Abstract
Our study explored the effects of lncRNA UCA1 on the proliferation and apoptosis in hypoxic human pulmonary artery smooth muscle cells (HPASMCs) and highlighted the endogenous relationship between UCA1, ING5, and hnRNP I in cell proliferation. Hypoxia-induced HPASMCs were used to simulate pulmonary arterial hypertension in vitro. Microarray assay was adopted to screen the dysregulated expressed lncRNAs in HPASMCs to find out the target gene of our study. And RT-qPCR was performed to detect the expression of lncRNA UCA1 under hypoxia and normoxia. After transfection, the relationship between UCA1 and cell proliferation in HPASMCs under hypoxia were determined by cell proliferation assay and relative expression of PCNA. Next, ELISA assays were conducted to measure the protein levels of PCNA and ING5. What’s more, flow cytometry was employed to measure the apoptosis rate in differentially UCA1-expressed HPASMCs. RIP assays were conducted to further clarify the endogenous relationship between UCA1 and ING5 in hypoxic HPASMCs. Finally, the effects of ING5 to HPASMCs were detected after transfection of ING5 and UCA1 to figure out the role of ING5 in HPASMCs. Hypoxia was revealed to induce proliferation and inhibited apoptosis in HPASMCs. Besides, UCA1 was confirmed to be highly expressed under hypoxia compared with normoxia. UCA1 boosted cell proliferation under hypoxia in HPASMCs. However, the apoptosis was suppressed in the hypoxic HPASMCs transfected with pcDNA3.1-UCA1. Further, mechanism studies found that UCA1 competed with ING5 for hnRNP I, so that upregulating UCA1 inhibited the protein levels of ING5. And finally we found that ING5 restrained cell viability, but promoted cell apoptosis in hypoxic HPASMCs, which was reversed by UCA1 over-expression. In summary, our findings manifested that UCA1 promoted proliferation and restrained apoptosis by competing with ING5 for hnRNP I in HPASMCs induced by hypoxia, indicating their potential roles for the cure of hypoxic pulmonary hypertension.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pulmonary arterial hypertension (PAH) is an intractable disorder primarily characterized by pulmonary vascular remodeling in PAH pathology [15]. In particular, pulmonary vascular remodeling is mainly composed of several cancer-like variations such as abnormal vascular proliferation, veering apoptosis and enhanced migration in vascular smooth muscle cells [3]. Despite the identification of several molecular pathways of vascular remodeling, the pathogenesis of vascular remodeling remains obscure. Pulmonary hypertension (PH) is known as a disease related to miscellaneous causes [16, 19]. Furthermore, Semenza et al. reported that hypoxic condition was regarded as a dominating origin [20]. However, the latent endogenous factors are not understood in PAH pathogenesis.
Long noncoding RNAs lack for protein coding capability with full length of over 200 nt [2]. An increasing number of findings have demonstrated that lncRNAs is marked by manifold biological functions such as excessive cell growth [32], cell differentiation [8], and apoptosis [13]. In addition to being famous as tumor promoters or suppressors, abnormal expressed lncRNAs shown by several studies play a pivotal role in human cancer and diseases containing colorectal cancer [34], schizophrenia [1], and cardiovascular disease as well [12, 14]. Particularly, lncRNAs are correlated with vascular functions. LncRNAs are revealed to be largely found in vascular cells and make contributions to the contractility of smooth muscle cells [2]. Besides, the proliferation and apoptosis of vascular muscle cells are regulated by lncRNAs [28].
LncRNA urothelial carcinoma associated 1 (UCA1) is composed of three exons that encode three isoforms containing 1.4 kb, 2.2 kb, and 2.7 kb in length separately [10, 33]. UCA1 is firstly observed to be upregulated and acted as an oncogenic biomarker in bladder carcinoma [10, 17, 25]. Of note, lncRNA UCA1 was reported to be hypoxia responsive for expediting cell proliferation in bladder carcinoma under hypoxia [30]. Despite that, it is not obvious whether lncRNA UCA1 is directly associated with the regulation of other non-tumor diseases such as PAH under hypoxia. Hence, the expression levels, functions, and its endogenous factors of UCA1 under hypoxia in pulmonary vascular remodeling need to be well clarified.
The inhibitor of growth (ING) proteins (ING1-ING5) have been identified and characterized as candidate tumor suppressors. All ING proteins share a highly conserved carboxy-terminal plant homeodomain (PHD) and are involved in the control of cell growth, senescence, apoptosis, DNA repair, and chromatin remodeling [4, 18, 21]. ING5 acts as tumor suppressor gene because of suppression in cell growth and promotion in cell apoptosis in certain cancers such as gastric carcinogenesis, human head and neck squamous cell carcinoma and oral squamous cell carcinoma [6, 22, 24, 29]. As PAH is mainly composed of several cancer-like variations such as abnormal vascular proliferation, veering apoptosis, and enhanced migration in vascular smooth muscle cells [3], we conjectured that ING5 may play a vital role in PAH.
Here, our observations manifested that lncRNA UCA1 promoted proliferation and prevented apoptosis in hypoxic pulmonary artery smooth muscle cells (HPASMCs). Remarkably, UCA1 was highly expressed in HPASMCs under hypoxia compared with normoxia. Furthermore, the endogenous mechanism underlying the cell proliferation was explored. Therefore, our results illustrated the mechanism that lncRNA UCA1 promoted HPASMCs growth by competing with ING5 for hnRNP I under hypoxia, giving an insight into the potential therapy for PAH.
Materials and methods
Cells culture
Human pulmonary artery smooth muscle cells (HPASMCs) were acquired from BeNa Culture Collection (BNCC338614, Beijing, China). HPASMCs were grown in high-glucose Dulbecco’s modified Eagle’s medium (DMEM) containing 4 mM L-glutamine and sodium pyruvate plus 10% fetal bovine serum (FBS). Cells were cultured at 37 °C with 95% air and 5% CO2 in humidified incubator. And for the hypoxic induction, PASMCs were incubated in the hypoxic condition with a gas mixture containing 92% N2, 5% CO2, 3% O2 for 72 h. Passages 2–3 were used for the further experiments. Before each experiment, the PASMCs were quiesced for 24 h in the DMEM medium without serum.
Cell proliferation assay
Cell counting kit-8 assays were executed ranging from different time points to detected cell proliferation. Cells were placed in 96-well plates and incubated under different circumstances such as hypoxia and normoxia. At 0, 24, 48, and 72 h, cell viability was measured by quantifying the optical density (OD) value at 450 nm using cell counting kit-8 (Beyotime, Shanghai, China). The whole experiments were made separately in triplicate.
Flow cytometry
Flow cytometry was conducted to analyze cell apoptosis under normoxia or hypoxia with the treatment in accordance with the protocol of annexin V-FITC/PI kit (Sigma-Aldrich, St. Louis, MO, USA). HPASMCs were trypsinized and later centrifuged for 5 min. After washing twice with PBS for 5 min, the cells were resuspended in a concentration of 200 μl binding buffer. Subsequently, 10 μl FITC-conjugated annexin V and 5 μl PI were placed into the cells and fixed for 15 min in the dark at 37 °C. Post staining within 1 h was conducted to analyze the cell lines. Hypoxic HPASMCs were stained with annexin V-FITC (green) shown in x axis and red propidium iodide (PI, red) shown in y axis. The apoptosis rate was counted as the early apoptosis percentage in bottom right quadrant plus the late apoptosis percentage in top right quadrant by flow cytometry.
Microarray
The normoxia-treated HPASMCs and relative hypoxia-treated HPASMCs were prepared for lncRNAs microarray. After extraction of the whole RNA via TRIzol reagent (Invitrogen, Carlsbad, CA, USA) and quantification, electrophoresis was used to denature the RNA integrity. Subsequently, double-stranded cDNA was synthesized and hybridized by Human LncRNA 4 × 180 K Expression Microarray (Agilent Technologies, Santa Clara, CA, USA). R language was utilized for analyzing the differentially expressed lncRNAs. The threshold used to screen the overexpression or knockdown of lncRNAs was fold change (FC) > 2 and P < 0.05, separately.
RT-qPCR
Total RNAs were isolated from HPASMCs by TRIzol reagent (Invitrogen, Carlsbad, CA, USA). Subsequently, cDNA was synthesized by reverse transcription with PrimeScript RT reagent kit (Takara, Dalian, China) and analyzed by SYBR-Green kit (Takara, Dalian, China). GAPDH was an internal control. Relative quantification levels were revealed by the 2−ΔΔCt method. All the premier sequences were as follows: UCA1 (forward) 5′-CTCTCCTATCTCCCTTCACTGA-3′, (reverse) 5′-CTTTGGGTTGAGGTTCCTGT-3′; ING5 (forward) 5′-TCCAGAACGCCTACAGCAAG-3′, (reverse) 5′-TGCCCTCCATCTTGTCCTTC-3′; GAPDH (forward) 5′-AGTGGCAAAGTGGAGATT-3′, (reverse) 5′-GTGGAGTCATACTGGAACA-3′.
Cell transfection
The HPASMCs were placed in 6-well dishes 24 h before transfection. Full length of UCA1 cDNA sequence was cloned into pCMV vector (GenePharma Co., Ltd., Shanghai, China) to construct UCA1 overexpression plasmid (p-UCA1), while sh-UCA1 was also cloned into pCMV vector to construct UCA1 downregulation plasmid (p-sh-UCA1). All of the plasmids were transfected into HPASMCs by lipofectamine 2000 reagent (Invitrogen, Carlsbad, CA, USA) under the guidance of protocol.
Enzyme-linked immunosorbent assay
PCNA and ING5 levels in the lysis of HPASMCs under normoxia or hypoxia were determined using the enzyme-linked immunosorbent assay (ELISA) kits (abcam, Cambridge, MA, USA) in accordance with the manufacturer’s instructions. The 100 μl serial dilution samples were put into the plate for 2 h incubation at 37 °C. Subsequently, the aspirated samples were washed with phosphate buffered saline with Tween 20 (PBST) for four times. Then each well was added with 100 μl antibody against PCNA and ING5 for 1 h incubation. After rinsing for four times, the plate was supplemented with 100 μl secondary antibodies conjugated with horseradish peroxidase (HRP) for 30 min incubation. With 100 μl substrate inoculated in the dark for 15 min, the optical density was determined using an ELISA reader (TECAN, Salzburg, Austria) at 450 nm.
RNA immunoprecipitation assays
To determine the endogenous relationship between UCA1 and ING5 for cell proliferation, RNA immunoprecipitation (RIP) assays were implemented adopting Magna RIP™ RNA-Binding Protein Immunoprecipitation Kit (Merck Millipore, Billerica, MA, USA). HPASMCs were harvested and lysed with RIP lysis buffer plus protease inhibitor (Thermo Fisher Scientific, Waltham, MA, USA) and RNase inhibitor (Thermo Fisher Scientific). Cell extracts were incubated with RIP buffer including magnetic beads conjugated with antihuman hnRNP I antibody (ab133734, abcam) for 1 h. At last, following the digestion of proteinase K, RNA was extracted for RT-qPCR. Signals of UCA1 and ING5 RNAs precisely binding to hnRNP I were certified by observing simultaneously input controls of total RNA and negative controls of rabbit IgG (ab190475, abcam).
Statistical analyses
The Graphpad Prism (Version 6.0, GraphPad software Inc., LA Jolla, CA, USA) was employed for statistical analyses. Data were presented as the standard deviation of the mean (mean ± SD) for studies in triplicate. Student’s t test was made to identify the differences between two groups.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Results
UCA1 was overexpressed in hypoxic HPASMCs
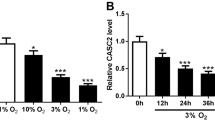
Hypoxia-induced HPASMCs were used to simulate PAH in vitro. Firstly, hypoxia promoted HPASMCs proliferation compared with normoxia by cell proliferation assay (Fig. 1a, P < 0.05). There was significant difference of cell viability under hypoxia at 72 h opposed to normoxia. Subsequently, flow cytometric annexin V assay revealed that hypoxia inhibited apoptosis in contrast with nomoxia under hypoxia at 72 h (Fig. 1b, c; P < 0.05). Hence, hypoxia promoted proliferation and reduced cell apoptosis in HPASMCs, suggesting that hypoxia-induced HPASMC models were constructed successfully. Then microarray assay of HPASMCs was adopted to screen the dysregulated expressed lncRNAs, which were shown in Fig. 1d. There were six lncRNAs that were upregulated in the hypoxia group and downregulated in the normoxia group. Then, we chose UCA1 as the research object because it had much higher expression induced by hypoxia compared with normoxia (Fig. 1d). The RT-qPCR results further conformed that UCA1 was highly expressed under hypoxia in HPASMCs (Fig. 1e, P < 0.001). Therefore, UCA1 was involved in the hypoxic HPASMCs.
UCA1 was overexpressed in hypoxic HPASMCs. a Cell viability under hypoxia or normoxia for 0, 24, 48, and 72 h in HPASMCs was measured by CCK-8 assay. Observation was made at 450 nm. b, c Flow cytometry assay revealed that hypoxia inhibited cell apoptosis and the total apoptosis rates (Q2 + Q3) were calculated. Q1: Annexin V-FITC negative + PI positive, Q2: Annexin V-FITC positive + PI positive, Q3: Annexin V-FITC positive + PI negative, Q4: Annexin V-FITC negative + PI negative. d Microarray data of the aberrant expressed lncRNAs were evaluated under normoxia or hypoxia. e Hypoxia increased relative UCA1 levels compared with normoxia. (*P < 0.001, ***P < 0.001, compared with normoxia)
UCA1 promoted cell growth under hypoxia in HPASMCs
Furthermore, to identify the role of UCA1 in HPASMCs, UCA1 was firstly downregulated by transfecting p-sh-UCA1 to hypoxic HPASMCs and overexpressed by transfecting p3.1-UCA1 to hypoxic HPASMCs (Fig. 2a, P < 0.05). Cell proliferation assay showed that the growth curve of the p-UCA1 group increased sharply from 48 to 72 h. Knockdown of UCA1 remarkably suppressed the cell growth while overexpression of UCA1 greatly boosted cell viability (Fig. 2b, P < 0.05). PCNA and ING5 levels were further measured to assess HPASMCs proliferation by ELISA assays. Protein level of PCNA was dramatically reduced and ING5 level was greatly elevated in p-sh-UCA1 group, suggesting that cell viability was restrained (Fig. 2c, d; all P < 0.05). After upregulation of UCA1, PCNA protein level rose substantially while ING5 protein level declined sharply, which demonstrated that cell viability was enhanced in p-UCA1 group. Thus, UCA1 induced cell proliferation in hypoxic HPASMCs.
UCA1 induced proliferation in hypoxic HPASMCs. a Relative UCA1 level was measured by RT-qPCR through transfection with pCMV-UCA1 (p-UCA1) and pCMV-sh-UCA1 (p-sh-UCA1) in hypoxic HPASMCs. b Cell proliferation assay was implemented to assess the cell viability after altered UCA1 expression through transfection in HPASMCs under hypoxia. c, d PCNA and ING5 protein levels were observed by ELISA kits in HPASMCs. (*P < 0.05, **P < 0.01, compared with NC)
UCA1 inhibited cell apoptosis in hypoxic HPASMCs
Cell apoptosis rate was dramatically increased in p-sh-UCA1 group, revealing that the knockdown of UCA1 expedited cell apoptosis (Fig. 3a, b, all P < 0.05). However, cell apoptosis rate was restrained in the p-UCA1 group, suggesting that overexpressed UCA1 prevented cell apoptosis. Taken together, UCA1 restrained cell apoptosis in hypoxic HPASMCs.
UCA1 promoted hypoxic HPASMCs proliferation by competing with ING5 mRNA for hnRNP I
What’s more, we then explored the underlying mechanism of the UCA1 involving in proliferation in hypoxic HPASMCs. Results above demonstrated that the protein level of ING5 was negative regulated by UCA1, and considering the example of the endogenous mechanism of UCA1 competing with p27 for hnRNP I, we suspected that UCA1 may negatively connect with ING5 under the same mechanism, which was confirmed by the further RIP assay. RIP assay revealed that hypoxia enhanced the interaction between UCA1 and hnRNP I in contrast with normoxia (Fig. 4a, P < 0.01). However, the interaction between ING5 mRNA level and hnRNP I significantly weakened under hypoxia compared with normoxia (Fig. 4b, P < 0.01). Hence, we hypothesized that competition exists between UCA1 and ING5 for hnRNP I binding. Subsequently, to test the hypothesis whether the interaction of hnRNP I with UCA1 suppresses the hnRNP I binding activity of ING5, a competition assay was carried out in HPASMCs. As expected, more UCA1 pulldown by hnRNP I antibody was found in the p-UCA1 group than the NC group (Fig. 4c, P < 0.01). In the meantime, UCA1 remarkably attenuated the capability of hnRNP I for pulling down ING5 (Fig. 4d, P < 0.01). Taken together, these results demonstrated that UCA1 competed with ING5 mRNA for hnRNP I.
UCA1 restrained ING5 protein level by competing for hnRNP I. a Relative UCA1 level bound by hnRNP I under normoxia or hypoxia were uncovered by RIP assay. b ING5 mRNA level was interacted with hnRNP I, as observed by RIP assay under normoxia or hypoxia. c, d RIP assay was performed under hypoxia to explore the suppressed interaction of ING5 mRNA with hnRNP I by UCA1. (**P < 0.01, compared with normoxia or the NC group)
ING5 restrained cell viability and proliferation, but promoted cell apoptosis, which was reversed by UCA1
Figure 5a indicated that there were corresponding changes of protein level of ING5 after transfection with pCMV-ING5 (p-ING5) and pCMV-sh-ING5 (p-sh-ING5) in hypoxic HPASMCs (P < 0.05). Overexpression ING5 decreased the expression of UCA1 and knockdown ING5 increased the expression of UCA1 in HPASMCs, which further verified the conclusions above (Fig. 5b, P < 0.05). As shown in Fig. 5c, overexpression of ING5 remarkably suppressed the cell viability, which was reversed by the overexpression of UCA1 (P < 0.05). And then the protein level of PCNA was detected to measure cell proliferation. We found that overexpression ING5 significantly reduced the expression of PCNA and overexpression UCA1 reversed the reduction (Fig. 5d). Cell apoptosis rate was dramatically increased in the p-ING5 group, revealing that the overexpression ING5 expedited cell apoptosis (Fig. 5e, f; all P < 0.05). However, cell apoptosis rate was restrained by UCA1. Taken together, ING5 restrained cell viability and proliferation, but promoted cell apoptosis in hypoxic HPASMCs, which were reversed by UCA1.
The effect of ING5 to UCA1 level, cell viability and apoptosis. a Relative protein level of ING5 was measured by ELISA kit through transfection with pCMV-ING5 (p-ING5) and pCMV-sh-ING5 (p-sh-ING5) in hypoxic HPASMCs. b UCA1 level was measured by RT-qPCR in HPASMCs. c Cell proliferation assay was implemented to assess the cell viability after altered UCA1 and ING5 expression through transfection in HPASMCs under hypoxia. d Relative protein level of PCNA was measured by ELISA kit through transfection with pCMV-ING5 (p-ING5) and pCMV-UCA1 (p-UCA1) in hypoxic HPASMCs. (E and F) The total apoptosis rates (Q2 + Q3) were calculated by Flow cytometry assay. (*P < 0.05, **P < 0.01, compared with NC; #P < 0.05, compared with both p-ING5 and p-UCA1)
Discussion
In the present study, a series of experiments proved that lncRNA UCA1 was overexpressed and played a critical role in the proliferation and apoptosis of HPASMCs under hypoxia inducing through regulating the expression of ING5.
LncRNAs were reported to play a pivotal part in cell proliferation, differentiation, and apoptosis in a set of studies recently [9, 23, 26]. Furthermore, aberrant expression of lncRNAs were connected with a list of human diseases such as cardiovascular disorders [7]. For instance, lncRNA CHRF was revealed to be a novel regulator for cardiac hypertrophy by miR-489 [27]. In HPASMCs, hypoxia-induced lncRNA MALAT1 was revealed by Brock et al. to be of great importance in regulation of cell proliferation [3]. LncRNA lnRPT modulated the proliferation in HPASMCs under exposure to PDGF-BB treatment [31]. Zhu et al. also reported that the knockdown of lncRNA MEG3 enhanced cell proliferation and migration through depressing PTEN by miR-21 in hypoxia-induced PASMCs [35]. PAH featured progressive development in pulmonary vessel resistance mainly because of vascular contraction, or hypoxic pulmonary vascular remodeling [5, 11]. In particular, the excessive growth of PASMCs was a key characteristic of pulmonary vascular remodeling in PAH [3]. Our result demonstrated that lncRNA UCA1 was the most highly expressed one under hypoxia. Thus, we speculated that lncRNA UCA1 would serve as a regulator in the proliferation and apoptosis in HPASMCs.
Ectopic expression of UCA1 had been observed in many cancers such as prostate cancer [2], gastric cancer [3], hepatocellular carcinoma [19], and ovarian cancer [3]. Moreover, UCA1 levels were knockdown under H2O2 treatment in cardiomyocytes after cardiac ischemia reperfusion injury [2]. Similarly, we observed that UCA1 was highly expressed in HPASMCs under hypoxia. This is the first study of lncRNA UCA1 in PAH.
LncRNA UCA1 elevated cell viability and refrained H2O2-exposed apoptosis in cardiomyocytes [3]. What’s more, according to Xue et al., UCA1 could expedite bladder cancer proliferation and prevent apoptosis by hypoxia [19], which was similar to our findings. Our observation revealed that lncRNA UCA1 promoted cell viability, proliferation, and suppressed apoptosis under hypoxia in HPASMCs.
Heterogeneous nuclear ribonucleoprotein I (hnRNP I) possessed certain RNA-binding domains and functions as a protein for biding RNA and splicing mRNA [3]. Hung et al. demonstrated that UCA1 promoted cell growth by competition with p27 for hnRNP I and UCA1 negatively connected with p27 [2]. Similar with the endogenous mechanism, our study considered hnRNP I as a significant player between UCA1 and ING5 mRNA in the competition for hnRNP I because overexpression of UCA1 led to a decline in the complex of ING5 mRNA and hnRNP I. Of note, one of our significant results was the detection of ING5 as a UCA1 competitor for the interaction with hnRNP I. ING5 acted as tumor suppressor gene because of suppression in cell growth and promotion in cell apoptosis in certain cancers such as gastric carcinogenesis, human head and neck squamous cell carcinoma, and oral squamous cell carcinoma [6, 22, 24, 29]. These findings supported our result that the complex of ING5 mRNA and hnRNP I declined under hypoxia, indicating that viability was boosted under hypoxia in HPASMCs.
While our study uncovered comprehensive insight into the function of UCA1 in PH in vitro with a series of experiments being conducted, whether UCA1 plays the same role in patients with PH was not investigated, which deserved further study.
In general, we showed that lncRNA UCA1 was overexpressed in PAH. UCA1 enhanced proliferation and refrained apoptosis in HPASMCs under hypoxia. Remarkably, competition assay revealed that UCA1 competed with ING5 for the interaction with hnRNP I in HPASMCs under hypoxia. Therefore, lncRNA UCA1 enhanced cell viability and restrained cell apoptosis by competing with ING5 for hnRNP I and shedding lights on the part of UCA1 in the diagnosis of PH.
References
Barry G, Briggs JA, Vanichkina DP, Poth EM, Beveridge NJ, Ratnu VS, Nayler SP, Nones K, Hu J, Bredy TW, Nakagawa S, Rigo F, Taft RJ, Cairns MJ, Blackshaw S, Wolvetang EJ, Mattick JS (2014) The long non-coding RNA Gomafu is acutely regulated in response to neuronal activation and involved in schizophrenia-associated alternative splicing. Mol Psychiatry 19:486–494. https://doi.org/10.1038/mp.2013.45
Batista PJ, Chang HY (2013) Long noncoding RNAs: cellular address codes in development and disease. Cell 152:1298–1307. https://doi.org/10.1016/j.cell.2013.02.012
Brock M, Schuoler C, Leuenberger C, Buhlmann C, Haider TJ, Vogel J, Ulrich S, Gassmann M, Kohler M, Huber LC (2017) Analysis of hypoxia-induced noncoding RNAs reveals metastasis-associated lung adenocarcinoma transcript 1 as an important regulator of vascular smooth muscle cell proliferation. Exp Biol Med (Maywood) 242:487–496. https://doi.org/10.1177/1535370216685434
Campos EI, Chin MY, Kuo WH, Li G (2004) Biological functions of the ING family tumor suppressors. Cell Mol Life Sci 61:2597–2613. https://doi.org/10.1007/s00018-004-4199-4
Farber HW, Loscalzo J (2004) Pulmonary arterial hypertension. N Engl J Med 351:1655–1665. https://doi.org/10.1056/NEJMra035488
Gou WF, Shen DF, Yang XF, Zhao S, Liu YP, Sun HZ, Su RJ, Luo JS, Zheng HC (2015) ING5 suppresses proliferation, apoptosis, migration and invasion, and induces autophagy and differentiation of gastric cancer cells: a good marker for carcinogenesis and subsequent progression. Oncotarget 6:19552–19579. https://doi.org/10.18632/oncotarget.3735
Greco S, Gorospe M, Martelli F (2015) Noncoding RNA in age-related cardiovascular diseases. J Mol Cell Cardiol 83:142–155. https://doi.org/10.1016/j.yjmcc.2015.01.011
Guttman M, Donaghey J, Carey BW, Garber M, Grenier JK, Munson G, Young G, Lucas AB, Ach R, Bruhn L, Yang X, Amit I, Meissner A, Regev A, Rinn JL, Root DE, Lander ES (2011) lincRNAs act in the circuitry controlling pluripotency and differentiation. Nature 477:295–300. https://doi.org/10.1038/nature10398
Harries LW (2012) Long non-coding RNAs and human disease. Biochem Soc Trans 40:902–906. https://doi.org/10.1042/BST20120020
Huang J, Zhou N, Watabe K, Lu Z, Wu F, Xu M, Mo YY (2014) Long non-coding RNA UCA1 promotes breast tumor growth by suppression of p27 (Kip1). Cell Death Dis 5:e1008. https://doi.org/10.1038/cddis.2013.541
Humbert M, Sitbon O, Simonneau G (2004) Treatment of pulmonary arterial hypertension. N Engl J Med 351:1425–1436. https://doi.org/10.1056/NEJMra040291
Kataoka M, Wang DZ (2014) Non-coding RNAs including miRNAs and lncRNAs in cardiovascular biology and disease. Cells 3:883–898. https://doi.org/10.3390/cells3030883
Khaitan D, Dinger ME, Mazar J, Crawford J, Smith MA, Mattick JS, Perera RJ (2011) The melanoma-upregulated long noncoding RNA SPRY4-IT1 modulates apoptosis and invasion. Cancer Res 71:3852–3862. https://doi.org/10.1158/0008-5472.CAN-10-4460
Klattenhoff CA, Scheuermann JC, Surface LE, Bradley RK, Fields PA, Steinhauser ML, Ding H, Butty VL, Torrey L, Haas S, Abo R, Tabebordbar M, Lee RT, Burge CB, Boyer LA (2013) Braveheart, a long noncoding RNA required for cardiovascular lineage commitment. Cell 152:570–583. https://doi.org/10.1016/j.cell.2013.01.003
Liu Y, Sun Z, Zhu J, Xiao B, Dong J, Li X (2018) LncRNA-TCONS_00034812 in cell proliferation and apoptosis of pulmonary artery smooth muscle cells and its mechanism. J Cell Physiol 233:4801–4814. https://doi.org/10.1002/jcp.26279
McLaughlin VV, Davis M, Cornwell W (2011) Pulmonary arterial hypertension. Curr Probl Cardiol 36:461–517. https://doi.org/10.1016/j.cpcardiol.2011.08.002
Mercer TR, Dinger ME, Mattick JS (2009) Long non-coding RNAs: insights into functions. Nat Rev Genet 10:155–159. https://doi.org/10.1038/nrg2521
Russell M, Berardi P, Gong W, Riabowol K (2006) Grow-ING, age-ING and die-ING: ING proteins link cancer, senescence and apoptosis. Exp Cell Res 312:951–961. https://doi.org/10.1016/j.yexcr.2006.01.020
Schermuly RT, Ghofrani HA, Wilkins MR, Grimminger F (2011) Mechanisms of disease: pulmonary arterial hypertension. Nat Rev Cardiol 8:443–455. https://doi.org/10.1038/nrcardio.2011.87
Semenza GL (2011) Oxygen sensing, homeostasis, and disease. N Engl J Med 365:537–547. https://doi.org/10.1056/NEJMra1011165
Soliman MA, Riabowol K (2007) After a decade of study-ING, a PHD for a versatile family of proteins. Trends Biochem Sci 32:509–519. https://doi.org/10.1016/j.tibs.2007.08.006
Tian Y, Hu Y, Wang Z, Chen K, Zhang L, Wang L, Ren M, Huang A, Tang H (2011) Hepatitis B virus regulates Raf1 expression in HepG2.2.15 cells by enhancing its promoter activity. Arch Virol 156:869–874. https://doi.org/10.1007/s00705-010-0901-z
Tripathi V, Ellis JD, Shen Z, Song DY, Pan Q, Watt AT, Freier SM, Bennett CF, Sharma A, Bubulya PA, Blencowe BJ, Prasanth SG, Prasanth KV (2010) The nuclear-retained noncoding RNA MALAT1 regulates alternative splicing by modulating SR splicing factor phosphorylation. Mol Cell 39:925–938. https://doi.org/10.1016/j.molcel.2010.08.011
Ullah M, Pelletier N, Xiao L, Zhao SP, Wang K, Degerny C, Tahmasebi S, Cayrou C, Doyon Y, Goh SL, Champagne N, Cote J, Yang XJ (2008) Molecular architecture of quartet MOZ/MORF histone acetyltransferase complexes. Mol Cell Biol 28:6828–6843. https://doi.org/10.1128/MCB.01297-08
Wang F, Li X, Xie X, Zhao L, Chen W (2008) UCA1, a non-protein-coding RNA up-regulated in bladder carcinoma and embryo, influencing cell growth and promoting invasion. FEBS Lett 582:1919–1927. https://doi.org/10.1016/j.febslet.2008.05.012
Wang KC, Yang YW, Liu B, Sanyal A, Corces-Zimmerman R, Chen Y, Lajoie BR, Protacio A, Flynn RA, Gupta RA, Wysocka J, Lei M, Dekker J, Helms JA, Chang HY (2011) A long noncoding RNA maintains active chromatin to coordinate homeotic gene expression. Nature 472:120–124. https://doi.org/10.1038/nature09819
Wang K, Liu F, Zhou LY, Long B, Yuan SM, Wang Y, Liu CY, Sun T, Zhang XJ, Li PF (2014) The long noncoding RNA CHRF regulates cardiac hypertrophy by targeting miR-489. Circ Res 114:1377–1388. https://doi.org/10.1161/CIRCRESAHA.114.302476
Wu G, Cai J, Han Y, Chen J, Huang ZP, Chen C, Cai Y, Huang H, Yang Y, Liu Y, Xu Z, He D, Zhang X, Hu X, Pinello L, Zhong D, He F, Yuan GC, Wang DZ, Zeng C (2014) LincRNA-p21 regulates neointima formation, vascular smooth muscle cell proliferation, apoptosis, and atherosclerosis by enhancing p53 activity. Circulation 130:1452–1465. https://doi.org/10.1161/CIRCULATIONAHA.114.011675
Xing YN, Yang X, Xu XY, Zheng Y, Xu HM, Takano Y, Zheng HC (2011) The altered expression of ING5 protein is involved in gastric carcinogenesis and subsequent progression. Hum Pathol 42:25–35. https://doi.org/10.1016/j.humpath.2010.05.024
Xue M, Li X, Li Z, Chen W (2014) Urothelial carcinoma associated 1 is a hypoxia-inducible factor-1alpha-targeted long noncoding RNA that enhances hypoxic bladder cancer cell proliferation, migration, and invasion. Tumour Biol 35:6901–6912. https://doi.org/10.1007/s13277-014-1925-x
Yang Y, Chen K, Zhou Y, Hu Z, Chen S, Huang Y (2018) Application of serum microRNA-9-5p, 21-5p, and 223-3p combined with tumor markers in the diagnosis of non-small-cell lung cancer in Yunnan in southwestern China. Onco Targets Ther 11:587–597. https://doi.org/10.2147/OTT.S152957
Zhang E, Han L, Yin D, He X, Hong L, Si X, Qiu M, Xu T, De W, Xu L, Shu Y, Chen J (2017) H3K27 acetylation activated-long non-coding RNA CCAT1 affects cell proliferation and migration by regulating SPRY4 and HOXB13 expression in esophageal squamous cell carcinoma. Nucleic Acids Res 45:3086–3101. https://doi.org/10.1093/nar/gkw1247
Zhang Y, Liu Y, Xu X (2018) Knockdown of LncRNA-UCA1 suppresses chemoresistance of pediatric AML by inhibiting glycolysis through the microRNA-125a/hexokinase 2 pathway. J Cell Biochem 119:6296–6308. https://doi.org/10.1002/jcb.26899
Zheng Y, Song D, Xiao K, Yang C, Ding Y, Deng W, Tong S (2016) LncRNA GAS5 contributes to lymphatic metastasis in colorectal cancer. Oncotarget 7:83727–83734. https://doi.org/10.18632/oncotarget.13384
Zhu B, Gong Y, Yan G, Wang D, Qiao Y, Wang Q, Liu B, Hou J, Li R, Tang C (2018) Down-regulation of lncRNA MEG3 promotes hypoxia-induced human pulmonary artery smooth muscle cell proliferation and migration via repressing PTEN by sponging miR-21. Biochem Biophys Res Commun 495:2125–2132. https://doi.org/10.1016/j.bbrc.2017.11.185
Funding
This work was supported by the National Natural Science Foundation of China (81800051, 81570723, 81673423, U1704168), Natural Science Foundation of Henan Province (162300410216, 182300410332, 20171410118), and Research project of Xinxiang Medical University (XYBSKYZZ201626, 2016PN-KFKT-02, 2017BSQDJF). This work was also supported by vascular remodeling intervention and molecular targeted therapy drug development innovation team and cardiovascular remodeling intervention and molecular targeting drug research and development key laboratory.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Zhu, TT., Sun, RL., Yin, YL. et al. Long noncoding RNA UCA1 promotes the proliferation of hypoxic human pulmonary artery smooth muscle cells. Pflugers Arch - Eur J Physiol 471, 347–355 (2019). https://doi.org/10.1007/s00424-018-2219-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00424-018-2219-8