staining, the monoclonal antibody (mib-1) was used according to our standard diagnostic procedures. Ki-67 labeling was scored as 1 for ≤14%, 2 for 14–25%, and 3 for >25% of stained cells [23].
Statistics
All statistical calculations were performed with SPSS version 22 (IBM). To test for correlations between clinicopathological parameters and high or low NNAT score, cross tabulation with Pearson’s Χ2 was applied. To determine the threshold for high and low NNAT score, receiver operator characteristics (ROC) curve analysis was performed. Relapse-free survival (RFS) and overall survival (OS) probability distribution were studied using the Kaplan-Meier method. The equality of survival curves was tested using the log-rank test. DFS was defined as the time between primary diagnosis and disease recurrence of all types as well as breast cancer-specific death. OS was defined as the time between primary diagnosis and death caused by breast cancer. Univariate Cox proportional hazards regression analysis was used to identify significant prognostic factors and then the prognostic significance was evaluated using multivariate analysis. A p value less than 0.05 was considered as statistically significant, less than 0.1 as statistical trend.
Results
Study population
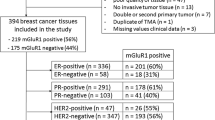
Clinicopathological parameters of our study population, consisting of 148 females, are listed in Table 1. These parameters of our cohort are similar to those of other cohorts published in Germany and Europe, and we therefore regarded ours as a representative cohort.
Neuronatin expression
Comparing NNAT expression in normal and tumor tissue, we found NNAT staining significantly higher in tumor tissue. The staining pattern was cytoplasmic granular, consistent with localization in the cisterns of the endoplasmic reticulum (Fig. 1). In breast parenchyma, the average NNAT IRS was 5.9, while in carcinoma, this was 8.6 (p < 0.001). Receiver operator characteristics curve analysis, on the basis of the survival curves, allowed us to define 14 as the best cutoff value to distinguish between low and high expression. With this IRS, 28% of the tumors showed high expression, but no correlations were found between high NNAT expression and most clinicopathological parameters. Only for the Nottingham prognostic index we found a statistical trend (by Spearman’s correlation analysis) towards higher NNAT expression in high-risk cancers (Table 1). We did not find a correlation with the proliferation marker Ki-67 either (p = 0.767).
Neuronatin immunohistochemistry. a Negative immunostaining (staining intensity = 0), invasive carcinoma of no special type. b Weak immunostaining (staining intensity = 1), invasive carcinoma of no special type. c Moderate immunostaining (staining intensity = 2), invasive carcinoma of no special type. d Strong immunostaining (staining intensity = 3), invasive carcinoma of no special type. e Weak immunostaining (staining intensity = 1), invasive lobular carcinoma. f Moderate immunostaining (staining intensity = 2), mucinous carcinoma. Bar = 50 μm. Insets show higher magnification (40×–objective) to demonstrate the cytoplasmic granular localization of the neuronatin signal
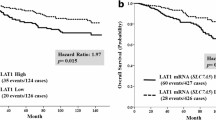
Survival analysis
We then analyzed whether NNAT IRS might be indicative for tumor prognosis. Kaplan-Meier analysis (Fig. 2, Table 2) revealed a significant correlation between high NNAT IRS and shorter relapse-free (log-rank p = 0.003) as well as overall survival (log-rank p < 0.001). In all subgroups analyzed, survival was better in the low NNAT IRS group (Fig. 3). However, for the subgroup of patients with PR-positive, triple negative (TNBC), HER2-positive tumors, and tumors smaller than 2 cm, there was no significant difference in relapse-free survival (by Kaplan-Meier analysis) between NNAT IRS high and low.
Similar results were obtained by univariate Cox regression analysis (Table 3). In addition to NNAT IRS, tumor size was a major prognostic factor in our population. In multivariate Cox regression analysis, NNAT IRS remained as an independent prognostic factor (Table 4).
We finally explored by Kaplan-Meier analysis whether high or low NNAT IRS status was associated with response to chemo- and endocrine therapy (Table 5). A statistically significant association was found between unfavorable relapse-free survival and NNAT IRS high expression, in patients treated with chemotherapy but not endocrine therapy. For tamoxifen-treated patients, there was a statistical trend (p = 0.06), but for patients treated with an aromatase inhibitor, no significant correlation with survival was found. For overall survival, high NNAT IRS was correlated with poor outcome regardless of treatment.
Discussion
Currently, the choice of treatment of breast cancer is based on several morphological and molecular features such as tumor size, presence of lymph node metastasis, and tumor grade, which are represented in the Nottingham prognostic index [24,25,26]. In addition, proliferative activity as reflected in the Ki-67 status [27] and hormone receptor status are important for prognostic stratification. Most patients with a hormone receptor positive breast cancer are treated with anti-endocrine compounds, while those with a HER2/neu positive cancer receive anti-HER2-based therapy and those with a triple negative cancer mostly chemotherapy. In high-risk patients, endocrine and anti-HER-based therapy is combined with chemotherapy. Especially in ER-positive cases, the decision whether chemotherapy should also be applied relies on additional prognostic factors, such as the proliferation index based upon Ki-67 expression [27] or gene expression assays [28]. We evaluated whether NNAT expression might constitute an additional prognostic marker. NNAT IRS was higher in cancer tissue than in non-neoplastic neighboring cells, but this varied between patients. Furthermore, high immunohistochemical expression of NNAT was significantly associated with poor prognosis, both for RFS and OS. This observation fits with the higher Nottingham prognostic index in high NNAT IRS high patients. Only in patients with a small tumor did NNAT IRS not significantly correlate with relapse-free survival. In some groups, this might have been due to the low number of available cases (i.e., TNBC n = 22). In most of these groups, the prognosis as such is relatively good (i.e., PR-positive or small tumor size).
These data suggest that NNAT IRS might be an alternative or supplementary prognostic marker, beyond receptor expression status. This was further corroborated by multivariate analysis, which confirmed that NNAT IRS was an independent risk factor.
We chose to study NNAT because of associations with prognosis in other cancer types [9], and also it has been found to be a target of miRNA-708, which is associated with poor prognosis in breast cancer. As a putative regulator of intracellular calcium, NNAT expression is likely to affect calcium-dependent processes, which include cell migration in the context of metastasis [20]. In our retrospective analysis, NNAT expression correlated with metastasis but not with proliferation as reflected by the Ki-67 labeling index. We had tissue samples available for Ki-67 analysis of only 100 patients, but nonetheless high Ki-67 (>25%) correlated with poor outcome (RFS: p = 0.123; OS: p = 0.009 Kaplan-Meier analysis, log-rank). This suggests that the association of NNAT with poor outcome is not a reflection of a high proliferation rate, but rather of cell migration and metastasis.
Also in other cancer types, established prognostic factors are associated with cellular Ca2+−homeostasis. The G-protein coupled estrogen receptor GPER1 signals via calcium flux, and its downregulation has been associated with breast tumorigenesis [29]. Cav1.3 is a GPER1 regulated calcium channel expressed in breast cancer cells, and its downregulation suppresses tumor growth [30]. The calcium-sensing receptor (CaSR) is involved in interleukin secretion by cancer cells [31], which modifies the inflammatory response. Protein kinase C isoforms also play a major role in breast cancer progression [32]. Finally, S100 Ca-binding proteins, in particular the S100A7 isoform, are involved in breast cancer aggressiveness [33]. Taken together, these data suggest that calcium signaling is an important factor in tumor biology.
In conclusion, the data obtained in our study population show that NNAT expression by immunohistochemistry might be an independent prognostic marker for breast cancer. Our data are based on a small number of patients and need confirmation in an independent larger patient cohort. Therefore, further prospective studies with more patients are needed to explore whether the NNAT IRS might be relevant in clinical practice.
References
Evans HK, Wylie AA, Murphy SK, Jirtle RL (2001) The neuronatin gene resides in a “micro-imprinted” domain on human chromosome 20q11.2. Genomics 77:99–104. doi:10.1006/geno.2001.6612
John RM, Aparicio SA, Ainscough JF et al (2001) Imprinted expression of neuronatin from modified BAC transgenes reveals regulation by distinct and distant enhancers. Dev Biol 236:387–399. doi:10.1006/dbio.2001.0327
Wijnholds J, Chowdhury K, Wehr R, Gruss P (1995) Segment-specific expression of the neuronatin gene during early hindbrain development. Dev Biol 171:73–84. doi:10.1006/dbio.1995.1261
Sel S, Patzel E, Poggi L et al (2017) Temporal and spatial expression pattern of Nnat during mouse eye development. Gene Expr Patterns 23–24:7–12. doi:10.1016/j.gep.2016.12.002
Usui H, Morii K, Tanaka R et al (1997) cDNA cloning and mRNA expression analysis of the human neuronatin. High level expression in human pituitary gland and pituitary adenomas. J Mol Neurosci MN 9:55–60. doi:10.1007/BF02789395
Joseph R, Dou D, Tsang W (1994) Molecular cloning of a novel mRNA (neuronatin) that is highly expressed in neonatal mammalian brain. Biochem Biophys Res Commun 201:1227–1234
Joseph RM (2014) Neuronatin gene: imprinted and misfolded: studies in Lafora disease, diabetes and cancer may implicate NNAT-aggregates as a common downstream participant in neuronal loss. Genomics 103:183–188. doi:10.1016/j.ygeno.2013.12.001
Siu I-M, Bai R, Gallia GL et al (2008) Coexpression of neuronatin splice forms promotes medulloblastoma growth. Neuro-Oncology 10:716–724. doi:10.1215/15228517-2008-038
Pitale PM, Howse W, Gorbatyuk M (2017) Neuronatin protein in health and disease. J cell Physiol 232:477–48.1. doi:10.1002/jcp.25498
Chu K, Tsai M-J (2005) Neuronatin, a downstream target of BETA2/NeuroD1 in the pancreas, is involved in glucose-mediated insulin secretion. Diabetes 54:1064–1073
Joe MK, Lee HJ, Suh YH et al (2008) Crucial roles of neuronatin in insulin secretion and high glucose-induced apoptosis in pancreatic beta-cells. Cell Signal 20:907–915. doi:10.1016/j.cellsig.2008.01.005
Mzhavia N, Yu S, Ikeda S et al (2008) Neuronatin: a new inflammation gene expressed on the aortic endothelium of diabetic mice. Diabetes 57:2774–2783. doi:10.2337/db07-1746
Suh YH, Kim WH, Moon C et al (2005) Ectopic expression of Neuronatin potentiates adipogenesis through enhanced phosphorylation of cAMP-response element-binding protein in 3T3-L1 cells. Biochem Biophys Res Commun 337:481–489. doi:10.1016/j.bbrc.2005.09.078
Xu DS, Yang C, Proescholdt M et al (2012) Neuronatin in a subset of glioblastoma multiforme tumor progenitor cells is associated with increased cell proliferation and shorter patient survival. PLoS One 7:e37811. doi:10.1371/journal.pone.0037811
Renner M, Wolf T, Meyer H et al (2013) Integrative DNA methylation and gene expression analysis in high-grade soft tissue sarcomas. Genome Biol 14:r137. doi:10.1186/gb-2013-14-12-r137
Uchihara T, Okubo C, Tanaka R et al (2007) Neuronatin expression and its clinicopathological significance in pulmonary non-small cell carcinoma. J Thorac Oncol Off Publ Int Assoc Study Lung Cancer 2:796–801. doi:10.1097/JTO.0b013e318145af5e
Okubo C, Minami Y, Tanaka R et al (2006) Analysis of differentially expressed genes in neuroendocrine carcinomas of the lung. J Thorac Oncol 1:780–786. doi:10.1016/S1556-0864(15)30406-8
Kuerbitz SJ, Pahys J, Wilson A et al (2002) Hypermethylation of the imprinted NNAT locus occurs frequently in pediatric acute leukemia. Carcinogenesis 23:559–564
Revill K, Dudley KJ, Clayton RN et al (2009) Loss of neuronatin expression is associated with promoter hypermethylation in pituitary adenoma. Endocr Relat Cancer 16:537–548. doi:10.1677/ERC-09-0008
Ryu S, McDonnell K, Choi H et al (2013) Suppression of miRNA-708 by polycomb group promotes metastases by calcium-induced cell migration. Cancer Cell 23:63–76. doi:10.1016/j.ccr.2012.11.019
Lin H-H, Bell E, Uwanogho D et al (2010) Neuronatin promotes neural lineage in ESCs via Ca(2+) signaling. Stem Cells Dayt Ohio 28:1950–1960. doi:10.1002/stem.530
Ignatov A, Ignatov T, Weissenborn C et al (2011) G-protein-coupled estrogen receptor GPR30 and tamoxifen resistance in breast cancer. Breast Cancer Res Treat 128:457–466. doi:10.1007/s10549-011-1584-1
Duffy MJ, Harbeck N, Nap M et al (2017) Clinical use of biomarkers in breast cancer: updated guidelines from the European Group on Tumor Markers (EGTM). Eur J Cancer Oxf Engl 75:284–298. doi:10.1016/j.ejca.2017.01.017
Haybittle JL, Blamey RW, Elston CW et al (1982) A prognostic index in primary breast cancer. Br J Cancer 45:361–366
Todd JH, Dowle C, Williams MR et al (1987) Confirmation of a prognostic index in primary breast cancer. Br J Cancer 56:489–492
Galea MH, Blamey RW, Elston CE, Ellis IO (1992) The Nottingham prognostic index in primary breast cancer. Breast Cancer Res Treat 22:207–219
Denkert C, Budczies J, von Minckwitz G et al (2015) Strategies for developing Ki-67 as a useful biomarker in breast cancer. Breast Edinb Scotl 24(Suppl 2):S67–S72. doi:10.1016/j.breast.2015.07.017
Buus R, Sestak I, Kronenwett R et al (2016) Comparison of EndoPredict and EPclin with oncotype DX recurrence score for prediction of risk of distant recurrence after endocrine therapy. J Natl Cancer Inst. doi:10.1093/jnci/djw149
Ignatov T, Weißenborn C, Poehlmann A et al (2013) GPER-1 expression decreases during breast cancer tumorigenesis. Cancer Investig 31:309–315. doi:10.3109/07357907.2013.789901
Ji Y, Han Z, Shao L, Zhao Y (2016) Ultrasound-targeted microbubble destruction of calcium channel subunit α 1D siRNA inhibits breast cancer via G protein-coupled receptor 30. Oncol Rep 36:1886–1892. doi:10.3892/or.2016.5031
Hernández-Bedolla MA, González-Domínguez E, Zavala-Barrera C et al (2016) Calcium-sensing-receptor (CaSR) controls IL-6 secretion in metastatic breast cancer MDA-MB-231 cells by a dual mechanism revealed by agonist and inverse-agonist modulators. Mol Cell Endocrinol 436:159–168. doi:10.1016/j.mce.2016.07.038
Urtreger AJ, Kazanietz MG, Bal de Kier Joffé ED (2012) Contribution of individual PKC isoforms to breast cancer progression. IUBMB Life 64:18–26. doi:10.1002/iub.574
Emberley ED, Murphy LC, Watson PH (2004) S100A7 and the progression of breast cancer. Breast Cancer Res 6:153–159. doi:10.1186/bcr816
Acknowledgments
Parts of this study have been supported by a grant of the Deutsche Forschungsgemeinschaft (DFG) to T.K. (KA2663/3-1). Professional assistance of our immunohistological laboratory, especially Carola Kügler, Claudia Miethke, and Nadine Wiest, is greatly appreciated.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by a grant of the Deutsche Forschungsgemeinschaft (DFG) to T.K. (KA2663/3-1).
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Nass, N., Walter, S., Jechorek, D. et al. High neuronatin (NNAT) expression is associated with poor outcome in breast cancer. Virchows Arch 471, 23–30 (2017). https://doi.org/10.1007/s00428-017-2154-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-017-2154-7