Abstract
We studied the potassium current flowing through TREK-1 channels in rat cardiac ventricular myocytes. We separated the TREK-1 current from other current components by blocking most other channels with a blocker cocktail. We tried to inhibit the TREK-1 current by activating protein kinase A (PKA) with a mixture of forskolin and isobutyl-methylxanthine (IBMX). Activation of PKA blocked an outwardly rectifying current component at membrane potentials positive to −40 mV. At 37 °C, application of forskolin plus IBMX reduced the steady-state outward current measured at positive voltages by about 52 %. Application of the potassium channel blockers quinidine or tetrahexylammonium also reduced the steady-state outward current by about 50 %. Taken together, our results suggest that the increase in temperature from 22 to 37 °C increased the TREK-1 current by a factor of at least 5 and that the average density of the TREK-1 current in rat cardiomyocytes at 37 °C is about 1.5 pA/pF at +30 mV. The contribution of TREK-1 to the action potential was assessed by using a dynamic patch clamp technique. After subtraction of simulated TREK-1 currents, action potential duration at 50 or 90 % repolarisation was increased by about 12 %, indicating that TREK-1 may be functionally important in rat ventricular muscle. During sympathetic stimulation, inhibition of TREK-1 channels via PKA is expected to prolong the action potential primarily in subendocardial myocytes; this may decrease the transmural dispersion of repolarisation and thus may serve to prevent the occurrence of arrhythmias.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
During each heartbeat, all cardiomyocytes in the mammalian heart are excited in a clearly defined order. Within the cardiac ventricles, the action potentials elicited in different regions largely overlap temporally, leading to successive and nearly synchronous contraction and relaxation of all ventricular myocytes, which is a prerequisite for the normal pump function of the heart. The configuration of the cardiac ventricular action potential shows considerable variation. Electrophysiological experiments with isolated hearts and isolated cardiac muscle preparations have shown that (i) action potential duration (APD) shows spatial variation; for example, action potentials are shorter in subepicardial myocytes than those in subendocardial myocytes [31, 32]. (ii) APD depends on stimulation frequency (even in the absence of sympathetic stimulation) [3, 21, 23, 31]. (iii) APD depends on sympathetic stimulation (even at a constant stimulation frequency) [2, 5, 6, 61]. (iv) Under physiological conditions, sympathetic stimulation increases heart rate. Thus, APD underlies a very complex spatio-temporal and humoral regulation.
Premature excitation of cardiomyocytes is prevented by the refractory period (which depends on APD). Since the heart is a highly excitable muscular tissue, arrhythmias can easily occur when the APD deviates from its normal value in a certain region of the heart at a certain time [35]. When the APD is too short, re-entry of cardiac excitation may be observed [45], which leads to atrial fibrillation, tachycardic ventricular arrhythmia or life-threatening ventricular fibrillation. When the APD is too long, torsade-de-pointes arrhythmias may be elicited [1], which also can cause sudden cardiac death. In large mammals such as humans, the heart is particularly prone to developing arrhythmias. This can be explained by the longer distances over which excitation has to propagate, by the greater difficulty of maintaining synchronisation and by the higher risk of aberrant excitation at ectopic foci in comparison to small animals. Accordingly, a number of monogenetic human channelopathies have a predominantly cardiac phenotype, for example the long-QT syndrome (resulting from a prolongation of the ventricular action potential) [47, 54] or the short-QT syndrome (resulting from a shortening of the ventricular action potential) [59].
The mechanisms underlying the regulation of APD have been studied extensively [32]. It is generally assumed that APD depends on the fine balance between inward and outward currents flowing during the plateau of the action potential. Two current components are especially sensitive to changes in heart rate and sympathetic stimulation: (i) the voltage-activated calcium current (I Ca; mainly carried by Cav1.2 and KCa3 channel proteins) [12, 22, 64] and (ii) the slow component of the delayed rectifier current (I Ks; carried by KvLQT channels, consisting of Kv7.1 plus KCNE1 channel proteins) [16, 42, 55, 62, 65]. However, in the human heart, there is another, possibly very large, current component that is regulated by stimulation of the sympathetic nervous system: the outward current flowing through TREK-1 channels (TWIK-related K+ channels) [14, 20, 24, 56]. This current component has not been adequately described so far in cardiac ventricular muscle. TREK-1 channels are known to be expressed in human atria and ventricles [15], and their expression is higher in subendocardial as compared to subepicardial myocytes [52, 68]. TREK-1 channels are stretch sensitive and may play a role in mechano-electric feedback in the heart [24]. Furthermore, TREK-1 channels are very temperature sensitive [17, 28] and can be inhibited via activation of protein kinase A (PKA) [9, 30, 34]. At present, the contribution of TREK-1 currents to the electrical activity of the human heart at 37 °C is poorly understood, and the outward current carried by TREK-1 channels is not normally included in any pathophysiological and therapeutic considerations. As a first step towards filling this gap in our knowledge, we have tried to quantify the current flowing through TREK-1 channels in rat cardiac ventricular muscle and to give an estimate of the contribution of these channels to the regulation of APD.
Materials and methods
Rats weighing 200–300 g were anaesthetised by evaporating a lethal concentration of isoflurane in a closed cage (2 ml liquid isoflurane/4 l air). When the righting reflex had subsided and nociceptive withdrawal reflexes could no longer be elicited by pinching the forepaws, the animals were decapitated and the heart was quickly excised. The experimental procedures were approved by the animal protection committee of Marburg University and by the Regierungspräsidium Giessen; the investigation conforms with the Directive 2010/63/EU of the European Parliament. The isolation of cardiomyocytes and patch-clamp experiments were performed as described previously [24, 37]. In brief, the aorta was attached to a cannula, and the coronary arteries were perfused for 10 min with HEPES-buffered physiological salt solution (PSS) at pH 7.4; the flow rate was 6–8 ml/min, the temperature was 37 °C. Subsequently, the heart was perfused for 5 min with a nominally Ca2+-free PSS and for further 9 min with Ca2+-free PSS to which collagenase (type II, Worthington; 70–90 mg/50 ml) was added. Then, the heart was incubated in ‘recovery solution’ [24] and minced with fine scissors; then the cardiomyocytes were dispersed by trituration with a glass pipette. The myocytes were used for patch clamping within 6 h of isolation.
For recording steady-state outward currents, we used holding potential of −30 mV to inactivate most of the voltage-activated sodium current (I Na) and the transient outward current (I to). From the holding potential, the membrane potential was stepped to +40 mV for 3.7 s to inactivate any residual I Na and I to. This depolarizing voltage step was followed by a slow ramp (−15 mV/s) from +40 to −100 mV to measure current voltage relation. Preliminary experiments showed that this ramp was slow enough for the current to reach a steady state at all potentials. The membrane capacitance was measured with fast voltage ramps (500 mV/s) [44]. Action potentials were elicited by brief current pulses (50 % above the threshold for initiation of an action potential) of 1-ms duration at a frequency of 1 Hz. Data acquisition was performed with an Axopatch 200B amplifier (Molecular Devices, Sunnyvale, CA, USA), an A/D converter (PCI-6052E, National Instruments), and software developed in our laboratory (PC.DAQ1.1). The sampling rate was 1 or 2 kHz. The experiments were either performed at room temperature (~22 °C) or at 37 °C.
A bath solution consisting of (mM) 3 KCl, 137 NaCl, 10 HEPES, 1 MgCl2, 1 CaCl2, 0.33 NaH2PO4, 2 Na-pyruvate, 10 glucose was used; the pH was adjusted to 7,4 with NaOH. The pipette solution consisted of (mM): 60 KCl, 65 K-glutamate, 5 EGTA, 3.5 MgCl2, 2 CaCl2, 3 K2ATP, 0.2 Na3GTP, 5 HEPES; the pH was adjusted to 7.2 with KOH. The resting potential of the cardiomyocytes under these conditions was -84.0 ± 0.3 mV at 37 °C (n = 73) and -80.3 ± 0.7 mV at RT (n = 18); this was significantly different p < 0.01. The average membrane capacitance was 107 ± 4 pF (n = 81). To separate the current flowing through TREK-1 channels (I TREK) from other current components, the cardiomyocytes were superfused with a blocker cocktail that eliminated the L-type Ca2+ current (I Ca; 1 μM nifedipine), the TASK-1 current (I TASK; 0.2 μM A1899), the ATP-sensitive K+ current (I KATP; 2 μM glibenclamide), the rapid voltage-activated K+ current (I Kr; 1 μM E-4031) and the slow voltage-activated K+ current (I Ks; 2 μM HMR1556). The inward rectifier channels were not blocked, and we carefully monitored the shape of the steady-state current-voltage relation during the experiment. There was always a negative slope conductance in the voltage range −60 to −30 mV. When, during the measurement, there were any indications that the access resistance had increased or the gigaseal had deteriorated, the results were discarded.
Dynamic patch-clamp [46, 66] measurements were performed using a custom-written program based on the system design software LabView (National Instruments, Austin, TX). We made full use of the capabilities of LabView. The analog membrane potential was measured at 1-ms intervals. After converting the analog voltage signal to a digital signal, a compensating current, which depended on the measured membrane potential and on the scaling factor described below, was injected into the cell. The compensating current was designed to subtract the current carried by TREK-1 channels (I TREK). I TREK was assumed to be instantaneous and to follow the Goldman–Hodgkin–Katz equation; after measuring the membrane capacitance of the cell, the simulated TREK-1 current was scaled to 1.5 pA/pF at +30 mV. This procedure mimics the specific block of I TREK during the action potential. Measurement of the membrane potential and update of the compensating current occurred in ~1 ms. A train of 30 action potentials at a stimulation rate of 1 Hz was elicited by injection of an inward current pulses of 1-ms duration. The last ten action potentials were used to determine APD at 50 % repolarisation (APD50) and at 90 % repolarisation (APD90) either under control conditions or under dynamic clamp conditions.
Data are reported as means ± s.e.m. Statistical significance was determined using Student’s t test. In the figures, significant differences to control values are marked by asterisks (*, p < 0.05; **, p < 0.01; ***, p < 0.001).
Results
Isolation of TREK-1 currents in rat cardiomyocytes
We tried to separate the TREK-1 current (I TREK) from other potassium currents flowing in rat ventricular cardiomyocytes at 37 °C by using a suitable voltage clamp protocol and by blocking most other current components with a blocker cocktail. In most experiments, the cardiomyocytes were superfused with a blocker cocktail (see “Materials and methods”) designed to eliminate the currents carried by TASK-1 channels (I TASK), KATP-channels (I KATP), voltage-activated K+ channels (I Kr and I Ks) and voltage-activated Ca2+ channels (I Ca). The blocker cocktail had no effect on TREK-1 channels expressed in H293 cells.
The voltage protocol (Fig. 1a) was designed to inactivate the voltage-activated sodium current (I Na) and most of the transient outward current (I to). The membrane potential was held at −30 mV and then stepped to +40 mV for 3.7 s. This depolarising voltage step from −30 to +40 mV activated a residual transient outward current that inactivated within ~3 s (Fig. 1b). It was followed by a slow ramp (−15 mV/s) from +40 to −100 mV which allowed us to measure the steady-state current voltage relation (see “Materials and methods”). Figure 1c shows the current voltage relation obtained in this way at 37 °C. The potassium concentration in the bath solution was 3 mM throughout. Compared to normal physiological salt solution, our salt solution containing only 3 mM K+ caused a shift of the peak outward current flowing through inward rectifier channels towards more negative potentials [57] and allowed a clearer separation between currents flowing through inward rectifier channels (Kir2.1 and Kir2.2) and the currents flowing through K2P-channels.
Typical current-voltage relation of a ventricular myocyte at 37 °C. a The voltage protocol and the corresponding whole-cell current recording; the ramp was slow enough (15 mV/s) for the current to reach a steady state at all potentials. The bath solution contained a blocker cocktail designed to eliminate I Kr, I Ks, I TASK, I KATP, and I Ca (see “Materials and methods”). b The currents recorded with the voltage protocol shown in a. c The ‘steady-state’ current-voltage relation derived from the recording shown in panels a and b
The temperature dependence of the steady-state current voltage relation in rat cardiomyocytes
It has been shown previously in whole-cell measurements and cell-attached patches that TREK-1 channels display a high thermosensitivity [17, 28]. The steady-state current voltage relation in the presence of the blocker cocktail also showed a pronounced temperature dependence (Fig. 2a). At 37 °C the steady-state outward current measured at +30 mV was 2.88 ± 0.20 pA/pF (n = 36); at room temperature, it was 1.13 ± 0.10 pA/pF (n = 14). The steady-state outward current increased with increasing depolarisation in the range −20 to +40 mV. The temperature-sensitive outward current (the difference between 37 °C and room temperature) measured at +30 mV was ~1.75 pA/pF. This current component probably consists mainly of TREK-1 because most other non-inactivating currents (including TASK-1) were blocked with the blocker cocktail. The transient outward current (I to) made only a very small contribution to the steady-state current voltage relation, as indicated by experiments in which 4-aminopyridine (4-AP), an inhibitor of I to, was added to the blocker cocktail. No significant difference between steady-state outward currents measured before and after application of 2 mM 4-AP could be detected (Fig. 2b); this was most likely related to the fact that I to was inactivated completely by the depolarising voltage step to +40 mV which preceded the voltage ramp.
Effects of temperature and 4-amino pyridine on the current-voltage relation; all solutions contained the blocker cocktail described above. a Steady-state current-voltage relations recorded at 37 °C (black curve; n = 36) and at room temperature (22–24 °C; blue curve; n = 14). b Effects of 4-AP on the steady-state current-voltage relation of rat cardiomyocytes at 37 °C; black curve, control; cyan: 5 min after application of 2 mM 4-AP (n = 8, paired). The difference between the currents measured before and after application of 4-AP was not statistically significant at any membrane potential (p > 0.05)
Block of steady-state outward current by activation of protein kinase A
It has long been known that TREK-1a currents can be inhibited by phosphorylation of residue S333 via PKA [30, 34, 56]. Residue S333 in human TREK-1a corresponds to residue S348 in human TREK-1b and to residue S344 in human TREK-1c [40]. We tried to obtain an estimate of the contribution of TREK-1 to the steady-state outward current by inhibiting it completely through activation of PKA. We used a combination of the PKA activator forskolin (10 μM) and the phosphodiesterase inhibitor isobutyl-methylxanthine (IBMX; 500 μM) to maximally activate PKA. Application of forskolin plus IBMX for 120 s at 37 °C inhibited an outwardly rectifying current component in the range −40 to +40 mV (Fig. 3a), as expected for TREK-1. At 37 °C, forskolin/IBMX inhibited 52.3 ± 7.7 % (n = 9) of the steady-state outward current at +30 mV (Fig. 3c). The residual current remaining after application of forskolin/IBMX was probably also a potassium current, but its molecular nature is currently unknown. At room temperature, application of forskolin/IBMX inhibited ~24 % of the steady-state outward current at +30 mV (Fig. 3b, d). Due to the relatively small current changes at +30 mV, this difference was not statistically significant in the paired t test (p = 0.057; n = 9). However, at +35 mV, the current change produced by forskolin/IBMX became significant (p = 0.042; n = 9).
Activation of protein kinase A. a Steady-state current voltage relation of cardiomyocytes before and 120 s after application of 500 μM IBMX plus 10 μM forskolin at 37 °C. b The same experiment at room temperature. c The fractional inhibition of the steady-state outward current produced by application of 500 μM IBMX plus 10 μM forskolin, by 400 μM quinidine and by 10 μM THA at 37 °C. d The fractional inhibition produced by the same drugs at 22 °C. The number of cardiomyocytes from which the data were obtained is indicated in brackets
Since only few currents are inhibited by activation of PKA, the effects of forskolin/IBMX probably provide a reliable estimate of the amplitude of the outward current carried by TREK-1 channels at 37 °C. Using a current density at +30 mV of 2.88 pA/pF and mean fractional inhibition of 52.3 %, we arrive at an estimate of 1.5 pA/pF at 37 °C (see “Discussion”). The current carried by TREK-1 currents at room temperature can be estimated in a similar way. Using a total current of 1.13 pA/pF at +30 mV and the apparent fractional inhibition of 24 %, we arrive at an estimate of 0.27 pA/pF. Thus, our results suggest that the TREK-1 current is at least 5 times larger at 37 °C than that at 22 °C.
Block of steady-state outward current by quinidine and tetrahexylammonium
To obtain a second estimate of the amplitude of the TREK-1 current in native rat cardiomyocytes, we used two drugs known to inhibit I TREK: quinidine [29, 34] and tetrahexylammonium (THA) [36]. This approach is not as straightforward as the activation of PKA because both drugs are not specific for TREK-1. Although most other potassium channels known to be expressed in rat cardiomyocytes had been eliminated by the blocker cocktail, the possibility remains that the blockers also inhibited a fraction of the residual current, whose nature is unknown. We tried to avoid blocking the inward rectifier channels, because the precise shape of the current voltage relation at potentials negative to −40 mV (mainly controlled by inward rectifier channels) is a useful indicator of the quality of the recordings and of the intactness of the cardiomyocytes (see “Materials and methods”). In heterologous expression systems, the IC50 for block of TREK-1 by quinidine has been estimated to be about 100 μM [27, 29]; thus, 800 μM quinidine should be sufficient to block TREK-1 currents almost completely. Preliminary experiments showed that application of 800 μM quinidine blocked more than 50 % of the outward current flowing at +30 mV, which is in good agreement with the data obtained with forskolin/IBMX (see above). However, application of 800 μM quinidine also blocked a fraction of the inward rectifier current, which made it difficult to judge the quality of the recordings. Application of 400 μM quinidine did not change the inward rectifier component of the current voltage relation and blocked an outwardly rectifying current flowing at potentials positive to −40 mV (Fig. 4a); this current component had a similar voltage dependence as the forskolin/IBMX-sensitive outward current described above (Fig. 3a). At 37 °C, application of 400 μM quinidine for 120 s inhibited 50.8 ± 1.9 % (n = 18) of the steady-state outward current flowing at +30 mV, consistent with the results obtained with forskolin/IBMX (Fig. 3c). The effects of quinidine reached a steady state within 2 min and were reversible (Fig. 4c). Application of 100 μM quinidine has a somewhat smaller effect; it inhibited ~38 % of the steady-state outward current at +30 mV. This finding suggests that the IC50 for the inhibitory effect of quinidine on TREK-1 in rat cardiomyocytes was well below 100 μM. Therefore, our results with 400 μM quinidine were used to obtain a second, independent estimate of the magnitude of TREK-1 currents in cardiomyocytes at 37 °C (see “Discussion”). At room temperature, the outward current inhibited by quinidine was much smaller than that at 37 °C, but it also showed outward rectification (Fig. 4b); on average, application of 400 μM quinidine at room temperature inhibited 58.2 ± 3.6 % (n = 9) of the outward current at +30 mV (Fig. 3d).
Application of quinidine and tetrahexylammonium. a The effect of application of 400 μM quinidine on the steady-state current-voltage relation at 37 °C. b The same experiment at room temperature. c Time course of the effect of 400 μM quinidine on the current measured at +30 mV. The arrow illustrates how the quinidine-sensitive current was measured
Application of 10 μM tetrahexylammonium (THA) also blocked an outwardly rectifying current component. At 37 °C, application of 10 μM THA blocked 49.4 ± 12.8 % (n = 4) of the steady-state outward current measured at +30 mV (Fig. 3c); at room temperature, application of 10 μM THA blocked 52.2 ± 6.8 % (n = 8) of the outward current (Fig. 3d). Thus, the values obtained with 400 μM quinidine and with 10 μM THA were very similar. We also tried to block the TREK-1 current with 200 μM fluoxetine [13]. However, this drug also inhibited a fraction of the inward rectifier current, and the effect on the outward current at positive potentials took several minutes to equilibrate. Therefore, fluoxetine appears to be less suitable for quantifying the current carried by TREK-1 channels in ventricular cardiomyocytes.
The possible effect of TREK-1 currents on action potential duration
To get more information on the functional importance of TREK-1 channels in rat ventricular myocytes, we analysed its influence on APD at 37 °C. We performed dynamic patch clamp experiments to simulate the consequences of TREK-1 channel inhibition [25, 66]. Action potentials were recorded in the current-clamp mode at a sampling rate of 1000 Hz, and TREK-1 currents were subtracted by injection of a compensatory current between the individual membrane potential measurements. The compensatory current injected through the patch electrode was calculated between individual voltage samples on the basis of a simulated TREK-1 current-voltage relation (see “Materials and methods”); it was assumed that the TREK-1 current was instantaneous and time independent. Despite these simplifications, this approach should allow a reasonable estimate of the contribution of TREK-1 to the configuration of the action potential.
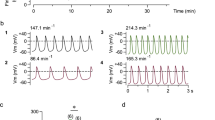
The cardiomyocytes were stimulated by brief (1 ms) current pulses through the patch electrode at a rate of 1 Hz at 37 °C. First, 30 consecutive action potentials were elicited under control conditions; subsequently, 30 action potentials were elicited under dynamic clamp conditions. After that, another 30 action potentials were elicited under control conditions (to test for possible slow changes in APD independent of any intervention); there were no significant changes between control and re-control. To eliminate the well-known changes in APD at the beginning of a stimulus train [3], we averaged only the last ten action potentials and determined the mean APD50 (APD at 50 % repolarisation) and APD90. A typical example of an averaged action potential recorded under control conditions (black curve) and under dynamic clamp conditions (magenta) is shown in Fig. 5a. APD was increased when the calculated TREK-1 current was subtracted (i.e., compensated by injection of an inverse current). The average changes in APD measured in 25 different cardiomyocytes is shown in Fig. 5b: APD50 was increased by 11.5 ± 2.1 % under dynamic clamp conditions (from 7.4 ± 0.9 to 8.3 ± 1.0 ms). APD90 was increased by 11.5 ± 1.4 % under dynamic clamp conditions (from 24.4 ± 1.5 to 27.2 ± 1.7 ms). The average resting potential was −84.7 ± 0.6 mV under control conditions and 84.2 ± 0.6 mV under dynamic clamp conditions. Thus, there was only a very small (but statistically significant; p < 0.01) change in resting potential, which was expected because the membrane conductance at rest is dominated by the inward rectifier current. In conclusion, dynamic patch clamp measurements predict that I TREK has a significant influence on APD in rat cardiomyocytes.
Dynamic patch clamp experiments mimicking the selective inhibition of I TREK. a Typical dynamic clamp measurement of a ventricular action potential in the steady state at a stimulation rate of 1 Hz; the temperature was 37 °C; the extracellular K+ concentration was 3 mM; no blocker cocktail was added. Black curve control; magenta dynamic subtraction of I TREK. b Statistical evaluation of the changes in APD50 and APD90 (n = 25) produced by the subtraction of the calculated I TREK
Discussion
TREK-1 channels are highly expressed in rodent and human cardiac muscle cells [10, 15, 24, 52], and single TREK-1 channels can easily be recorded from rat atrial or ventricular cardiomyocytes [19, 24, 56]. However, the outward current carried by TREK-1 channels (I TREK) is difficult to characterise because there are so many different potassium channels in cardiomyocytes. We have tried to isolate the TREK-1 current in rat cardiomyocytes at 37 °C under conditions where other steady-state currents (I TASK, I to, I Ca, I KATP, I Kr, and I Ks) were inhibited by a blocker cocktail.
First, we measured the steady-state outward current that could be blocked by activation of PKA, using forskolin (10 μM) and IBMX (500 μM) as tools to elevate intracellular cAMP. The fractional current inhibited by this combination of drugs was approximately 52 % (Fig. 3c). The two drugs, forskolin and IBMX, had only minor effects on the inward rectifier currents; the normal shape of the current-voltage relation negative to -40 mV served as a check of the quality of the cardiomyocytes. Because only very few potassium channels are known to be inhibited rapidly via PKA, these measurements allow a reasonable estimate of the steady-state current carried by TREK-1 channels at 37 °C. Taking into account the absolute current measured in the presence of the blocker cocktail at 37 °C (2.88 pA/pF), our data translate to a value of ~1.5 pA/pF for the TREK-1 current at +30 mV. The fractional inhibition of the outward current at room temperature by forskolin/IBMX, which was determined in a similar way, was ~24 %. Taking into account the absolute current measured at +30 mV (1.13 pA/pF), this translates to a TREK-1 current of ~0.27 pA/pF at room temperature. Thus, the change in temperature from 22 to 37 °C increased the TREK-1 current by factor of at least 5 in rat cardiomyocytes. This corresponds to a Q10 ≥ 3 but is still somewhat less than had been predicted on the basis of measurements in cell attached patches [17] or whole-cell measurements in heterologous expression systems [28].
Second, we measured the steady-state current that could be blocked by quinidine in the presence of the blocker cocktail. At 37 °C; the fractional current blocked by 400 μM quinidine was approximately 50 %. However, in view of our estimate of the IC50 for quinidine (<100 μM), it is possible that with 400 μM quinidine, the TREK-1 current was not blocked completely by application of 400 μM quinidine. This would lead to a slight underestimation of the TREK-1 current at 37 °C. On the other hand, we found that at room temperature, 400 μM quinidine had a larger effect than forskolin/IBMX (Fig. 3d). This finding is most likely attributable to the fact that quinidine also blocked a fraction of the residual current (which was unaffected by forskolin and IBMX), both at room temperature and at 37 °C. This may lead to a slight overestimation of the TREK-1 current at 37 °C. It may well be that the two relatively small errors described here may roughly cancel each other out. Similar considerations apply to the effects of THA. Despite these limitations, it is pleasing to note that our data obtained with the K+ channel blockers are in reasonable agreement with the data obtained with forskolin/IBMX at 37 °C (Fig. 3c). Taken together, our measurements suggest that the average current carried by TREK-1 channels represents about 50 % of the steady-state outward current that remained in the cardiomyocytes at positive potentials after removal of I TASK, I to, I Ca, I KATP, I Kr, and I Ks (Fig. 3c) and that the average amplitude of this current is about 1.5 pA/pF.
It should be noted, however, that the density of the net outward current measured at positive membrane potentials showed a considerable scatter from one cardiomyocyte to the next, probably because there is a gradient of the expression of TREK-1 channels across the ventricular wall [52]. In our experiments, we did not discriminate between myocytes coming from different regions in the ventricular wall; thus, the values given here represent averages across the entire wall thickness; the range of current densities observed in our experiments was 0.15 to 3.8 pA/pF.
We also tried to assess the effects of I TREK on the ventricular action potential. This was difficult because the blocker cocktail used for the isolation of TREK-1 also had a marked effect on APD and because there was no specific TREK-1 blocker available. Quinidine and THA are known to block other channels as well, and fluoxetine could not be used because it also partially inhibited the inward rectifier current in cardiomyocytes. Therefore, we chose to use a dynamic patch clamp system to obtain an estimate of the contribution of I TREK to the repolarisation of rat ventricular muscle. After eliciting an action potential, current pulses compensating for the TREK-1 current were injected into the cardiomyocytes at 1-ms intervals (see “Materials and methods”). After the subtraction of the calculated TREK-1 current, both APD50 and APD90 were increased by 11.5 %; this applies for action potentials in the steady state during continuous stimulation at a rate of 1 Hz. Thus, TREK-1 was clearly relevant for determining the rate of repolarisation in rat cardiac ventricular muscle. In rat atrium, a steady-state outward current has been measured that shares many properties with TREK-1 [2]. Application of 1 μM noradrenaline inhibited this TREK-like current and caused a distinct prolongation of the atrial action potential [2].
One of the conclusions that can be drawn from our experiments is that at potentials near the plateau I TREK in rat ventricular muscle is relatively large (1–2 pA/pF) in comparison to other potassium currents. If I TREK were of similar magnitude in the human heart, this would have some interesting functional implications:
-
1.
In the human cardiac ventricles, I TREK would be expected to have a much larger effect on APD than in the rat, because in larger mammals (who tend to have long action potentials), I to is not as dominant as in the rat, the plateau is relatively flat and the repolarisation is initiated by the relatively small voltage-activated outward currents I Kr and I Ks [32].
-
2.
The duration of the cardiac action potential shows a marked temperature dependence in many species [21, 26, 50, 58]. After cooling from 37 °C to room temperature, APD50 and APD90 of guinea pig and cat ventricular muscle increased by a factor of about 2 [50, 58]. Since both of these animal species have long ventricular action potentials, a large fraction of the effect of temperature on APD may be due to the temperature dependence of I TREK.
-
3.
A transmural gradient was found for the transient outward current [4, 8, 31]: I to is much larger in subepicardial than in subendocardial myocytes. The gradient in the density and inactivation properties of I to causes differences in the configuration of the action potential and may (indirectly) be responsible for the shorter APD observed in subepicardial myocytes compared to subendocardial myocytes [4, 8, 31]. A transmural gradient in the expression level of TREK-1 was found in rat [52] and porcine [68] heart; interestingly, this channel was found to be more strongly expressed in subendocardial than that in subepicardial myocytes. Such a transmural gradient of I TREK (subendocardial > subepicardial) would be expected to antagonise the effect of the transmural gradient in I to (subepicardial > subendocardial) on APD, i.e., it would make the difference in APD between subendocardial and subepicardial myocytes smaller.
-
4.
Opening of stretch-activated nonselective cation channels (SACs) constitutes one of the major pro-arrhythmic factors in the mammalian [11, 39, 54, 67]. TREK-1 is a (potentially anti-arrhythmic) stretch-activated K+ channel (SAK), and one of its major functions may be to counterbalance the inward current produced by SACs and thus to prevent the occurrence of ventricular extrasystoles during stretch of the ventricles at the end of the filling phase [18, 24] or during strong contractions. Interestingly, computer models of cardiac mechanics suggest that the mechanical strain both in systole and in diastole is much greater in the subendocardium than near the epicardial surface [18], in line with the gradient of expression of TREK-1.
-
5.
In cardiac ventricular muscle of humans and other mammals, adrenergic agonists can either cause an increase or a decrease in APD, depending on heart rate, species and experimental conditions. Activation of β-adrenergic receptors causes an increase in I Ks, mediated by activation of PKA [42], and this is expected to produce a decrease in APD [42, 55, 62]. In contrast, inhibition of I TREK, also mediated by activation of PKA [34, 43, 56], is expected to produce an increase in APD. In canine heart, stimulation of β-adrenergic receptors with isoprenaline produces a slight decrease in APD in subepicardial myocytes [41, 51]. In feline heart, isoprenaline produces a biphasic change in APD: an initial lengthening followed by a shortening [53]. In porcine heart, which is often used as a model for the human heart, isoprenaline causes a prolongation of the ventricular action potential [21], and similar results have been obtained in guinea pig heart [33, 38] and in cardiomyocytes from human hearts [6, 60]. This increase in APD caused by sympathetic stimulation may be at least partially due to inhibition of I TREK.
-
6.
The susceptibility of TREK-1 channels to inhibition via PKA would tend to increase APD mainly in subendocardial myocytes. Thus, it is tempting to speculate that sympathetic stimulation has differential effects on APD in different zones of the ventricle: The activation of I Ks may give rise to an overall shortening of the action potential, while the inhibition of TREK-1 might give rise to an increase in APD mainly in the subendocardial zone. At low levels of sympathetic stimulation, the increase in APD produced by inhibition of I TREK would probably outweigh the effect of activation of I Kr, consistent with the prolongation of the action potential observed in human, porcine and guinea-pig heart. At higher levels of sympathetic stimulation, the accompanying increase in heart rate is expected to lead to an overall shortening of the action potential (mediated by cumulative activation of I Kr and I Ks [3, 16] and by accumulation of extracellular K+ and intracellular Na+ ions [3, 7]) and a relative prolongation of APD in subendocardial myocytes due to inhibition of I TREK. The overall effect of strong sympathetic stimulation would then be an accentuation of the difference in APD between subendocardial and subepicardial cells, leading to a smaller transmural dispersion of repolarisation [1], and this may serve to minimise the propensity of the heart to arrhythmias. Thus, the inhibition of TREK-1 via PKA may play an important role in the adaptation of the electrical activity of the heart to sympathetic stimulation.
-
7.
Our hypothesis of a complementary function of I TREK and I Ks during sympathetic stimulation is supported by some clinical observations in long-QT syndrome (LQTS). The LQT1 subtype is caused by autosomal dominant or autosomal recessive mutations in the genes coding for subunits of Kv7.1 channels (KCNQ1 and KCNE), which are responsible for I Ks. When I Ks is reduced or eliminated, sympathetic stimulation is expected to elicit a prolongation of the action potential, due to inhibition of I TREK. Indeed, a ‘paradoxical QT prolongation’ during bolus administration of adrenaline has been discovered in LQT1 patients [63], and this has been widely used clinically as a screening procedure for the LQT1 subtype of the LQTS [47–49, 63] (with a specificity of 86 % for LQT1 versus non-LQT1 patients [63]). Furthermore, LQT1 patients have long been known to be most sensitive to sympathetic stimulation and much more prone to arrhythmias and sudden cardiac death during physical exercise than patients with other LQT subtypes. Accordingly, sudden cardiac death in LQT1 patients can be effectively prevented by β-receptor blockade [47]. It may well be that the paradoxical QT prolongation induced by adrenaline and the cardiac events triggered by physical exercise in LQT1 patients are at least partially attributable to inhibition of I TREK.
References
Antzelevitch C (2007) Role of spatial dispersion of repolarization in inherited and acquired sudden cardiac death syndromes. Am J Physiol Heart Circ Physiol 293:H2024–H2038
Bond RC, Choisy SC, Bryant SM, Hancox JC, James AF (2014) Inhibition of a TREK-like K+ channel current by noradrenaline requires both beta1- and beta2-adrenoceptors in rat atrial myocytes. Cardiovasc Res 104:206–215
Carmeliet E (2006) Action potential duration, rate of stimulation, and intracellular sodium. J Cardiovasc Electrophysiol 17(Suppl 1):S2–S7
Casis O, Iriarte M, Gallego M, Sanchez-Chapula JA (1998) Differences in regional distribution of K+ current densities in rat ventricle. Life Sci 63:391–400
Chandrasekera PC, Wan TC, Gizewski ET, Auchampach JA, Lasley RD (2013) Adenosine A1 receptors heterodimerize with beta1- and beta2-adrenergic receptors creating novel receptor complexes with altered G protein coupling and signaling. Cell Signal 25:736–742
Conrath CE, Opthof T (2006) Ventricular repolarization: an overview of (patho)physiology, sympathetic effects and genetic aspects. Prog Biophys Mol Biol 92:269–307
Daut J, Rüdel R (1982) The electrogenic sodium pump in guinea-pig ventricular muscle: inhibition of pump current by cardiac glycosides. J Physiol 330:243–264
Dixon JE, Shi W, Wang HS, McDonald C, Yu H, Wymore RS, Cohen IS, McKinnon D (1996) Role of the Kv4.3 K+ channel in ventricular muscle. A molecular correlate for the transient outward current. Circ Res 79:659–668
Enyeart JA, Danthi SJ, Enyeart JJ (2004) TREK-1 K+ channels couple angiotensin II receptors to membrane depolarization and aldosterone secretion in bovine adrenal glomerulosa cells. Am J Physiol Endocrinol Metab 287:E1154–E1165
Fink M, Duprat F, Lesage F, Reyes R, Romey G, Heurteaux C, Lazdunski M (1996) Cloning, functional expression and brain localization of a novel unconventional outward rectifier K+ channel. EMBO J 15:6854–6862
Franz MR, Cima R, Wang D, Profitt D, Kurz R (1992) Electrophysiological effects of myocardial stretch and mechanical determinants of stretch-activated arrhythmias. Circulation 86:968–978
Hartzell HC, Fischmeister R (1986) Opposite effects of cyclic GMP and cyclic AMP on Ca2+ current in single heart cells. Nature 323:273–275
Heurteaux C, Lucas G, Guy N, El Yacoubi M, Thummler S, Peng XD, Noble F, Blondeau N, Widmann C, Borsotto M, Gobbi G, Vaugeois JM, Debonnel G, Lazdunski M (2006) Deletion of the background potassium channel TREK-1 results in a depression-resistant phenotype. Nat Neurosci 9:1134–1141
Honore E (2007) The neuronal background K2P channels: focus on TREK1. Nat Rev Neurosci 8:251–261
Hund TJ, Snyder JS, Wu X, Glynn P, Koval OM, Onal B, Leymaster ND, Unudurthi SD, Curran J, Camardo C, Wright PJ, Binkley PF, Anderson ME, Mohler PJ (2014) beta(IV)-Spectrin regulates TREK-1 membrane targeting in the heart. Cardiovasc Res 102:166–175
Jespersen T, Grunnet M, Olesen SP (2005) The KCNQ1 potassium channel: from gene to physiological function. Physiology (Bethesda) 20:408–416
Kang D, Choe C, Kim D (2005) Thermosensitivity of the two-pore domain K+ channels TREK-2 and TRAAK. J Physiol 564:103–116
Kelly D, Mackenzie L, Hunter P, Smaill B, Saint DA (2006) Gene expression of stretch-activated channels and mechanoelectric feedback in the heart. Clin Exp Pharmacol Physiol 33:642–648
Kim D (1992) A mechanosensitive K+ channel in heart cells. Activation by arachidonic acid. J Gen Physiol 100:1021–1040
Kim D, Clapham DE (1989) Potassium channels in cardiac cells activated by arachidonic acid and phospholipids. Science 244:1174–1176
Laursen M, Olesen SP, Grunnet M, Mow T, Jespersen T (2011) Characterization of cardiac repolarization in the Göttingen minipig. J Pharmacol Toxicol Methods 63:186–195
Leroy J, Abi-Gerges A, Nikolaev VO, Richter W, Lechene P, Mazet JL, Conti M, Fischmeister R, Vandecasteele G (2008) Spatiotemporal dynamics of beta-adrenergic cAMP signals and L-type Ca2+ channel regulation in adult rat ventricular myocytes: role of phosphodiesterases. Circ Res 102:1091–1100
Li GR, Feng J, Yue L, Carrier M (1998) Transmural heterogeneity of action potentials and Ito1 in myocytes isolated from the human right ventricle. Am J Physiol 275:H369–H377
Li XT, Dyachenko V, Zuzarte M, Putzke C, Preisig-Müller R, Isenberg G, Daut J (2006) The stretch-activated potassium channel TREK-1 in rat cardiac ventricular muscle. Cardiovasc Res 69:86–97
Limberg SH, Netter MF, Rolfes C, Rinné S, Schlichthörl G, Zuzarte M, Vassiliou T, Moosdorf R, Wulf H, Daut J, Sachse FB, Decher N (2011) TASK-1 channels may modulate action potential duration of human atrial cardiomyocytes. Cell Physiol Biochem 28:613–624
Lin E, Ribeiro A, Ding W, Hove-Madsen L, Sarunic MV, Beg MF, Tibbits GF (2014) Optical mapping of the electrical activity of isolated adult zebrafish hearts: acute effects of temperature. Am J Physiol Regul Integr Comp Physiol 306:R823–R836
Lotshaw DP (2007) Biophysical, pharmacological, and functional characteristics of cloned and native mammalian two-pore domain K+ channels. Cell Biochem Biophys 47:209–256
Maingret F, Lauritzen I, Patel AJ, Heurteaux C, Reyes R, Lesage F, Lazdunski M, Honore E (2000) TREK-1 is a heat-activated background K+ channel. EMBO J 19:2483–2491
Meadows HJ, Benham CD, Cairns W, Gloger I, Jennings C, Medhurst AD, Murdock P, Chapman CG (2000) Cloning, localisation and functional expression of the human orthologue of the TREK-1 potassium channel. Pflugers Arch 439:714–722
Murbartian J, Lei Q, Sando JJ, Bayliss DA (2005) Sequential phosphorylation mediates receptor- and kinase-induced inhibition of TREK-1 background potassium channels. J Biol Chem 280:30175–30184
Näbauer M, Beuckelmann DJ, Überfuhr P, Steinbeck G (1996) Regional differences in current density and rate-dependent properties of the transient outward current in subepicardial and subendocardial myocytes of human left ventricle. Circulation 93:168–177
Nerbonne JM, Kass RS (2005) Molecular physiology of cardiac repolarization. Physiol Rev 85:1205–1253
Overholser BR, Zheng X, Tisdale JE (2008) Catecholaminergic effects on ventricular repolarization during inhibition of the rapid component of the delayed rectifier potassium current in a perfused heart model. Pharmacotherapy 28:1315–1324
Patel AJ, Honore E, Maingret F, Lesage F, Fink M, Duprat F, Lazdunski M (1998) A mammalian two pore domain mechano-gated S-like K+ channel. EMBO J 17:4283–4290
Patel C, Yan GX, Antzelevitch C (2010) Short QT syndrome: from bench to bedside. Circ Arrhythm Electrophysiol 3:401–408
Piechotta PL, Rapedius M, Stansfeld PJ, Bollepalli MK, Ehrlich G, Andres-Enguix I, Fritzenschaft H, Decher N, Sansom MS, Tucker SJ, Baukrowitz T (2011) The pore structure and gating mechanism of K2P channels. EMBO J 30:3607–3619
Putzke C, Wemhöner K, Sachse FB, Rinné S, Schlichthörl G, Li XT, Jae L, Eckhardt I, Wischmeyer E, Wulf H, Preisig-Müller R, Daut J, Decher N (2007) The acid-sensitive potassium channel TASK-1 in rat cardiac muscle. Cardiovasc Res 75:59–68
Quadbeck J, Reiter M (1975) Adrenoceptors in cardiac ventricular muscle and changes in duration of action potential caused by noradrenaline and isoprenaline. Naunyn Schmiedeberg's Arch Pharmacol 288:403–414
Ravens U (2003) Mechano-electric feedback and arrhythmias. Prog Biophys Mol Biol 82:255–266
Rinné S, Renigunta V, Schlichthörl G, Zuzarte M, Bittner S, Meuth SG, Decher N, Daut J, Preisig-Müller R (2014) A splice variant of the two-pore domain potassium channel TREK-1 with only one pore domain reduces the surface expression of full-length TREK-1 channels. Pflugers Arch 466:1559–1570
Ruzsnavszky F, Hegyi B, Kistamas K, Vaczi K, Horvath B, Szentandrassy N, Banyasz T, Nanasi PP, Magyar J (2014) Asynchronous activation of calcium and potassium currents by isoproterenol in canine ventricular myocytes. Naunyn Schmiedeberg's Arch Pharmacol 387:457–467
Sanguinetti MC, Jurkiewicz NK, Scott A, Siegl PK (1991) Isoproterenol antagonizes prolongation of refractory period by the class III antiarrhythmic agent E-4031 in guinea pig myocytes. Mechanism of action. Circ Res 68:77–84
Scamps F (1996) Characterization of a beta-adrenergically inhibited K+ current in rat cardiac ventricular cells. J Physiol 491(Pt 1):81–97
Schiekel J, Lindner M, Hetzel A, Wemhöner K, Renigunta V, Schlichthörl G, Decher N, Oliver D, Daut J (2013) The inhibition of the potassium channel TASK-1 in rat cardiac muscle by endothelin-1 is mediated by phospholipase C. Cardiovasc Res 97:97–105
Schmitt N, Grunnet M, Olesen SP (2014) Cardiac potassium channel subtypes: new roles in repolarization and arrhythmia. Physiol Rev 94:609–653
Sharp AA, O'Neil MB, Abbott LF, Marder E (1993) The dynamic clamp: artificial conductances in biological neurons. Trends Neurosci 16:389–394
Shimizu W, Horie M (2011) Phenotypic manifestations of mutations in genes encoding subunits of cardiac potassium channels. Circ Res 109:97–109
Shimizu W, Noda T, Takaki H, Kurita T, Nagaya N, Satomi K, Suyama K, Aihara N, Kamakura S, Sunagawa K, Echigo S, Nakamura K, Ohe T, Towbin JA, Napolitano C, Priori SG (2003) Epinephrine unmasks latent mutation carriers with LQT1 form of congenital long-QT syndrome. J Am Coll Cardiol 41:633–642
Shimizu W, Noda T, Takaki H, Nagaya N, Satomi K, Kurita T, Suyama K, Aihara N, Sunagawa K, Echigo S, Miyamoto Y, Yoshimasa Y, Nakamura K, Ohe T, Towbin JA, Priori SG, Kamakura S (2004) Diagnostic value of epinephrine test for genotyping LQT1, LQT2, and LQT3 forms of congenital long QT syndrome. Heart Rhythm 1:276–283
Shutt RH, Howlett SE (2008) Hypothermia increases the gain of excitation-contraction coupling in guinea pig ventricular myocytes. Am J Physiol Cell Physiol 295:C692–C700
Szentandrassy N, Kistamas K, Hegyi B, Horvath B, Ruzsnavszky F, Vaczi K, Magyar J, Banyasz T, Varro A, Nanasi PP (2014) Contribution of ion currents to beat-to-beat variability of action potential duration in canine ventricular myocytes. Pflugers Arch. doi:10.1007/s00424-014-1581-4
Tan JH, Liu W, Saint DA (2004) Differential expression of the mechanosensitive potassium channel TREK-1 in epicardial and endocardial myocytes in rat ventricle. Exp Physiol 89:237–242
Tatewaki T, Inagaki M, Kawada T, Shishido T, Yanagiya Y, Takaki H, Sato T, Sugimachi M, Sunagawa K (2003) Biphasic response of action potential duration to sudden sympathetic stimulation in anesthetized cats. Circ J 67:876–880
ter Bekke RM, Volders PG (2012) Arrhythmogenic mechano-electric heterogeneity in the long-QT syndrome. Prog Biophys Mol Biol 110:347–358
Terrenoire C, Clancy CE, Cormier JW, Sampson KJ, Kass RS (2005) Autonomic control of cardiac action potentials: role of potassium channel kinetics in response to sympathetic stimulation. Circ Res 96:e25–e34
Terrenoire C, Lauritzen I, Lesage F, Romey G, Lazdunski M (2001) A TREK-1-like potassium channel in atrial cells inhibited by beta-adrenergic stimulation and activated by volatile anesthetics. Circ Res 89:336–342
Trautwein W (1973) Membrane currents in cardiac muscle fibers. Physiol Rev 53:793–835
Trautwein W, Dudel J (1954) Action potential and mechanogram of cat's papillary muscle as a function of temperature. Pflugers Arch 260:104–115
Tristani-Firouzi M (2014) the long and short of it: insights into the short QT syndrome. J Am Coll Cardiol 63:1309–1310
Veldkamp MW, Verkerk AO, van Ginneken AC, Baartscheer A, Schumacher C, de Jonge N, de Bakker JM, Opthof T (2001) Norepinephrine induces action potential prolongation and early afterdepolarizations in ventricular myocytes isolated from human end-stage failing hearts. Eur Heart J 22:955–963
Volders PG (2010) Novel insights into the role of the sympathetic nervous system in cardiac arrhythmogenesis. Heart Rhythm 7:1900–1906
Volders PG, Stengl M, van Opstal JM, Gerlach U, Spatjens RL, Beekman JD, Sipido KR, Vos MA (2003) Probing the contribution of IKs to canine ventricular repolarization: key role for beta-adrenergic receptor stimulation. Circulation 107:2753–2760
Vyas H, Hejlik J, Ackerman MJ (2006) Epinephrine QT stress testing in the evaluation of congenital long-QT syndrome: diagnostic accuracy of the paradoxical QT response. Circulation 113:1385–1392
Walsh KB, Begenisich TB, Kass RS (1988) Beta-adrenergic modulation in the heart. Independent regulation of K and Ca channels. Pflugers Arch 411:232–234
Walsh KB, Kass RS (1988) Regulation of a heart potassium channel by protein kinase A and C. Science 242:67–69
Wilders R (2006) Dynamic clamp: a powerful tool in cardiac electrophysiology. J Physiol 576:349–359
Zabel M, Koller BS, Sachs F, Franz MR (1996) Stretch-induced voltage changes in the isolated beating heart: importance of the timing of stretch and implications for stretch-activated ion channels. Cardiovasc Res 32:120–130
Zhao LN, Fu L, Gao QP, Xie RS, Cao JX (2011) Regional differential expression of TREK-1 at left ventricle in myocardial infarction. Can J Cardiol 27:826–833
Acknowledgments
We thank Brigitte Burk for excellent technical support. This study was supported by the Deutsche Forschungsgemeinschaft (FOR 1086, TP7).
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is published as part of the special issue on K2P channels.
Rights and permissions
About this article
Cite this article
Bodnár, M., Schlichthörl, G. & Daut, J. The potassium current carried by TREK-1 channels in rat cardiac ventricular muscle. Pflugers Arch - Eur J Physiol 467, 1069–1079 (2015). https://doi.org/10.1007/s00424-014-1678-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00424-014-1678-9