Abstract
Purpose
This study aims to compare posterior retroperitoneal laparoscopic adrenalectomy (PRLA) and laparoscopic transperitoneal adrenalectomy (LTA) in adults using pan-European data as conflicting results have been published regarding length of hospital stay, institutional volume, and morbidity.
Methods
This retrospective cohort study analyzed data from the surgical registry EUROCRINE®. All patients undergoing PRLA and TLA for adrenal tumours and registered between 2015 and 2020 were included and compared for morbidity, length of hospital stay, and conversion to open surgery.
Results
A total of 2660 patients from 11 different countries and 69 different hospitals were analyzed and 1696 LTA were compared to 964 PRLA. Length of hospital stay was shorter after RPLA, with less patients (N = 434, 45.5%, vs N = 1094, 65.0%, p < 0.001) staying more than 2 days. In total, 96 patients (3.6%) developed a complication Clavien-Dindo grade 2 or higher. No statistical difference was found between both study groups. After propensity score matching, length of hospital stay was shorter after PRLA (> 2 days 45.2% vs 63.0%, p < 0.001). After multivariable logistic regression, factors associated with morbidity were age (OR 1.03), male sex (OR 1.52), and conversion to open surgery (OR 5.73).
Conclusion
This study presents the largest retrospective observational analysis comparing LTA and PRLA. Our findings confirm the shorter length of hospital stay after PRLA. Both techniques are safe leading to comparable morbidity and conversion rates.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Laparoscopic transperitoneal adrenalectomy (LTA) is routinely performed to remove most adrenal tumours [1]. The keyhole approach has led to significant pain reduction, a shorter length of hospital stay, faster recovery, and better cosmetic results, without increasing morbidity or operating times compared to open surgery [2, 3]. Posterior retroperitoneal laparoscopic adrenalectomy (PRLA) was introduced as a feasible alternative to LTA with equal clinical outcomes [4,5,6]. Possible advantages of PRLA compared to LTA include less pain, shorter time to oral intake, even shorter length of hospital stay, less significant incisional hernias, and avoiding the intraperitoneal space [7,8,9].
A recent state-of-the-art meta-analysis comparing both minimal access techniques found significantly less estimated blood loss and length of hospital stay [4]. Remarkably, this difference was not seen in more recent studies. Only 12 randomized and non-randomized single-centre studies with small sample sizes in a high-volume tertiary setting could be included in an overall analysis of 775 patients. Categorization of studies according to surgical or institutional volume could not be performed and two separate time periods as surrogate for the learning curve had to be used instead.
The conflicting results from these small sample size studies merit further evaluation, as a potentially shorter hospital stay can reduce healthcare costs. Moreover, surgeon and institutional volume impact the outcome of endocrine surgery, including adrenalectomy, but minimum volume thresholds have not been set [10, 11].
This study aims to analyze PRLA versus LTA in adults using pan-European data comparing the largest number of patients to date, focusing on morbidity, length of hospital stay, and the influence of institutional volume on surgical outcome.
Material and methods
Study cohort
All adult patients that underwent PRLA or TLA between January 2015 and December 2020, registered in EUROCRINE®, were included in the analysis. Patients without histopathology results were excluded. Robot-assisted cases and bilateral adrenalectomies were excluded as they present subgroups with possible different advantages and morbidity, and as they were unequally divided amongst both study groups [12]. EUROCRINE® is an online, endocrine surgical quality registry that initially focused on rare endocrine tumours but has evolved into a pan-European database collecting data on all endocrine surgical procedures. It has already led to several papers in the field of adrenal surgery [12, 13]. Data entry is not mandatory, but EUROCRINE® board members are responsible for assessment of compliance on national level. Every participating centre has signed a specific agreement for correct data entry. Quality control happens at local, national, and international level. The study was approved by the EUROCRINE® board and by the institutional ethics review board of Ege University, Izmir (15e2/10). Neither financial support nor any free devices were received from the industry.
Patient characteristics and other variables
Basic patient characteristics (age, sex, body mass index (BMI, kg/m2)) were collected. Preoperative characteristics included hormonal status (active, inactive), type of hormonal excess (aldosterone, cortisol, catecholamines, sex steroids), suspected malignancy on imaging and/or cytology, tumour side, and tumor size (mm). Operative characteristics included surgical technique, conversion to open surgery, and reasons for conversion. Conversion from either technique to open surgery was analyzed as “intention-to-treat”. Surgical centres were classified as experienced if at least 36 adrenal surgical procedures were reported (6 cases per year for 6 years in a row), according to the European Society of Endocrine Surgeons (ESES) consensus guidelines [11]. Postoperative characteristics included length of hospital stay (defined as the number of days in hospital after surgery, dichotomized at a threshold of 2 days), 30-day morbidity, hospital readmission, and 30-day all-cause mortality. In view of the information provided from predefined and free text data fields, all complications were categorized according to the Clavien-Dindo classification [14]. Also, histopathological outcomes and completeness of resection were collected.
The primary outcome was morbidity (Clavien-Dindo score of 2 or more). The secondary outcomes were length of hospital stay and conversion to open surgery. Sensitivity analyses were performed for patients with tumour sizes > 50 mm, patients with BMI > 30 kg/m2, patients with phaeochromocytoma, and according to side of the tumour as they present additional surgical and anatomical challenges. Threshold values were set based on previous studies [15,16,17].
Statistical analysis
The Shapiro–Wilk test was used to test normality of the numerical variables. Categorical continuous variables are reported as medians and interquartile ranges (IQR), and nominal variables as counts and percentages. Descriptive statistics were used to compare differences between patients that underwent PRLA and LTA, using the chi-square test, Fisher’s exact test, and the Mann–Whitney U test, as appropriate.
To identify associations between morbidity with preoperative and postoperative variables, forward stepwise (likelihood ratio) logistic regression analysis was conducted. Variables with associations p < 0.100 in univariate analysis were included in multiple logistic regression model to generate odds ratios (OR). For the logistic model, OR, 95% confidence intervals (CI), and associated p values are reported.
Propensity score matching was used to account for possible confounders on outcome [18]. Propensity scores (ranging from 0 to 1, the probability of a patient assigned to PRLA or LTA) were derived using a logistic regression model including age, sex, BMI, tumour size, centre experience, and hormonal excess status. One-to-one propensity score matching was performed by nearest neighbour matching within a calliper of 0.2. The balance of confounding variables between both groups of the matched data was assessed with standardized mean differences (SMD). SMD < 10% is a recommended threshold for reporting balance [18]. All statistical analyses were conducted using IBM SPSS Statistics for Windows (version 25.0, Armonk, NY) and R 3.6.3 open-source software with “MatchIt” package (http://www.R-project.org).
Results
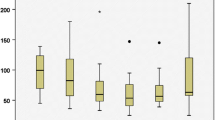
A total of 3780 patients were entered in the EUROCRINE® registry from 01/2015 to 12/2020, and 2660 patients from 11 different countries and 69 different hospitals met the criteria to be included in the study. Reasons for exclusion are summarized in Fig. 1. Of those, 1696 underwent an LTA (63.8%) and 964 a PRLA (36.2%). Patient, hospital, preoperative, and tumour characteristics are summarized in Table 1. In the overall cohort, median age was 54 (44–64) years, female-to-male was ratio 1.4, and median BMI was 27.2 (23.8–30.9) kg/m2 with 777 patients (30%) being obese. PRLA was more frequently performed in experienced centres, in female, younger, heavier patients, and in right-sided tumours. Most tumours (N = 1671, 62.8%) were hormonally active, with aldosterone (N = 767, 28.8%) being the most frequent hormone. More phaeochromocytomas and less cortisol-secreting tumours were operated via LTA (p < 0.001). Median tumour size was 33 (20–50) mm. In 844 patients (31.8%), a malignancy was suspected on imaging and/or cytology prior to surgery, whereas 206 patients (7.7%) underwent adrenal surgery for metastasis. Tumour size was the main indication for surgery in 283 patients (10.6%), with a median tumour size of 50 (40–63) mm in this subgroup. A conversion to open surgery was performed in 44 patients (1.7%), mainly because of bleeding (N = 20), difficult access (N = 12), unclear anatomy (N = 11), or adhesions (N = 5).
Surgical outcome, morbidity, and final histopathology are summarized in Table 2. In total, 96 patients (3.6%) developed a complication Clavien-Dindo grade 2 or higher. No statistical difference was found between both study groups. Most common complications were all-cause infections (N = 45, 1.7%), respiratory complications (N = 18, 0.7%), and haemorrhage requiring blood transfusion (N = 17, 0.6%).
Length of hospital stay was longer in the LTA group, with more patients staying over 2 days (N = 1094, 65.0% vs N = 434, 45.5%, p < 0.001). Thirteen patients (0.5%) were reoperated, and 40 patients (1.5%) had to be readmitted after discharge. The 30-day all-cause mortality was low (N = 4, 0.2%). Final histopathology showed 60 adrenocortical cancers (2.3%), 1382 adrenocortical adenomas (52.0%), and 546 phaeochromocytomas (20.5%).
Factors associated with morbidity (Clavien-Dindo grade 2 or higher) after adrenalectomy in the univariate logistic regression analysis included age, male sex, conversion to open surgery, and centre inexperience. After multivariable logistic regression analysis, age (OR 1.03, 95%CI 1.01–1.04, p = 0.002), male sex (OR 1.52, 95%CI 1.01–2.29, p = 0 0.047), and conversion to open surgery (OR 5.73, 95%CI 2.57–12.79, p < 0.001) were the only factors associated with morbidity (Clavien-Dindo grade 2 or higher) (Table 3).
Sensitivity analyses comparing LTA and PRLA showed a longer length of hospital stay after LTA in patients with BMI ≥ 30 kg/m2 (63.7% vs 50.2%, p < 0.001), with tumour size ≥ 50 mm (71.7% vs 47.7%, p < 0.001), and with phaeochromocytoma (77.9% vs 60.3%, p < 0.001). No differences in conversion rate were found in these subgroups (data not shown).
Sixty patients (39 LTA vs 21 PRLA) underwent surgery for adrenocortical cancer. PRLA was only performed in experienced centres (100%) in younger patients (44 vs 58 years old, p < 0.001) without differences in length of hospital stay (p = 0.465) or morbidity (Clavien-Dindo grade 2 or higher) (p = 0.537). Remarkably, in 185 patients (121 LTA and 64 PRLA) undergoing surgery for malignant adrenal tumours (other than adrenocortical cancer and phaeochromocytomas), length of hospital stay was not statistically different (p = 0.307), but morbidity (Clavien-Dindo grade 2 or higher) significantly higher after PRLA (15.6% vs 5.0%, p = 0.014).
Subgroup analysis according to side of the tumour showed that patients with left-sided tumours were slightly younger (54 vs 55 years old, p = 0.047), heavier (BMI ≥ 30 kg/m2, 33.7% vs 28.0%, p = 0.030), and operated more in experienced centres (87.8% vs 83.3%, p = 0.008) when operated via PRLA. Length of hospital stay was shorter (> 2 days, 41.6% vs 65.7%, p < 0.001) and morbidity (Clavien-Dindo grade 2 or higher) lower in the PRLA group (2.1% vs 4.4%, p = 0.035) (Supplementary Table S1). Patients with right-sided tumours were slightly younger (54 vs 55 years old, p = 0.010) and heavier (BMI ≥ 30 kg/m2, 33.6% vs 26.7%, p = 0.010) with smaller tumour sizes (≥ 50 mm 26.2% vs 31.9%, p = 0.037) when operated via PRLA. Length of hospital stay was shorter (> 2 days 47.4% vs 62.9%, p < 0.001) (Supplementary Table S2).
After propensity score matching, 865 patients could be included in both groups. The predefined possible confounding variables (age, sex, BMI, centre experience, and hormonal status) were equally distributed (SMD < 10%) (Supplementary Table S3). Length of hospital stay was shorter after PRLA (> 2 days, 45.2% vs 63.0%, p < 0.001). There was no significant difference between LTA and PRLA in terms of conversion rate, morbidity (Clavien-Dindo grade 2 or higher), wound infection, reoperation, or hospital readmission (Table 4).
Discussion
This European retrospective analysis of a prospective cohort compared 964 posterior retroperitoneal and 1696 transperitoneal laparoscopic adrenalectomies. Length of hospital stay was significantly shorter after PRLA. Overall morbidity (Clavien-Dindo grade 2 or higher) was low and comparable between both groups. Factors associated with morbidity after multivariable logistic regression included age, male sex, and conversion to open surgery. Sensitivity analysis for obesity (BMI ≥ 30 kg/m2), tumour size (≥ 50 mm), and phaeochromocytoma confirmed the shorter length of hospital stay after PRLA. The statistical significance of the shorter length of hospital stay after PRLA remained after propensity score matching.
The significant reduction in length of hospital stay after PRLA compared to LTA was previously found in a recent state-of-the-art meta-analysis analyzing 775 patients from 3 randomized controlled and 9 non-randomized comparative trials [4]. Possible explanations are reduced insufflation pressures and avoiding a pneumoperitoneum in PRLA [8]. In addition, avoiding surgical access to the retroperitoneum via the lumbar region with less sensitive skin innervation, the use of only 3 ports, and avoiding intra-abdominal dissection also might result in faster postoperative recovery [8]. The previous doubts on PRLA in larger tumour sizes and male/female differences were not confirmed by our subgroup analyses. In our series, the side of the adrenalectomy was not a risk factor for morbidity (including postoperative bleeding) in contrast with the findings of a recent meta-analysis including 780 patients with LTA.
Surgical volume and institutional volume have proven to impact outcomes after adrenalectomy [19, 20]. Moreover, a recent multicentre study evaluated hemodynamic instability during surgery for phaeochromocytoma via LTA and PRLA and noticed a significant inter-centre effect [21]. The previously mentioned meta-analysis could only include single-centre studies from high-volume, tertiary endocrine surgery units [4]. After propensity score matching for centre experience in our European series, morbidity remained comparable, and length of hospital stay remained shorter. No modifiable risk factors for morbidity could be identified.
In case of adrenalectomy for adrenal malignancies beyond phaeochromocytomas and adrenocortical cancers, no differences in length of hospital stay were found and significantly more morbidity after PRLA. This subgroup mainly includes surgery for adrenal metastases. To our knowledge, the increased morbidity after PRLA has not been previously reported and warrants further research.
To our knowledge, this is the largest, international, multicentre analyses of a recent surgical cohort based on a European quality registry. Data from high- and low-volume centres could be evaluated. Different subgroup analyses have confirmed the overall results.
Some limitations of this study are acknowledged. Data on specific surgeon experience within the high- and low-volume experienced centres is lacking. Length of hospital stay might be influenced by differences of healthcare reimbursement amongst the participating European countries. As other registries, EUROCRINE registry is prone to typing and coding errors, and missing data. No information on estimated blood loss, operative times, and healthcare costs was available. The type of complication data had been registered in the predefined and free text data fields for only 108 patients.
Both surgical techniques are feasible and safe and have a clear advantage on open surgery. The shorter length of hospital stay after PRLA is important as it can influence future healthcare and hospital ward planning, and it may subsequently reduce healthcare costs. However, prospective studies are necessary to confirm the health economic impact of a shorter length of hospital stay. Future studies should try to correct for surgeon experience, differences in operative times, and estimated blood loss.
Conclusion
This study presents the largest retrospective observational analysis comparing LTA and PRLA. Our findings confirm the shorter length of hospital stay after PRLA. Both techniques are safe leading to comparable morbidity and conversion rates.
Data availability
The data that support the findings of this study are available from the corresponding author, KV, upon reasonable request.
References
Assalia A, Gagner M (2004) Laparoscopic adrenalectomy. Br J Surg 91:1259–1274
Brunt LM (2002) The positive impact of laparoscopic adrenalectomy on complications of adrenal surgery. Surg Endosc 16:252–257
Li J, Wang Y, Chang X, Han Z (2020) Laparoscopic adrenalectomy (LA) vs open adrenalectomy (OA) for pheochromocytoma (PHEO): a systematic review and meta-analysis. Eur J Surg Oncol 46:991–998
Gavriilidis P, Camenzuli C, Paspala A et al (2021) Posterior retroperitoneoscopic versus laparoscopic transperitoneal adrenalectomy: a systematic review by an updated meta-analysis. World J Surg 45:168–179
Walz MK, Peitgen K, Hoermann R et al (1996) Posterior retroperitoneoscopy as a new minimally invasive approach for adrenalectomy: results of 30 adrenalectomies in 27 patients. World J Surg 20:769–774
Mercan S, Seven R, Ozarmagan S, Tezelman S (1995) Endoscopic retroperitoneal adrenalectomy. Surgery 118:1071–1075 discussion 1075-1076
Lee CR, Walz MK, Park S et al (2012) A comparative study of the transperitoneal and posterior retroperitoneal approaches for laparoscopic adrenalectomy for adrenal tumors. Ann Surg Oncol 19:2629–2634
Barczynski M, Konturek A, Nowak W (2014) Randomized clinical trial of posterior retroperitoneoscopic adrenalectomy versus lateral transperitoneal laparoscopic adrenalectomy with a 5-year follow-up. Ann Surg 260:740–747 discussion 747-748
Arezzo A, Bullano A, Cochetti G et al (2018) Transperitoneal versus retroperitoneal laparoscopic adrenalectomy for adrenal tumours in adults. Cochrane Database Syst Rev 12:CD011668
Gray WK, Day J, Briggs TWR et al (2021) Volume-outcome relationship for adrenalectomy: analysis of an administrative dataset for the Getting It Right First Time Programme. Br J Surg 108:1112–1119
Mihai R, Donatini G, Vidal O, Brunaud L (2019) Volume-outcome correlation in adrenal surgery-an ESES consensus statement. Langenbecks Arch Surg 404:795–806
Vatansever S, Nordenstrom E, Raffaelli M et al (2022) Robot-assisted versus conventional laparoscopic adrenalectomy: results from the EUROCRINE Surgical Registry. Surgery 171:1224–1230
Hallin Thompson L, Makay O, Brunaud L et al (2021) Adrenalectomy for incidental and symptomatic phaeochromocytoma: retrospective multicentre study based on the Eurocrine(R) database. Br J Surg 108:1199–1206
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Ragavan N, Selvaraj N, Raghavan D et al (2020) Robot assisted laparoscopic adrenalectomy: does size matter? Cureus 12:e9887
Agcaoglu O, Akbas M, Ozdemir M, Makay O (2019) The impact of body mass index on perioperative outcomes of robotic adrenalectomy: an update. Surg Innov 26:687–691
Brunaud L, Bresler L, Ayav A et al (2008) Robotic-assisted adrenalectomy: what advantages compared to lateral transperitoneal laparoscopic adrenalectomy? Am J Surg 195:433–438
Zhao QY, Luo JC, Su Y et al (2021) Propensity score matching with R: conventional methods and new features. Ann Transl Med 9:812
Greco F, Hoda MR, Rassweiler J et al (2011) Laparoscopic adrenalectomy in urological centres - the experience of the German Laparoscopic Working Group. BJU Int 108:1646–1651
Walz MK, Alesina PF, Wenger FA et al (2006) Posterior retroperitoneoscopic adrenalectomy–results of 560 procedures in 520 patients. Surgery 140:943–948 discussion 948-950
Vorselaars W, Postma EL, Mirallie E et al (2018) Hemodynamic instability during surgery for pheochromocytoma: comparing the transperitoneal and retroperitoneal approach in a multicenter analysis of 341 patients. Surgery 163:176–182
Acknowledgements
We would like to thank all participating clinics in the EUROCRINE database (https://eurocrine.eu) and all members of the EUROCRINE® council: David Scott-Coombes, Anders Bergenfelz, Thomas Clerici, Philipp Riss, Thomas Musholt, Erik Nordenström, Sam Van Slycke, Maurizio Iacobone, Laurent Brunaud, Marcin Barczynski, Konstantinos Nastos, Marco Raffaelli, Marit Helene Hansen, Christina Martinez Santos, Olov Norlén, Menno Vriens, Özer Makay, Fausto Palazzo, and Arnold Trupka.
Author information
Authors and Affiliations
Consortia
Contributions
Drs S. Vatansever and Ö. Makay had full access to all data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study conception and design: Drs K. Van Den Heede, S. Vatansever, and Ö. Makay.
Acquisition of data: Drs S. Vatansever and Ö. Makay.
Analysis and interpretation of data: All authors.
Drafting of manuscript: Dr K. Van Den Heede.
Critical revision of the manuscript: All authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Van Den Heede, K., Vatansever, S., Girgin, T. et al. Posterior retroperitoneal versus transperitoneal laparoscopic adrenalectomy in adults: results from the EUROCRINE® surgical registry. Langenbecks Arch Surg 408, 241 (2023). https://doi.org/10.1007/s00423-023-02975-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00423-023-02975-5