Abstract
Autophagy and mitophagy are important for training-inducible muscle adaptations, yet it remains unclear how these systems are regulated throughout the adaptation process. Here, we studied autophagic and mitophagic flux in the skeletal muscles of Sprague–Dawley rats (300–500 g) exposed to chronic contractile activity (CCA; 3 h/day, 9 V, 10 Hz continuous, 0.1 ms pulse duration) for 1, 2, 5, and 7 days (N = 6–8/group). In order to determine the flux rates, colchicine (COL; 0.4 mg/ml/kg) was injected 48 h before tissue collection, and we evaluated differences of autophagosomal protein abundances (LC3-II and p62) between colchicine- and saline-injected animals. We confirmed that CCA resulted in mitochondrial adaptations, including improved state 3 respiration as early as day 1 in permeabilized muscle fibers, as well significant increases in mitochondrial respiratory capacity and marker proteins in IMF mitochondria by day 7. Mitophagic and autophagic flux (LC3-II and p62) were significantly decreased in skeletal muscle following 7 days of CCA. Notably, the mitophagic system seemed to be downregulated prior (day 3–5) to changes in autophagic flux (day 7), suggesting enhanced sensitivity of mitophagy compared to autophagy with chronic muscle contraction. Although we detected no significant change in the nuclear translocation of TFEB, a regulator of lysosomal biogenesis, CCA increased total TFEB protein, as well as LAMP1, in skeletal muscle. Thus, chronic muscle activity reduces mitophagy in parallel with improved mitochondrial function, and this is supported by enhanced lysosomal degradation capacity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Skeletal muscle adapts to exercise training via structural and biochemical alterations. These training-inducible adaptations include an increased oxidative capacity, which is ultimately attributed to enhanced mitochondrial biogenesis and content [10]. However, a growing number of studies have suggested an important role for mitochondrial turnover in the adaptations associated with chronic muscle use, including a branch of the autophagic pathway devoted to mitochondrial degradation, termed mitophagy [11, 31].
During autophagy, intracellular components are engulfed in a double membrane autophagosome and transported to the lysosome for subsequent degradation by lysosomal enzymes. Damaged or dysfunctional mitochondria, featuring a loss of membrane potential (Δψ), can be polyubiquitinated on outer membrane proteins by Parkin, an E3-ubiquitin ligase. These ubiquitin structures are then conjugated by the adaptor protein, p62, to the microtubule-associated protein 1 light chain 3-II (LC3-II), which is embedded in a phagophore membrane. After being completely encircled by a double-membrane, the resulting autophagosome-containing mitochondria are delivered to lysosomes, resulting in a formation of an autolysosome, where degradation will occur.
Exercise training and chronic muscle activity have been shown to modify the regulation of autophagy and mitophagy, thereby promoting muscle and mitochondrial adaptations [4, 25, 31]. Based on previous results which demonstrated a downregulation of the ratio of LC3-II to LC3-I, as well as reduced p62 levels, it has been conjectured that exercise training may upregulate muscle autophagic/mitophagic flux rates, likely due to accelerated autophagosomal degradation [14, 22]. However, these results may also be interpreted as slowed autophagosome formation and/or reduced p62 synthesis. In contrast to these findings, other studies have observed elevated autophagic/mitophagic markers in skeletal muscle following exercise training which the authors interpreted as an indication of increased autophagy flux [28]. These discrepancies strongly suggest that an investigation into determining changes in autophagy/mitophagic flux within skeletal muscle in response to chronic muscle activity is warranted.
As an effective and reliable method to evaluate autophagy and mitophagy flux, the microtubule destabilizer colchicine has been utilized. Colchicine acts by preventing the transport of autophagosomes to lysosomes and thus inhibits flux, and comparisons can be made between vehicle- and colchicine-treated groups. Recent studies in rodent models have used colchicine to assess flux of skeletal muscle autophagy/mitophagy following endurance exercise training. For example, Chen et al. (2018) revealed that the acute exercise-induced elevations in mitophagic flux in mouse skeletal muscle were diminished at the end of 6 weeks of voluntary wheel training [6]. However, it remains unknown how autophagic/mitophagic flux is regulated over the course of muscle adaptations. Therefore, utilizing colchicine, the current study aimed to determine temporal changes in autophagy/mitophagy flux during chronic contractile activity (CCA)-associated muscle adaptations, a unique and effective model for studying the adaptations to endurance training.
In addition, our recent work has shown that the lysosomal system is upregulated in skeletal muscle in response to CCA [5, 14] which occurs concomitantly with mitochondrial biogenesis. In this study we hypothesized that, in response to CCA, muscle autophagy and mitophagy flux will be activated prior to the onset of lysosomal and mitochondrial biogenesis, and we sought to understand the chronological relationship between changes in the lysosomal system, as compared to autophagic/mitophagic flux rates.
Methods
Animals and chronic contractile activity
Adult male Sprague–Dawley rats (350–500 g; 3–6 months old) were obtained from Charles River Laboratories (St. Constant, QC, Canada) and were given chow and water ad libitum. Following an acclimatization period, the animals underwent a surgical procedure to induce chronic contractile activity (CCA), as described in previous studies [15, 22]. Briefly, following anesthetization with isoflurane, medical grade electric wires were unilaterally implanted beside the common peroneal nerve that innervates tibialis anterior (TA) and extensor digitorum longus (EDL) muscle. The wires were subcutaneously extended to an external stimulator that can be switched on and off via exposure to infrared light. The contralateral, non-operated TA and EDL muscles were used as internal control (CON) muscle groups. After fully recovering from the surgeries, rats were randomly assigned to CCA for 1, 2, 5, or 7 days, respectively (3 h/day, 10 Hz continuous, 0.1 ms pulse duration). This time course was used to determine the early (1, 2 days) and later (5, 7 days) adaptations to CCA. In order to determine autophagy and mitophagy flux, colchicine (0.4 mg/kg/day; COL) or vehicle (0.9% saline; SAL) was administered via an intraperitoneal injection 24 and 48 h before the last bout of CCA. Ninety minutes following the cessation of CCA, animals were sacrificed and tissues were harvested.
Mitochondrial isolation
In order to isolate intermyofibrillar (IMF) mitochondrial fractions, TA muscles were minced, homogenized, and underwent differential centrifugation, as previously described [23, 26]. These fresh mitochondria were used for assessing both respiration and ROS production. Remaining mitochondrial samples were stored at − 80 °C for subsequent Western blotting procedures.
Mitochondrial respiration
A Clarke oxygen electrode (Strathkelvin Instruments, North Lanarkshire, UK) was used to assess mitochondrial respiration (O2/min/mg). Briefly, IMF mitochondria were incubated in VO2 buffer (250 mM sucrose, 50 mM KCl, 25 mM Tris, and 10 mM K2HPO4, pH 7.4) at 30 °C. After baseline respiration was achieved, 10 mM glutamate and 0.44 mM ADP were added to the chamber in order to measure complex I-supported state 3 and state 4 respirations, respectively. NADH was subsequently added to the chamber to test mitochondrial integrity.
ROS production
ROS production was measured in freshly isolated IMF mitochondria, as done previously [1, 6]. In brief, mitochondria (~ 75 μg) were incubated in VO2 buffer in a white polystyrene 96-well plate, with glutamate (11 mM), in the presence of (state 3) or absence of (state 4) ADP (0.4 mM). Following substrate addition, 50 μM of 2,7-dichlorodihydrofluorescein diacetate (D399, Thermo Fisher Scientific) was added to the samples, and fluorescence was measured at 37 °C for 30 min at 480–520 nm using a Synergy HT microplate reader (Bio-Tek, Winooski, VT). Data were analyzed with KC4 software (version 3.0) and normalized to O2 consumption levels measured during either state 3 or 4 as appropriate.
High-resolution respiration
High-resolution respirometry (Oroboros O2k, Austria) was used to measure oxygen consumption in the muscle fibers from the mid-portion of EDL muscle, as done in the previously [5]. Briefly, the muscle was excised and kept in ice-cold biopsy preservation solution (BIOPS) buffer (2.77 mM CaK2EGTA, 7.23 mM K2EGTA, 7.55 mM Na2ATP, 6.56 mM MgCl2⋅6H2O, 20 mM Taurine, 15 mM Na2 phosphocreatine, 20 mM imidazole, 0.5 mM dithiothreitol, 50 mM MES-hydrate, pH 7.1), after which fibers were gently separated into bundles using fine forceps. Following mechanical separation, fibers were incubated in BIOPS solution supplemented with saponin (40μg/μL) at 4 °C for 30 min for permeabilization. Fibers were subsequently washed in Miro-5 solution (110 mM sucrose, 60 mM K-lactobionate, 0.5 mM EGTA, 3 mM MgCl2, 20 mM taurine, 10 mM KH2PO4, 20 mM HEPES, pH 7.1), and muscle mass was measured after briefly blotting to remove excess water. Subsequently, they were incubated in the chambers that were filled with oxygenated Miro-5. After obtaining background values, substrates were titrated to assess state 4 (complex I), state 3 (complex I), and state 4 (complex I + II) respiration. Substrates were added in the following order: 10 mM glutamate + 2 mM malate, 2.5 mM ADP, and 10 mM succinate. To test for mitochondrial membrane integrity, cytochrome c was added to the chamber. Any increase in respiration following its addition was indicative of damaged mitochondria, and the samples were excluded from the data. Respiratory function was determined by oxygen flux rates (pmol/s ml) minus background rates and corrected to fiber mass (pmol/s ml/mg).
Western blotting
Frozen TA muscle pieces were incubated in Sakamoto buffer (20 mM HEPES, 2 mM EGTA, 1% Triton X-100, 50% glycerol, 50 mM ß-glycerophosphate) containing both phosphatase and protease inhibitors and were disrupted using a Qiagen TissueLyser II for 2–3 min at 50 Hz. Samples were then centrifuged at 16,000×g for 10 min at 4 °C, and the supernatant fraction was collected. After determining protein concentrations via the Bradford assay, 30–50 μg of proteins were separated via SDS-PAGE and transferred onto nitrocellulose membranes. Membranes were blocked in wash buffer (0.12% Tris-HCl, 0.585% NaCl, 0.1% Tween, pH 7.5) supplemented with 5% milk at room temperature for 1 h. The membranes were then incubated with primary antibodies overnight at 4 °C. Information on the primary antibodies used in this study is provided in Table 1. The following day, membranes were washed 3 × 5 min and subsequently incubated with the corresponding HRP-tagged secondary antibodies for 1 h at room temperature, after which time they were washed 3 × 5 min. Clarity™ ECL substrate (1705061, Bio-Rad) was used, and blots were imaged using a Carestream Imaging System. Band densities were quantified by ImageJ software (NIH). Ponceau stain images and VDAC were used as loading controls for whole cell lysates and mitochondrial fractions, respectively. For the calculation of autophagy and mitophagy fluxes, we determined the band densities for LC3-II or p62, corrected these for loading, and calculated the differences in LC3-II and/or p62 between SAL and COL groups (i.e., Flux = COL − SAL).
Nuclear and cytosolic fractionation
Nuclear and cytosolic fractions from fresh TA muscles were obtained using the NE-PER extraction reagents (38835, Thermo Scientific) with minor modifications. Briefly, 50~100 mg of TA muscle was minced on ice and homogenized in cytosolic extraction reagent (CER) I using a Dounce homogenizer. Homogenates were then vortexed and let to stand on ice for 10 min. Following addition of CER II solution, samples were briefly vortexed and centrifuged (16,000×g) for 10 min. The supernatant cytosolic fractions were then collected. The pellets, containing nuclei and cellular debris, were washed in cold 1× PBS and suspended in nuclear extraction buffer (NER). Nuclear fractions were then sonicated three times for ~ 3–5 s at 30% power, and incubated on ice for 40 min. The nuclear fractions were vortexed every 10 min during the incubation and subsequently underwent centrifugation (16,000 g) for 10 min. The resulting supernatant nuclear fractions were collected and stored at − 80 °C until further analysis.
Statistical analysis
Prism software (version 7) was used for statistical analysis. Data were analyzed by two-way ANOVA (time × CCA) and depicted as compared to the pooled control group that was a combination of all control groups. We also confirmed that there was no significant difference between control groups. A Dunnett’s post hoc test was used to compare significant values of each group with the corresponding control group. All data are shown as means ± SEM, and P < 0.05 represents a significant difference.
Results
Chronic contractile activity leads to mitochondrial adaptations in skeletal muscle
First, we sought to determine the temporal relationship between mitochondrial content and function in response to chronic contractile activity (CCA). In permeabilized EDL muscle fibers, ADP-stimulated complex I respiration was elevated by CCA in the EDL muscle at all time points as compared to CON (P < 0.05; Fig. 1a). State 3 respiration associated with mitochondrial complex I + II showed a trend to increase as early as day 2 and was elevated by 30% (P < 0.05) at day 5 of CCA (Fig. 1b). In addition, basal respiration supported by complex I (state 4) displayed a similar pattern as state 3 complex I + II respiration, with a 1.6-fold elevation at day 5 of CCA (P < 0.05; Fig. 1c).
Effect of chronic contractile activity (CCA) on respiration of permeabilized EDL muscle. High-resolution respirometry determines complex I- and I + II-associated basal (state 4) and maximal (state 3) respiration. a CCA increased complex I-specific state 3 respiration at all time points as compared to the pooled CON (days 1–7; P < 0.05). b Complex I + II-associated state 3 respiration was increased by CCA, which reached at a significant point at day 5 (P < 0.05). c Complex I-related basal respiration (state 4) was significantly upregulated at day 5 (P < 0.05). #P < 0.05, effect of time; *P < 0.05, CCA vs. CON (combined). All data is shown as mean ± SEM
To provide additional understanding of the changes in mitochondrial capacity for respiration and ROS emission, we also made measures in isolated IMF mitochondria. Our data reveal that CCA did not alter mitochondrial state 3 respiration until the late phase of CCA, as shown by the 1.4-fold elevation at day 7 (P < 0.05; Fig. 2a). State 4 mitochondrial respiration was reduced over the course of CCA treatment and was ~ 50% lower at day 5 when compared to the CON group (P < 0.05; Fig. 2b).
Effect of CCA on mitochondrial respiration and ROS production in TA muscle. a, b Clark electrode respirometry showed that CCA significantly increased state 3 respiration in the IMF mitochondria of TA muscle at day 7 (P < 0.05). State 4 mitochondrial respiration was decreased by CCA, which was significant at day 5 (P < 0.05). c, d CCA downregulated maximal ROS production at day 7 (P < 0.05), and basal ROS production was increased during early phase of CCA and was back to the basal level at day 7 (P < 0.05). e Western blots showed that protein abundances of both mtDNA- and nDNA-encoded mitochondrial respiration factors (COX-I and COX-IV, respectively) were significantly increased at day 7 (P < 0.05). g Representative images for Western blots are depicted and Ponceau images were used as loading control. #P < 0.05, effect of time; *P < 0.05, CCA vs. CON (combined). All data is shown as mean ± SEM
CCA significantly reduced state 3 mitochondrial ROS emission by ~ 40% following 7 days of CCA (P < 0.05; Fig. 2c). In contrast, state 4 ROS emission was upregulated during the initial time course of CCA but returned to basal levels at day 7 (P < 0.05; Fig. 2d).
Nuclear and mitochondrially encoded components are increased by CCA
To determine if the functional changes observed in permeabilized fibers were due to alterations in mitochondrial content, we quantified the protein levels of the mitochondrially encoded COX subunit I (COX-I) and the nuclear-encoded COX subunit IV (COX-IV). CCA significantly increased the protein abundance of both COX subunits by 1.5-fold, but this increase was only evident following 7 days of CCA (P < 0.05; Fig. 2e–g).
Autophagy flux in skeletal muscle is decreased following training adaptations
To evaluate autophagy flux, we examined protein levels of LC3-II, the active form of the autophagosome embedded protein LC3, along with the autophagosomal adaptor protein p62, in whole cell lysates of muscles subjected to CCA for 1–7 days, following either saline or colchicine injection. CCA had no significant effect on either LC3-II or p62 flux on days 1 through 5; however, these flux rates were reduced by 60–70% following 7 days of CCA (P < 0.05; Fig. 3a–c).
Effect of CCA on TA muscle autophagic flux. a CCA significantly decreased LC3-II flux by 50% in the TA muscle at day 7 (P < 0.05). b Muscle p62 flux was significantly downregulated by CCA at day 7 (P < 0.05). c Representative images of Western blots for LC3-II and p62 proteins. Ponceau was used for loading control. #P < 0.05, effect of time; *P < 0.05, CCA vs. CON (combined). All data is shown as mean ± SEM
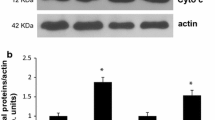
Mitophagy flux is downregulated by CCA prior to autophagic flux
Our goal was to compare mitochondrial functional changes with alterations in mitophagy flux. Thus, we specifically explored how mitophagy flux was regulated during CCA-induced muscle adaptations by measuring protein abundance of LC3-II localized on intermyofibrillar (IMF) mitochondria. Our results indicate a decrease in LC3-II accumulation on IMF mitochondria by as much as 50% by day 2 of CCA, which was maintained at 5 and 7 days as compared to CON (P < 0.05; Fig. 4a). Furthermore, our results demonstrate a downregulation of LC3-II mitophagy flux during the late phase of CCA (i.e., days 5–7), as quantified by ~ 42% (P = 0.07) and ~ 50% (P < 0.05) reduction at day 5 and day 7, respectively (Fig. 4b). This took place while there was absolutely no change in muscle LC3-II (or p62) flux even by 5 days of CCA but was convincingly reduced by day 7, as noted above. Thus, these data suggest that mitophagy flux is reduced prior to a decline in autophagy flux as a result of CCA.
Effect of CCA on TA muscle mitophagic flux. Mitophagic flux was determined in IMF mitochondria isolated from the TA muscles. a CCA decreased total protein abundances of LC3-II in IMF mitochondria of TA during days 2–7. b Mitophagic flux (LC3-II) was downregulated by CCA, which was significant at day 7 (P < 0.05). c Representative images for Western blots are depicted. VDAC was used as loading control. #P < 0.05, effect of time; *P < 0.05, CCA vs. CON (combined). All data is shown as mean ± SEM
CCA regulates the lysosomal system concomitantly with mitochondrial biogenesis
We also wished to relate changes in mitophagy with regulatory factors associated with lysosomal capacity. In response to CCA, the lysosomal transcription factor TFEB was increased by 1.7-fold by day 7, as compared to CON (P < 0.05; Fig. 5a), of which approximately 20–35% was localized to the nucleus. This fraction remained unaltered with CCA. In contrast, PGC-1α accumulated in the nucleus over the course of CCA and was increased by days 5 and 7 (P < 0.05; Fig. 5b). The lysosomal protein marker, LAMP1, was increased 1.4-fold by CCA at day 7. (P < 0.05; Fig. 5c).
Effect of CCA on lysosomal system in TA skeletal muscle. a CCA increased muscle protein expression levels of TFEB, a key marker of lysosomal biogenesis, at day 7, compared to CON (P < 0.05). b CCA increased nuclear translocation of PGC-1α, a primary factor for mitochondrial biogenesis, in skeletal muscle, which was significant at days 5–7 (P < 0.05). However, CCA did not result in a significant TFEB nuclear translocation in skeletal muscle. c CCA upregulated muscle protein abundances of lysosomal membrane marker, LAMP1 (P < 0.05). d Representative images for Western blots are shown. Ponceau images were used as loading control. #P < 0.05, effect of time; *P < 0.05, CCA vs. CON (combined). All data is shown as mean ± SEM
Discussion
Exercise training leads to metabolic adaptations in skeletal muscle, including an increase in mitochondrial content via an elevation in organelle biogenesis. However, the impact of training on mitochondrial degradation (i.e., mitophagy) remains incompletely understood. Mitophagy is vital for controlling the degradation of poorly functioning mitochondria in coordination with the lysosomal system. In this study, we aimed to explore temporal changes in mitophagy, as well as in bulk autophagy, within skeletal muscle exposed to chronic contractile activity (CCA). Here, we highlight that CCA-inducible muscle adaptations are accompanied by decreases in autophagic and mitophagic flux, as well as an upregulated lysosomal capacity in skeletal muscle.
Since changes in mitophagy are normally triggered by signals evoked by alterations in mitochondrial function, we first examined the chronology of CCA-induced adaptations in mitochondrial function using permeabilized muscle fibers, as well as isolated mitochondria. We did this because we wanted to compare changes in mitochondrial function in their native environment within muscle, with in vitro capacities for mitochondrial respiration and ROS emission. Our results in isolated mitochondria reveal increases in the capacity for state 3 respiration by 7 days of CCA, accompanied by expected increases in the expression of electron transport chain components encoded by both the nuclear and mitochondrial genomes. This represents an adaptive increase in mitochondrial biogenesis per gram of muscle, as well as organelle compositional changes, because respiration is measured on a per mitochondrion basis.
However, our data also reveal that increases in mitochondrial function occurred prior to changes in organelle biogenesis. Indeed, CCA increased complex-I supported state 4 (basal) and 3 (active) respiration in permeabilized EDL fibers at all time points of contractile activity (i.e., days 1–7). Since muscle samples were removed 90 min following the final bout of contractile activity, we surmise that these functional changes reflect alterations in the cellular metabolic environment within the contracting muscle. An acute change in mitochondrial respiration has also been observed in a study, wherein one bout of treadmill exercise upregulated respiration in permeabilized cardiac muscle fibers [18]. The authors attributed this to exercise-induced increases in ROS emission and the associated inflammatory response. Accordingly, we also detected significantly elevated basal ROS emission during the initial days of CCA (Fig. 2). Scheibye-Knudsen (2009) also suggested that permeabilized fibers exhibit higher oxygen consumption rates in both oxidative and glycolytic fibers of rats compared to isolated mitochondria, possibly due to higher concentrations of inorganic phosphate in the permeabilized fibers [27]. This further supports the notion that the cellular environment may impact measurements of mitochondrial respiration using this methodology. Importantly, it is changes in this metabolic milieu that are partially responsible for the enhancement, or attenuation, of mitophagy in muscle.
Using Atg6 heterozygous mice, Lira et al. (2013) showed that autophagy is required for training-induced improvements in running capacity, as well as for metabolic adaptations [19]. In addition, a growing number of studies have revealed that molecular markers related to the autophagic and mitophagic systems are altered in skeletal muscle in response to various types of exercise regimens [9, 12, 17]. However, these findings have been challenged because of either inconsistent results or controversial interpretations of autophagosomal protein abundances (LC3-II/I and p62 proteins) and ratios (LC3-II/LC3-I). However, most studies have not measured flux rates, a measurement which is required to account for the dynamic nature of the autophagic/mitophagic process. Thus, we have used a well-accepted method [16] of injecting animals with the microtubule destabilizer colchicine, which represents a cost- and time-efficient method of assessing flux in rodent skeletal muscle [13]. A number of studies have successfully demonstrated its efficacy and reliability on estimating muscle autophagosomal turnover rates [3, 6]. Nonetheless, it cannot be ruled out that colchicine could lead to systemic effects, as it has been reported to result in a disruption of GLUT4 trafficking in 3T3-L1 adipocytes [8]. On the other hand, Ai et al. revealed that colchicine-associated microtubule destabilization did not block either insulin- or contraction-inducible GLUT4 translocation in skeletal muscle of rats [2]. Furthermore, no evidence of physiological (e.g., body weight) and myopathic changes was observed following both high and low dosage of colchicine for 2 days (0.4, 2, and 50 mg/kg/day) [13]; thus, it is unlikely that 2 days of low-dose colchicine would have resulted in adverse effects in the current study.
Our results indicate that 7 days of CCA led to lower muscle autophagic and mitophagic flux rates as compared to control muscle groups. These results are similar to recent studies that observed decreases in mitophagy flux in colchicine-treated mice exposed to endurance exercise training (i.e., 6 weeks of running wheel exercise) [6] or 9 days of CCA [5]. However, contrary to the findings of our study, Ju et al. (2016) reported that 8 weeks of swimming exercise training elevated autophagic flux in the triceps skeletal muscle of mice [12]. In their study, mitophagy-related protein markers including PINK1 and parkin were not changed by the swimming training and appeared similar between saline- and colchicine-treated groups [12], suggesting that mitophagy flux remained unaltered. However, a recent study by Brandt et al. (2018) showed an upregulation in both PINK1 and the mitophagy receptor BNIP3 in human skeletal muscle following 8 weeks of endurance training [4]. Although these divergent results may be explained by the different exercise protocols employed (i.e., swimming vs. CCA vs. cycling), the timing of tissue collection, or the muscle groups examined (triceps vs. tibialis anterior vs. vastus lateralis), our data suggest that the enhancement of mitochondrial content and function brought about by training leads to attenuated signaling toward autophagy and mitophagy pathways as the muscle adapts. An attenuation of metabolic signaling in response to exercise is a feature of the phenotypic character of adapted muscle [20].
A further observation worthy of note from our data is that CCA-induced a decrease in muscle autophagic flux only at day 7, while the downregulation of mitophagy flux began at day 5. This suggests that regulation of the mitochondrial specific turnover system may occur prior to the onset of autophagic regulation in muscle following CCA. In addition, these changes in flux occurred prior to significant alterations in autophagic and mitophagic protein levels. These data indicate that (1) changes in protein markers do not reflect the dynamic nature of the autophagic flux patterns, and (2) the regulation toward mitophagy via changes in mitochondrial function can occur independently of those which regulate autophagic flux.
Our previous results [6, 30] showed that one bout of exhaustive exercise sharply increased mitophagy fluxes (LC3-II and p62) in the muscle of untrained mice. This effect was dependent on PGC1-α [30], which serves to drive the transcription of Tfeb, as well its translocation to the nucleus [7]. These acute effects of exercise on mitophagy are reversed during recovery (i.e., 90 min post-exercise), the time at which we collected tissue from our animals. Thus, this accounts for the absence of an acute flux response in our data. Repeated bouts of acute exercise lead to an adaptive training response, in which signaling is diminished, thus leading to an attenuation in mitophagy flux [6], which we also observe in response to long-term CCA.
The lysosomal system is also required for attaining complete autophagic and mitophagic regulations, for which TFEB, a key transcriptional regulator of lysosomal biogenesis, plays a pivotal role [21]. As noted above, the function of TFEB is interrelated with PGC-1α, a primary transcriptional coactivator for mitochondrial biogenesis [7]. Similar to previous studies [5, 14], our results show that chronic muscle use results in significant elevations in the abundance of TFEB protein, as well as in the lysosomal membrane marker LAMP1, in skeletal muscle. Accompanying these increases are significant elevations in the lysosomal proteins such as cathepsin D, MCOLN1, LAMP2, and LAMP2A [5, 14], supporting the idea that CCA leads to a marked enhancement of lysosomal capacity within skeletal muscle. Thus, chronic exercise may have therapeutic benefits to those individuals in which autophagy/mitophagy flux is inhibited at the terminal steps involving lysosomal degradation. Indeed, our data using a cell culture model have recently shown that CCA of myotubes can overcome autophagy blockage and improve mitochondrial dysfunction [24]. This process is likely initiated with each bout of acute contractile activity, which provokes TFEB localization to the nucleus, leading to the expression of lysosome and autophagy-related genes [7, 21].
The current study provides evidence that chronic muscle activity enhances mitochondrial content and function, concomitant with a progressive downregulation of mitophagy, likely because mitochondrial health is improved. This is accompanied by a concurrent upregulation of lysosomal degradation capacity as a possible safeguard to enhance the clearance of dysfunctional organelles. This adaptation contrasts with opposite findings in chronically inactive muscle, in which autophagic and mitophagic systems are abnormally upregulated, as shown in the denervated [29] and aged [3, 5] skeletal muscles.
References
Adhihetty PJ, Ljubicic V, Hood DA (2007) Effect of chronic contractile activity on SS and IMF mitochondrial apoptotic susceptibility in skeletal muscle. Am J Physiol Endocrinol Metab 292:E748–E755. https://doi.org/10.1152/ajpendo.00311.2006
Ai H, Ralston E, Lauritzen HP, Galbo H, Ploug T (2003) Disruption of microtubules in rat skeletal muscle does not inhibit insulin- or contraction-stimulated glucose transport. Am J Physiol Endocrinol Metab 285:E836–E844. https://doi.org/10.1152/ajpendo.00238.2002
Baehr LM, West DW, Marcotte G, Marshall AG, De Sousa LG, Baar K, Bodine SC (2016) Age-related deficits in skeletal muscle recovery following disuse are associated with neuromuscular junction instability and ER stress, not impaired protein synthesis. Aging (Albany NY) 8:127–146. https://doi.org/10.18632/aging.100879
Brandt N, Gunnarsson TP, Bangsbo J, Pilegaard H (2018) Exercise and exercise training-induced increase in autophagy markers in human skeletal muscle. Phys Rep 6:e13651. https://doi.org/10.14814/phy2.13651
Carter HN, Kim Y, Erlich AT, Zarrin-Khat D, Hood DA (2018) Autophagy and mitophagy flux in young and aged skeletal muscle following chronic contractile activity. J Physiol 596:3567–3584. https://doi.org/10.1113/JP275998
Chen CCW, Erlich AT, Hood DA (2018) Role of Parkin and endurance training on mitochondrial turnover in skeletal muscle. Skelet Muscle 8:10. https://doi.org/10.1186/s13395-018-0157-y
Erlich AT, Brownlee DM, Beyfuss K, Hood DA (2018) Exercise induces TFEB expression and activity in skeletal muscle in a PGC-1alpha-dependent manner. Am J Phys Cell Physiol 314:C62–C72. https://doi.org/10.1152/ajpcell.00162.2017
Fletcher LM, Welsh GI, Oatey PB, Tavare JM (2000) Role for the microtubule cytoskeleton in GLUT4 vesicle trafficking and in the regulation of insulin-stimulated glucose uptake. Biochem J 352(Pt 2):267–276
Halling JF, Ringholm S, Nielsen MM, Overby P, Pilegaard H (2016) PGC-1alpha promotes exercise-induced autophagy in mouse skeletal muscle. Phys Rep 4:e12698. https://doi.org/10.14814/phy2.12698
Hood DA (2001) Invited review: contractile activity-induced mitochondrial biogenesis in skeletal muscle. J Appl Physiol (1985) 90:1137–1157
Hood DA, Tryon LD, Carter HN, Kim Y, Chen CC (2016) Unravelling the mechanisms regulating muscle mitochondrial biogenesis. Biochem J 473:2295–2314. https://doi.org/10.1042/BCJ20160009
Ju JS, Jeon SI, Park JY, Lee JY, Lee SC, Cho KJ, Jeong JM (2016) Autophagy plays a role in skeletal muscle mitochondrial biogenesis in an endurance exercise-trained condition. J Physiol Sci 66:417–430. https://doi.org/10.1007/s12576-016-0440-9
Ju JS, Varadhachary AS, Miller SE, Weihl CC (2010) Quantitation of “autophagic flux” in mature skeletal muscle. Autophagy 6:929–935. https://doi.org/10.4161/auto.6.7.12785
Kim Y, Hood DA (2017) Regulation of the autophagy system during chronic contractile activity-induced muscle adaptations. Phys Rep 5:e13307. https://doi.org/10.14814/phy2.13307
Kim Y, Memme JM, Hood DA (2018) Application of chronic stimulation to study contractile activity-induced rat skeletal muscle phenotypic adaptations. J Vis Exp 131. https://doi.org/10.3791/56827
Klionsky DJ, Abdelmohsen K, Abe A et al. (2016) Guidelines for the use and interpretation of assays for monitoring autophagy (3rd edition). Autophagy 12:1–222. https://doi.org/10.1080/15548627.2015.1100356
Laker RC, Drake JC, Wilson RJ, Lira VA, Lewellen BM, Ryall KA, Fisher CC, Zhang M, Saucerman JJ, Goodyear LJ, Kundu M, Yan Z (2017) Ampk phosphorylation of Ulk1 is required for targeting of mitochondria to lysosomes in exercise-induced mitophagy. Nat Commun 8:548. https://doi.org/10.1038/s41467-017-00520-9
Li H, Miao W, Ma J, Xv Z, Bo H, Li J, Zhang Y, Ji LL (2016) Acute exercise-induced mitochondrial stress triggers an inflammatory response in the myocardium via NLRP3 inflammasome activation with mitophagy. Oxidative Med Cell Longev 2016:1987149–1987111. https://doi.org/10.1155/2016/1987149
Lira VA, Okutsu M, Zhang M, Greene NP, Laker RC, Breen DS, Hoehn KL, Yan Z (2013) Autophagy is required for exercise training-induced skeletal muscle adaptation and improvement of physical performance. FASEB J 27:4184–4193. https://doi.org/10.1096/fj.13-228486
Ljubicic V, Hood DA (2009) Specific attenuation of protein kinase phosphorylation in muscle with a high mitochondrial content. Am J Physiol Endocrinol Metab 297:E749–E758. https://doi.org/10.1152/ajpendo.00130.2009
Mansueto G, Armani A, Viscomi C, D'Orsi L, De Cegli R, Polishchuk EV, Lamperti C, Di Meo I, Romanello V, Marchet S, Saha PK, Zong H, Blaauw B, Solagna F, Tezze C, Grumati P, Bonaldo P, Pessin JE, Zeviani M, Sandri M, Ballabio A (2016) Transcription factor EB controls metabolic flexibility during exercise. Cell Metab 25:182–196. https://doi.org/10.1016/j.cmet.2016.11.003
Memme JM, Oliveira AN, Hood DA (2016) Chronology of UPR activation in skeletal muscle adaptations to chronic contractile activity. Am J Phys Cell Physiol 310:C1024–C1036. https://doi.org/10.1152/ajpcell.00009.2016
Menzies KJ, Singh K, Saleem A, Hood DA (2013) Sirtuin 1-mediated effects of exercise and resveratrol on mitochondrial biogenesis. J Biol Chem 288:6968–6979. https://doi.org/10.1074/jbc.M112.431155
Parousis A, Carter HN, Tran C, Erlich AT, Mesbah Moosavi ZS, Pauly M, Hood DA (2018) Contractile activity attenuates autophagy suppression and reverses mitochondrial defects in skeletal muscle cells. Autophagy 14:1886–1897. https://doi.org/10.1080/15548627.2018.1491488
Rodnick KJ, Henriksen EJ, James DE, Holloszy JO (1992) Exercise training, glucose transporters, and glucose transport in rat skeletal muscles. Am J Phys 262:C9–C14. https://doi.org/10.1152/ajpcell.1992.262.1.C9
Saleem A, Iqbal S, Zhang Y, Hood DA (2015) Effect of p53 on mitochondrial morphology, import, and assembly in skeletal muscle. Am J Phys Cell Physiol 308:C319–C329. https://doi.org/10.1152/ajpcell.00253.2014
Scheibye-Knudsen M, Quistorff B (2009) Regulation of mitochondrial respiration by inorganic phosphate; comparing permeabilized muscle fibers and isolated mitochondria prepared from type-1 and type-2 rat skeletal muscle. Eur J Appl Physiol 105:279–287. https://doi.org/10.1007/s00421-008-0901-9
Tam BT, Pei XM, Yu AP, Sin TK, Leung KK, Au KK, Chong JT, Yung BY, Yip SP, Chan LW, Wong CS, Siu PM (2015) Autophagic adaptation is associated with exercise-induced fibre-type shifting in skeletal muscle. Acta Physiol (Oxford, England) 214:221–236. https://doi.org/10.1111/apha.12503
Vainshtein A, Desjardins EM, Armani A, Sandri M, Hood DA (2015) PGC-1alpha modulates denervation-induced mitophagy in skeletal muscle. Skelet Muscle 5:9. https://doi.org/10.1186/s13395-015-0033-y
Vainshtein A, Tryon LD, Pauly M, Hood DA (2015) Role of PGC-1alpha during acute exercise-induced autophagy and mitophagy in skeletal muscle. Am J Phys Cell Physiol 308:C710–C719. https://doi.org/10.1152/ajpcell.00380.2014
Yan Z, Lira VA, Greene NP (2012) Exercise training-induced regulation of mitochondrial quality. Exerc Sport Sci Rev 40:159–164. https://doi.org/10.1097/JES.0b013e3182575599
Acknowledgements
We thank Jenny Lai for her dedicated technical assistance on this project.
Funding
This work was supported by funding from the Natural Sciences and Engineering Research Council of Canada (NSERC) to D. A. Hood. D. A. Hood is also the holder of a Canada Research Chair in Cell Physiology.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All animal procedures were approved and performed in accordance with the guidelines of the York University Animal Care Committee.
Additional information
This article is part of the special issue on Exercise Physiology: future opportunities and challenges in Pflügers Archiv—European Journal of Physiology
Rights and permissions
About this article
Cite this article
Kim, Y., Triolo, M., Erlich, A.T. et al. Regulation of autophagic and mitophagic flux during chronic contractile activity-induced muscle adaptations. Pflugers Arch - Eur J Physiol 471, 431–440 (2019). https://doi.org/10.1007/s00424-018-2225-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00424-018-2225-x