Abstract
Purpose
Recurrent laryngeal nerve (RLN) injury is a feared complication of thyroid surgery occurring in 1–5% of cases. The present approaches to RLN preservation include RLN visualization with no nerve monitoring (No-NM), intermittent intra-operative nerve monitoring (I-IONM) and continuous intra-operative nerve monitoring (C-IONM). There is ambiguity as to which of these strategies should be the preferred method of RLN preservation.
Methods
A systematic review of the PubMed, Embase and the Cochrane Collaboration databases was undertaken with network meta-analysis (NMA) performed according to the PRISMA and Cochrane Collaboration guidelines. A Bayesian NMA was conducted using R packages netmeta with outcomes expressed as odds ratios (ORs) with 95% credible intervals (CrI). Only prospective studies were included.
Results
Eighteen studies met inclusion criteria, including 22,080 patients and 40,642 nerves at risk (NAR). Overall, 23,364 NARs (57.5%) underwent I-IONM, 17,176 (42.3%) No-NM and 98 (0.2%) underwent C-IONM. There were no significant differences between groups regarding the incidence of permanent RLN injury following thyroid surgery (I-IONM vs.No-NM, OR 0.84, 95% CrI 0.55–1.19; C-IONM vs. No-NM, OR 0.44, 95% CrI 0.02–5.00). Pooled analysis showed that IONM (I-IONM or C-IONM) demonstrated a protective effect versus No-NM in reducing the incidence of transient RLN injury (OR 0.75, 95% CI 0.59–0.97, p = 0.03).
Conclusions
IONM strategies did not significantly reduce the incidence of permanent RLN injury following thyroid surgery. However, the small number of C-IONM NARs limits conclusions that may be drawn. Further well-designed prospective studies will be required to definitively assess the utility of C-IONM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recurrent laryngeal nerve (RLN) injury leading to vocal cord palsy is a serious complication of thyroid surgery occurring in between 1 and 5% of cases [1, 2]. Unilateral RLN injury has implications for a patient’s quality-of-life by inducing voice changes (either permanent or transient), while bilateral nerve injury may be life threatening for patients and can necessitate emergency tracheostomy [3, 4]. As such, translational research efforts have focused on ways to either reduce unnecessary thyroid surgery [5] or ways to reduce the incidence of RLN injury as a complication of thyroid surgery.
In 1938, Lahey and Hoover were the first to highlight the necessity of RLN identification as routine during thyroid surgery as a strategy to significantly reduce RLN injury in their prospective analysis of 3000 consecutive patients [6]. The paradigm has since evolved. Recent advances now propose the use of intra-operative nerve monitoring (IONM) strategies which provide electro-myographic monitoring of the RLN during surgery [7]. Most commonly, IONM is performed using a stimulating probe intermittently (I-IONM) to both identify and confirm the functional integrity of the RLN. As such, I-IONM gained widespread acceptance over past 2 decades [8, 9]. Despite this, a major limitation of I-IONM use is its inability to detect impending RLN injury, as I-IONM can only detect RLN injury after the injury has occurred [10]. This shortcoming has facilitated the advent of continuous-IONM (C-IONM), which provides uninterrupted real-time functional monitoring of the RLN during thyroid surgery [11]. This is advantageous as C-IONM has the ability to inform resecting surgeon of imminent RLN injury; thus, in theory, preventing the surgeon performing the procedural steps putting the RLN at risk of injury.
Previous meta-analyses have demonstrated conflicting results regarding the benefit of I-IONM in reducing the incidence of RLN injury following thyroid surgery compared to No-NM [12,13,14]. A disadvantage of these standard pairwise meta-analyses is their inability to make comparisons between more than two nerve-monitoring strategies and C-IONM has never been directly compared to I-IONM or No-NM in a previous systematic review or meta-analyses analysing the prevention of RLN injury [10, 14,15,16]. An analysis of patients from 23 studies undergoing C-IONM during thyroid surgery by Ku et al. estimated an incidence of 2.26% (95% CI: 1.6–2.9) of transient RLN (T-RLN) palsy and 0.05% (95% CI: 0.08–0.2) for permanent RLN (P-RLN) palsy [17]. Additionally Kim et al. have demonstrated that C-IONM has a better ability to predict postoperative RLN injury versus I-IONM [18]. Network meta-analysis (NMA) methodology is required to fairly distinguish the role of C-IONM compared to I-IONM and No-NM, due to NMA allowing simultaneous comparison of all three of these approaches to RLN preservation [19, 20]. The aim of the present study was to perform a systematic review and NMA of prospective studies, comparing the efficacy of I-IONM, C-IONM and No-NM as methods of RLN preservation during thyroid surgery.
Methods
Search strategy
We performed a Systematic Review and NMA according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) for NMA [21] and Cochrane Handbook for Systematics Reviews of Interventions [22]. Institutional ethical review board approval was not required. This study was not preregistered.
A comprehensive search was performed using PubMed, Embase and the Cochrane Collaboration database using the following terms: ‘(thyroidectomy) ‘AND’ (nerve monitoring ‘OR’ nerve stimulation) ‘AND’ (RLN ‘OR’ recurrent laryngeal nerve ‘OR’ vagus ‘OR’ vocal cord)’. The most recent search was performed on the 30th of October 2021. Studies were limited to those published in the English language. Studies were not restricted based on year of publication. All duplicate studies were manually removed, before titles were screened and studies deemed appropriate had their abstracts reviewed. The full texts of remaining studies were then reviewed.
Inclusion and exclusion criteria
All randomised control trials (RCTs) or prospective observational studies addressing RLN injury in patients undergoing thyroid surgery. Studies were required to evaluate RLN function postoperatively in patients undergoing thyroid surgery using laryngoscopic evaluation. Studies were not limited based on timing of postoperative RLN assessment. We included studies reporting on a previously unreported group. Exclusion criteria were defined as follows: (1) any publication that was not an RCT or prospective observational study (e.g. retrospective cohort studies, case series, abstracts, guidelines, editorials, systematic reviews); (2) single-arm prospective studies; (3) studies not differentiating between I-IONM and C-IONM; (4) studies with no full English text.
Data extraction and quality assessment
Two independent reviewers independently reviewed the literature according to the predefined search strategy (E.F.C and M.G.D). Where discrepancies occurred a third reviewer arbitrated (M.J.K). Included full texts had the following data extracted: (1) title; (2) reference details (first author, journal, year, country); (3) study population characteristics; (4) number of patients in study; (5) number of nerves at risk (NAR); (6) mean age; (7) number of total thyroidectomies; (8) number of patients being treated for benign and malignant thyroid disease; (9) number of patients who had I-IONM, No-NM and C-IONM respectively); and (10) primary outcomes measures (i.e. rate of RLN injury, both transient and permanent).
Quality assessment of included studies was conducted by 2 reviewers independently (E.F.C and M.G.D). For RCTs, the Cochrane Risk of Bias for Randomized trials (RoB 2) [23] tool was used and for prospective observational studies, the Cochrane Risk of Bias In Non-Randomized Studies of Interventions (ROBINS-I) tool was used [24].
Definitions
-
1.
IONM: Use of a device to monitor the functional integrity of the RLN during thyroid surgery.
-
2.
I-IONM: Intermittent use of a stimulating probe to identify the RLN and intermittently confirm its integrity during thyroid surgery.
-
3.
C-IONM: Continuous monitoring of the RLN by using an automatic periodic stimulating probe placed on the ipsilateral vagus nerve during thyroid surgery.
-
4.
No-NM: Thyroid surgery carried out without the use of a RLN nerve monitoring device.
-
5.
NAR: Any RLN exposed to potential injury during thyroid surgery, e.g. during right thyroid lobectomy, only the right RLN is exposed and at risk. Therefore, 1 NAR for this procedure.
-
6.
RLN injury: Abnormal vocal cord movement detected on laryngoscopic evaluation following thyroid surgery.
-
7.
Transient RLN (T-RLN) injury: Impaired vocal cord movement recovering within 6 months.
-
8.
Permanent RLN (P-RLN) injury: Impaired vocal cord movement lasting greater than 6 months.
-
9.
Bilateral thyroid surgery (BTS): For the purposes of analysis, patients undergoing total thyroidectomy (TT) or Dunhills’ operation were classed as BTS as both recurrent laryngeal nerves were classified as at risk.
Statistical analysis
Descriptive studies and pooled values were used to analyse study characteristics. The incidence of RLN injury was expressed as a proportion of NARs. Our primary analysis compared the incidence of P-RLN injury between groups. Sensitivity analysis was then performed for this outcome evaluating RCTs and non-RCTs. We also analysed studies by incidence of T-RLN. NMA was conducted using R packages’ netmeta add-on (function netmeta) [25]. A random effects model was used for all study arms. The incidence of RLN injury was compared using odds ratios (ORs) from crude event data reported in the original articles. We plotted rank probabilities against possible ranks for all competing treatments. As per the Cochrane Handbook for systematic reviews of interventions, we applied a fixed count correction of 0.5 in the instances where no RLN injury was observed in either group within a study [26]. Effect sizes for the Bayesian NMA were described with 95% credible interval (CrI). Results were considered statistically significant at the p < 0.05 level if the 95% CrI did not include or cross the value of 1. To evaluate NMA result accuracy, assessment of consistency between all direct and indirect data was conducted and deemed inaccurate if indirect data differed by p > 0.05. Pooled analysis of IONM (incorporating I-IONM and C-IONM) vs. No-NM using RevMan (ver 5.4) software. Results were described as ORs using 95% confidence interval (CI) and again results were considered statistically significant at the p < 0.05 level.
Results
Literature search
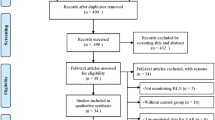
The initial search of PUBMED, EMBASE and Cochrane Collaboration resulted in a total of 969 studies identified with a further 4 studies identified through other sources. Following removal of 84 duplicates, 889 studies remained. These studies were then screened by title and abstract for relevance after which 43 studies remained and all had their full text analysed for eligibility. Finally, 18 studies remained for inclusion in the analysis as depicted by Fig. 1 [27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44].
Study characteristics
Eighteen studies from 9 different countries met inclusion and exclusion criteria with 8 RCTs [28, 29, 31, 33, 35, 38, 40, 42] and 10 prospective cohort studies [27, 30, 32, 34, 36, 37, 39, 41, 43, 44]. This included 22,080 patients undergoing thyroid surgery and 40,642 NARs. Sixteen studies reported patient gender: 924 patients were male (14.2%) and 5563 patients were female (85.8%) [27,28,29,30,31, 33,34,35,36,37,38,39,40,41,42, 44]. Among 17 studies reporting patients age, the mean age of patients was 53.1 years (range: 28.2–57.5 years) [27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42, 44]. Seventeen studies reported extent of thyroid surgery with 15,708 patients undergoing BTS (71.9%) [27,28,29,30,31,32,33, 35,36,37,38,39,40,41,42,43,44]. Similarly, 17 studies reported on thyroid pathology [27,28,29,30,31,32,33, 35,36,37,38,39,40,41,42,43,44], with 2001 patients (9.1%) having malignant thyroid pathology resected and 20,039 (90.9%) had benign thyroid pathology (Table 1). It was not possible to assess the impact of RLN examination timing on the incidence of RLN injury due to a lack of clarity on timing of RLN assessment in available data. Risk of bias assessment of included studies is outlined in Supplementary Material 1A and 1B.
Of the 40,642 NAR within this NMA, 23,364 (57.5%) underwent I-IONM, 17,176 (42.3%) did not have NM (No-NM) and 98 (0.2%) underwent C-IONM (Table 1). Fifteen studies compared I-IONM and No-NM groups [28,29,30,31,32,33, 35, 37,38,39,40,41,42,43,44], 2 studies compared I-IONM and C-IONM [34, 36], and 1 study compared all 3 groups (I-IONM vs. No-NM vs. C-IONM) [27]. The network plots for these studies are outlined in Supplementary Material 2. One study only reported rates of P-RLN injury [32]. Among the 98 patients undergoing C-IONM, no adverse events were reported during placement of the C-IONM vagus nerve stimulating probe [27, 34, 36].
Impact of nerve monitoring on permanent RLN injury
The overall incidence of P-RLN injury among all 18 studies was 0.9% (360/40,642 NARs). This represented an incidence of 0.8% for I-IONM (194/23,364), 1.0% for No-NM (165/17,176) and 1.0% for C-IONM (1/98). Overall, there was no difference in P-RLN injury rates at NMA among each of the nerve monitoring techniques (Fig. 2B), although there was a non-significantly reduced incidence of P-RLN injury in patients with I-IONM compared with No-NM (OR: 0.84; 95% CrI: 0.55–1.19). Conversely, there was lower incidence of P-RLN injury with C-IONM compared with I-IONM (OR: 0.53; 95%: CrI 0.02–5.47) (Fig. 2C). At NMA, C-IONM demonstrated a numerically lower but not significantly reduced incidence of P-RLN injury when compared to No-NM (OR: 0.44; 95% CrI: 0.02–5.00) (Fig. 2B). Deviance analysis for P-RLN injury is outlined in Supplementary Material 3. Pooled analysis of IONM vs. No-NM demonstrated a non-significant reduction in P-RLN injury following thyroid surgery (OR 0.86, 95% CI 0.70–1.06, p = 0.17) (Supplementary data 4).
Sensitivity analysis was subsequently performed to evaluate the impact of each method of nerve preservation for the prevention of P-RLN injury. In the 8 RCTs (all of which compared I-IONM to No-NM), there was no statistically significant benefit for I-IONM versus No-NM (OR 0.78; 95% CrI 0.22–2.81) (Fig. 3A). When evaluating the non-randomised studies, C-IONM was associated with a non-significant reduced incidence of P-RLN palsy in comparison to No-NM (OR 0.41; 95% CrI 0.01–6.25). Similarly, I-IONM was also associated with a non-significantly reduced incidence of P-RLN palsy in comparison to No-NM within these studies (OR 0.85; 95% CrI 0.47–1.35) (Fig. 3B).
Impact of nerve monitoring on transient RLN injury
As the study by Dralle et al. only reported P-RLN injury following thyroid surgery, this left 17 studies included for the analysis of T-RLN injury. The overall incidence of T-RLN injury reported among included studies was 2.3% (250/10,640 NARs). This represented an incidence of 2.1% for I-IONM (115/5532), 2.7% for No-NM (135/5010) and 0.0% for C-IONM (0/98). Overall, C-IONM did not significantly decrease the rate of T-RLN injury compared to No-NM (OR: 0.59, 95% CrI: 0.11–2.56) (Fig. 4B). Additionally, T-RLN injury was numerically although not significantly reduced following use of C-IONM compared with I-IONM (OR: 0.82; 95% CrI: 0.15–3.44) (Fig. 4C). The rate of T-RLN injury among the I-IONM group was lower in comparison to the No-NM group (OR 0.72; 95% CrI 0.50–1.05) (Fig. 4B). Deviance analysis for T-RLN injury is outlined in Supplementary Material 5. Pooled analysis of IONM (C-IONM or I-IONM) vs. No-NM revealed that IONM was associated with a significant reduction in the incidence of overall RLN injury (OR 0.75, 95% CI 0.59–0.97, p = 0.03) (Supplementary data 6).
Discussion
This systematic review and NMA are the first to compare all three major nerve monitoring techniques used to prevent unintentional RLN injury during thyroidectomy (C-IONM vs. I-IONM vs. No-NM). The present NMA includes only RCTs and prospective study data to best represent real-world results regarding RLN injury in thyroid surgery [45]. The present study incorporates over 22,000 patients and over 40,000 NARs and demonstrates a similar rate of P-RLN injury: C-IONM: 1.0% (1/98) vs. I-IONM: 0.8% (194/23,364) vs. No-NM: 1.0% (165/17,176) which was supported in the NMA (C-IONM Vs. No-NM: OR 0.44, p = NS; I-IONM vs. No-NM: OR 0.84, p = NS). Conversely, a stepwise increase was noted in T-RLN injury: C-IONM 0.0% (0/98) vs. I-IONM 2.1% (115/5532) vs. No-NM 2.7% (135/5010). Although this data may be interpreted to suggest routine use of C-IONM is an effective means of reducing T-RLN injury while not preventing P-RLN injury, the small sample size of nerves monitored using C-IONM (n = 98) must be recognised and acknowledged, limiting the conclusions which may definitively be drawn. Moreover, pooled analysis detailed that IONM (either I-IONM Or C-IONM) reduces the incidence T-RLN injury (OR 0.75, p = 0.03) but not P-RLN injury (OR 0.86, p = 0.17) in comparison to No-NM. Thus, while the present data is promising to suggest that C-IONM may reduce the incidence of T-RLN injury, it must be acknowledged that I-IONM is also superior to No-NM in this regard. However, it is apparent from the present analysis that neither C-IONM or I-IONM should be considered superior to No-NM in the prevention of P-RLN injury.
The present analysis demonstrated a reduction in T-RLN injury associated with the use of IONM overall (both I-IONM and C-IONM combined) versus No-NM during thyroid surgery (OR 0.75). Over the last two decades, I-IONM has gained widespread acceptance in thyroid surgery to reduce the incidence of RLN injury following thyroid surgery [8, 9]. IONM during thyroid surgery is recommended by the German Association of Endocrine Surgeons [46], Australian College of Surgeons [47] and International Intraoperative Neural Monitoring Study Group [7] in their expert consensus statements and guidelines. I-IONM provides reassurance and acts as a ‘comfort blanket’ to the operating surgeon by demonstrating the RLN functional integrity once located as well as detection of RLN injury post-operatively [48]. I-IONM also aids in the localization and identification of the RLN during thyroid surgery and in recent years, stimulating dissecting instruments have been introduced to further improve RLN identification through I-IONM [49, 50]. However, I-IONM is limited by one major inherent shortcoming. While I-IONM can successfully reassure the operating surgeon of the RLNs integrity, it is limited in that it only informs the surgeon of RLN damage once the injury has occurred [10]. Thus, the surgeon is unaware of the dangerous action prior to RLN injury. Lamadé et al. introduced C-IONM with the primary objective of overcoming this fundamental limitation of I-IONM [51]. C-IONM provides real-time monitoring of ipsilateral RLN function through indirect stimulation by a vagus nerve probe [10]. Thus, theoretically, dangerous operative action (e.g. excessive RLN traction, nerve compression or thermal injury) may be identified in real-time prompting the operating surgeon to reconsider their approach prior to RLN injury. However, some believe the practice of dissecting out and placing a stimulating probe on the ipsilateral vagus nerve to facilitate C-IONM is invasive, prolongs operative time and exposes the patient to risks, such as bradycardia, hypotension and even cardiac arrest [52, 53]. Additionally, system malfunction has limited the utility of C-IONM in previous small, retrospective series by Brauckhoff et al. although this is more likely to occur in the hands of a surgeon not familiar with the setup and use of C-IONM systems [54]. Consequently, due to the above reasons and a lack of available high level evidence, C-IONM is yet to gain widespread acceptance and consideration as a ‘gold standard’. Interestingly, within the 98 patients included in our analysis, no adverse events were noted during placement of the C-IONM vagus nerve stimulating probe. At present, it is evident that limitations still exist for both I-IONM and C-IONM during thyroid surgery [10], although both nerve monitoring techniques appear superior to No-NM in preventing T-RLN injury. Nevertheless, the benefit of IONM systems is not preserved in the reduction of P-RLN injury within this analysis, a finding consistent with previously published meta-analyses [14, 16, 55]. This supports the argument that IONM is no more than a ‘comfort blanket’ to inform the operating surgeon of the RLNs functional integrity at the end of the procedure. Additionally, previous studies have demonstrated the increased costs associated with IONM use versus No-NM in thyroid surgery [56]. In addition to this, C-IONM may be more expensive versus I-IONM due to the additional cost of the vagus nerve electrode. Further studies will be necessary to define the number needed to treat with I-IONM or C-IONM to prevent an additional RLN injury in order to give a better understanding of the cost effectiveness of these strategies. At present, without clear data to support the benefit of IONM in reducing the incidence of P-RLN injury or to support the cost-effectiveness of IONM, one may reasonably argue whether routine IONM use is justified and in particular whether exposing the patient to additional operative risk in the case of C-IONM is justified.
However, one could argue that a lack of evidence does not mean a lack of benefit. Although an underpowered analysis due to the small number of NARs in those with C-IONM and overall low incidence of RLN injury in this group (1/98), C-IONM did outperform both I-IONM and No-NM in the present NMA. Additionally, none of the studies utilising C-IONM was RCTs. Therefore, it is plausible that the actual clinical difference in RLN injury reduction in those undergoing C-IONM may have been underestimated or overestimated. In support of C-IONM, the recent work of Schneider et al. illustrates an advantage of using C-IONM over I-IONM in reducing the incidence of RLN injury following thyroid surgery in their recent large retrospective study [57]. This appears promising in surgeons plight to reduce the incidence of RLN during thyroid surgery and supports further investigation of this RLN monitoring strategy. Nonetheless, further well-designed, suitably powered, randomised controlled trials are necessary to fully establish the value of C-IONM in reducing RLN injury in order to accurately eliminate the inherent biases in retrospective studies. Due to a low incidence of RLN injury following thyroid surgery, previous studies have demonstrated that large sample sizes are required to either prove or disprove the utility of IONM during thyroid surgery [55], which renders performing well-designed RCTs a challenge to academic surgery. Owing to the low incidence of RLN injury following thyroid surgery, the large numbers of patients required to detect clinically relevant differences and the challenges in minimising local factors confounding RLN palsy rates, it is likely that large, multicenter collaborations seem the most fruitful means of achieving consensus in relation to this issue.
While the present systematic-review and NMA incorporates only the highest levels of evidence, it is subject to several inherent limitations. Firstly, as previously outlined, analysis in relation to the C-IONM group is underpowered, limiting the conclusions which may be drawn. Secondly, the volume of thyroid surgery performed by the operating surgeon has been demonstrated to be an important factor in the incidence of RLN injury [58, 59]. It was not possible to address this within the present NMA. The high variability in the number of patients in included studies (n = 32–16,448) may reflect overall high variations in the number of thyroid surgeries being performed by individual study authors, thereby confounding results within individual studies. In addition to this, the timing of laryngoscopic RLN evaluation may impact the incidence of RLN injury detected. ‘Early’ laryngoscopy (< 3–4 days postoperatively) is typically associated with a higher incidence of RLN injury detected. Due to a lack of available data, we were not able to assess the impact of laryngoscopic evaluation timing on the incidence of RLN injury detected. Another important point to consider is the impact of cancelled contralateral thyroid surgery owing to loss of nerve monitoring signal during thyroidectomy which may delay or prevent a necessary the contralateral surgery. This was not analysed by any of the included studies. Additionally the present study did not evaluate the benefit of IONM strategies in complex thyroid surgery such as reoperations and the identification of non-recurrent RLNs. IONM strategies may be of more benefit in these instances and future work is necessary to provide guidance in this area.
Conclusions
In conclusion, the present NMA of prospective studies demonstrated a benefit of I-IONM over No-NM in reducing the incidence of T-RLN injury following thyroid surgery. C-IONM may provide additional benefit when compared to I-IONM in this regard, although the paucity of available high level evidence regarding C-IONM (n = 98) limits this analysis. IONM (both I-IONM and C-IONM) failed to significantly reduce P-RLN injury incidence following thyroid surgery. The necessity for further prospective, suitably powered randomised controlled trials evaluating C-IONM is evident from the current NMA, before the consensus can be reached regarding the utility of C-IONM in thyroid surgery.
References
Wang TS, Sosa JA (2018) Thyroid surgery for differentiated thyroid cancer - recent advances and future directions. Nat Rev Endocrinol 14(11):670–683
Kasemsuwan L, Nubthuenetr S (1997) Recurrent laryngeal nerve paralysis: a complication of thyroidectomy. J Otolaryngol 26(6):365–367
Sanapala A, Nagaraju M, Rao LN, Nalluri K (2015) Management of bilateral recurrent laryngeal nerve paresis after thyroidectomy. Anesth Essays Res 9(2):251–253
Dralle H, Lorenz K, Machens A (2012) Verdicts on malpractice claims after thyroid surgery: emerging trends and future directions. Head Neck 34(11):1591–1596
Cleere EF, Davey MG, O'Neill S, Corbett M, O'Donnell JP, Hacking S, et al. Radiomic detection of malignancy within thyroid nodules using ultrasonography-a systematic review and meta-analysis. Diagnostics (Basel). 2022;12(4).
Lahey FH, Hoover WB (1938) Injuries to the recurrent laryngeal nerve in thyroid operations: their management and avoidance. Ann Surg 108(4):545–562
Randolph GW, Dralle H, International Intraoperative Monitoring Study G, Abdullah H, Barczynski M, Bellantone R et al (2011) Electrophysiologic recurrent laryngeal nerve monitoring during thyroid and parathyroid surgery: international standards guideline statement. Laryngoscope. 121(Suppl 1):S1-16
Ritter A, Ganly I, Wong RJ, Randolph GW, Shpitzer T, Bachar G et al (2020) Intraoperative nerve monitoring is used routinely by a significant majority of head and neck surgeons in thyroid surgery and impacts on extent of surgery-survey of the American Head and Neck Society. Head Neck 42(8):1757–1764
Feng AL, Puram SV, Singer MC, Modi R, Kamani D, Randolph GW (2020) Increased prevalence of neural monitoring during thyroidectomy: global surgical survey. Laryngoscope 130(4):1097–1104
Schneider R, Machens A, Randolph GW, Kamani D, Lorenz K, Dralle H (2017) Opportunities and challenges of intermittent and continuous intraoperative neural monitoring in thyroid surgery. Gland Surg 6(5):537–545
Stankovic P, Wittlinger J, Georgiew R, Dominas N, Hoch S, Wilhelm T (2020) Continuous intraoperative neuromonitoring (cIONM) in head and neck surgery-a review. HNO 68(Suppl 2):86–92
Cirocchi R, Arezzo A, D’Andrea V, Abraha I, Popivanov GI, Avenia N et al (2019) Intraoperative neuromonitoring versus visual nerve identification for prevention of recurrent laryngeal nerve injury in adults undergoing thyroid surgery. Cochrane Database Syst Rev. 1:012483
Davey MG, Cleere EF, Lowery AJ, Kerin MJ. 2022 Intraoperative recurrent laryngeal nerve monitoring versus visualisation alone - a systematic review and meta-analysis of randomized controlled trials. Am J Surg
Yang S, Zhou L, Lu Z, Ma B, Ji Q, Wang Y (2017) Systematic review with meta-analysis of intraoperative neuromonitoring during thyroidectomy. Int J Surg 39:104–113
Bai B, Chen W (2018) Protective effects of intraoperative nerve monitoring (IONM) for recurrent laryngeal nerve injury in thyroidectomy: meta-analysis. Sci Rep 8(1):7761
Pisanu A, Porceddu G, Podda M, Cois A, Uccheddu A (2014) Systematic review with meta-analysis of studies comparing intraoperative neuromonitoring of recurrent laryngeal nerves versus visualization alone during thyroidectomy. J Surg Res 188(1):152–161
Ku D, Hui M, Cheung P, Chow O, Smith M, Riffat F et al (2021) Meta-analysis on continuous nerve monitoring in thyroidectomies. Head Neck 43(12):3966–3978
Kim DH, Kim SW, Hwang SH (2021) Intraoperative neural monitoring for early vocal cord function assessment after thyroid surgery: a systematic review and meta-analysis. World J Surg 45(11):3320–3327
Jansen JP, Naci H (2013) Is network meta-analysis as valid as standard pairwise meta-analysis? It all depends on the distribution of effect modifiers. BMC Med 11:159
Mills EJ, Ioannidis JP, Thorlund K, Schunemann HJ, Puhan MA, Guyatt GH (2012) How to use an article reporting a multiple treatment comparison meta-analysis. JAMA 308(12):1246–1253
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71
Chaimani A. Undertaking network meta-analyses. 2021. In: Cochrane handbook for systematic reviews of interventions [Internet]. Cochrane Collaborative.
Sterne JAC, Savovic J, Page MJ, Elbers RG, Blencowe NS, Boutron I et al (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366:l4898
Sterne JA, Hernan MA, Reeves BC, Savovic J, Berkman ND, Viswanathan M et al (2016) ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 355:i4919
Schwarzer G. 2015. Meta-analysis with R.: Springer
Deeks JJH, J.; Altman, D.G. Analysing data and undertaking meta-analyses. 2022. In: Cochrane handbook for systematic reviews of interventions [Internet]. Internet: Cochrane Collaborative.
Adamczewski Z, Chwalkiewicz M, Lewinski A, Brzezinski J, Dedecjus M (2015) Continuous intraoperative neuromonitoring (CIONM) of the recurrent laryngeal nerve is sufficient as the only neuromonitoring technique in thyroidectomy performed because of benign goitre. Ann Agric Environ Med 22(3):495–498
Barczynski M, Konturek A, Cichon S (2009) Randomized clinical trial of visualization versus neuromonitoring of recurrent laryngeal nerves during thyroidectomy. Br J Surg 96(3):240–246
Barczynski M, Konturek A, Stopa M, Honowska A, Nowak W (2012) Randomized controlled trial of visualization versus neuromonitoring of the external branch of the superior laryngeal nerve during thyroidectomy. World J Surg 36(6):1340–1347
Chan WF, Lang BH, Lo CY (2006) The role of intraoperative neuromonitoring of recurrent laryngeal nerve during thyroidectomy: a comparative study on 1000 nerves at risk. Surgery. 140(6):866–872 (discussion 72-3)
Dionigi G, Boni L, Rovera F, Bacuzzi A, Dionigi R (2009) Neuromonitoring and video-assisted thyroidectomy: a prospective, randomized case-control evaluation. Surg Endosc 23(5):996–1003
Dralle H, Sekulla C, Haerting J, Timmermann W, Neumann HJ, Kruse E et al (2004) Risk factors of paralysis and functional outcome after recurrent laryngeal nerve monitoring in thyroid surgery. Surg 136(6):1310–1322
Ercetin C, Sahbaz A, Acar S, Tutal F, Aksakal N, Sari S, et al. 2018 Intraoperative nerve monitoring is useful for surgical training in thyroid surgery. Turk J Surg. 1–4.
Friedrich C, Ulmer C, Rieber F, Kern E, Kohler A, Schymik K et al (2012) Safety analysis of vagal nerve stimulation for continuous nerve monitoring during thyroid surgery. Laryngoscope 122(9):1979–1987
Hei H, Zhou B, Qin J, Song Y (2016) Intermittent intraoperative nerve monitoring in thyroid reoperations: preliminary results of a randomized, single-surgeon study. Head Neck 38(Suppl 1):E1993–E1997
Julien N, Ferrary E, Sokoloff A, Lamas G, Sterkers O, Bernardeschi D (2017) Vagal and recurrent laryngeal nerves neuromonitoring during thyroidectomy and parathyroidectomy: a prospective study. Eur Ann Otorhinolaryngol Head Neck Dis 134(2):77–82
Loch-Wilkinson TJ, Stalberg PL, Sidhu SB, Sywak MS, Wilkinson JF, Delbridge LW (2007) Nerve stimulation in thyroid surgery: is it really useful? ANZ J Surg 77(5):377–380
Maneeprasopchoke P, Chongkolwatana C, Pongsapich W, Iwata AJ, Kamani D, Randolph GW (2021) Intraoperative nerve monitoring in thyroid surgery: analysis of recurrent laryngeal nerve identification and operative time. Laryngoscope Investig Otolaryngol 6(2):354–361
Mirallie E, Caillard C, Pattou F, Brunaud L, Hamy A, Dahan M et al (2018) Does intraoperative neuromonitoring of recurrent nerves have an impact on the postoperative palsy rate? Results of a prospective multicenter study. Surg 163(1):124–129
Sari S, Erbil Y, Sumer A, Agcaoglu O, Bayraktar A, Issever H et al (2010) Evaluation of recurrent laryngeal nerve monitoring in thyroid surgery. Int J Surg 8(6):474–478
Stevens K, Stojadinovic A, Helou LB, Solomon NP, Howard RS, Shriver CD et al (2012) The impact of recurrent laryngeal neuromonitoring on multi-dimensional voice outcomes following thyroid surgery. J Surg Oncol 105(1):4–9
Teksoz S, Bukey Y, Ozcan M, Arikan AE, Ozyegin A (2015) Is nerve monitoring required in total thyroidectomy? Cerrahpasa experience. Indian J Surg 77(Suppl 2):466–471
Terris DJ, Anderson SK, Watts TL, Chin E (2007) Laryngeal nerve monitoring and minimally invasive thyroid surgery: complementary technologies. Arch Otolaryngol Head Neck Surg 133(12):1254–1257
Wojtczak B, Sutkowski K, Kaliszewski K, Glod M, Barczynski M (2017) Experience with intraoperative neuromonitoring of the recurrent laryngeal nerve improves surgical skills and outcomes of non-monitored thyroidectomy. Langenbecks Arch Surg 402(4):709–717
Burns PB, Rohrich RJ, Chung KC (2011) The levels of evidence and their role in evidence-based medicine. Plast Reconstr Surg 128(1):305–310
Dralle H, Lorenz K, Schabram P, Musholt TJ, Dotzenrath C, Goretzki PE et al (2013) Intraoperative neuromonitoring in thyroid surgery Recommendations of the Surgical Working Group for Endocrinology. Chirurg 84(12):1049–56
Serpell J, Sidhu S, Vallance N, Panizza B, Randolph G (2014) Consensus statement on intra-operative electrophysiological recurrent laryngeal nerve monitoring during thyroid surgery. ANZ J Surg 84(9):603–604
Thong G, Brophy C, Sheahan P (2021) Use of intraoperative neural monitoring for prognostication of recovery of vocal mobility and reduction of permanent vocal paralysis after thyroidectomy. Head Neck 43(1):7–14
Chiang FY, Lu IC, Chang PY, Sun H, Wang P, Lu XB et al (2015) Stimulating dissecting instruments during neuromonitoring of RLN in thyroid surgery. Laryngoscope 125(12):2832–2837
Zhang D, Li S, Dionigi G, Zhang J, Wang T, Zhao Y et al (2020) Stimulating and dissecting instrument for transoral endoscopic thyroidectomy: proof of concept investigation. Surg Endosc 34(2):996–1005
Lamade W, Meyding-Lamade U, Buchhold C, Brauer M, Brandner R, Uttenweiler V et al (2000) First continuous nerve monitoring in thyroid gland surgery. Chirurg 71(5):551–557
Almquist M, Thier M, Salem F (2016) Cardiac arrest with vagal stimulation during intraoperative nerve monitoring. Head Neck 38(S1):E2419–E2420
Terris DJ, Chaung K, Duke WS (2015) Continuous vagal nerve monitoring is dangerous and should not routinely be done during thyroid surgery. World J Surg 39(10):2471–2476
Brauckhoff K, Vik R, Sandvik L, Heimdal JH, Aas T, Biermann M et al (2016) Impact of EMG changes in continuous vagal nerve monitoring in high-risk endocrine neck surgery. World J Surg 40(3):672–680
Sanabria A, Ramirez A, Kowalski LP, Silver CE, Shaha AR, Owen RP et al (2013) Neuromonitoring in thyroidectomy: a meta-analysis of effectiveness from randomized controlled trials. Eur Arch Otorhinolaryngol 270(8):2175–2189
Rocke DJ, Goldstein DP, de Almeida JR (2016) A cost-utility analysis of recurrent laryngeal nerve monitoring in the setting of total thyroidectomy. JAMA Otolaryngol Head Neck Surg 142(12):1199–1205
Schneider R, Machens A, Sekulla C, Lorenz K, Elwerr M, Dralle H (2021) Superiority of continuous over intermittent intraoperative nerve monitoring in preventing vocal cord palsy. Br J Surg 108(5):566–573
Aspinall S, Oweis D, Chadwick D (2019) Effect of surgeons’ annual operative volume on the risk of permanent hypoparathyroidism, recurrent laryngeal nerve palsy and haematoma following thyroidectomy: analysis of United Kingdom Registry of Endocrine and Thyroid Surgery (UKRETS). Langenbecks Arch Surg 404(4):421–430
Lorenz K, Raffaeli M, Barczynski M, Lorente-Poch L, Sancho J (2020) Volume, outcomes, and quality standards in thyroid surgery: an evidence-based analysis-European Society of Endocrine Surgeons (ESES) positional statement. Langenbecks Arch Surg 405(4):401–425
Author information
Authors and Affiliations
Contributions
Study concept and design: all authors. Acquisition of data: E.F.C and M.G.D. Analysis and interpretation of data: all authors. Drafting manuscript: E.F.C and M.G.D. Critical revision of manuscript: all authors. All authors contributed significantly to this work and approved submission of the final version of this manuscript.
Corresponding author
Ethics declarations
Ethical approval
not required for this systematic review and meta-analysis.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cleere, E.F., Davey, M.G., Young, O. et al. Intra-operative nerve monitoring and recurrent laryngeal nerve injury during thyroid surgery: a network meta-analysis of prospective studies. Langenbecks Arch Surg 407, 3209–3219 (2022). https://doi.org/10.1007/s00423-022-02651-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-022-02651-0