Abstract
Lymphatic invasion (LI) and venous invasion (VI) are regarded as important risk factors of nodal disease in early-stage colorectal cancer (CRC) but with variable reporting and poor distinction of these parameters in previous studies. This study examines the application of a double immunohistochemistry (D-IHC) method to help detect and distinguish LI and VI, in comparison with haematoxylin and eosin (H&E) staining, in a clinical series of cases of stage pT1 CRC. The aims were to demonstrate feasibility of this methodology in routine practice and compare rates of LI and VI reporting with and without D-IHC application. D-IHC utilising CAM5.2 with the endothelial marker CD34 and with the specific lymphatic endothelial marker D2-40 was performed on parallel sections from single representative paraffin tissue blocks in 28 cases of stage pT1 CRC from routine clinical practice. D-IHC significantly increased rates of both LI and VI reporting, from 14.3 to 35.7 % and from 14.3 to 28.6 %, respectively. The D-IHC methodology described is technically feasible in routine practice and potentially offers a more sensitive and robust assay for detection and distinction of LI and VI in early CRC pathology reporting. The reproducibility and clinical significance of enhanced LI and VI detection by this method and the relative importance of LI and VI in this clinical setting require further study.
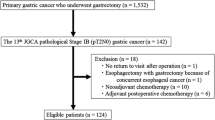
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The introduction of screening programmes to detect colorectal cancer (CRC) has resulted in an increased number of early-stage cancers [1]. Many of these early-stage cancers are detected within polyps, but the evidence base for the subsequent management of malignant polyps is poor and based largely on data derived from symptomatic patients [2]. Notwithstanding this, local excision is now deemed a safe and effective treatment for many such early-stage CRCs and is associated with significantly less morbidity and mortality compared with surgical intervention [3–5]. Local excision is generally considered acceptable only for stage pT1 CRC as more advanced cancers are associated with an unacceptable recurrence rate and reduced survival [5, 6].
However, stage pT1 tumours have some risk of regional lymph node metastatic disease (LNM), considered between 8 and 17 % overall, and this is not evaluated in local resection specimens, as regional lymph nodes are not removed [7–11]. Thus, some patients with stage pT1 CRC treated by polypectomy alone are at low but significant risk of residual disease in regional nodes, potentially curative by surgery. Management must balance the risks of surgical intervention against LNM, and this has long been a clinicopathological challenge, the ideal being to offer surgery to those perceived to be at considerable risk of LNM and avoid surgery in those with minimal risk [12, 13].
Histopathological features of the primary tumour may indicate risk of aggressive behaviour, including LNM, with traditional features considered the most predictive of adverse outcome being depth of invasion, poor differentiation, lymphovascular invasion (LVI) and completeness of excision [12–15]. There has been considerable focus on methods of evaluation of depth of tumour invasion [16–18]. More recent studies have examined other primary tumour features possibly predictive of LNM [18–21]. Two recent meta-analyses found that lymphatic invasion (LI) was a strong histological predictor of LNM, and in one study, by Bosch et al., LI was found to be the single morphological feature most predictive of LNM [22, 23]. Both meta-analyses found LI to be significantly more powerful than venous invasion (VI) in predicting LNM.
Developments in immunohistochemistry have now made possible robust distinction between LI and VI, difficult on haematoxylin and eosin (H&E)-stained sections alone. As this may be an important issue in the routine evaluation of polypectomy specimens demonstrating stage pT1 CRC, it formed the basis of this study. LI and VI detection rates were evaluated in a series of cases of stage pT1 CRC, on routine H&E-stained sections and independently on immunohistochemistry, utilising a double immunohistochemistry (D-IHC) detection method to distinguish LI and VI. The epithelial antibodies CAM5.2 and D2-40, which stain lymphatic but not venous endothelium, were applied to the same tissue section and similarly CAM5.2 and CD34, which stains venous endothelium strongly and lymphatic endothelium weakly or negatively, the comparison in parallel sections allowing distinction between LI and VI [24, 25]. The main study aims were to demonstrate feasibility of this methodology in routine practice and compare rates of LI and VI reporting with and without D-IHC application.
Materials and methods
Twenty-eight cases of stage pT1 CRC within local excision specimens were identified within routine pathology practice in the Royal Victoria Hospital, Belfast Trust, over a 2-year period (2012 and 2014). All were polypectomy specimens; 25 removed intact and three removed piecemeal. These included both symptomatic and screen-detected cases. No cases received neoadjuvant therapy. Few cases had follow-up surgical resection, and therefore, it was not possible to evaluate clinical significance of study findings regarding prediction of LNM. Routine laboratory practice for the duration of the study involved submission of the entire specimen for processing, keeping any polyp stalk intact where possible, and examination of all blocks through at least three H&E-stained levels.
H&E-stained sections were examined by two pathologists (MBL and AJE) to evaluate for LI and VI independently, without knowledge of immunohistochemistry. For the purposes of this study arm, LI was defined as the presence of one or more tumour cells within an endothelial-lined space containing few or no red blood cells. VI was defined as one or more tumour cells within an endothelial-lined space with either abundant red blood cells in the lumen or a surrounding muscular wall. Consensus was reached on double-headed microscopy review for any cases with initial disagreement.
Double immunohistochemistry
A single representative paraffin block from each case was selected for application of D-IHC. Sequential double immunohistochemical staining was performed on a BOND III Immunostainer (Leica Microsystems) using a Bond Polymer Refine detection kit (DS9800) as the first stain and Bond Polymer Refine Red detection kit (DS9390) as the second stain. D2-40 (Dako M3619) was used at a dilution of 1:100 and retrieved in ER1 (AR9961) for 30 min. CD34 (Leica PA0212) is a ready to use antibody and was retrieved in ER2 (AR9640) for 20 min. CAM5.2 (BD 920005) was used at a dilution of 1:20 and retrieved in ER2 for 20 min. D2-40 and CD34 were visualised with DAB chromogen, and CAM5.2 was visualised with Fast Red chromogen.
D-IHC was evaluated by two pathologists (MBL and AJE) without knowledge of the H&E classification for LI and VI status. For the purposes of this study arm, LI was immunohistochemically defined as the presence of one or more CAM5.2-positive tumour cells within the lumen of a vessel showing complete circumferential staining for D2-40. VI was immunohistochemically defined as the presence of one or more CAM5.2-positive tumour cells within the lumen of a vessel showing complete circumferential staining for CD34 but weak or negative staining for D2-40 (on parallel sections). Consensus was reached on double-headed microscopy review for any cases with initial disagreement. Because of the small study numbers, reproducibility was not formally examined.
Results
Table 1 demonstrates the baseline clinicopathological features of the 28 study cases. Of the participants, 22 (78.6 %) were male. By far, the most common location was the sigmoid colon, accounting for 19 (67.9 %) of the cases. Most of the measurable polypectomy specimens harbouring cancers were in the 10–20 mm in size range, although interestingly, seven of 25 (28 %) measured less than 10 mm in diameter (overall polypectomy specimen size).
Venous or lymphatic invasion (lymphovascular invasion, LVI) was recorded in six of the 28 cases (21.4 %) by H&E examination alone (Table 2). Of these, two were classified as VI only, two as LI only and two as demonstrating both VI and LI. In each of these six cases, these findings were also recorded independently on D-IHC evaluation. No case demonstrated VI or LI on H&E which was undetected by D-IHC. In one case, where only LI was detected on H&E, VI was also identified after CAM5.2/CD34 D-IHC. D-IHC also identified either VI or LI, or both, in a further eight cases, which had not been detected on H&E, one showing both VI and LI, two showing VI only and five showing LI only (Tables 2, 3 and 4).
In summary, lymphatic or venous invasion was detected in six cases (21.4 %) by H&E but in 14 cases (50 %) where D-IHC was employed. Venous invasion was detected in four (14.3 %) cases on H&E and eight (28.6 %) cases on D-IHC (CAM5.2/CD34), and lymphatic invasion was detected in four (14.3 %) cases on H&E and in ten (35.7 %) cases on D-IHC (CAM5.2/D2-40).
Discussion
Many studies have reported LI and VI as adverse features in stage pT1 CRC predictive of LNM. Most such studies do not distinguish LI from VI, rather grouping together as “lymphovascular invasion” (LVI). Those that do distinguish between LI and VI rarely provide definitions of these terms and where presented; the definitions vary, making the comparison between studies difficult. The most consistently utilised definitions describe LI as tumour cells within an endothelial-lined space containing few or no red blood cells and VI as tumour cells within an endothelial-lined space with either red blood cells in the lumen or a surrounding muscular wall [21, 26]. However, red blood cells are not uncommonly seen in significant number apparently lying in lymphatic channels, and small venules typically lack a muscular wall, so these definitions, whilst pragmatic, have limitations in application. Using morphological features alone, it may sometimes be impossible to confidently designate a thin-walled submucosal vessel as lymphatic or venous in nature.
The idea of using immunohistochemistry to facilitate detection of LI and VI in early-stage CRC is not novel. Early attempts using antibodies against factor VIII and the lectin Ulex Europaeus I were largely unsuccessful [27]. More recent studies applying single-marker immunostains, including CD34 and D2-40 antibodies, have been more successful [18, 28, 29]. Some have compared detection rates with H&E evaluation, and most of these studies have reported enhanced detection using immunohistochemistry [30–33]. Importantly, a recent meta-analysis of 23 studies involving 4510 patients showed LI (odds ratio (OR) 7.66, 95 % confidence interval (CI) 4.73–12.39) to be a stronger predictor of LMN in stage pT1 than VI (OR 4.03, 95 % CI 2.60–6.25) [23]. Similar results were found in another meta-analysis which concluded that LI was the single most powerful histological predictor of LNM in stage pT1 CRC (relative risk ratio (RR) 5.2, 95 % CI 4.0–6.8) [22]. VI was considered a much weaker predictor (RR 2.2, 95 % CI 1.4–3.2 [22]. As such, it was concluded that separate reporting of LI and VI was recommended.
In this study, we have evaluated a series of 28 stage pT1 CRCs, comparing rates of detection of LI and VI on routine H&E examination with those found on applying D-IHC combining the epithelial marker CAM5.2 with the endothelial markers D2-40 and CD34 on parallel sections. A similar D-IHC technique using a cytokeratin marker and CD31 has been applied previously in the setting of endometrial cancer within hysterectomy specimens to enhance detection of lymphovascular invasion [24]. To the best of our knowledge, this technique has not been applied before to CRC specimens.
We demonstrated that D-IHC is technically feasible and can easily be embedded into routine laboratory practice, once the methodology is optimised, particularly with respect to appropriate antigen retrieval. Compared to H&E evaluation, we found that D-IHC increased the detection of VI from 14.3 to 28.6 % of the cases and the detection of LI from 14.3 to 35.7 %. These findings are comparable to those from previous studies employing single-marker endothelial immunostains [30–32]. Higher overall detection rates for LI and VI in this study are to be expected given the heightened sensitivity afforded by the application of a cytokeratin marker to detect small clusters or single tumour cells within small lymphatic or venous channels. We detected foci of single-cell LI and VI which we consider would have been essentially undetectable on H&E examination (Fig. 1e, h). We did not compare detection rates of LI and VI with and without use of the CAM5.2 “counterstain” i.e., single versus double immunohistochemistry, but suggest that, whereas single-stain immunohistochemistry is likely to detect most LI and VI, detection of such single-cell LI and VI is likely to be enhanced by D-IHC. This requires further study.
a Pedunculated stage pT1 colorectal cancer (CRC), Haggitt level 2, arising within a tubulovillous adenoma (haematoxylin & eosin, H&E). b High power of shaded area from (a), demonstrating obvious tumour lymphatic invasion (LI) (H&E). c D2-40 single marker immunohistochemistry on parallel section to (a/b), demonstrating positive staining of lymphatic endothelial cells but negative staining of blood vessel endothelial cells, confirming LI rather than venous invasion (VI) (immunoperoxidase). d High-power view of early-stage CRC, with differential diagnosis of LI versus retraction artefact (H&E). e CAM5.2/D2-40 double immunohistochemistry (D-IHC) on parallel section to (d), revealing foci of LI, allowing confident distinction from retraction artefact. f Similar field from a different case of early-stage CRC, with CAM5.2/D2-40 D-IHC suggesting retraction artefact and “tumour budding” rather than LI. g Pedunculated stage pT1 CRC demonstrating VI within the stalk, obvious on low-power examination (H&E). h CAM5.2/CD34 D-IHC on parallel section to (g), from shaded area, confirming VI, with CAM5.2 staining tumour epithelial cells and CD34 staining venous endothelial cells. h (inset) More subtle focus of venular invasion from same case, evident only on CAM5.2/CD34 D-IHC, a CAM5.2-positive tumour cell lying within a channel containing red blood cells and surrounding strongly CD34-positive endothelial lining (D2-40 negative, not shown) (immunoperoxidase)
A further potential advantage of immunostaining in this setting is that cases considered to have LI or VI on H&E examination may be revealed instead as retraction artefact on immunostaining. Indeed, the difficulty in distinguishing retraction artefact from true LI or VI on H&E has long been an issue and the application of immunohistochemistry has been suggested as a potential solution [34]. There were no such cases reported in this study, most likely reflecting awareness of this mimicry and a high threshold for reporting LI or VI on H&E examination. The problem of overcalling retraction artefact as LI is well reported in other studies and can result in significant interobserver variation [35, 36]. Indeed, in the past, this has led to at least one distinguished pathology unit to advocate no reporting of the presence or absence of LI [13, 37]. This overcalling of retraction artefact as LI is the likely explanation for a significantly lower detection rate of LI in D2-40 stained sections (32.3 %) over H&E-stained sections (39.5 %), in one study by Suzuki et al. of early stage CRC [29]. This study also demonstrated higher interobserver agreement with D2-40 evaluation compared to H&E evaluation (kappa values 0.56 and 0.30, respectively). Others have studied interobserver variability specifically and have concluded that the application of immunohistochemistry (single) increased the detection of small vessel invasion (either LI or VI) but did not significantly improve the interobserver agreement (kappa values: H&E—0.28, CD31—0.26, D2-40—0.32) [33]. This study, however, did not agree amongst the study pathologists criteria for defining LI or VI, and H&E sections were not available alongside immunostains during case evaluation, two factors likely to influence agreement. Although we did not formally examine intraobserver or interobserver reproducibility of LI and VI detection given the small study numbers, we consider that D-IHC offers a more robust and reproducible diagnosis of LI or VI than H&E or single immunohistochemistry, particularly in the distinction of single-cell invasion of small vessels from tumour “budding” or retraction artefact. Formal reproducibility studies are required in this regard.
Barresi et al. evaluated LI by D2-40 single-marker immunohistochemistry in 82 cases of stage 1 surgically resected CRC; 29 of which underwent disease progression. VI was not examined. This study found a positive correlation between LI and the presence of regional lymph node micrometastases and also disease progression. Notably, 21 of 29 cases undergoing disease progression demonstrated LI compared to only two of 53 cases without disease progression. D2-40 IHC increased detection of LI over H&E evaluation, from 18 to 23 cases (out of the total of 82 cases). LI detected by D2-40 immunohistochemistry may therefore represent an adverse prognostic factor even in the absence of overt regional lymph node metastases and could select patients who might benefit from adjuvant therapy. This study did not examine the association of LI and overt LNM (stage pN1+ disease). These results suggest a potential prognostic role for LI in polypectomy specimens demonstrating pT1 CRC beyond prediction of regional LNM.
The role of Elastica van Gieson (EVG) staining to enhance detection of VI in early stage CRC is well established [18, 29]. Although meta-analysis has suggested VI is a much weaker predictor of LNM than LI, some studies of stage pT1 CRC have found VI, enhanced by EVG staining, to be a strong predictor of both LNM and distant metastatic disease [22, 29]. In our study, CAM5.2/CD34 D-IHC generally detected smaller calibre VI than that typically detected by EVG (Fig. 1h). CAM5.2/CD34 D-IHC generally adds little to the detection of tumour invasion within large calibre veins, although we have occasionally found CD34 immunohistochemistry useful in cases where tumour completely occludes the vein lumen, mimicking a rounded discontinuous tumour deposit or “satellite”. Identification of a CD34-positive endothelial lining confirms designation as VI, although EVG may be equally, or more, useful in this situation. Thus, histochemical and immunohistochemical techniques may be complementary in the detection of VI. Further studies are required to clarify the relative predictive roles of VI and LI and the clinical significance of subtle invasion of small venules by single tumour cells, detected on immunohistochemistry alone.
In conclusion, although this study is limited by its respective nature and small numbers, it suggests D-IHC employing epithelial and endothelial markers may offer a routine, sensitive and accurate method of detecting and distinguishing LI and VI. This is of particular relevance to early-stage CRC but of potential clinical application to a wide range of other cancers. The clinical significance of LI and VI detected in early-stage CRC by this method remains to be more fully understood and has not been examined by this study. Such an investigation would statistically require large numbers of cases of CRC with early local stage (pT1) but adverse outcome in the form of regional LNM, distant metastases or recurrence. These cases are relatively rare but important because they offer the opportunity to study primary tumour features which predict adverse outcome, providing much needed evidence for the appropriate management of “malignant polyps”. Such a study would be best conducted in the setting of CRC screening, which generates relatively large numbers of cases of early-stage CRC associated with high-quality routine pathology practice.
References
Ellul P, Fogden E, Simpson CL, Nickerson CLR, McKaig BC, Swarbrick ET, Veitch AM (2010) Downstaging of colorectal cancer by the national bowel cancer screening programme in England: first round data from the first centre. Color Dis 12:420–422
Williams JG, Pullan RD, Hill J, Horgan PG, Salmo E, Buchanan GN, Rasheed S, McGee SG, Haboubi N (2013) Management of the malignant colorectal polyp: ACPGBI position statement. Color Dis 15(Suppl 2):1–38
Winde G, Nottberg H, Keller R, Schmid KW, Bünte H (1996) Surgical cure for early rectal carcinomas (T1). Transanal endoscopic microsurgery vs. anterior resection. Dis Colon Rectum 39:969–976
Langer C, Liersch T, Süss M, Siemer A, Markus P, Ghadimi BM, Füzesi L, Becker H (2003) Surgical cure for early rectal carcinoma and large adenoma: transanal endoscopic microsurgery (using ultrasound or electrosurgery) compared to conventional local and radical resection. Int J Color Dis 18:222–229
Wu Y, Wu Y-Y, Li S, Zhu B-S, Zhao K, Yang X-D, Xing CG (2011) TEM and conventional rectal surgery for T1 rectal cancer: a meta-analysis. Hepato-Gastroenterology 58:364–368
Mellgren A, Sirivongs P, Rothenberger DA, Madoff RD, García-Aguilar J (2000) Is local excision adequate therapy for early rectal cancer? Dis Colon Rectum 43:1064–1071, Discussion 1071–4
Tanaka S, Haruma K, Teixeira CR, Tatsuta S, Ohtsu N, Hiraga Y, Yoshihara M, Sumii K, Kajiyama G, Shimamoto F (1995) Endoscopic treatment of submucosal invasive colorectal carcinoma with special reference to risk factors for lymph node metastasis. J Gastroenterol 30:710–717
Kobayashi H, Mochizuki H, Morita T et al (2011) Characteristics of recurrence after curative resection for T1 colorectal cancer: Japanese multicenter study. J Gastroenterol 46:203–211
Coverlizza S, Risio M, Ferrari A, Fenoglio-Preiser CM, Rossini FP (1989) Colorectal adenomas containing invasive carcinoma. Pathologic assessment of lymph node metastatic potential. Cancer 64:1937–1947
Kitamura K, Taniguchi H, Yamaguchi T, Sawai K, Takahashi T (1997) Clinical outcome of surgical treatment for invasive early colorectal cancer in Japan. Hepato-Gastroenterology 44:108–115
Son HJ, Song SY, Lee WY, Yang SS, Park SH, Yang MH, Yoon SH, Chun HK (2008) Characteristics of early colorectal carcinoma with lymph node metastatic disease. Hepato-Gastroenterology 55:1293–1297
Cooper HS (1983) Surgical pathology of endoscopically removed malignant polyps of the colon and rectum. Am J Surg Pathol 7:613–623
Morson BC, Whiteway JE, Jones EA, Macrae FA, Williams CB (1984) Histopathology and prognosis of malignant colorectal polyps treated by endoscopic polypectomy. Gut 25:437–444
Hassan C, Zullo A, Risio M, Rossini FP, Morini S (2005) Histologic risk factors and clinical outcome in colorectal malignant polyp: a pooled-data analysis. Dis Colon Rectum 48:1588–1596
Vieth M, Quirke P, Lambert R, von Karsa L, Risio M (2011) Annex to Quirke et al. quality assurance in pathology in colorectal cancer screening and diagnosis: annotations of colorectal lesions. Virchows Arch 458:21–30
Haggitt RC, Glotzbach RE, Soffer EE, Wruble LD (1985) Prognostic factors in colorectal carcinomas arising in adenomas: implications for lesions removed by endoscopic polypectomy. Gastroenterology 89:328–336
Kikuchi R, Takano M, Takagi K, Fujimoto N, Nozaki R, Fujiyoshi T, Uchida Y (1995) Management of early invasive colorectal cancer. Risk of recurrence and clinical guidelines. Dis Colon Rectum 38:1286–1295
Ueno H, Mochizuki H, Hashiguchi Y et al (2004) Risk factors for an adverse outcome in early invasive colorectal carcinoma. Gastroenterology 127:385–394
Egashira Y, Yoshida T, Hirata I, Hamamoto N, Akutagawa H, Takeshita A, Noda N, Kurisu Y, Shibayama Y (2004) Analysis of pathological risk factors for lymph node metastasis of submucosal invasive colon cancer. Mod Pathol 17:503–511
Ishikawa Y, Akishima-Fukasawa Y, Ito K, Akasaka Y, Yokoo T, Ishii T (2008) Histopathologic determinants of regional lymph node metastasis in early colorectal cancer. Cancer 112:924–933
Wang H-S, Liang W-Y, Lin T-C, Chen W-S, Jiang J-K, Yang S-H, Chang S-C, Lin J-K (2005) Curative resection of T1 colorectal carcinoma: risk of lymph node metastasis and long-term prognosis. Dis Colon Rectum 48:1182–1192
Bosch SL, Teerenstra S, de Wilt JHW, Cunningham C, Nagtegaal ID (2013) Predicting lymph node metastasis in pT1 colorectal cancer: a systematic review of risk factors providing rationale for therapy decisions. Endoscopy 45:827–841
Beaton C, Twine CP, Williams GL, Radcliffe AG (2013) Systematic review and meta-analysis of histopathological factors influencing the risk of lymph node metastasis in early colorectal cancer. Color Dis 15:788–797
Alexander-Sefre F, Singh N, Ayhan A, Salveson HB, Wilbanks G, Jacobs IJ (2003) Detection of tumour lymphovascular space invasion using dual cytokeratin and CD31 immunohistochemistry. J Clin Pathol 56:786–788
Kahn HJ, Marks A (2002) A new monoclonal antibody, D2-40, for detection of lymphatic invasion in primary tumors. Lab Investig 82:1255–1257
Tsuruta O, Tsuji Y, Kawano H et al (2000) Indication for endoscopic resection of submucosal colorectal carcinoma: special reference to lymph node metastasis. Diagn Ther Endosc 6:101–109
Muller S, Chesner IM, Egan MJ, Rowlands DC, Collard MJ, Swarbrick ET, Newman J (1989) Significance of venous and lymphatic invasion in malignant polyps of the colon and rectum. Gut 30:1385–1391
Ishii M, Ota M, Saito S, Kinugasa Y, Akamoto S, Ito I (2009) Lymphatic vessel invasion detected by monoclonal antibody D2-40 as a predictor of lymph node metastasis in T1 colorectal cancer. Int J Color Dis 24:1069–1074
Suzuki A, Togashi K, Nokubi M, Koinuma K, Miyakura Y, Horie H, Lefor AT, Yasuda Y (2009) Evaluation of venous invasion by Elastica van Gieson stain and tumor budding predicts local and distant metastases in patients with T1 stage colorectal cancer. Am J Surg Pathol 33:1601–1607
Saad RS, Kordunsky L, Liu YL, Denning KL, Kandil HA, Silverman JF (2006) Lymphatic microvessel density as prognostic marker in colorectal cancer. Mod Pathol 19:1317–1323
Walgenbach-Bruenagel G, Tolba RH, Varnai AD, Bollmann M, Hirner A, Walgenbach KJ (2006) Detection of lymphatic invasion in early stage primary colorectal cancer with the monoclonal antibody D2-40. Eur Surg Res 38:438–444
Barresi V, Reggiani Bonetti L, Vitarelli E, Di Gregorio C, Ponz de Leon M, Barresi G (2012) Immunohistochemical assessment of lymphovascular invasion in stage I colorectal carcinoma: prognostic relevance and correlation with nodal micrometastases. Am J Surg Pathol 36:66–72
Harris EI, Lewin DN, Wang HL, Lauwers GY, Srivastava A, Shyr Y, Shakhtour B, Revetta F, Washington MK (2008) Lymphovascular invasion in colorectal cancer: an interobserver variability study. Am J Surg Pathol 32:1816–1821
Quirke P, Risio M, Lambert R, von Karsa L, Vieth M (2011) Quality assurance in pathology in colorectal cancer screening and diagnosis—European recommendations. Virchows Arch 458:1–19
Volk EE, Goldblum JR, Petras RE, Carey WD, Fazio VW (1995) Management and outcome of patients with invasive carcinoma arising in colorectal polyps. Gastroenterology 109:1801–1807
Geraghty JM, Williams CB, Talbot IC (1991) Malignant colorectal polyps: venous invasion and successful treatment by endoscopic polypectomy. Gut 32:774–778
Williams CB, Geraghty JM (1990) The malignant polyp—when to operate: the St. Mark’s experience. Can J Gastroenterol 4:549–553
Acknowledgments
M.B. Loughrey was responsible for the study design, performed the research and analysed the data. A.J. Ervine performed the research and analysed the data. H.A. McBride optimised and performed the immunohistochemistry. All authors contributed to manuscript writing, editing and proof reading.
Conflict of interest
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ervine, A.J., McBride, H.A., Kelly, P.J. et al. Double immunohistochemistry enhances detection of lymphatic and venous invasion in early-stage colorectal cancer. Virchows Arch 467, 265–271 (2015). https://doi.org/10.1007/s00428-015-1792-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-015-1792-x