Abstract
Purpose
The use of a small circular stapler has been reported to increase the incidence of benign anastomotic stenosis in reconstruction. In circular stapling anastomosis after esophagectomy, the anastomotic lumen is dependent on the size of the esophagus and the replacement organ. We developed a new and foolproof method to prevent stenosis in esophagogastric tube anastomosis for patients with esophageal cancer that is not dependent on operator skill.
Methods
Seven patients with esophageal squamous cell carcinoma underwent minimally invasive McKeown esophagectomy in our hospital. Esophagogastric tube anastomosis was tried for all patients using the novel “hybrid esophagogastric tube anastomosis” technique. A 21-mm circular stapler was applied to perform an end-to-side anastomosis between the cervical esophagus and the posterior wall of the gastric tube. Then, a 30-mm linear stapler was positioned in the esophagogastric anastomosis formed by the 21-mm circular stapler with the anvil fork inserted into the esophagus and the cartridge fork inserted into the gastric tube. A supplementary side-to-side anastomosis of appropriately 15 mm was created. Afterward, the entry hole was closed with a linear stapler.
Results
The hybrid esophagogastric tube anastomosis was successful in all seven patients receiving it between June 2020 and March 2022. No postoperative complications related to this anastomosis were observed in any of the patients. Five patients underwent follow-up gastrointestinal endoscopy at 6 months after esophagectomy. No patient had an anastomotic stenosis.
Conclusions
Hybrid esophagogastric tube anastomosis can be performed easily and safely and can reduce the complications associated with anastomosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
McKeown esophagectomy with reconstruction using a gastric tube is considered the standard procedure for surgical treatment of resectable thoracic esophageal cancer [1]. However, anastomotic complications, including benign stenosis formation, continue to be the main problems after resection of esophageal cancer. These problems are associated with high mortality rates and often compromise patient quality of life [2, 3].
More effort has been devoted to reducing anastomotic complications in the most recent decade. Several authors reported that cervical linear stapler anastomosis was associated with a lower rate of anastomotic complications [4, 5]. If the cervical esophagus is shortened to secure the distance of the oral margin, the difficulty of esophagogastric tube anastomosis by linear stapler is definitely raised, and it is not always possible to create an anastomosis with a linear stapler [6]. Additionally, the anastomotic stoma formed by a linear stapled anastomosis is too large and can easily cause gastroesophageal reflux [7], resulting in patients possibly experiencing discomfort when swallowing after a cervical anastomosis due to an excessive residual end of the esophageal stump [8]. We believe that anastomosis with a circular stapler can provide stable anastomotic reconstruction without changing the difficulty of the anastomosis, even if the cervical esophagus is shortened to secure the distance of the oral margin.
When performing a circular stapled anastomosis, the esophageal stump does not need to be dissociated [6]. In addition, since a circular stapled anastomosis is closer to a normal digestive tract structure, the incidence of gastroesophageal reflux is significantly lower than that with a linear anastomosis, with no swallowing discomfort; however, the incidence of anastomotic fistula is not significantly different [9]. Wang et al. showed that an esophagogastric anastomosis created with a circular stapler could increase the rate of stenosis [10].
In this paper, we described a simple new anastomotic method to prevent stenosis, a weakness of the circular stapler, and secure the size of the anastomosis. We can easily perform this method in any situation when we perform esophagogastric tube anastomosis with a 21-mm circular stapler. We also describe the patients’ favorable postoperative courses.
Patients
Medical records of consecutive patients with primary esophageal cancer who underwent McKeown (three-incision) esophagectomy at Teikyo University Hospital, Mizonokuchi, between June 2020 and March 2022 were retrospectively reviewed. The patients comprised 5 males and 2 females with thoracic esophageal squamous cell carcinoma. The diagnosis for all patients was based on preoperative examinations including gastrointestinal endoscopy, upper gastrointestinal series, and a thoracic computed tomography scan. This study followed the principles of the 1964 Declaration of Helsinki and was approved by Teikyo University Institutional Review Boards. All patients received information about this study, including details of the treatment procedure, and provided written informed consent. Inclusion criteria were as follows: patients with histologically proven thoracic esophageal squamous cell carcinoma, tumor (cT1-3, N0-3, M0) that was surgically resectable by minimally invasive McKeown esophagectomy with cervical esophagogastric tube anastomosis, and Eastern Cooperative Oncology Group Performance Status 0 or 1. Patients were excluded if they were < 20 years old or unable to provide informed consent.
Surgical techniques
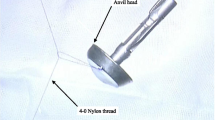
After the thoracic operation was completed, upper abdominal lymphadenectomy including the paracardial, lesser curvature, left gastric common hepatic, celiac, and splenic nodes was performed, and a gastric tube was prepared. A 35-mm-wide gastric tube was constructed along the lesser curvature of the stomach using 60-mm linear staples with an interrupted Lambert suture along the staple line. The gastric tube was pulled up through the posterior mediastinal route and extracted from the left neck incision for alimentary tract reconstruction. We used a 21-mm circular stapler because the anvil was small and easy to insert regardless of the size of the patient’s cervical esophageal lumen. The main body of the circular stapler was inserted into the gastric tube. Subsequently, an end-to-side esophagogastric tube anastomosis was performed by circular stapler (Fig. 1). Next, a 30-mm linear stapler was inserted caudally from the gastric tube stump and positioned in the esophagogastric tube anastomosis created by the circular stapler with the anvil fork inserted into the cervical esophagus and the cartridge fork inserted into the gastric tube (Fig. 2A, B). Insertion of the linear stapler was easy, and it only needed to be inserted far enough to create a supplementary side-to-side anastomosis of about 15 mm in length (Supplemental Video 1). Importantly, when inserting the linear stapler, the gastric tube should be pushed into the dorsal space of the remnant esophagus and anastomosed like an overlap anastomosis by pulling the posterior wall of the gastric tube over the posterior wall of the esophagus. We termed this anastomosis “hybrid esophagogastric tube anastomosis.” Finally, the gastric stump was closed with a linear stapler, and for reinforcement, several through-and-through sutures were placed at this anastomosis, especially at both the lesser and greater curvature lines of the anastomosis formed by the circular stapler and the crotch of the side-to-side anastomosis, for reinforcement, and the hybrid esophagogastric tube anastomosis was completed (Fig. 3 and Supplemental Video 2).
Use of the linear stapler. A The cartridge fork of the linear stapler is inserted into the gastric tube and the anvil fork is inserted into the remnant esophagus. B Actual view of a linear stapler insertion. The residual esophagus is indicated with the black arrow, and the reconstructed gastric tube is indicated with the white arrow
Results
We analyzed the short-term surgical outcomes of all 7 patients in whom we performed this anastomosis technique and the mid-term outcomes of the 5 patients who completed 6-month follow-up and underwent postoperative endoscopy at 6 months. The median age of the patients was 70.5 years old, and their clinicopathological characteristics are shown in Table 1. Four patients had middle thoracic esophageal squamous cell carcinoma, 2 patients had lower thoracic esophageal squamous carcinoma, and 1 patient had upper thoracic esophageal squamous cell carcinoma.
The operative data and the short- and mid-term outcomes are shown in Table 2. All patients underwent minimally invasive McKeown esophagectomy. The mean operative time was 459.8 min (range, 347–543 min), and the reconstructions were successful in all 7 patients. There were no problems associated with linear stapler insertion or the anastomosis, and this novel technique was completed safely. In addition, no leakage or stricture occurred at this anastomosis. The postoperative course of 6 of the patients was good. But oral intake was delayed until postoperative day 22 in the remaining patient because of unilateral recurrent laryngeal nerve palsy, whereas it was resumed within 7 days after surgery in the other 6 patients. The average postoperative hospital stay was 31.2 days.
The use of a proton pump inhibitor was recommended until 6 months postoperatively, and all patients continued the medication. A follow-up endoscopic examination performed at 6 months after surgery in 5 of the patients revealed a large hybrid esophagogastric anastomosis lumen (Fig. 4). There were 4 patients in this study that were more than 1 year postoperative. None of the patients had upper gastrointestinal endoscopic findings of anastomotic stenosis after more than 1 year. These patients also had no problems with oral intake.
Discussion
This report showed that our novel “hybrid esophagogastric tube anastomosis” was viable, could be performed safely, and resulted in satisfactory postoperative outcomes.
There are three methods of cervical esophagogastric tube anastomosis, hand-sewn anastomosis, linear stapler anastomosis, and circular stapler anastomosis, and each method has its advantages and disadvantages. The conventional hand-sewn anastomosis is both convenient and economical because expensive specialized instruments are not needed. However, its disadvantages are the long operative time, the need for a certain degree of surgical training, and the high risk of anastomotic leakage [6].
The linear stapler anastomosis, including the Collard method, is a side-to-side anastomosis. This technique prevents postoperative anastomotic stenosis by extension of the anastomosis along the sidewall of the esophagus, thereby avoiding the already narrowed esophageal lumen [5]. Nevertheless, anastomotic stenosis with the linear stapler occurs with a certain frequency, and there were no significant differences between the linear stapler anastomosis group and circular stapler anastomosis group in terms of time from esophagectomy until the first diagnosis of stricture or in the frequency of dilatation [11, 12]. Furthermore, the disadvantage of this anastomosis is that it requires a sufficient length of the remnant cervical esophagus to be anastomosed side-to-side. Hence, if the remnant esophagus is short, this anastomosis should be avoided [11].
Anastomosis with a circular stapler is considered to be a relatively simple procedure not dependent on operator skill level and results in a reduced length of surgical time [7]. However, anastomosis by this method has a high incidence of anastomotic stenosis, which can be a serious anastomotic complication after esophagectomy, and has a reported incidence ranging from 27 to 45% [8]. When creating an anastomosis by circular stapler, the lumen of the anastomosis depends on the size of the organs to be anastomosed [9]. In addition, the lumen of the cervical esophagus is small, and we have experienced difficulty in many Asian patients when attempting to insert an anvil larger than 21 mm. Due to the small size of the anvil head, the use of the 21-mm size, which is easy to insert into the cervical esophagus even if its length is short, causes anastomotic stricture with some frequency. Further, in the anastomosis created by the circular stapler, the anastomotic tissue is turned inward and fixed, such that the smooth muscles of both tissues are sandwiched and fixed between the esophageal mucosa and the gastric mucosa, which can result in an anastomotic stricture from associated scar formation [10]. To resolve this problem, we added a simple, clever technique by referring to the creativity of the anastomosis of the esophagojejunostomy in total gastrectomy and succeeded in reducing the rate of esophagogastric tube stenosis by circular stapler although the number of cases is still small [13].
In this report, we described a new method of performing an additional anastomosis with a linear stapler at the anastomosis site formed with a 21-mm circular stapler to prevent stenosis at the site of the esophagogastric tube anastomosis. The advantage of the hybrid esophagogastric tube anastomosis over other anastomotic methods is that the surgeon can anastomose with confidence because this is a simple, easy, and time-saving technique that is independent of operator skill. And the advantages also include avoidance of esophageal mucosal tearing associated with anastomosis-related complications due to insertion of an excessively large anvil to avoid anastomotic stricture [14], and sufficient blood flow to the remnant esophagus, contributing to a reduced risk of suture failure, since the neck esophagus does not need to be left longer than in the Collard method.
Although we use a linear stapler to add supplementary side-to-side anastomosis, it would not be difficult even if the cervical esophagus is short because a supplemental slit of about 15 mm would be sufficient. By adding a slit of about 15 mm, the area of the anastomotic ostium is roughly doubled, assuming that the circle formed by the circular stapler becomes an oval. To date, we have accomplished this procedure uneventfully in patients with esophageal cancer below the superior margin of the sternum.
So far, we have performed this anastomosis method in only 7 patients. No complications associated with the anastomosis have occurred. However, the limitations of this study are that the number of cases is small, and it is not a controlled study.
It remains to be determined which current major esophagogastric tube anastomosis method, that with circular stapler or linear stapler, is superior. The hybrid esophagogastric tube anastomosis that we devised is a novel method that compensates for the shortcomings of the esophagogastric tube anastomosis caused by the circular stapler method, and we consider it to be simple and not dependent on operator skill. Although analysis of the clinical results from well-planned randomized control trials of esophagogastric tube anastomosis techniques between circular stapler and linear stapler methods is required to determine which method is superior, the present study has shown satisfactory results.
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Change history
16 February 2023
A Correction to this paper has been published: https://doi.org/10.1007/s00423-023-02824-5
References
Hochwald SN, Ben-David K (2012) Minimally invasive esophagectomy with cervical esophagogastric anastomosis. J Gastrointest Surg 16:1775–1781
Kassis ES, Kosinski AS, Ross P Jr, Koppes KE, Donahue JM, Daniel VC (2013) Predictors of anastomotic leak after esophagectomy: an analysis of the society of thoracic surgeons general thoracic database. Ann Thorac Surg 96:1919–1926
Price TN, Nichols FC, Harmsen WS (2013) A comprehensive review of anastomotic technique in 432 esophagectomies. Ann Thorac Surg 95:1154–1161
Toh Y, Sakaguchi Y, Ikeda O et al (2009) The triangulating stapling technique for cervical esophagogastric anastomosis after esophagectomy. Surg Today 39:201–206
Collard JM, Romagnoli R, Goncette L, Otte JB, Kestens PJ (1998) Terminalized semimechanical side-to-side suture technique for cervical esophagogastrostomy. Ann Thorac Surg 65:814–817
Hsu HH, Chen JS, Huang PM, Lee JM, Lee YC (2004) Comparison of manual and mechanical cervical esophagogastric anastomosis after esophageal resection for squamous cell carcinoma: a prospective randomized controlled trial. Eur J Cardiothorac Surg 25:1097–1101
Honda M, Kuriyama A, Noma H, Nunobe S, Furukawa T (2013) Hand-sewn versus mechanical esophagogastric anastomosis after esophagectomy a systemic review and meta-analysis. Ann Surg 257:238–248
Furukawa Y, Hanyu N, Hirai K et al (2005) Usefulness of automatic triangular anastomosis for esophageal cancer surgery using a linear stapler (TA-30). Ann Thorac Cardiovasc Surg 11:80–86
Wang J, Yao F, Yao J, Xu L, Qian JL, Shan LM (2020) 21- versus 25-mm circular staplers for cervical anastomosis: a propensity-matched study. J Surg Res 246:427–434
Wang WP, Gao Q, Wang KN, Shi H, Chen LQ (2013) A prospective randomized controlled trial of semi-mechanical versus hand-sewn or circular stapled esophagogastrostomy for prevention of anastomotic stricture. World J Surg 37:1043–1050
Sugimura K, Miyata H, Matsunaga T et al (2019) Comparison of the modified Collard and hand-sewn anastomosis for cervical esophagogastric anastomosis after esophagectomy in esophageal cancer patients: a propensity score-matched analysis. Ann Gastroenterol Surg 3:104–113
Hayata K, Nakamori M, Nakamura M et al (2017) Circular stapling versus triangulating stapling for the cervical esophagogastric anastomosis after esophagectomy in patients with thoracic esophageal cancer: a prospective, randomized, controlled trial. Surgery 162:131–138
Fujimoto D, Taniguchi K, Kobayashi H (2020) A novel and simple esophagojejunostomy “Hybrid anastomosis” to prevent stenosis for patients with gastric cancer. Asian J Surg 43:711–712
Zhang S, Huang W, Liu X, Jian Li J (2017) Pilot study on preventing anastomotic leakage in stapled gastroesophageal anastomosis. Thorac cancer 9:142–145
Author information
Authors and Affiliations
Contributions
DF: data collection and drafting or revision of the manuscript. KT: study design. JT and FM: data analysis. HK: approval of the final version of the manuscript.
Corresponding author
Ethics declarations
Human rights statement
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1964 and later versions.
Informed consent
Informed consent was obtained from all patients included in this study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 117977 KB)
Supplementary file2 (MP4 311396 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fujimoto, D., Taniguchi, K., Takashima, J. et al. Hybrid esophagogastric tube anastomosis after minimally invasive McKeown esophagectomy to prevent stenosis in patients with esophageal cancer. Langenbecks Arch Surg 408, 7 (2023). https://doi.org/10.1007/s00423-022-02743-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00423-022-02743-x