Abstract
We investigated the mechanisms behind the endothelial-derived hyperpolarization (EDH)-induced renal vasodilation in vivo and in vitro in rats. We assessed the role of Ca2+-activated K+ channels and whether K+ released from the endothelial cells activates inward rectifier K+ (Kir) channels and/or the Na+/K+-ATPase. Also, involvement of renal myoendothelial gap junctions was evaluated in vitro. Isometric tension in rat renal interlobar arteries was measured using a wire myograph. Renal blood flow was measured in isoflurane anesthetized rats. The EDH response was defined as the ACh-induced vasodilation assessed after inhibition of nitric oxide synthase and cyclooxygenase using L-NAME and indomethacin, respectively. After inhibition of small conductance Ca2+-activated K+ channels (SKCa) and intermediate conductance Ca2+-activated K+ channels (IKCa) (by apamin and TRAM-34, respectively), the EDH response in vitro was strongly attenuated whereas the EDH response in vivo was not significantly reduced. Inhibition of Kir channels and Na+/K+-ATPases (by ouabain and Ba2+, respectively) significantly attenuated renal vasorelaxation in vitro but did not affect the response in vivo. Inhibition of gap junctions in vitro using carbenoxolone or 18α-glycyrrhetinic acid significantly reduced the endothelial-derived hyperpolarization-induced vasorelaxation. We conclude that SKCa and IKCa channels are important for EDH-induced renal vasorelaxation in vitro. Activation of Kir channels and Na+/K+-ATPases plays a significant role in the renal vascular EDH response in vitro but not in vivo. The renal EDH response in vivo is complex and may consist of several overlapping mechanisms some of which remain obscure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endothelium-induced vasodilation plays an important role in the regulation of microvascular tone. In addition to release of nitric oxide (NO) and prostacyclin (PGI2), the endothelium mediates vasodilation via endothelium-derived hyperpolarization (EDH). The residual vasodilation in response to endothelial stimulation with acetylcholine (ACh) or bradykinin after inhibition of eNOS and cyclooxygenase (COX) is defined as EDH [19]. However, the initiator of EDH seems to vary as K+, EETs, or H2O2 have been suggested for different vascular beds [19]. Other studies suggest that EDH is not caused by a factor released by the endothelium but rather originates from a transfer of hyperpolarizing current through myoendothelial junctions [14]. It is also probable that several of these factors operate in concert [20].
ACh-induced activation of endothelial muscarinergic receptors increases endothelial cell (EC) intracellular Ca2+ concentration ([Ca2+]i) [21] possibly by activation of TRP channels [40]. EC in several vascular beds from different species express small (SKCa) and intermediate (IKCa) conductance K+ channels activated by Ca2+ [26]. In renal arteries and arterioles expression of Kir2.1-, SKCa2-, and SKCa3 channels has been found in the vascular smooth muscle cells (VSMC) and EC [10, 23, 24, 48]. Pharmacological inhibition of SKCa and IKCa channels in isolated perfused kidneys suggests that these channels are present and functional in the renal vasculature [46, 51, 53].
Activation of endothelial SKCa and IKCa channels leads to hyperpolarization of EC which in turn may hyperpolarize the underlying VSMC via a hyperpolarizing current through myoendothelial gap junctions [56]. This notion is supported by the fact that especially IKCa channels co-localize with myoendothelial gap junctions [43]. Another proposed mechanism for initiation of EDH is that K+ released by EC SKCa and IKCa channels accumulates in the intercellular space between EC and VSMC and activates VSMC inward rectifying K+ (Kir2.1) channels and/or Na+/K+-ATPase. This in turn induces hyperpolarization and vasodilation [11, 18].
In IKCa channel knockout mice, the EDH response was significantly reduced in the cremaster microcirculation in vivo [55]. The EDH response in SKCa knockouts was also reduced and combined knockout of SKCa and IKCa channels further reduced the EDH response [4]. In the renal vasculature, in vitro studies have shown that the EDH response can be abolished by co-treatment with apamin and charybdotoxin inhibitors of SKCa and IKCa channels, respectively [6, 52, 53]. Although this implies a role for Ca2+-activated K+ channels in the EDH response in this vascular bed, it is difficult to extrapolate results from in vitro studies to the situation in the intact organism. The significance of EDH in vivo as well as the mechanism behind may vary between species, vascular beds, and vessel size [22]. In rats, the renal vascular response to ACh in vivo is composed of an NO/PGI2-dependent part and an EDH part. The renal EDH response in vivo has been suggested to be sensitive to apamin and/or charybdotoxin as they reduce the peak vasodilation [17] and to gap junction inhibition, which reduces the renal EDH response in vivo [12].
In this study, we wished to examine the role of IK and SK channels and Kir channels and Na+/K+-ATPase in the renal EDH response in Sprague-Dawley rats. The importance of K+ channels and gap junctions was also investigated in isolated interlobar arteries in the wire myograph. The in vitro results were tested in vivo by assessing renal blood flow (RBF). Our hypothesis was that Ca2+-activated K+ channels play an essential role in the renal EDH-induced vasodilation in vivo and in vitro. Furthermore, we hypothesized that subsequent VSMC hyperpolarization can be induced by two different pathways. Firstly, accumulation of extracellular K+ that leads to activation of Kir channels and Na+/K+-ATPase and, secondly, spread of hyperpolarization from EC to VSMC via gap junctions.
Methods
We performed our experiments in 25 male Sprague-Dawley rats (BW 316 ± 4 g) for the myograph experiments and 28 male Sprague-Dawley rats (BW 316 ± 5 g) for the in vivo experiments. Rats were obtained from Taconic (Lille Skensved, Denmark). The rats were fed standard rat laboratory chow and tap water ad libitum and kept in a 12-h day/night cycle. All experimental protocols were approved by the Danish National Animal Experiments Inspectorate and conform to the European Convention for the Protection of Vertebrate Animals used for Experimental and other Scientific Purposes.
Tissue preparation and myograph force measurement
The animals were anesthetized with 5 % isofluran delivered in 35 % oxygen and 65 % nitrogen and euthanized with spinal cord dislocation. The kidneys were excised and bathed in cold dissection buffer (in mM: NaCl 135, KCl 5, MgSO4·7H2O 1, HEPES 10, glucose 5, CaCl2 1, and albumin 5 g/l, pH 7.4). Renal interlobar arteries were dissected and cleaned under a dissection microscope. The arteries were cut into 2 mm pieces and threaded onto two stainless steel wires (Ø40 μm). The vessels were transferred to a preheated (37 °C) myograph chamber (Danish Myograph Technology A/S, Aarhus, Denmark) containing a physiological saline solution (PSS in mM: NaCl 130, NaHCO3 14.9, KCl 4.7, MgSO4·7H2O 1.17, KH2PO4 1.18, glucose 5.5, CaCl2 1.6, EDTA 0.026) aerated with 95 % O2 and 5 % CO2, resulting in a pH of 7.4. The period between isolation and the start of experiments was less than 2 h. The vessels were normalized according to Mulvany et al. [38] to a tension equivalent to 0.9 times the tension found at a transmural pressure equivalent to 100 mmHg.
Myograph protocol
All protocols were initiated with two successive exposures to PSS containing 60 mM K+ and 10 μM norepinephrine (NE) serving as viability test and reference contractions. Vessels developing a tension <1 mN were discarded. The vessels were incubated for 30 min with PSS containing N (G)-nitro-L-arginine methyl ester (L-NAME, Sigma-Aldrich; 300 μM) and indomethacin (3 μM) to inhibit production of NO and PGI2. The vessels were pre-constricted with NE (100 nM) and cumulative concentration-response curves to ACh (1 nM to 10 μM) were performed. These measurements represent the EDH response. The vessels were then incubated with PSS containing L-NAME, indomethacin, and the relevant potassium channel or gap junction blockers for 30 min.
In one group, apamin (50 nM) and 1-[(2-chlorophenyl)diphenylmethyl]-1H-pyrazole (TRAM-34; 1 μM) were added to block SKCa and IKCa, respectively. The vessels were pre-constricted with 100 nM NE and the EDH response was measured during a cumulative ACh concentration-response curve (1 nM to 10 μM).
In a second group, we used Ba2+ (30 μM) and/or ouabain (100 nM) to block Kir channels and Na+/K+-ATPase, respectively. The vessels were pre-constricted with 100 nM NE and the EDH response was measured during a cumulative ACh concentration-response curve (1 nM to 10 μM). The vessels were incubated for 30 min with Ba2+ or ouabain separately as well as in combination to assess the individual responses.
In a third group, the gap junction uncouplers carbenoxolone (100 μM) or 18-α glycyrrhetinic acid (100 μM) were used. The vessels were pre-constricted with 100 nM NE and the EDH response was obtained by administration of cumulative concentrations of ACh (1 nM to 10 μM).
Finally, we tested the influence of the incubation time of the K+ channel blockers on the EDH response. Instead of 30 min, we used the shorter incubation times utilized in the in vivo experiments (4 min with TRAM-34 and apamin and 2.5 min with Ba2+ and ouabain).
Surgical procedure for in vivo experiments
Twenty-three rats were anesthetized with isoflurane delivered in 65 % nitrogen and 35 % oxygen. For arterial pressure measurements, a polyethylene (PE-50) catheter was placed in the left carotid artery. Mean arterial pressure (MAP) was measured using a Statham P23-dB pressure transducer (Gould, Oxnard, CA, USA). Two PE-10 catheters in the right jugular vein allowed for continuous i.v. infusions. Isotonic saline was given continuously at a rate of 20 μl/min. The muscle relaxant cisatracurium (Nimbex, 0.85 mg/ml; GlaxoSmithKline, Brøndby, Denmark) was administered as a 0.5 ml bolus, followed by continuous infusion (17 μg/min in physiological saline (20 μl/min)). Five additional rats were anesthetized using pentobarbital (Mebumal SAD; 120–150 μg/min) given i.v. through the jugular vein.
A tracheotomy was performed and the rat was connected to a small animal ventilator to ensure sufficient ventilation (tidal volume 0.8 ml/100 g body weight) at a frequency of ∼65 breaths/min. To maintain a body temperature of 37 °C, the rat was placed on a servo-controlled heating table. The final isoflurane concentration (∼2 %) needed to maintain sufficient anesthesia was adjusted to ensure a stable blood pressure. After midline and subcostal incisions, the abdominal aorta and left kidney were exposed. A tapered and curved PE-10 catheter was introduced through the left iliac artery and advanced through the abdominal aorta and 1 mm into the left renal artery. Test agents were administered through this catheter directly into the renal artery to minimize systemic effects. The catheter did not interfere with RBF measurements. A perivascular flow probe (1PRB; Transonic T 420) was placed around the left renal artery to measure RBF. The left urether was catheterized (PE-10 connected to PE-50) to ensure free urine flow. After the surgical procedure was completed, the rat was allowed to recover for ∼30 min before the experimental protocol was initiated.
Experimental protocol in vivo
An Upchurch six-port injection valve (Upchurch Scientific, Oak Harbor, WA USA) was used for administration of ACh (calculated renal plasma concentration 0.5 μM given for 90 s) and inhibitors into the renal artery. The rate of infusion in the renal artery catheter was increased from 10 to 144 μl/min when substances were administered to ensure that they reached the renal vasculature almost instantly [49]. All concentrations are estimated renal arterial plasma concentration if not stated otherwise. After an initial ACh response was recorded, indomethacin (5 mg/kg i.v. Sigma-Aldrich, Copenhagen, Denmark) was given as a bolus followed by L-NAME (10 mg/kg/h i.v. for 30 min). After 30 min equilibration, ACh was infused again to estimate EDH-induced renal vasodilation.
In six rats, the effect of the SKCa channel inhibitor apamin and the IKCa channel inhibitor TRAM-34 on the EDH-induced vasodilation was assessed. Apamin (0.5 μM) and TRAM-34 (10 μM) were administered for 4 and 6 min, prior to the following ACh infusion. The order of infusion was randomized. Thereafter, ACh was administered in combination with apamin and TRAM-34 for an additional 90 s.
In eight rats, we investigated how inhibition of Kir channels with Ba2+ (25 μM) and inhibition of the Na+/K+-ATPase with ouabain (100 μM) affected the EDH-induced renal vasodilation. Ba2+ and ouabain were administered 2.5 min prior to ACh administration. Then ACh, Ba2+ and ouabain were administered as a combination for an additional 90 s.
In nine rats, we assessed the effect of inhibiting Kir channels alone. Ba2+ was administered 2.5 min prior to ACh administration. Then ACh and Ba2+ were administered together for 90 s.
In five rats, the effect of volatile anesthesia (isoflurane) on EDH response was compared to that of intraperitoneal pentobarbital anesthesia. The effect of SKCa and IKCa channel inhibition was also examined with the different anesthesia.
Ba2+ at a calculated renal plasma concentration of 25 μM has been shown to have an inhibitory effect on Kir channels in vivo [35]. Similarly, the estimated concentration of apamin (0.25 μM) has previously been shown to be effective in vivo [17] and TRAM-34 at 1 μM to be effective in isolated arterioles [37].
Due to variations in baseline RBF, the RBF responses to ACh are expressed as ∆ increase (increase from baseline). Baseline was calculated as the mean of the values obtained the last minute before each ACh injection (where flow in the renal artery catheter was 144 μl/min). The RBF responses presented are averaged over the 30 s where the RBF response was maximal.
Solution and drugs
Myograph experiments
All compounds were prepared as stock solutions in water or DMSO (≤0.1 % in final solution) and diluted in PSS. The different types of inhibitors were administered in amounts to give the following final bath concentrations: indomethacin 3 μM, L-NAME 300 μM, TRAM-34 1 μM (dissolved in DMSO), apamin 50 nM, Ba2+ 30 μM, ouabain 100 nM, carbenoxolone 100 μM (dissolved in DMSO), and 18-α GA 100 μM (dissolved in DMSO). Norepinephrine and acetylcholine chloride were both added directly to the myograph chamber, according to the concentrations stated above (see Experimental protocols). Viability tests were made using KPSS (in mM): NaCl 74.7, NaHCO3 14.9, KCl 60, MgSO4·7H2O 1.17, KH2PO4 1.18, glucose 5.5, CaCl2 1.6, EDTA 0.026. Myograph bath buffers were temperated at 37 °C.
In vivo experiments
ACh and Ba2+ were dissolved in saline to concentrations, calculated to give a renal plasma concentration of approximately 0.5 and 25 μM, respectively, when infused into the renal artery at 144 μl/min. The stock solutions contained 10.4 μM ACh and 0.52 mM Ba2+. Apamin was dissolved in 1 ml 0.05 M acetic acid and further diluted in saline containing 1 % BSA to a stock solution of 10.4 μM (giving a calculated renal arterial plasma concentration of ∼0.5 μM). TRAM-34 was dissolved in DMSO and further diluted in saline containing 1 % BSA (giving a stock solution of 0.21 mM) to give a renal arterial plasma concentration of ∼10 μM. Indomethacin was dissolved in PBS (140 mM NaCl, 2.6 mM KCl, 1.4 mM KH2PO4, and 8.2 mM Na2HPO4) to a concentration of 5.8 mM. L-NAME was dissolved in saline to give a dose of 10 mg/kg/h. Previous experiments have shown that vehicle containing the used concentrations of acetic acid or DMSO did not affect RBF.
All chemicals were obtained from Sigma-Aldrich (Copenhagen, Denmark).
Statistics
For statistical analysis, SigmaPlot software (Systat Software Inc., USA) was used. Data from the myograph experiments are expressed as mean ± SEM of n animals. Initial NE contractions are expressed as the mean maximum NE contraction of all animals in the group. Relaxations are expressed as the peak percentage reduction of the total NE contraction. The means are calculated at a stable response over a time period of 30 s. In vivo data are presented as the increase from baseline RBF (∆ RBF) ± SEM. To evaluate whether the change in RBF induced by ACh was significant, a paired Student’s t test was utilized. Repeated measures ANOVA followed by Newman-Keuls test was used for statistical analysis within groups. A P value <0.05 was considered statistically significant. Graphs were drawn using GraphPad Prism.
Results
Effect of IKCa and SKCa blockers on EDH responses in vitro
Measurements of interlobar artery tension in the wire myograph during addition of cumulative concentration of ACh showed that the IKCa blocker TRAM-34 (1 μM) and the SKCa blocker apamin (50 nM) significantly attenuate the EDH response (Fig. 1a; P < 0.05). In the original tracing shown in Fig. 1c, the effect of cumulative concentrations of ACh on a vessel pre-constricted with 100 nM NE is shown. Addition of a combination of apamin and TRAM-34 clearly attenuated the EDH response (from 69 ± 4 % relaxation to 23 ± 2 %; P < 0.05, Fig. 1a, d). The pre-constricting effect of 100 nM NE was reduced when the vessels were incubated with TRAM-34 and apamin (from 8.0 ± 0.8 to 5.3 ± 0.5 mN, Table 1).
Concentration-dependent responses to ACh in renal interlobar arteries after addition of TRAM-34 and apamin or Ba2+ and ouabain. a Inhibition of IKCa and SKCa channels using TRAM-34 (1 μM) and apamin (50 nM) attenuated the EDH response significantly (n = 5). b Adding Kir and Na+/K+-ATPase blockers (Ba2+ (30 μM) and ouabain (100 nM)) also significantly attenuated the EDH response (n = 6). c Vasodilatory responses to increasing concentrations of ACh added to the myograph chamber (increasing in logarithmic steps from 10−9 to 10−5) in the presence of L-NAME and indomethacin (EDH response). d Effect of apamin and TRAM-34 on EDH. *P < 0.05 showing significant different values between the two groups
Effect of Kir and Na+/K+-ATPase blockers on isometric EDH responses
Incubation with Ba2+ and ouabain also attenuated the EDH response significantly (Fig. 1b). Ba2+ and ouabain treatment did not significantly affect pre-constriction with NE in these experiments (Table 1). In the control experiments, the EDH response induced by 10 μM ACh relaxed the vessels by 82 ± 5 % of the NE pre-constriction value. Inhibition of Kir channels alone with Ba2+ (30 μM) reduced the EDH response by 70 ± 4 % (results not shown). After blocking with ouabain (1 mM) alone, the EDH response at 10 μM ACh was reduced by 44 ± 4 % (results not shown). The reduction of the EDH response was larger when the blockers were combined (31 ± 2 % relaxation, Fig. 1b).
Effect of gap junction blockers on EDH responses
We applied two gap junction blockers: carbenoxolone (100 μM) and 18-α glycyrrhetinic acid (100 μM). The pre-constricting effects of 100 nM NE were significantly reduced (P < 0.05) when the vessels were incubated with the inhibitors (Table 1). Both carbenoxolone and 18-α glycyrrhetinic acid significantly attenuated the EDH-induced relaxation (from 82 ± 5 to 41 ± 6 %, Fig. 2a; and 83 ± 3 to 28 ± 3 %, respectively, Fig. 2b).
Concentration-dependent responses to ACh in renal interlobar arteries after addition of gap junction inhibitors carbenoxolone or 18-α glycyrrhetin acid. Adding carbenoxolone (100 μM; n = 4) (a) and 18-α-glycyrrhetinic acid (100 μM; n = 6) (b) significantly attenuates the EDH response. *P < 0.05 showing significant different values between the two groups
We tested if carbenoxolone or 18-α glycyrrhetinic acid affected overall endothelial function. These experiments were conducted without L-NAME and indomethacin. After incubation with gap junction inhibitors, pre-contraction with 100 nM NE was followed by addition of increasing doses of ACh. The vessels dilated normally in response to ACh after exposure to the gap junction blockers (e.g., pre-constriction reduced by 77 ± 5 % after 10 μM ACh and 82 ± 3 % after addition of 18α-GA and 10 μM ACh, results not shown).
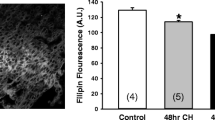
Effect of incubation time on EDH responses
In the first experiments, we incubated the vessels for 30 min with the respective K+ channel inhibitors. To compare with the incubation time used in vivo, we incubated the vessels for 4 min (TRAM-34 and apamin) or 2.5 min (Ba2+ and ouabain). Pre-constriction with 100 nM NE was followed by 1 and 10 μM ACh. We only used two ACh concentrations in order to reduce the exposure time to the inhibitors. With both inhibitor combinations, we found a significant decrease in the EDH response at both ACh concentrations (Fig. 3; P < 0.05). The inhibitory effect was slightly attenuated compared to the effect seen after 30 min. However, the results suggest that the inhibitors are effective in reducing the EDH response even after the shorter exposure times.
Physiological status of rats used in in vivo experiments
A total of 28 Sprague-Dawley rats were used for the in vivo experiments. Bodyweight, MAP, and RBF (Table 2) were comparable between groups. Treatment with indomethacin and L-NAME significantly increased MAP in all groups. In the TRAM-34 and apamin group and Ba2+ and ouabain group, RBF decreased significantly after L-NAME and indomethacin treatment (Table 2). Treatment with Ba2+ and ouabain or Ba2+ alone also decreased RBF further (Table 2).
Influence of Ca2+-activated K+ channels on renal blood flow in vivo
Intrarenal infusion of ACh at a rate of 1.5 nmol/min, resulting in an estimated renal arterial plasma concentration of 0.5 μM, significantly increased RBF (ΔRBF 2.2 ± 0.4 ml/min, P < 0.01 vs. baseline). After treatment with L-NAME and indomethacin, the EDH-induced increase in RBF was 0.5 ± 0.1 ml/min. Pre-treatment with TRAM-34 (10 μM) and apamin (0.5 μM) for 4 min slightly reduced the EDH response to 0.3 ± 0.1 ml/min and treatment for 6 min further decreased the EDH response (ΔRBF 0.1 ± 0.1 ml/min; Fig. 4a) such that it was no longer significantly different from baseline. However, there was no statistical difference between the EDH responses elicited without and with apamin and TRAM-34. Changing anesthesia from isoflurane to pentobarbital did not influence the results (Fig. 4b). These results suggest that SKCa- and/or IKCa channels might play a role in EDH in vivo but the incubation time seems essential in this regard.
Increases in renal blood flow (∆RBF) after infusion of ACh and SK/IK channels inhibitors. In isoflurane anesthetized rats (a), treatment with L-NAME (10 mg/kg/h) and indomethacin (5 mg/kg) (L/I) significantly decreased the response to ACh infusions from a change in RBF of 2.2 ± 0.4 to 0.5 ± 0.1 ml/min. Pre-treatment with TRAM-34 (10 μM) and apamin (0.5 μM) (TRAM & apa 4 min) for 4 min did not affect the in vivo EDH (n = 6). After pre-treatment with TRAM-34 and apamin (TRAM & apa 6 min) for 6 min, there was no significant increase in RBF after ACh infusion compared to baseline (n = 6). In pentobarbital anesthetized rats (b), changes in RBF in response to ACh infusions were similar (n = 5)
Influence of Kir channels and Na+/K+-ATPases
To test whether intercellular K+, via activation of Kir channels and/or Na+/K+-ATPases, acts as a mediator of the EDH response in the renal vasculature, indomethacin- and L-NAME-treated rats received intrarenal infusions of Ba2+ (25 μM) or a combination of Ba2+ and ouabain (100 μM) before the ACh infusion. Both treatments reduced RBF significantly (Table 2). Again, the ACh response was significantly larger than the EDH response. Inhibition of Kir channels and Na+/K+-ATPases using Ba2+ and ouabain did not change the EDH response (Δ RBF 0.4 ± 0.1 ml/min vs. 0.6 ± 0.1 ml/min; Fig. 5a). Interestingly, inhibition of Kir channels alone increased the EDH response to a value significantly different from the EDH response in the presence of L-NAME and indomethacin (Fig. 5b).
Increases in renal blood flow (∆RBF) after infusion of ACh and inhibitors of Kir channels and Na+/K+-ATPases. In isoflurane anesthetized rats (a), treatment with L-NAME (10 mg/kg/h) and indomethacin (5 mg/kg) (L/I) significantly decreased the response to ACh infusions from 1.3 ± 0.1 to 0.4 ± 0.1 ml/min. Pre-treatment with Ba2+ (25 μM) and ouabain (100 μM) (Ba + Ou) did not affect the in vivo EDH (n = 8). b Pre-treatment with Ba2+ alone significantly increased the EDH response (n = 9). *P < 0.05 vs. ACh + L/I
Discussion
In this study, we report that combined inhibition of SKCa and IKCa channels significantly attenuated the renal interlobar artery EDH response in vitro as did inhibition of Kir channels and/or Na+/K+-ATPase. The renal EDH-induced responses in vitro were related to EDH-induced responses in vivo. In vivo, we found an EDH-mediated RBF response. Inhibition of SKCa and IKCa channels or Kir channels and/or Na+/K+-ATPase did not significantly reduce the EDH response.
The role of EDH-induced renal vasodilation has been examined in isolated renal vessels and isolated kidneys but in vivo studies are sparse. In the hydronephrotic rat kidney, inhibition of IKCa or SKCa channels using charybdotoxin or apamin significantly reduced the EDH response and the combination of the inhibitors abolished the response [53, 54]. Likewise, Jiang et al. reported that treatment with apamin and charybdotoxin abolished the EDH response in renal interlobar arteries from Wistar-Kyoto rat [27]. However, in interlobar arteries from Sprague-Dawley rats, the same authors found no effect of either apamin or charybdotoxin inhibition on the maximum EDH response [28]. We used rat interlobar arteries to assess EDH-induced renal vasodilation under isometric conditions. In our hands, TRAM-34 and apamin significantly reduced the EDH response supporting the importance of endothelial Ca2+-activated K+ channels.
Accumulation of K+ released from the EC may activate the Kir channel and/or the Na+/K+-ATPase in the VSMC membrane leading to hyperpolarization of the VSMC and subsequent vasodilation, as has been demonstrated in carotid arteries [18]. Kir channels are extensively expressed and functional [9, 35, 48] in VSMC of the rat renal circulation. In the present study, we found in vitro that Ba2+ had a minor but significant effect on the EDH-mediated response whereas the effect of ouabain was more pronounced. When combined, an additive effect was found. This is in agreement with studies on porcine interlobar arteries [7] but in contrast to studies conducted on rat interlobar arteries and afferent arterioles [27, 53]. These experiments indicate that in isolated interlobar arteries, the EDH response is in part initiated by endothelial IKCa/SKCa channels releasing K+ to activate Kir channels and Na+/K+-ATPases. However, in the smaller afferent arterioles, this mechanism does not seem to be crucial [53].
We quantified the EDH response in vivo as the change in RBF following infusion of ACh after blockade of NO and PGI2 synthesis. The EDH response in vivo was significant and amounted to ∼18 % of the response to ACh in the absence of L-NAME and indomethacin. We did not find a statistical difference between the change in RBF following inhibition of the IKCa and SKCa channels. When IKCa and SKCa channels were blocked for 4 min, there was still a significant increase in RBF. However, after 6 min incubation, the change in RBF after ACh administration was not significantly different from baseline. This suggests that the IKCa and SKCa channels might play a role for the EDH response in vivo and this effect is strongly affected by the incubation time. In contrast to the in vitro results, inhibition of Kir channels and/or Na+/K+-ATPases in vivo did not affect the EDH response. On the contrary, inhibition of Kir channels alone increased renal EDH response, a finding not compatible with the current understanding of the action of this channel in the renal vasculature. Thus, we cannot exclude the possibility that this finding is a result of systemic blockade of this channel, e.g., in the central nervous system. However, as judged from the changes in RBF after infusion of Ba2+ or Ba2+ in combination with ouabain (Table 2), the inhibitors reached and exerted an effect on the renal circulation which indicates that the failure of these agents to reduce the EDH response is not due to an inability to reach the renal circulation and affect the targeted channels. The discrepancy between the in vivo and in vitro results in this regard deserves some attention. In vivo, we measured RBF as the integrated flow of the whole kidney. Non-adrenergic non-cholinergic (NANC) nerves containing substance P (SP), vasoactive intestinal peptide (VIP), and calcitonin gene-related peptide (CGRP) have been shown to surround the renal vasculature [29–31]. All three neuropeptides have been shown to increase RBF [15, 41, 47]. It is possible that activation of NANC nerves in vivo contribute to a more sustained renal vasodilation. For the isometric experiments, we used interlobar vessels with a diameter of 380–500 μm. Most of the renal vascular resistance is located in the small arterioles. As shown by Wang et al. [53], the EDH response in afferent arterioles was not reduced by Ba2+ and ouabain which is in contrast to what we and others found in interlobar arteries. It is possible that the significance of Kir channels and Na+/K+-ATPases changes with vessel size.
In mice and rat, renal vasculature myoendothelial junctions have been found in interlobular, afferent, and efferent arteries with the highest density in the smaller arterioles [36, 50]. We and others show that inhibition of gap junctions significantly decreases EDH-induced vasodilation, in the renal vasculature as well as in other vascular beds, in vitro [2, 8, 13, 16]. However, Jiang and Dusting reported no effect of 18-α glycyrrhetinic acid in the same preparation [27]. Currently, we have no complete explanation for this discrepancy, but it should be noted that these authors used a lower concentration of 18-α glycyrrhetinic acid (50 μM). The effect of gap junction inhibition could be even more pronounced in vivo if the EDH response in smaller arterioles is more dependent on the myoendothelial junctions. The renal EDH response was strongly attenuated when gap junctions were blocked using connexin mimetic peptides against Cx40 in vivo [12]. The myoendothelial gap junction creates a restricted space allowing signaling between the EC and the VSMC [5, 32]. Key to this theory is the activation of IKCa or SKCa channels in the endothelium to induce the hyperpolarization [45]. The influence of myoendothelial gap junctions on the EDH response has previously been compared in different experimental settings. The EDH-induced vasodilatation was independent of myoendothelial gap junctions when measured under isobaric conditions, whereas under isometric conditions, the EDH-induced vasodilatation was abolished in Cx40 knockout mice [3]. This is in line with our findings that the EDH response in the renal interlobar artery depends on gap junctions under isometric conditions in the wire myograph. Furthermore, we cannot exclude the possibility that mechanisms suggested to induce endothelium-induced VSMC hyperpolarization and vasodilation independent of EC IKCa and SKCa channels, such as activation of VSMC KATP channels by H2S released from the EC, play a more significant role in the resistance vessels [39]. There are also other known mediators of EDH such as H2O2. H2O2 has most likely several mechanisms of action [44]. One of them is activation of VSMC PKGI-α which subsequently activates potassium channels in the VSMC [42]. Also, the BKCa channel is redox sensitive [57], and could also be a direct target for H2O2-mediated EDH [44].
Edgley et al. reported that pre-treatment with charybdotoxin and apamin attenuated the renal EDH response in vivo in Wistar rats [17]. We also found that pre-treatment with apamin and TRAM-34 for 6 min significantly abolished the renal EDH response in vivo. Interestingly, after 4 min pre-treatment, the inhibitory effect of TRAM-34 and apamin was not significant. Also, there was no statistical significant difference between the EDH responses before treatment with the KCa channel blockers and after treatment. This makes the data somewhat difficult to interpret but we consider it likely that the combined blockade of SKCa and IKCa channels attenuate the EDH response also in vivo.
However, the comparison between our results and those of Edgley et al. deserves some consideration. Aside from using a different rat strain (Wistar), Edgley et al. administered ACh as a bolus while we used a 90-s infusion. It is possible that the importance of SKCa and IKCa channel may be different in this prolonged EDH response. Also, Edgley et al. found that only the peak response was inhibited. This peak response is not present in our experiments. Possibly, the prolonged EDH response depends on other mechanisms than the transient response. Also, they used a longer infusion time (10 min) for the inhibitors but, as shown in both our in vitro and in vivo experiments, also a shorter incubation time can significantly reduce the renal EDH response. Furthermore, Edgley et al. used the more unspecific charybdotoxin to inhibit IKCa channels while we used TRAM-34. In addition to IKCa channels, charybdotoxin also inhibits BKCa channels. If the renal EDH response also depends on BKCa channel activation, this would be detected by Edgley et al. but not by us.
It has been shown that isoflurane and other volatile anesthetics can decrease the EDH response [1, 25, 33, 34] possibly by a cytochrome P450-dependent pathway. To test this, we replaced the isoflurane anesthesia with pentobarbital. However, we did not find any significant changes in the NO/PGI2-dependent or EDH-induced renal vasodilation after pentobarbital anesthesia.
In conclusion, our results show that the EDH response in the rat renal vasculature in vitro is significantly affected by blockade of SKCa and IKCa channels and by blocking Kir channels and Na+/K+-ATPases. However, in vivo, we did not find evidence that extracellular K+ act as an EDH mediator in the renal vasculature. Hence, the true nature and the mechanisms behind the renal EDH-induced vasodilation are still unresolved and remain a topic of great interest to the research community.
References
Akata T, Nakashima M, Kodama K, Boyle WA III, Takahashi S (1995) Effects of volatile anesthetics on acetylcholine-induced relaxation in the rabbit mesenteric resistance artery. Anesthesiology 82:188–204
Boedtkjer E, Kim S, Aalkjaer C (2013) Endothelial alkalinisation inhibits gap junction communication and endothelium-derived hyperpolarisations in mouse mesenteric arteries. J Physiol 591:1447–1461
Boettcher M, de Wit C (2011) Distinct endothelium-derived hyperpolarizing factors emerge in vitro and in vivo and are mediated in part via connexin 40-dependent myoendothelial coupling. Hypertension 57:802–808
Brahler S, Kaistha A, Schmidt VJ, Wolfle SE, Busch C, Kaistha BP, Kacik M, Hasenau AL, Grgic I, Si H, Bond CT et al (2009) Genetic deficit of SK3 and IK1 channels disrupts the endothelium-derived hyperpolarizing factor vasodilator pathway and causes hypertension. Circulation 119:2323–2332
Brasen JC, Jacobsen JC, Holstein-Rathlou NH (2012) The nanostructure of myoendothelial junctions contributes to signal rectification between endothelial and vascular smooth muscle cells. PLoS One 7:e33632
Bussemaker E, Popp R, Binder J, Busse R, Fleming I (2003) Characterization of the endothelium-derived hyperpolarizing factor (EDHF) response in the human interlobar artery. Kidney Int 63:1749–1755
Bussemaker E, Wallner C, Fisslthaler B, Fleming I (2002) The Na-K-ATPase is a target for an EDHF displaying characteristics similar to potassium ions in the porcine renal interlobar artery. Br J Pharmacol 137:647–654
Chaytor AT, Evans WH, Griffith TM (1998) Central role of heterocellular gap junctional communication in endothelium-dependent relaxations of rabbit arteries. J Physiol 508(Pt 2):561–573
Chilton L, Loutzenhiser R (2001) Functional evidence for an inward rectifier potassium current in rat renal afferent arterioles. Circ Res 88:152–158
Chilton L, Loutzenhiser K, Morales E, Breaks J, Kargacin GJ, Loutzenhiser R (2008) Inward rectifier K+ currents and Kir2.1 expression in renal afferent and efferent arterioles. J Am Soc Nephrol 19:69–76
Crane GJ, Gallagher N, Dora KA, Garland CJ (2003) Small- and intermediate-conductance calcium-activated K+ channels provide different facets of endothelium-dependent hyperpolarization in rat mesenteric artery. J Physiol 553:183–189
De Vriese AS, Van DV, Lameire NH (2002) Effects of connexin-mimetic peptides on nitric oxide synthase- and cyclooxygenase-independent renal vasodilation. Kidney Int 61:177–185
de Wit C, Roos F, Bolz SS, Kirchhoff S, Kruger O, Willecke K, Pohl U (2000) Impaired conduction of vasodilation along arterioles in connexin40-deficient mice. Circ Res 86:649–655
de Wit C, Wolfle SE (2007) EDHF and gap junctions: important regulators of vascular tone within the microcirculation. Curr Pharm Biotechnol 8:11–25
DeFelice AF, Brousseau A (1988) Natriuretic and vasodilating activities of intrarenally administered atriopeptin II, substance P and bradykinin in the dog. J Pharmacol Exp Ther 246:183–188
Dora KA, Martin PE, Chaytor AT, Evans WH, Garland CJ, Griffith TM (1999) Role of heterocellular Gap junctional communication in endothelium-dependent smooth muscle hyperpolarization: inhibition by a connexin-mimetic peptide. Biochem Biophys Res Commun 254:27–31
Edgley AJ, Tare M, Evans RG, Skordilis C, Parkington HC (2008) In vivo regulation of endothelium-dependent vasodilation in the rat renal circulation and the effect of streptozotocin-induced diabetes. Am J Physiol Regul Integr Comp Physiol 295:R829–R839
Edwards G, Dora KA, Gardener MJ, Garland CJ, Weston AH (1998) K+ is an endothelium-derived hyperpolarizing factor in rat arteries. Nature 396:269–272
Edwards G, Feletou M, Weston AH (2010) Endothelium-derived hyperpolarising factors and associated pathways: a synopsis. Pflugers Arch 459:863–879
Ellinsworth DC, Earley S, Murphy TV, Sandow SL (2014) Endothelial control of vasodilation: integration of myoendothelial microdomain signalling and modulation by epoxyeicosatrienoic acids. Pflugers Arch 466:389–405
Falcone JC, Kuo L, Meininger GA (1993) Endothelial cell calcium increases during flow-induced dilation in isolated arterioles. Am J Physiol 264:H653–H659
Feletou M, Kohler R, Vanhoutte PM (2012) Nitric oxide: orchestrator of endothelium-dependent responses. Ann Med 44:694–716
Gauthier KM, Spitzbarth N, Edwards EM, Campbell WB (2004) Apamin-sensitive K+ currents mediate arachidonic acid-induced relaxations of rabbit aorta. Hypertension 43:413–419
Gebremedhin D, Kaldunski M, Jacobs ER, Harder DR, Roman RJ (1996) Coexistence of two types of Ca(2+)-activated K+ channels in rat renal arterioles. Am J Physiol 270:F69–F81
Iranami H, Hatano Y, Tsukiyama Y, Yamamoto M, Maeda H, Mizumoto K (1997) Halothane inhibition of acetylcholine-induced relaxation in rat mesenteric artery and aorta. Can J Anaesth 44:1196–1203
Jackson WF (2005) Potassium channels in the peripheral microcirculation. Microcirculation 12:113–127
Jiang F, Dusting GJ (2001) Endothelium-dependent vasorelaxation independent of nitric oxide and K(+) release in isolated renal arteries of rats. Br J Pharmacol 132:1558–1564
Jiang F, Li CG, Rand MJ (2000) Mechanisms of nitric oxide-independent relaxations induced by carbachol and acetylcholine in rat isolated renal arteries. Br J Pharmacol 130:1191–1200
Knight DS, Beal JA, Yuan ZP, Fournet TS (1987) Substance P-immunoreactive nerves in the rat kidney. J Auton Nerv Syst 21:145–155
Knight DS, Beal JA, Yuan ZP, Fournet TS (1987) Vasoactive intestinal peptide-immunoreactive nerves in the rat kidney. Anat Rec 219:193–203
Knight DS, Cicero S, Beal JA (1991) Calcitonin gene-related peptide-immunoreactive nerves in the rat kidney. Am J Anat 190:31–40
Ledoux J, Taylor MS, Bonev AD, Hannah RM, Solodushko V, Shui B, Tallini Y, Kotlikoff MI, Nelson MT (2008) Functional architecture of inositol 1,4,5-trisphosphate signaling in restricted spaces of myoendothelial projections. Proc Natl Acad Sci U S A 105:9627–9632
Lischke V, Busse R, Hecker M (1995) Inhalation anesthetics inhibit the release of endothelium-derived hyperpolarizing factor in the rabbit carotid artery. Anesthesiology 83:574–582
Loeb AL, Godeny I, Longnecker DE (1997) Anesthetics alter relative contributions of NO and EDHF in rat cremaster muscle microcirculation. Am J Physiol 273:H618–H627
Magnusson L, Sorensen CM, Braunstein TH, Holstein-Rathlou NH, Salomonsson M (2011) Mechanisms of K(+) induced renal vasodilation in normo- and hypertensive rats in vivo. Acta Physiol (Oxf) 202:703–712
Mink D, Schiller A, Kriz W, Taugner R (1984) Interendothelial junctions in kidney vessels. Cell Tissue Res 236:567–576
Mishra RC, Tripathy S, Desai KM, Quest D, Lu Y, Akhtar J, Gopalakrishnan V (2008) Nitric oxide synthase inhibition promotes endothelium-dependent vasodilatation and the antihypertensive effect of L-serine. Hypertension 51:791–796
Mulvany MJ, Halpern W (1977) Contractile properties of small arterial resistance vessels in spontaneously hypertensive and normotensive rats. Circ Res 41:19–26
Mustafa AK, Sikka G, Gazi SK, Steppan J, Jung SM, Bhunia AK, Barodka VM, Gazi FK, Barrow RK, Wang R, Amzel LM et al (2011) Hydrogen sulfide as endothelium-derived hyperpolarizing factor sulfhydrates potassium channels. Circ Res 109:1259–1268
Nilius B, Droogmans G, Wondergem R (2003) Transient receptor potential channels in endothelium: solving the calcium entry puzzle? Endothelium 10:5–15
Porter JP, Reid IA, Said SI, Ganong WF (1982) Stimulation of renin secretion by vasoactive intestinal peptide. Am J Physiol 243:F306–F310
Prysyazhna O, Rudyk O, Eaton P (2012) Single atom substitution in mouse protein kinase G eliminates oxidant sensing to cause hypertension. Nat Med 18:286–290
Sandow SL, Neylon CB, Chen MX, Garland CJ (2006) Spatial separation of endothelial small- and intermediate-conductance calcium-activated potassium channels (K(Ca)) and connexins: possible relationship to vasodilator function? J Anat 209:689–698
Shimokawa H (2014) 2014 Williams Harvey Lecture: importance of coronary vasomotion abnormalities—from bench to bedside. Eur Heart J 35:3180–3193
Si H, Heyken WT, Wolfle SE, Tysiac M, Schubert R, Grgic I, Vilianovich L, Giebing G, Maier T, Gross V, Bader M et al (2006) Impaired endothelium-derived hyperpolarizing factor-mediated dilations and increased blood pressure in mice deficient of the intermediate-conductance Ca2+-activated K+ channel. Circ Res 99:537–544
Simonet S, Isabelle M, Bousquenaud M, Clavreul N, Feletou M, Vayssettes-Courchay C, Verbeuren TJ (2012) KCa 3.1 channels maintain endothelium-dependent vasodilatation in isolated perfused kidneys of spontaneously hypertensive rats after chronic inhibition of NOS. Br J Pharmacol 167:854–867
Siren AL, Feuerstein G (1988) Cardiovascular effects of rat calcitonin gene-related peptide in the conscious rat. J Pharmacol Exp Ther 247:69–78
Sorensen CM, Braunstein TH, Holstein-Rathlou NH, Salomonsson M (2012) Role of vascular potassium channels in the regulation of renal hemodynamics. Am J Physiol Renal Physiol 302:F505–F518
Steendahl J, Holstein-Rathlou NH, Sorensen CM, Salomonsson M (2004) Effects of chloride channel blockers on rat renal vascular responses to angiotensin II and norepinephrine. Am J Physiol Renal Physiol 286:F323–F330
Taugner R, Kirchheim H, Forssmann WG (1984) Myoendothelial contacts in glomerular arterioles and in renal interlobular arteries of rat, mouse and Tupaia belangeri. Cell Tissue Res 235:319–325
Waeckel L, Bertin F, Clavreul N, Damery T, Kohler R, Paysant J, Sansilvestri-Morel P, Simonet S, Vayssettes-Courchay C, Wulff H, Verbeuren TJ et al (2015) Preserved regulation of renal perfusion pressure by small and intermediate conductance KCa channels in hypertensive mice with or without renal failure. Pflugers Arch 467:817–831
Wang D, Borrego-Conde LJ, Falck JR, Sharma KK, Wilcox CS, Umans JG (2003) Contributions of nitric oxide, EDHF, and EETs to endothelium-dependent relaxation in renal afferent arterioles. Kidney Int 63:2187–2193
Wang X, Loutzenhiser R (2002) Determinants of renal microvascular response to ACh: afferent and efferent arteriolar actions of EDHF. Am J Physiol Renal Physiol 282:F124–F132
Wang X, Trottier G, Loutzenhiser R (2003) Determinants of renal afferent arteriolar actions of bradykinin: evidence that multiple pathways mediate responses attributed to EDHF. Am J Physiol Renal Physiol 285:F540–F549
Wolfle SE, Schmidt VJ, Hoyer J, Kohler R, de Wit C (2009) Prominent role of KCa3.1 in endothelium-derived hyperpolarizing factor-type dilations and conducted responses in the microcirculation in vivo. Cardiovasc Res 82:476–483
Yamamoto Y, Imaeda K, Suzuki H (1999) Endothelium-dependent hyperpolarization and intercellular electrical coupling in guinea-pig mesenteric arterioles. J Physiol 514(Pt 2):505–513
Yi L, Morgan JT, Ragsdale SW (2010) Identification of a thiol/disulfide redox switch in the human BK channel that controls its affinity for heme and CO. J Biol Chem 285:20117–20127
Acknowledgments
The skillful technical assistance of Ms. Cecilia Vallin, Ms. Nadia Soori, and Mr. Kristoffer Racz is gratefully acknowledged. We acknowledge the Core Facility for Integrated Microscopy, Faculty of Health and Medical Sciences, University of Copenhagen. This study was supported by the Danish National Research Foundation, the Danish Heart Foundation, and the A.P Møller Foundation for the Advancement of Medical Sciences.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Rasmussen, K.M.B., Braunstein, T.H., Salomonsson, M. et al. Contribution of K+ channels to endothelium-derived hypolarization-induced renal vasodilation in rats in vivo and in vitro. Pflugers Arch - Eur J Physiol 468, 1139–1149 (2016). https://doi.org/10.1007/s00424-016-1805-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00424-016-1805-x