Abstract
Background
Long-term outcomes in gastric cancer patients with positive lavage cytology (CY1) are generally poor. This multi-institutional retrospective cohort study aims to evaluate the clinical significance of the neutrophil–lymphocyte ratio (NLR) and the lymphocyte-monocyte ratio (LMR) in CY1 gastric cancer patients.
Methods
A total of 121 CY1 gastric cancer patients without other non-curative factors, who underwent macroscopically curative resection, were enrolled in this study. The cutoff values of preoperative NLR (pre-NLR), postoperative NLR (post-NLR), preoperative LMR (pre-LMR), and postoperative LMR (post-LMR) were defined by the Contal and O’Quigley method as 2.3, 3.0, 2.5, and 3.2, respectively. A Cox proportional hazard model was used to identify the independent prognostic factors among NLR, LMR, and other clinicopathological factors.
Results
There were significant differences in the overall survival (OS) between the two groups: high post-NLR groups vs. low post-NLR group (median survival time, months) (10.9 vs. 22.8, P = 0.006) and high pre-LMR group vs. low pre-LMR group (21.3 vs. 11.0, P = 0.001). The LMR value elevated significantly after gastrectomy (P = 0.020), although not in the NLR value (P = 0.733). On multivariate analysis, high post-NLR (hazard ratio = 1.506; 95% confidence interval = 1.047–2.167; P = 0.027), low pre-LMR (1.773; 1.135–2.769, 0.012), and no postoperative chemotherapy (1.558; 1.053–2.305, 0.027) were found to be independent prognostic factors for adverse OS.
Conclusions
Because a combination of high post-NLR and low pre-LMR may be an adverse prognostic marker in resectable CY1 gastric cancer patients, it is necessary to conduct a prospective trial to confirm a useful perioperative chemotherapeutic regimen for these patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastric cancer is still the third leading cause of cancer-related deaths in both sexes [1], although its incidence and associated mortality has been declining globally [2]. Positive results for peritoneal lavage cytology (CY1) in gastric cancer patients are associated with poor survival because of high incidences of peritoneal dissemination after surgery [3, 4]. The Japanese Gastric Cancer Association included CY1, which is classified as M1, as a key prognostic factor for diagnosing gastric cancer [5]. A prospective phase II study reported that radical gastrectomy followed by postoperative chemotherapy with tegafur-gimeracil-oteracil (S-1), as a single non-curative factor, showed relatively enhanced long-term survival in gastric cancer patients with CY1 [6, 7]. Therefore, recently published guidelines suggested that CY1, without other non-curative factors, can be managed by radical gastrectomy with D2 lymph node dissection combined with perioperative chemotherapy [8].
Although gastric cancer with CY1 is considered a candidate for surgery with curative intent, a convenient biomarker for this population is still unclear. Recently, the correlation between inflammation and malignant tumors has been well discussed [9,10,11,12]. Inflammation can be a potential therapeutic target for the treatment of neoplasms, and the peripheral blood count may reflect the tumor inflammatory condition [13]. Similar to other solid and hematological malignancies [10, 11, 14,15,16,17], high preoperative levels of neutrophil–lymphocyte ratio (NLR) and low levels of lymphocyte-monocyte ratio (LMR) were reported as negative prognostic factors for gastric cancer patients undergoing curative treatment [9, 13, 18, 19]. In addition, postoperative NLR is also considered a prognostic factor for patients undergoing curative gastrectomy [20,21,22]. However, no study has focused on the effect of NLR and LMR in CY1 gastric cancer patients undergoing R1 gastrectomy. Therefore, we conducted a multi-institutional retrospective cohort study to identify the prognostic significance of pre-/postoperative NLR and LMR in these patients.
Methods
Ethics statement and informed consent
This retrospective study protocol conformed to the provisions of the Declaration of Helsinki and was approved by the Institutional Review Board for the Use of Human Subjects at the Yokohama City Medical Center (approval number: B200500020), Yokohama City University School of Medicine (approval number: B200500039), and Yokohama Municipal Citizen’s Hospital (approval number: 19–09-04). According to the law of personal information protection, the survey items of this study for patients to give an opportunity to opt-out from this study were published in each institution (URL: https://www.yokohama-cu.ac.jp/amedrc/ethics/ethical/center_optout.html, https://www.yokohama-cu.ac.jp/amedrc/ethics/ethical/fuzoku_optout.html, https://yokohama-shiminhosp.jp/index.html).
Patients
From January 1992 to December 2018, a series of 6359 gastric cancer patients diagnosed with primary gastric adenocarcinoma underwent gastrectomy at the Department of Surgery of Yokohama City University Gastroenterological Center, Department of Gastroenterological Surgery, Yokohama City University Hospital, and the Department of Gastroenterological Surgery of Yokohama Municipal Citizen’s Hospital. In principle, peritoneal lavage cytology was performed for clinical T3 or T4a/b tumors, and as a result, a total of 1278 patients underwent peritoneal lavage cytology analysis. Of these, CY1 as a single non-curative factor was detected by intraoperative peritoneal lavage cytology performed at staging laparoscopy or during gastrectomy in 159 patients. A total of 121 patients were enrolled in this study because the leukocyte fraction data were not available from the medical records of 38 patients.
Surgery and chemotherapy
After exclusion of macroscopic peritoneal dissemination via laparotomy or staging laparoscopy, standard D2 gastrectomy was performed under curative intent. Neoadjuvant chemotherapy (NAC) was limitedly performed for clinical stage III tumors on the clinical trial settings, mainly for macroscopically type 4 and large type 3 tumors because this treatment is not standard in the Japanese Guidelines for the treatment of gastric cancer [23, 24]. In that cases, if positive lavage cytology was antecedently evidenced by the staging laparoscopy, NAC was performed before gastrectomy. Postoperative chemotherapy was performed for patients with good performance and nutritional status and those who provided informed consent. After the CCOG0301 study, S-1-based regimens were principally used as postoperative chemotherapy in this population [6].
Blood sample analyses
Preoperative NLR (pre-NLR) and LMR (pre-LMR) were defined as peripheral blood data obtained within a month before gastrectomy. Postoperative NLR (post-NLR) and LMR (post-LMR) were defined as peripheral blood data obtained at the time of chemotherapy initiation, or within 2 months after surgery if chemotherapy was not administered. Absolute counts of neutrophils, lymphocytes, and monocytes were calculated as the product of the percentage of each granulocyte and the total number of white blood cells [9].
Statistical analysis
Continuous variables are expressed as median values (interquartile ranges). The differences between pre-NLR and post-NLR values and pre-LMR and post-LMR values were compared using Student’s t-test. We measured overall survival (OS) from the date of surgery or, if performed, the date of the first administration of NAC to the date of the last follow-up. Relapse-free survival (RFS) was measured from the date of surgery to the date of recurrence. OS and RFS were calculated using the Kaplan–Meier method, and differences between groups were compared using the log-rank test.
To evaluate the differences between the high and low post-NLR groups and low and high pre-LMR groups, continuous variables were compared using Student’ s t-test, and categorical data were analyzed using the Chi-square test.
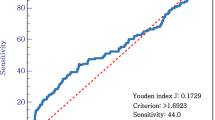
For multivariable analysis, we determined the optimal cutoff values of pre-/post-NLR and LMR, which maximize the log-rank test statistic of OS under a Cox proportional hazard model proposed by Contal and O’Quigley [25] as ROC analysis does not include the survival time. Multivariate survival analysis for OS using a Cox proportional hazard regression model included covariates that were selected by the Lasso method from the following factors: sex, age, tumor depth, histological type, administration of NAC, administration of adjuvant chemotherapy, pre-NLR, post-NLR, pre-LMR, and post-LMR. Using this method, the following candidate variables were selected: tumor depth, histological type, administration of postoperative chemotherapy, post-NLR, and pre-LMR.
All statistical analyses were performed using JMP® 13 (SAS Institute Inc., Cary, NC, USA) and R version 3.5.1 (R, Foundation for Statistical Computing, Vienna, Austria). Differences with probability values of P < 0.05 were considered significant.
Results
Patient characteristics
The demographics and tumor characteristics of the 121 CY1 patients are listed in Table 1. As every patient was diagnosed with stage IV disease, serosa invasion and lymph node metastasis were frequently observed; 110 patients (90.9%) had T4 tumor depth, and 112 patients (92.6%) had positive lymph node metastasis. A total of 85 patients (70.2%) had a histologically undifferentiated type of cancer. Neoadjuvant chemotherapy was administered to 24 patients (19.8%), and the chemotherapy regimens were as follows: S-1 in one patient, S-1 plus cisplatin in eight patients, S-1 plus oxaliplatin in two patients, S-1 plus docetaxel in three patients, S-1 plus docetaxel plus cisplatin in one patient, capecitabine plus cisplatin in one patient, and fluorouracil plus cisplatin in eight patients. Postoperative chemotherapy was administered to 84 patients (69.4%), and the chemotherapy regimens were as follows: S-1 in 65 patients, S-1 plus oxaliplatin in three patients, S-1 plus trastuzumab in two patients, S-1 plus docetaxel in one patient, irinotecan plus cisplatin in three patients, docetaxel plus cisplatin in two patients, and other regimens in eight patients. The reasons for the omission of postoperative chemotherapy were as follows: therapy rejection for six patients, early recurrence before chemotherapy in three patients, medical conditions in three patients (Parkinson’s disease, dermatomyositis, and mental disease, respectively), adverse effects in two patients, others in four patients (mixed type of neuroendocrine carcinoma, administration of intra-peritoneal chemotherapy, poor nutrition, and no cancer notification, respectively), and unknown reasons (by medical records survey) in 17 patients.
Changes in NLR and LMR after surgery
LMR was significantly elevated after surgery, although there was no significant change in NLR after surgery (Table 2).
OS and cause of death
The median survival time (MST) of all enrolled patients was 16.8 months (95% confidence interval [CI] 14.2–22.8). During this study, 94 patients (77.7%) died of gastric cancer recurrence, and three patients (2.5%) died of other diseases (brain infarction in one patient, dermatomyositis in one patient, and renal cell cancer in one patient). Of these, 73 patients (60.3%) had peritoneal dissemination, 19 patients (15.7%) had lymph node metastasis, 10 patients (8.3%) had liver metastasis, three patients (2.5%) had lung metastasis, two patients (1.7%) had bone metastasis, and two patients (1.7%) had brain metastasis.
Optimal cutoff values of pre-/post-NLR and LMR
As mentioned above, the cutoff value that maximizes the log-rank test statistic of the OS rate was calculated. The optimal cutoff values (95% CI) were detected as 2.3 (1.4–5.6), 3.0 (2.8–3.6), 2.5 (2.5–5.4), and 3.2 (2.7–7.1) for pre-NLR, post-NLR, pre-LMR, and post-LMR, respectively.
Prognostic significance of pre-/post-NLR and LMR
For clarifying the effects of pre-NLR, post-NLR, pre-LMR, and post-LMR on long-term prognosis, patient survival, classified according to the cutoff value, was compared in each ratio group at the same phase. As shown in Fig. 1, low post-NLR and high pre-LMR significantly affected favorable prognosis.
Kaplan–Meier plots of overall survival. a There was no significant difference in survival between the high pre-NLR group (≥ 2.3) (n = 68) and the low pre-NLR group (< 2.3) (n = 53) (MST [month]: 14.7 vs. 22.8, P = 0.145). b The high post-NLR group (≥ 3.0) (n = 41) showed worse survival compared with the low post-NLR group (< 3.5) (n = 80) (MST [month]: 10.9 vs. 22.8, P = 0.006). c The low pre-LMR group (< 2.5) (n = 23) showed worse survival compare with the high pre-LMR group (≥ 2.5) (n = 98) (MST[month]: 21.3 vs. 11.0, P = 0.001). d There was no significant difference in survival between the low post-LMR group (< 3.2) (n = 29) and the high post-LMR group (≥ 3.2) (n = 92) (MST[month]: 10.9 vs. 21.8, P = 0.073). NLR, neutrophil–lymphocyte ratio; LMR, lymphocyte-monocyte ratio; MST, median survival time
Characteristics of the high and low post-NLR and pre-LMR groups in CY1 gastric cancer patients
The high post-NLR group showed high age, high frequency of pathological T4, low frequency of NAC administration, and low frequency of postoperative chemotherapy administration compared with the low post-NLR group (Table 3). However, there was no difference in the postoperative infectious morbidity rate between the two groups. In contrast, the low pre-LMR group showed a higher age and lower frequency of postoperative infectious morbidity rate than the high pre-LMR group (Table 3).
Univariate and multivariate analyses of independent prognostic factors for OS
Univariate survival analysis for OS using the Cox proportional regression model for each covariate showed that high post-NLR and low pre-LMR predict poor survival (Table 4). Multivariate analysis showed that high post-NLR, low pre-LMR, and omission of postoperative chemotherapy were significant independent prognostic factors for poor survival (Table 4). Although postoperative chemotherapy was selected as an independent prognostic factor, patients undergoing postoperative chemotherapy did not show longer OS compared with patients without postoperative chemotherapy (MST, 19.3 months vs. 11.2 months, P = 0.222). Since post-NLR and pre-LMR were detected as independent prognostic factors for CY1 gastric cancer, the patients were divided into four groups according to post- NLR and pre-LMR. The MST in each group were 24.6 months in the low post-NLR/high pre-LMR group, 17.9 months in the low post-NLR/low pre-LMR group, 11.6 months in the high post-NLR/high pre-LMR group, and 8.3 months in the high post-NLR/low pre-LMR group, respectively. The low post-NLR/high pre-LMR group showed a significantly better OS rate than the low post-NLR/low pre-LMR group (P = 0.016), the high post-NLR/high pre-LMR group (0.024), and the high post-NLR/low pre-LMR group (P = 0.000) (Fig. 2).
Kaplan–Meier plots of overall survival among the four groups according to post-NLR and pre-LMR. The MST in each group was as follows: 24.6 months (95% CI, 16.8–35.0) in the low post-NLR/high pre-LMR group (n = 70), 17.9 months (95% CI, 5.3–26.2) in the low post-NLR/low pre-LMR group (n = 10), 11.6 months (95% CI, 8.2–21.8) in the high post-NLR/high pre-LMR group (n = 28), and 8.3 months (95% CI 4.8–12.9) in the high post-NLR/low pre-LMR group (n = 13), respectively. The low post-NLR/high pre-LMR group showed significantly longer survival than the low post-NLR/low pre-LMR group (P = 0.016), the high post-NLR/high pre-LMR group (P = 0.024), and the high post-NLR/low pre-LMR group (P = 0.000). MST, median survival time; CI, confidence interval; NLR: neutrophil–lymphocyte ratio; LMR: lymphocyte-monocyte ratio
RFS
The median RFS time was 9.0 months (95% CI 6.8–11.3). The majority of patients (61.4%) had postoperative recurrence within a year, 89.6% of which involved peritoneal dissemination. RFS tended to be longer in low post-NLR group compared with high post-NLR group (MST (month) 10.3 vs. 6.8, P = 0.200) and high pre-LMR group compared with low pre-LMR group (MST (month) 9.4 vs. 7.0, P = 0.116). The low post-NLR/high pre-LMR group tended to show better RFS than other group (MST 10.3 months vs. 7.0 months, P = 0.088). There were no statistically significant prognostic factors found that affected RFS.
Discussion
In this multi-institutional retrospective study, post-NLR value, pre-LMR value, and postoperative chemotherapy in gastric cancer patients with CY1 as a single non-curative factor were found to be associated with poor long-term prognosis.
NLR and LMR are readily available and inexpensive biomarkers in resectable gastric cancer patients; however, association of neutrophils, lymphocytes, and monocytes with CY1 gastric cancer is not fully understood [9, 18, 20].
Neutrophils accelerate tumor progression and metastasis via cytokine secretion (tumor necrosis factor, interleukin [IL]-1, IL-6) [20]. In contrast, lymphocytes play critical roles in host immune responses and suppress cancer progression [26]. The immunological evaluation of NLR system has been analyzed by tumor microenvironment (TME) with CD8-positive T cells and/or FoxP3-positive regulatory T cells in several types of cancer including gastric cancer [27,28,29,30]. IL-6 and IL-8 levels showed a significant correlation with NLR in blood and Foxp3 + cells around muscle-invasive bladder cancer [28]. Although CD3 + and CD8 + immune cell density were not associated with the NLR in resectable gastric cancer, high-NLR group showed decreased CD4 + immune cell density within TME compared with low-NLR group [30]. These results suggest that NLR in peripheral blood reflect the antitumor immune response in TME. Although there was no significant difference between pre-NLR and post-NLR, post-NLR showed a stronger influence on long-term survival in this study. Persisting high NLR status after gastrectomy may support cancer growth by regulating the microenvironment of residual cancer cells, despite the primary tumor being removed in this population [20]. In this study, the high post-NLR group underwent postoperative chemotherapy infrequently compared with the low post-NLR group. We easily suppose the correlation between persisting inflammation and poor performance status after surgery, and therefore, further examination is required to reveal the clinical impact of post-NLR, postoperative chemotherapy and postoperative performance status for survival time in CY1 gastric cancer patients.
In this study, pre-NLR was not calculated as an independent prognostic factor although OS tended to be worse in the high pre-NLR group. In the current study, postoperative treatments were heterogeneous, and the sample size was relatively small. Therefore, it is necessary to conduct a well-designed, validated study in many patients to examine that pre-NLR can be an independent prognostic factor.
LMR showed significant elevation after gastrectomy, which indicates that the number of monocytes reduced after R1 resection. However, post-LMR did not independently affect long-term prognosis. Meanwhile, pre-LMR showed a significant influence on survival and is, therefore, a valuable blood test parameter to predict the prognosis of CY1 gastric cancer before gastrectomy. Tumor-associated macrophages (TAMs) (more differentiated monocytes) promote angiogenesis and the breakdown of the extracellular matrix, which contribute to tumor cell invasion, migration, and progression [31, 32], and suppress host anticancer immune responses [33]. TAMs can comprise 50% of a tumor mass, forming a major component of infiltrated immune cell in the TME [34, 35]. TAMs can be classified as M1-like (pro-inflammatory and anti-tumor) and M2-like (anti-inflammatory and pro-tumor). High levels of TAMs in the TME are generally associated with high adverse prognosis and/or poor sensitivity to treatment in a variety of solid tumors [36], because TAMs acquire the properties of M2-like phagocytic population and phenotypes [35]. An increase in circulating monocytes may reflect a larger population of TAMs, and thus, monocyte count serves as an indicator of a high tumor burden [18]. Therefore, monocyte count may reflect the resistance of tumors towards host immunity more directly than neutrophil counts in the preoperative scenario in gastric cancer patients with CY1. In contrast, decreased monocytes after gastrectomy may have a small impact on the progression of residual cancer cells in the peritoneal cavity, which may explain why post-LMR did not affect the long-term prognosis.
A few studies have evaluated the predictive factors for survival in CY1 gastric cancer patients. Previous studies have shown that gross type of tumor, lymph node metastasis, nutritional status, and performance status are predictors for this population [37]. However, few studies have evaluated blood-based biomarkers [38, 39]. Although therapeutic strategy for CY1 gastric cancer is still controversial, radical gastrectomy showed better survival compared with palliative gastrectomy or palliative chemotherapy, and thus curative intent surgery with postoperative chemotherapy is recommended for this population [40, 41]. Moreover, a multi-institutional retrospective cohort study showed the efficacy of postoperative chemotherapy after macroscopically curative resection for CY1 gastric cancer regardless of chemotherapy regimen [42]. Systematic review and meta-analysis of gastric cancer with CY1 also showed that change to CY0 following NAC was associated with improved survival [43, 44]. In the current study, 19% of enrolled patients underwent NAC, and not every patient underwent staging laparoscopy for confirmation of CY1 before NAC. There was no difference in OS between patients receiving NAC and patients who did not receive NAC (MST 22.3 months vs. 16.5 months, P = 0.765). We can suppose the reason why NAC was less effective on OS as follows: the small number of patients receiving NAC; the exclusion of patients with conversion from CY1 to CY0 after NAC, in other words good response for NAC; and a possibility of macroscopic peritoneal dissemination in patients without diagnostic laparoscopy in the early phase of this study. Therefore, a prospective study is warrant to perform NAC for CY1 gastric cancer confirmed by lavage cytology to reveal the utility of peripheral blood-based predictive factors for negative conversion of peritoneal lavage cytology.
Although the low post-NLR/high pre-LMR group tended to show better RFS than the other group, we could not identify predictive factors for RFS in this study. Approximately 80% of CY1 patients experienced recurrence, and more than 60% of cases relapsed within a year in this study. This highly frequent and rapid recurrence may explain why pre-/post-NLR and LMR and other clinicopathological factors had no significant impact on RFS. Although inflammatory and nutritional status predicts OS for advanced gastric cancer [45, 46], prevention of cancer recurrence may depend on chemosensitivity to postoperative chemotherapy. Further studies are required to reveal the prognostic factors for RFS.
This study has some limitations. First, this was a retrospective cohort study; therefore, the therapeutic strategy for CY1 gastric cancer differed between each institution. Second, NAC and postoperative chemotherapy regimens were selected depending on the era. After the CCOG0301 study [6], S-1 monotherapy for a year is regarded as standard postoperative chemotherapy in this population. However, the actual administration of S-1 depended on patients’ performance status and intention. Third, the study period is so long, and standard chemotherapy was completely different depending on the period, so it is difficult to evaluate the correlation between peripheral blood score and therapeutic effect of chemotherapy. Fourth, the cutoff value of NLR and LMR was determined by the training set, and thus, the usefulness of the cutoff value should be evaluated in the validation set. The sample size of this study is insufficient; hence, accumulation of CY1 patients by prospective cohort study is required.
In conclusion, the results of this multi-institutional retrospective study support the importance of post-NLR and pre-LMR in CY1 gastric cancer patients. To the best of our knowledge, this is the first report showing blood-based predictors for survival in CY1 gastric cancer patients, which are available in daily clinical practice. These predictors may contribute to determining the strategies of perioperative chemotherapy for CY1 gastric cancer. It is also warranted to conduct a prospective trial in larger patient cohorts to confirm a useful perioperative chemotherapeutic regimen referring post-NLR and pre-LMR for CY1 gastric cancer.
References
Ferlay J EM, Lam F, Colombet M, Mery L, Pineros M, Znaor A, Soerjomataram I, Bray F (2018) Global cancer observatory: cancer today. Lyon, France: International Agency for Research on Cancer. https://gco.iarc.fr/today. Accessed 18 Dec 2018
Torre LA, Siegel RL, Ward EM, Jemal A (2016) Global cancer incidence and mortality rates and trends–an update. Cancer Epidemiol Biomarkers Prev 25:16–27
Bonenkamp JJ, Songun I, Hermans J, van de Velde CJ (1996) Prognostic value of positive cytology findings from abdominal washings in patients with gastric cancer. Br J Surg 83:672–674
Miyashiro I, Takachi K, Doki Y, Ishikawa O, Ohigashi H, Murata K, Sasaki Y, Imaoka S, Nakaizumi A, Takenaka A, Furukawa H, Hiratsuka M (2005) When is curative gastrectomy justified for gastric cancer with positive peritoneal lavage cytology but negative macroscopic peritoneal implant? World J Surg 29:1131–1134
Japanese classification of gastric carcinoma: 3rd English edition (2011). Gastric cancer: 14:101–112
Kodera Y, Ito S, Mochizuki Y, Kondo K, Koshikawa K, Suzuki N, Kojima H, Kojima T, Matsui T, Takase T, Tsuboi K, Fujiwara M, Nakao A (2009) A phase II study of radical surgery followed by postoperative chemotherapy with S-1 for gastric carcinoma with free cancer cells in the peritoneal cavity (CCOG0301 study). Eur J Surg Oncol 35:1158–1163
Kodera Y, Ito S, Mochizuki Y, Ohashi N, Tanaka C, Kobayashi D, Kojima H, Matsui T, Kondo K, Fujiwara M (2012) Long-term follow up of patients who were positive for peritoneal lavage cytology: final report from the CCOG0301 study. Gastric Cancer 15:335–337
Japanese gastric cancer treatment guidelines 2014 (ver. 4) (2017). Gastric Cancer 20:1-19
Shimada H, Takiguchi N, Kainuma O, Soda H, Ikeda A, Cho A, Miyazaki A, Gunji H, Yamamoto H, Nagata M (2010) High preoperative neutrophil-lymphocyte ratio predicts poor survival in patients with gastric cancer. Gastric Cancer 13:170–176
Li ZM, Huang JJ, Xia Y, Sun J, Huang Y, Wang Y, Zhu YJ, Li YJ, Zhao W, Wei WX, Lin TY, Huang HQ, Jiang WQ (2012) Blood lymphocyte-to-monocyte ratio identifies high-risk patients in diffuse large B-cell lymphoma treated with R-CHOP. PLoS One 7:e41658
Stotz M, Pichler M, Absenger G, Szkandera J, Arminger F, Schaberl-Moser R, Samonigg H, Stojakovic T, Gerger A (2014) The preoperative lymphocyte to monocyte ratio predicts clinical outcome in patients with stage III colon cancer. Br J Cancer 110:435–440
Takahashi R, Mabuchi S, Kawano M, Sasano T, Matsumoto Y, Kuroda H, Hisamatsu T, Kozasa K, Sawada K, Hamasaki T, Kimura T (2015) Prognostic significance of systemic neutrophil and leukocyte alterations in surgically treated endometrial cancer patients: a monoinstitutional study. Gynecol Oncol 137:112–118
Chen L, Hao Y, Zhu L, Li S, Zuo Y, Zhang Y, Song H, Xue Y (2017) Monocyte to lymphocyte ratio predicts survival in patients with advanced gastric cancer undergoing neoadjuvant chemotherapy. Onco Targets Ther 10:4007–4016
Walsh SR, Cook EJ, Goulder F, Justin TA, Keeling NJ (2005) Neutrophil-lymphocyte ratio as a prognostic factor in colorectal cancer. J Surg Oncol 91:181–184
Halazun KJ, Aldoori A, Malik HZ, Al-Mukhtar A, Prasad KR, Toogood GJ, Lodge JP (2008) Elevated preoperative neutrophil to lymphocyte ratio predicts survival following hepatic resection for colorectal liver metastases. Eur J Surg Oncol 34:55–60
Sarraf KM, Belcher E, Raevsky E, Nicholson AG, Goldstraw P, Lim E (2009) Neutrophil/lymphocyte ratio and its association with survival after complete resection in non-small cell lung cancer. J Thorac Cardiovasc Surg 137:425–428
Porrata LF, Ristow K, Habermann TM, Witzig TE, Colgan JP, Inwards DJ, Ansell SM, Micallef IN, Johnston PB, Nowakowski GS, Thompson C, Markovic SN (2012) Peripheral blood lymphocyte/monocyte ratio at diagnosis and survival in nodular lymphocyte-predominant Hodgkin lymphoma. Br J Haematol 157:321–330
Hsu JT, Wang CC, Le PH, Chen TH, Kuo CJ, Lin CJ, Chou WC, Yeh TS (2016) Lymphocyte-to-monocyte ratios predict gastric cancer surgical outcomes. J Surg Res 202:284–290
Zhou X, Du Y, Xu J, Huang Z, Qiu T, Wang X, Qian J, Zhu W, Liu P (2014) The preoperative lymphocyte to monocyte ratio predicts clinical outcomes in patients with stage II/III gastric cancer. Tumour Biol 35:11659–11666
Min KW, Kwon MJ, Kim DH, Son BK, Kim EK, Oh YH, Wi YC (2017) Persistent elevation of postoperative neutrophil-to-lymphocyte ratio: a better predictor of survival in gastric cancer than elevated preoperative neutrophil-to-lymphocyte ratio. Sci Rep 7:13967
Miyatani K, Saito H, Kono Y, Murakami Y, Kuroda H, Matsunaga T, Fukumoto Y, Osaki T, Ashida K, Fujiwara Y (2018) Combined analysis of the pre- and postoperative neutrophil-lymphocyte ratio predicts the outcomes of patients with gastric cancer. Surg Today 48:300–307
Tanaka H, Tamura T, Toyokawa T, Muguruma K, Miki Y, Kubo N, Sakurai K, Hirakawa K, Ohira M (2018) Clinical relevance of postoperative neutrophil-lymphocyte ratio (NLR) to recurrence after adjuvant chemotherapy of S-1 for gastric cancer. Anticancer Res 38:3745–3751
Kosaka T, Akiyama H, Miyamoto H, Sato S, Tanaka Y, Sato K, Kunisaki C, Endo I (2019) Outcomes of preoperative S-1 and docetaxel combination chemotherapy in patients with locally advanced gastric cancer. Cancer Chemother Pharmacol 83:1047–1055
Tanaka Y, Kunisaki C, Izumisawa Y, Makino H, Kimura J, Sato S, Miyamoto H, Kosaka T, Ono HA, Takahashi M, Sato K, Akiyama H, Endo I (2018) A phase I/II study of NAC with docetaxel, cisplatin, and S-1 for stage III gastric cancer. Anticancer Res 38:6015–6021
Cécile Contal JOQ (1999) An application of changepoint methods in studying the effect of age on survival in breast cancer. Comput Stat Data Anal 30:253–270
Feng F, Sun L, Zheng G, Liu S, Liu Z, Xu G, Guo M, Lian X, Fan D, Zhang H (2017) Low lymphocyte-to-white blood cell ratio and high monocyte-to-white blood cell ratio predict poor prognosis in gastric cancer. Oncotarget 8:5281–5291
Wu B, Zhao S, Sheng Y, Ren L, Song G (2018) The prognostic value of combining the CD8 + lymphocyte density and the circulating lymphocyte ratio in circumferential resection margin biopsy in rectal cancer. Medicine (Baltimore) 97:e11972
Morizawa Y, Miyake M, Shimada K, Hori S, Tatsumi Y, Nakai Y, Onishi S, Tanaka N, Konishi N, Fujimoto K (2018) Correlation of immune cells and cytokines in the tumor microenvironment with elevated neutrophil-to-lymphocyte ratio in blood: an analysis of muscle-invasive bladder cancer. Cancer Invest 36:395–405
Lee KH, Kim EY, Yun JS, Park YL, Do SI, Chae SW, Park CH (2018) The prognostic and predictive value of tumor-infiltrating lymphocytes and hematologic parameters in patients with breast cancer. BMC Cancer 18:938
Choi Y, Kim JW, Nam KH, Han SH, Kim JW, Ahn SH, Park DJ, Lee KW, Lee HS, Kim HH (2017) Systemic inflammation is associated with the density of immune cells in the tumor microenvironment of gastric cancer. Gastric Cancer 20:602–611
Condeelis J, Pollard JW (2006) Macrophages: obligate partners for tumor cell migration, invasion, and metastasis. Cell 124:263–266
Gabrilovich DI, Nagaraj S (2009) Myeloid-derived suppressor cells as regulators of the immune system. Nat Rev Immunol 9:162–174
Donskov F, von der Maase H (2006) Impact of immune parameters on long-term survival in metastatic renal cell carcinoma. J Clin Oncol 24:1997–2005
Vitale I, Manic G, Coussens LM, Kroemer G, Galluzzi L (2019) Macrophages and metabolism in the tumor microenvironment. Cell Metab 30:36–50
Kim J, Bae JS (2016) Tumor-associated macrophages and neutrophils in tumor microenvironment. Mediators Inflamm 2016:6058147
Cassetta L, Pollard JW (2018) Targeting macrophages: therapeutic approaches in cancer. Nat Rev Drug Discov 17:887–904
Endo S, Ikenaga M, Ohta K, Ueda M, Tsuda Y, Kato R, Itakura H, Matsuyama J, Nishikawa K, Yamada T (2019) Prognostic factors for cytology-positive gastric cancer. Surg Today 49:56–64
Mezhir JJ, Shah MA, Jacks LM, Brennan MF, Coit DG, Strong VE (2010) Positive peritoneal cytology in patients with gastric cancer: natural history and outcome of 291 patients. Ann Surg Oncol 17:3173–3180
Oh CA, Bae JM, Oh SJ, Choi MG, Noh JH, Sohn TS, Kim S (2012) Long-term results and prognostic factors of gastric cancer patients with only positive peritoneal lavage cytology. J Surg Oncol 105:393–399
Fukuchi M, Mochiki E, Ishiguro T, Ogura T, Sobajima J, Kumagai Y, Ishibashi K, Ishida H (2016) Prognostic factors for gastric cancer with cancer cells in the peritoneal cavity. Anticancer Res 36:2481–2485
Komatsu S, Shioaki Y, Furuke H, Ohta A, Tsuji R, Tanaka S, Kumano T, Imura KI, Shimomura K, Ikeda J, Taniguchi F, Ueshima Y, Lee CJ, Deguchi E, Ikeda E, Otsuji E (2019) Is curative gastrectomy justified for gastric cancer with cytology positive as the only stage IV factor? Langenbecks Arch Surg 404:599–604
Yamaguchi T, Takashima A, Nagashima K, Makuuchi R, Aizawa M, Ohashi M, Tashiro K, Yamada T, Kinoshita T, Hata H, Kawachi Y, Kawabata R, Tsuji T, Hihara J, Sakamoto T, Fukagawa T, Katai H, Higuchi K, Boku N (2020) Efficacy of postoperative chemotherapy after resection that leaves no macroscopically visible disease of gastric cancer with positive peritoneal lavage cytology (CY1) or localized peritoneum metastasis (P1a): a multicenter retrospective study. Ann Surg Oncol 27:284–292
Jamel S, Markar SR, Malietzis G, Acharya A, Athanasiou T, Hanna GB (2018) Prognostic significance of peritoneal lavage cytology in staging gastric cancer: systematic review and meta-analysis. Gastric Cancer 21:10–18
Yasufuku I, Nunobe S, Ida S, Kumagai K, Ohashi M, Hiki N, Sano T (2020) Conversion therapy for peritoneal lavage cytology-positive type 4 and large type 3 gastric cancer patients selected as candidates for R0 resection by diagnostic staging laparoscopy. Gastric Cancer 23:319–327
Zhang CX, Wang SY, Chen SQ, Yang SL, Wan L, Xiong B (2016) Association between pretreatment Glasgow prognostic score and gastric cancer survival and clinicopathological features: a meta-analysis. Onco Targets Ther 9:3883–3891
Li QQ, Lu ZH, Yang L, Lu M, Zhang XT, Li J, Zhou J, Wang XC, Gong JF, Gao J, Li J, Li Y, Shen L (2014) Neutrophil count and the inflammation-based Glasgow prognostic score predict survival in patients with advanced gastric cancer receiving first-line chemotherapy. Asian Pac J Cancer Prev 15:945–950
Author information
Authors and Affiliations
Contributions
SS, CK, and MT participated in study conception and design. SS, MT, HK, TN, KS, YT, HM, YT, HK, YN, KK, TK, and HA participated in acquisition of data. SS and YS participated in analysis and interpretation of data. SS, CK, and IE participated in drafting of manuscript and critical revision of manuscript.
Corresponding author
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sato, S., Kunisaki, C., Takahashi, M. et al. High postoperative neutrophil–lymphocyte ratio and low preoperative lymphocyte-monocyte ratio predict poor prognosis in gastric cancer patients receiving gastrectomy with positive lavage cytology: a retrospective cohort study. Langenbecks Arch Surg 406, 2295–2303 (2021). https://doi.org/10.1007/s00423-021-02233-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-021-02233-6