Abstract
Purpose
Internal biliary stenting (IBS) was reported to decrease biliary complications after liver transplantation (LT) but data in literature is scarce. The aim of the present study was to evaluate our experience with end-to-end choledoco-choledocostomy during liver transplantation with special focus on the influence of IBS on patient and biliary outcomes.
Methods
Between 2009 and 2013, 175 patients underwent deceased donor LT with end-to-end choledoco-choledocostomy and were included in the study. Supra-papillary silastic stent was inserted in 67 patients (38%) with small-size (< 5 mm) bile ducts (recipient or donor). Endoscopic retrograde cholangiopancreatography (ERCP) was scheduled for IBS removal, 6 months after LT. Operative outcomes and survival of patients who received internal stenting (IBS group) were compared with those of patients who did not (no-IBS group). Risk factors for biliary anastomotic complications were identified.
Results
Ten patients died (6%) and 104 (59%) experienced postoperative complications. Five-year patient and graft survival rates were 77 and 74%, respectively. Biliary complications were recorded in 61 patients (35%) and were significantly decreased by IBS insertion (p = 0.0003). Anastomotic fistulas occurred in 23 patients (13%) and stenoses in 44 patients (25%). On multivariate analysis, high preoperative MELD scores (p = 0.02) and hepatic artery thrombosis (p < 0.0001) were predictors of fistula; absence of IBS was associated with both fistula (p = 0.014) and stricture (p = 0.003) formation.
Conclusions
IBS insertion during LT decreases anastomotic complication.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Biliary reconstruction during liver transplantation (LT) is usually performed by a duct to duct anastomosis and may be viewed improperly as the easy step of a difficult operation [1]. Complications arising from the biliary anastomosis (leakage, stricture) are usually considered as the technical Achilles heel of LT; such complications are a significant source of postoperative morbidity and mortality, induce a severe financial burden, and may eventually compromise outcomes [2,3,4]. Despite significant advances in surgical technique and recipient and donor selection, the incidence of anastomotic biliary complications remains high, ranging from 10 to 50% in the literature [5].
Stenting of the biliary anastomosis has been proposed to preclude biliary complications after LT with contradictory results [1, 6,7,8,9]. Intraoperative T-tube placement has been advocated to lower pressure in the biliary system, provide easy postoperative radiological access to the biliary tree, and decrease anastomotic complications [3, 10,11,12]. Although the debate is still open, a growing number of centers have abandoned T-tube placement along with accumulating evidence pointing out at specific T-tube-induced morbidity and showing safe, efficient, and cost-effective outcomes without T-tube placement [13,14,15,16,17,18]. The use of internal biliary stenting (IBS) has been reported as a safe alternative to T-tube placement in LT [1, 6, 7]. The main advantage of IBS is the absence of choledochotomy which is a major source of biliary leakage after T-tube placement [10, 19]. Although IBS is an interesting option, several technical issues such as the nature of the material (silastic, rubber), optimal stent positioning in the biliary system (supra-papillary vs. trans-papillary), and delays in stent removal require further refinement.
Since January 2009, an IBS insertion program was started in our center in patients who underwent duct to duct biliary anastomosis during LT. The aim of the present study was to evaluate our experience with end-to-end choledoco-choledocostomy during liver transplantation with special focus on the influence of IBS on patient and biliary outcomes.
Material and methods
Study population
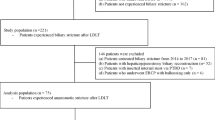
From January 2009 to December 2013, 200 patients underwent deceased donor LT in the department of Hepatobiliary Surgery of the Centre Hospitalier Universitaire Grenoble Alpes, France. Of them, 175 patients (88%), aged ≥ 18 years, received a whole graft LT with duct-to duct biliary reconstruction and were the subject of the present study.
Technical considerations
Grafts were recovered with the standard classic technique described by Starlz et al. [20], and IGL-1 solution (Waters Medical Systems) was used for organ preservation. A total hepatectomy with caval preservation was performed in all patients. The graft was flushed with 500 mL of 37 °C Albumin solution immediately before portal reperfusion. After the assessment of donor and recipient bile duct diameters, biliary reconstruction was performed using a standardized technique; duct-to-duct biliary reconstruction was performed through an end-to-end choledoco-choledocostomy in all patients. The connective tissue around the donor and recipient bile ducts was thoroughly preserved to avoid periductal devascularization. The posterior face of the biliary anastomosis was made with a 6/0 polydiaxanone running suture, and the anterior face with 6/0 polydiaxanone interrupted sutures. As a general rule, internal biliary stents (IBS) were positioned if at least one bile duct (graft or recipient) was measured < 5 mm; the decision of stent insertion remained at the discretion of the operative surgeon. The home-made stent was constructed from a silastic tube (8 to 12 French) and was inserted after construction of the posterior anastomotic suture. The stent diameter was chosen as to mold the bile duct walls and the length was tailored to bridge the whole common bile duct from the papilla to the hilar bifurcation. Care was taken to avoid transpapillary stent passage in order to prevent untimely stent migration. Two small (2 mm) lateral holes were performed at each end and the stent was positioned freely into the bile duct with no suture fixation.
All patients underwent daily liver function tests during the first week after surgery. Doppler ultrasonography was performed immediately after LT, daily during the first 3 postoperative days (POD) and repeated on postoperative days 7 to 10. In the absence of bile leakage, the abdominal drain was progressively mobilized starting POD 7 and was removed on POD 10. Adverse events occurring during the postoperative course that were thought to be stent related prompted immediate stent removal. In the absence of spontaneous migration, an ERCP procedure for stent removal was scheduled 6 months after LT; during the procedure, the stent was removed with an endoscopic staple extractor. Sphincterotomy was systematically performed for stent removal in all patients.
Outpatient follow-up monitoring of liver function tests and Doppler ultrasound was conducted monthly during the first 6 months, at 9 months, 1 year, and annually thereafter.
Definition and management of biliary complications
Biliary fistulas were defined according to the ISGLS classification [21] as bilirubin concentration in the drain fluid at least 3 times the serum bilirubin concentration on or after postoperative day 3, or as the need for radiologic or operative intervention resulting from biliary collections or bile peritonitis. Grade A biliary fistulas caused no change in patient’s clinical management; in these situations, prolongation of external drainage was enough to assure cessation of the bile leakage. Grade B fistulas required active therapeutic interventions without laparotomy; radiological drainage and endoscopic retrograde cholangiopancreatography (ERCP) manoeuvers were performed to obtain leakage control and speed up fistula closure. Grade C leakages required reoperation: at the beginning of the study period, an open approach was the rule but the use of an initial laparoscopy approach increased recently. During reoperation for biliary leakage, efforts were made to preserve the biliary anastomosis: lavage and drainage, T tube drainage, anastomosis reconstruction, etc. Dismantling of the anastomosis with intubation and external drainage of the graft bile duct were performed as a last resort in difficult situations.
Biliary stenosis was defined as narrowing of the biliary anastomosis detected on specific imaging exams (MRI cholangiography, ERCP). If other causes (rejection, viral reactivation, etc.) could be overruled, persistent clinical and/or biological cholestasis (increase > 2N of gamma-glutamyl transferase and alkaline phosphatase levels) was considered as anastomotic stenosis and managed accordingly. ERCP dilation and stenting were the first-line treatment of anastomotic biliary strictures. Surgery including re-laparotomy and construction of a biliary enteric anastomosis was considered secondarily in case of failure.
Anastomotic biliary complications were defined as biliary fistula and stricture formation involving the site of biliary anastomosis.
Postoperative medication
The induction of immunosuppression protocol was standardized and included the combination of corticosteroids started just before declamping and continued up to the 30th POD, gradually decreasing doses of calcineurin inhibitors (tacrolimus) started 8–12 h post-transplantation then adapted to plasma levels, and mycophenolate mofetil that was added on POD 3 for at least 6 months.
Antibiotic prophylaxis using piperacillin + tazobactam was administered to all patients on a systematic basis; antibiotics were started during LT and were pursued 48 h. In patients who developed infectious complications, administration was extended for at least 10 days relying on perioperative bile culture results and/or bacterial identification and antibiotic susceptibility testing.
Ursodeoxycholic acid was not used for the prevention of biliary complications.
Statistical analysis
Operative mortality and morbidity were defined as death or complications occurring within 90 days after LT. Postoperative complications were classified according to the Clavien-Dindo’s classification [22]. Results are expressed as median and first and third quartiles or counts and percent. Survival curves were made using Kaplan-Meier’s method and compared with the log-rank test. Survival was defined as the time between LT and death. Patients lost to follow-up for more than 1 year were contacted up to January 2016; when patients could not be reached directly, family members or general practitioners were contacted. Living patients were censored at the date of the last available information (visit or phone call). Marginal association between single variables and functional outcome was assessed by a Wilcoxon rank-sum test for quantitative variables and Fisher exact test for categorical variables. Univariate and multivariate analyses were performed to identify independent predictors of anastomotic biliary complications. All variables achieving statistical significance at a 0.1 level in the univariate analysis were considered in a multiple logistic model. A backward variable selection procedure with P value cut-off at 0.05 was used to identify the set of independent predictors of each considered variable.
Results
Patients
Among 175 patients included in the study, 144 (82%) were men and median age was 57 years [51; 61]. Sixty seven patients (38%) received an IBS while biliary reconstruction without stenting was performed in 108 patients. There was a significantly lower incidence of hepatocellular carcinoma in the IBS group (n = 18; 27% vs. n = 47; 44%, p = 0.036), Table 1.
Intraoperative management
The median operative and cold ischemia times were 400 [335; 450] min and 397 [324; 480] min, respectively; there was no significant difference between the IBS and no-IBS groups (Table 2). The median IBS size was 10 French (range 8F–12F). The median diameter of the recipient bile duct was 5[4; 7] mm in the IBS group and 6[5; 8] mm in patients who did not receive stenting (p = 0.0008). Similarly, the median diameter of the donor bile duct was smaller in the IBS group (6[4; 7.25] vs. 6[5; 8] mm, p = 0.045) Table 2. Overlap between bile duct size may induce bias in result interpretation and can be explained by IBS insertion if only one bile duct (donor, recipient) was < 5 mm and by non-respect of this rule by the attending surgeon in 9 patients (5%).
Postoperative course
Ten patients died (6%) in the postoperative period. Death occurred 15 days (range 1–86 days) after LT as a result of arterial rupture (n = 3), severe sepsis (n = 5), mesenteric ischemia (n = 1), and stroke (n = 1). Operative complications were recorded in 104 patients (59%) and were severe (Dindo-Clavien ≥ 3) in 83 patients (47%). There were no significant differences in operative mortality and overall and severe morbidity between patients with and without IBS Table 2.
Biliary complications
Overall biliary complications occurred in 65 patients (37%). Biliary anastomotic complications occurred in 61 patients (35%). Non-anastomotic biliary complications occurred in 10 patients (4 IBS, 6 no-IBS) and included bile cast syndrome in 3 patients and ischemic cholangitis in 7 patients; the small number did not allow statistical analysis.
The rate of anastomotic biliary complications was significantly lower in patients who underwent internal biliary stenting (n = 12; 18% vs. n = 49; 45%, p = 0.0003) Table 2. Back table hepatic artery reconstruction was performed in 28 (16%) patients (11 patients IBS, 17 patients no-IBS) because of the presence of replaced right (n = 28) and/or left (n = 20) donor arteries. Back table artery reconstruction did not influence the rate of anastomotic biliary complications (p = 0.24), of biliary fistula (p = 0.22), and of anastomotic stenosis (p = 0.49).
Anastomotic biliary fistulas occurred in 23 patients (13%). According to the ISGLS classification, there were 1 grade A, 6 grade B, and 16 grade C bile leaks. Median delay in diagnosis of biliary fistulas was 20 days [12; 35]. On univariate analysis, factors predictive of biliary fistula included older age (p = 0.01), the absence of IBS (p = 0.037), hepatic artery thrombosis (p = 0.007), increased preoperative MELD scores (p = 0.028), and donor bile duct size (p = 0.038) Table 3. There was a trend for increased recipient bile duct size which did not reach statistical significance (p = 0.07). In the multivariate model including all these factors, the absence of IBS (p = 0.014), hepatic artery thrombosis (p = 0.0001), and high preoperative MELD scores (p = 0.02) were associated with biliary fistula. Management of bile leaks required reoperation in 12 patients. Reoperation included peritoneal lavage and drainage (n = 7), T-tube biliary drainage (n = 2), external bile-duct intubation (n = 3), redo choledoco-choledocal reconstruction (n = 1), and biliary digestive reconstruction (n = 1). Overall, management of biliary fistulas required 31 ERCP procedures and insertion of 12 biliary stents.
Anastomotic biliary strictures occurred in 44 patients (25%) after a median delay of 3.5 [1.85; 5.7] months. On univariate analysis, the only predictive factor of biliary stricture was the absence of IBS (p = 0.002), Table 4. There was a trend for hepatic artery stenosis (p = 0.08) and perioperative transfusion (0.076) but figures did not reach statistical significance. In the multivariate model including all these factors, only the absence of IBS (p = 0.003) was associated with biliary stricture. Overall, stricture management required 127 ERCP procedures and insertion of 94 biliary stents.
Failure to treat anastomotic biliary complications was directly related to death in 4 patients (2%) and led to graft loss in 7 patients (4%).
IBS management and IBS-related complications
Spontaneous IBS migration occurred in 10 patients (15%). In 4 of them, the IBS migrated into the duodenum with no significant consequences. Intrahepatic IBS migration required stent retrieval in 6 patients. Specific IBS-related complications occurred in 2 (3%) patients (hemobilia n = 1, obstructive cholangitis n = 1) and required emergency IBS ablation. Eventually, ERCP IBS removal was undertaken in 60 (90%) of the 67 patients after a median delay of 6 [5; 7] months.
A total of 103 patients (58%) underwent at least 1 ERCP procedure after LT including 61 patients (91%) in the IBS group and 42 patients (39%) in the no-IBS group (p < 0.0001). However, the median number of post-LT ERCP procedures/patient was significantly lower in the IBS group when compared to the no-IBS group (median 1 [1; 3] vs. 3.5 [2; 5]; p < 0.0001).
Survival
Median patient follow-up was 30 months [17; 47]. Kaplan-Meier patient survival rates at 1, 3, and 5 years were 88, 82, and 77%, respectively (Fig. 1). Patient survival was similar in patients with and without IBS (p = 0.74) (Fig. 2).
Graft survival rates at 1, 3, and 5 years were 86, 80, and 74%, respectively (Fig. 1). Seven patients (4%) underwent re-transplantation for VHC recurrence (n = 3), arterial thrombosis and ischemic cholangitis (n = 3), and chronic rejection (n = 1). IBS had no significant influence on graft survival (p = 0.91) (Fig. 3).
Discussion
The present study compared outcomes of patients who underwent end-to-end bile duct anastomosis during LT, with (n = 67) or without (n = 108) IBS placement over a 7-year period. IBS were inserted preferentially in patients with small-size (donor and/or recipient) bile ducts (< 5 mm) who are at higher risk of developing biliary complications, at the discretion of the operating surgeon; this selection criterion is mirrored by the significant smaller size of both donor and recipient bile ducts in the IBS group. The main study finding was a significant decrease in anastomotic biliary complication rates in patients who received IBS. Actually, multivariate analysis revealed that the absence of IBS was an independent predictor of both anastomotic biliary fistula (p = 0.014) and anastomotic stricture formation (p = 0.003). On the other hand, IBS had no significant influence on operative morbidity and mortality rates, long-term survival, and graft loss. This can be explained by the fact that biliary complications although time- and resource-consuming cause seldom patient death or graft loss; in accordance with other publications [4, 9], failure to treat biliary complications was directly related to death in 2% and graft loss in 4% of patients in the present study.
Decreasing the incidence and severity of biliary complications is a major goal in liver transplantation. Studies focusing on the topic have identified several risk factors of biliary complications which can be related to the recipient (age [23], high MELD score [2]), to the graft (donor gender [24] and age [2], living vs. deceased [4], degree of steatosis [25]), to operative factors (warm [2] and cold [26] ischemia times, bile duct size [27], transfusion requirements [28], re-transplantation [29]), and to postoperative factors (rejection [29], hepatic artery thrombosis [30], CMV status [31] and the type of immunosuppression [32]). Of them, biliary stent placement targets mainly patients in whom the biliary anastomosis is rendered technically difficult by the small caliber of bile ducts [5]. Studies evaluating the influence of IBS on biliary outcomes after LT are scarce in the literature and the results controversial [1, 2, 6,7,8,9]. In accordance with the present finings, Barkun [7] reported a significant decrease of biliary complication by inserting an IBS in a group of 21 patients (4.8% biliary complications) when compared to 30 recent controls (30% biliary complications) and to a historical 224 patients control group (32.6% biliary complications). Similarly, Johnson et al. [6] compared 77 IBS patients with 18 T-tube controls and reported lower biliary complications rates (18 vs. 38%, p = 0.05) and shorter in-hospital stay (18.3 ± 1.9 vs. 30.1 ± 6. days, p = 0.017) in the IBS group. In a recent study, Tranchart et al. [1] reported 100% feasibility and good results of IBS insertion in 20 patients with small-size (< 5 mm) graft bile ducts. The promising results of this study motivated us to choose a 5-mm bile duct diameter as cut-off for IBS insertion. In contrast, the largest series to date comparing 221 IBS patients to 292 no-IBS patients failed to prove that IBS protects against anastomotic biliary complications although there was a statistical trend (p = 0.06) [9]. However, the inclusion in this study [9] of patients with Roux-en-Y hepaticojejunostomy and of patients who received split grafts as well as the absence of a multivariate analysis may be confounding when analyzing the results.
Concerns raised by IBS placement during LT include specific drain-related complications and the necessity to perform systematic ERCP for drain removal [1]. In the literature, spontaneous IBS migration was reported in 5–43% of patients and usually had no significant consequences [1, 6]. Severe IBS-related complications were seldom described which is in contrast to the high drain-related morbidity rates recorded after T-tube placement [4]. In the present study, IBS migration occurred in 15% of patients while specific IBS complications (bleeding, cholangitis) occurred in 3% of patients and were successfully managed by ERCP drain removal. One major shortcoming of IBS placement is the need to perform ERCP for stent removal [1, 9]; this was confirmed in the present study as the number of patients who underwent at least one post-LT ERCP procedure was significantly higher in the IBS group. However, the number of post-LT ERCP procedures/patient was significantly lower after IBS insertion. This is an important finding as reducing the need for (potentially complex) ERCP to treat anastomotic biliary complications may balance the inconvenience of systematic (usually simple) ERCP for drain removal. Recent development of resorbable IBS may be a promising lead to alleviate such drawbacks in the future [33].
The present study has several limitations. First, the study is a retrospective analysis which reflects a single-center experience and the clinical biases therein. Nevertheless, the results provide basic data for the planning and designing of a multicenter randomized controlled trial (RCT) for the analysis of the usefulness of IBS in liver transplantation. Actually, such a RCT is currently ongoing in France [5]. Second, biliary complication rates in the present study were quite high; the use of extended criteria to define biliary complications resulted in the inclusion of subclinical manifestations of fistula and strictures which are usually underreported in the literature.
Conclusion
The placement of internal biliary removable stents in end-to-end ductal anastomosis during liver transplantation is a simple and safe way to decrease biliary anastomotic complications. Specific IBS-related adverse events are seldom recorded and when complications occur they are usually mild. IBS insertion may decrease the number of complex endoscopic procedures/patient after LT. Internal stenting of end-to-end choledococholedocostomy should be considered systematically during liver transplantation.
References
Tranchart H, Zalinski S, Sepulveda A, Chirica M, Prat F, Soubrane O, Scatton O (2012) Removable intraductal stenting in duct-to-duct biliary reconstruction in liver transplantation. Transpl Int 25:19–24. https://doi.org/10.1111/j.1432-2277.2011.01339.x
Welling TH, Heidt DG, Englesbe MJ, Magee JC, Sung RS, Campbell DA, Punch JD, Pelletier SJ (2008) Biliary complications following liver transplantation in the model for end-stage liver disease era: effect of donor, recipient, and technical factors. Liver Transpl 14:73–80. https://doi.org/10.1002/lt.21354
Seehofer D, Eurich D, Veltzke-Schlieker W, Neuhaus P (2013) Biliary complications after liver transplantation: old problems and new challenges. Am J Transplant 13:253–265. https://doi.org/10.1111/ajt.12034
Akamatsu N, Sugawara Y, Hashimoto D (2011) Biliary reconstruction, its complications and management of biliary complications after adult liver transplantation: a systematic review of the incidence, risk factors and outcome. Transpl Int 24:379–392. https://doi.org/10.1111/j.1432-2277.2010.01202.x
Goumard C, Cachanado M, Herrero A, Rousseau G, Dondero F, Compagnon P, Boleslawski E, Mabrut JY, Salamé E, Soubrane O, Simon T, Scatton O (2015) Biliary reconstruction with or without an intraductal removable stent in liver transplantation: study protocol for a randomized controlled trial. Trials 16:598. https://doi.org/10.1186/s13063-015-1139-6
Johnson MW, Thompson P, Meehan A, Odell P, Salm MJ, Gerber DA, Zacks SL, Fried MW, Shrestha R, Fair JH (2000) Internal biliary stenting in orthotopic liver transplantation. Liver Transpl 6:356–361. https://doi.org/10.1053/lv.2000.5303
Barkun JS, Tzimas GN, Cantarovich M, Metrakos PP, Deschênes M, Alpert E, Paraskevas S, Tchervenkov JI (2003) Do biliary endoprostheses decrease biliary complications after liver transplantation? Transplant Proc 35:2435–2437
Bawa SM, Mathew A, Krishnan H, Minford E, Talbot D, Mirza DF, Thick MG, Gibbs P, Manas D (1998) Biliary reconstruction with or without an internal biliary stent in orthotopic liver transplantation: a prospective randomised trial. Transpl Int 11(Suppl 1):S245–S247
Mathur AK, Nadig SN, Kingman S, Lee D, Kinkade K, Sonnenday CJ, Welling TH (2015) Internal biliary stenting during orthotopic liver transplantation: anastomotic complications, post-transplant biliary interventions, and survival. Clin Transpl 29:327–335. https://doi.org/10.1111/ctr.12518
Grande L, Pérez-Castilla A, Matus D, Rodriguez-Montalvo C, Rimola A, Navasa M, García-Valdecasas JC, Visa J (1999) Routine use of the T tube in the biliary reconstruction of liver transplantation: is it worthwhile? Transplant Proc 31:2396–2397
Weiss S, Schmidt S-C, Ulrich F, Pascher A, Schumacher G, Stockmann M, Puhl G, Guckelberger O, Neumann UP, Pratschke J, Neuhaus P (2009) Biliary reconstruction using a side-to-side choledochocholedochostomy with or without T-tube in deceased donor liver transplantation. Ann Surg 250:766–771. https://doi.org/10.1097/SLA.0b013e3181bd920a
Wojcicki M, Milkiewicz P, Silva M (2008) Biliary tract complications after liver transplantation: a review. Dig Surg 25:245–257. https://doi.org/10.1159/000144653
Riediger C, Müller MW, Michalski CW, Hüser N, Schuster T, Kleeff J, Friess H (2010) T-tube or no T-tube in reconstruction of the biliary tract during orthotopic liver transplantation—systematic review and meta-analysis. Liver Transpl NA–NA:NA. https://doi.org/10.1002/lt.22070
Shimoda M, Saab S, Morrisey M et al (2001) A cost-effectiveness analysis of biliary anastomosis with or without T-tube after orthotopic liver transplantation. Am J Transplant 1:157–161
Scatton O, Meunier B, Cherqui D, Boillot O, Sauvanet A, Boudjema K, Launois B, Fagniez PL, Belghiti J, Wolff P, Houssin D, Soubrane O (2001) Randomized trial of choledochocholedochostomy with or without a T tube in orthotopic liver transplantation. Ann Surg 233:432–437
Sotiropoulos GC, Sgourakis G, Radtke A, Molmenti EP, Goumas K, Mylona S, Fouzas I, Karaliotas C, Lang H (2009) Orthotopic liver transplantation: T-tube or not T-tube? Systematic review and meta-analysis of results. Transplantation 87:1672–1680. https://doi.org/10.1097/TP.0b013e3181a5cf3f
Paes-Barbosa FC, Massarollo PC, Bernardo WM, Ferreira FG, Barbosa FK, Raslan M, Szutan LA (2010) Systematic review and meta-analysis of biliary reconstruction techniques in orthotopic deceased donor liver transplantation. J Hepato-Biliary-Pancreat Sci 18:525–536. https://doi.org/10.1007/s00534-010-0346-5
Amador A, Charco R, Martí J, Navasa M, Rimola A, Calatayud D, Rodriguez-Laiz G, Ferrer J, Romero J, Ginesta C, Fondevila C, Fuster J, García-Valdecasas JC (2007) Clinical trial on the cost-effectiveness of T-tube use in an established deceased donor liver transplantation program. Clin Transpl 21:548–553. https://doi.org/10.1111/j.1399-0012.2007.00688.x
Saab S (2000) Endoscopic management of biliary leaks after t-tube removal in liver transplant recipients: nasobiliary drainage versus biliary stenting. Liver Transpl 6:627–632. https://doi.org/10.1053/jlts.2000.8200
Starzl TE, Miller C, Broznick B, Makowka L (1987) An improved technique for multiple organ harvesting. Surg Gynecol Obstet 165:343–348
Koch M, Garden OJ, Padbury R et al (2011) Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the International Study Group of Liver Surgery. Surgery 149:680–688. https://doi.org/10.1016/j.surg.2010.12.002
Dindo D, Demartines N, Clavien P-A (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Sawyer RG, Punch JD (1998) Incidence and management of biliary complications after 291 liver transplants following the introduction of transcystic stenting. Transplantation 66:1201–1207
Verdonk RC, Buis CI, Porte RJ, van der Jagt EJ, Limburg AJ, van den Berg AP, Slooff MJH, Peeters PMJG, de Jong KP, Kleibeuker JH, Haagsma EB (2006) Anastomotic biliary strictures after liver transplantation: causes and consequences. Liver Transpl 12:726–735. https://doi.org/10.1002/lt.20714
Baccarani U, Isola M, Adani GL, Avellini C, Lorenzin D, Rossetto A, Currò G, Comuzzi C, Toniutto P, Risaliti A, Soldano F, Bresadola V, de Anna D, Bresadola F (2010) Steatosis of the hepatic graft as a risk factor for post-transplant biliary complications. Clin Transpl 24:631–635
Park JB, Kwon CHD, Choi G-S, Chun JM, Jung GO, Kim SJ, Joh JW, Lee SK (2008) Prolonged cold ischemic time is a risk factor for biliary strictures in duct-to-duct biliary reconstruction in living donor liver transplantation. Transplantation 86:1536–1542. https://doi.org/10.1097/TP.0b013e31818b2316
Marubashi S, Dono K, Nagano H, Kobayashi S, Takeda Y, Umeshita K, Monden M, Doki Y, Mori M (2009) Biliary reconstruction in living donor liver transplantation: technical invention and risk factor analysis for anastomotic stricture. Transplantation 88:1123–1130. https://doi.org/10.1097/TP.0b013e3181ba184a
Qian YB, Liu CL, Lo CM (1960) Fan ST (2004) risk factors for biliary complications after liver transplantation. Arch Surg Chic Ill 139:1101–1105. https://doi.org/10.1001/archsurg.139.10.1101
Verran DJ, Asfar SK, Ghent CN, Grant DR, Wall WJ (1997) Biliary reconstruction without T tubes or stents in liver transplantation: report of 502 consecutive cases. Liver Transpl Surg 3:365–373
Seo JK, Ryu JK, Lee SH, Park JK, Yang KY, Kim YT, Yoon YB, Lee HW, Yi NJ, Suh KS (2009) Endoscopic treatment for biliary stricture after adult living donor liver transplantation. Liver Transpl 15:369–380. https://doi.org/10.1002/lt.21700
Kasahara M, Egawa H, Takada Y, Oike F, Sakamoto S, Kiuchi T, Yazumi S, Shibata T, Tanaka K (2006) Biliary reconstruction in right lobe living-donor liver transplantation: comparison of different techniques in 321 recipients. Ann Surg 243:559–566. https://doi.org/10.1097/01.sla.0000206419.65678.2e
Tashiro H, Itamoto T, Sasaki T, Ohdan H, Fudaba Y, Amano H, Fukuda S, Nakahara H, Ishiyama K, Ohshita A, Kohashi T, Mitsuta H, Chayama K, Asahara T (2007) Biliary complications after duct-to-duct biliary reconstruction in living-donor liver transplantation: causes and treatment. World J Surg 31:2222–2229
Sánchez-Cabús S, Calatayud D, Ferrer J, Molina V, Pavel MC, Sampson J, Saavedra D, Fondevila C, Fuster J, García-Valdecasas JC (2016) Beneficial effect of a resorbable biliary stent in living donor liver transplantation. Eur Surg Res 56:123–131. https://doi.org/10.1159/000443271
Author information
Authors and Affiliations
Contributions
Seven authors make substantial contributions to the development of this manuscript. Girard, O. Risse, V. Leroy, and C. Letoublon design the study; E. Girard, O. Risse, and J. Abba performed acquisition of data; M. Medici and M. Chirica made data analysis. E. Girard and M. Chirica wrote the paper; O. Risse, J. Abba, M. Medici, V. Leroy, and C. Letoublon reviewed the paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Girard, E., Risse, O., Abba, J. et al. Internal biliary stenting in liver transplantation. Langenbecks Arch Surg 403, 487–494 (2018). https://doi.org/10.1007/s00423-018-1669-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-018-1669-y