Abstract
Both voluntary rebreathing (RB) of expired air and voluntary apneas (VA) elicit changes in arterial carbon dioxide and oxygen (CO2 and O2) chemostimuli. These chemostimuli elicit synergistic increases in cerebral blood flow (CBF) and sympathetic nervous system activation, with the latter increasing systemic blood pressure. The extent that simultaneous and inverse changes in arterial CO2 and O2 and associated increases in blood pressure affect the CBF responses during RB versus VAs are unclear. We instrumented 21 healthy participants with a finometer (beat-by-beat mean arterial blood pressure; MAP), transcranial Doppler ultrasound (middle and posterior cerebral artery velocity; MCAv, PCAv) and a mouthpiece with sample line attached to a dual gas analyzer to assess pressure of end-tidal (PET)CO2 and PETO2. Participants performed two protocols: RB and a maximal end-inspiratory VA. A second-by-second stimulus index (SI) was calculated as PETCO2/PETO2 during RB. For VA, where PETCO2 and PETO2 could not be measured throughout, SI values were calculated using interpolated end-tidal gas values before and at the end of the apneas. MAP reactivity (MAPR) was calculated as the slope of the MAP/SI, and cerebrovascular reactivity (CVR) was calculated as the slope of MCAv or PCAv/SI. We found that compared to RB, VA elicited ~ fourfold increases in MAPR slope (P < 0.001), translating to larger anterior and posterior CVR (P ≤ 0.01). However, cerebrovascular conductance (MCAv or PCAv/MAP) was unchanged between interventions (P ≥ 0.2). MAP responses during VAs are larger than those during RB across similar chemostimuli, and differential CVR may be driven by increases in perfusion pressure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The cardiorespiratory system is continuously exchanging blood gases between the external environment and metabolically active tissue. Metabolism utilizes arterial oxygen (O2), while simultaneously increasing venous carbon dioxide (CO2), a bioproduct of metabolism. Both voluntary rebreathing of expired air and apneas elicit changes in the partial pressures of respiratory gases at the metabolic rate. Specifically, without the ability to exchange gases with atmospheric air, the pressure of arterial (Pa)CO2 increases (hypercapnia) and PaO2 modestly decreases (hypoxia); this asphyxia causes significant physiological stress. In particular, the cerebral circulation is highly responsive to both hypercapnia and hypoxia, both of which facilitate cerebrovascular dilation and increases in cerebral blood flow (CBF; i.e., cerebrovascular reactivity; CVR; reviewed by Willie et al. (2012, 2014). Hypercapnia and hypoxia also activate the sympathetic nervous system through stimulation of central (brainstem) and peripheral (carotid body) chemoreceptors, which increases systemic blood pressure. Cerebral autoregulation is believed to buffer steady-state increases in cerebral perfusion pressure stabilizing CBF; however, the cerebrovasculature is pressure passive to acute changes, where brief elevations in blood pressure translate to increased CBF despite autoregulation, transiently increasing cerebral perfusion (e.g., Lucas et al. 2010; Smirl et al. 2015) These periods of hyperperfusion may be damaging to the cerebral vasculature in populations with impaired cerebral autoregulation (e.g., individuals with sleep apnea), contributing to increased stroke risk (Urbano et al. 2008).
Battisti-Charbonney et al. (2011) demonstrated that rebreathing causes a moderate increase in arterial blood pressure and CBF. They observed that vasodilation and cerebrovascular reactivity only increased CBF to a plateau. Once a maximum dilation has been reached, increases in perfusion pressure, driven by elevated systemic blood pressure, further contribute to increases in CBF. In addition, a separate study from our group demonstrated that muscle sympathetic nervous system (mSNS) activity is larger during voluntary apneas when compared to rebreathing at similar blood gas chemostimuli (Busch et al. 2019). Together, these findings suggest that the combined chemostimuli and augmented sympathetically mediated increase in perfusion pressure may produce exaggerated hyperperfusion compared to asphyxic rebreathing. With that in mind, augmented sympathetic activity may still be one mechanism linking pathologies such as sleep apnea to elevated risk of cardiovascular disease.
We aimed to characterize the differential effects of both asphyxic rebreathing and wakeful voluntary apneas on blood pressure and concomitant CBF velocity responses in anterior and posterior cerebrovasculature to (1) evaluate the effect of RB as compared to VA on MAP and anterior and posterior cerebral artery blood velocity and (2) to determine the effect of the surges in blood pressure on the cerebral circulation. We hypothesized that the increases in blood pressure and thus CBF velocity, would be larger during apneas compared to rebreathing due to a synergistic effect of blood gas challenges and sympathetically mediated increases in systemic blood pressure.
Methods and materials
Ethics and recruitment
This study received ethical approval in advance from the University of Alberta Human Research Ethics Board (Protocol #00048741), was harmonized with the Mount Royal University Human Research Ethics Board (Protocol #102663) and abided by the Canadian Government Tri-Council Policy Statement (TCPS2) for Integrity in Research, and the Declaration of Helsinki, except for registration in a data base. Twenty-three young, healthy male and female participants were recruited. All participants were free from taking prescription drugs, aside from oral contraceptives, were non-smokers and had no known existing cardiovascular, respiratory, or neurological diseases at the time of the study. Participants were asked to refrain from ingesting any caffeine or alcohol and engaging in vigorous exercise for 12-h before the experiment. Timing of the ovarian cycle was not considered in the recruitment of females for this study, and data from males and females were pooled to obtain a large representative sample of the population.
Once participants were pre-screened and provided verbal and written, informed and voluntary consent, they were brought into the laboratory to be familiarized with the equipment and protocol. Participant recruitment and data collection overlap investigations on effects of cerebrovascular responses on voluntary-apnea breaking point (Bruce et al. 2016), mSNS activity during rebreathing and voluntary apnea (Busch et al. 2019), and methodological techniques for illustrating voluntary-apnea physiology in laboratory education (Skow et al. 2015). While the study by Bruce et al. (2016) was primarily aimed at methodological development (utilized in the present study) and quantifying CVR in both the anterior and posterior cerebral circulations during voluntary apneas, the present study was focused on comparing blood pressure, cerebrovascular reactivity, and conductance between rebreathing and voluntary apneas. Our specific research question and data collection for the present study were determined a priori.
Instrumentation
Participants sat comfortably in a semi-recumbent position in a chair throughout instrumentation and data collection. All data were collected using a 16-channel PowerLab system [Powerlab/16SP ML880; ADInstruments (ADI), Colorado Springs, CO, USA] and analyzed offline using commercially available software (LabChart Pro software 7.2; ADI). Cardiovascular measurements included recording of ECG (Lead II configuration) and arterial blood pressure (finger photoplethysmography; Finometer Pro, Finapres Medical Systems, Netherlands). Cerebral blood velocity (CBV) of the middle and posterior cerebral arteries (MCA and PCA respectively) were recorded simultaneously in each participant using bilateral transcranial Doppler ultrasound (PMD150B, 2 MHz probes, Spencer Technologies, Redmond, WA, USA or TOC2M, 2 MHz probes, Multigon Industries, Yonkers, NY, USA). Ultrasound probes were fixed and stabilized to insonate the MCA and PCA (either P1 or P2 segments, remaining consistent within participant) through the right and left anterior temporal windows, respectively. Standardized techniques were used to locate and confirm insonation of the two cerebral arteries (e.g., probe placement, direction of flow, resting velocities, and functional tests; Willie et al. 2011). The mean CBV (cm/s) of both the MCA (MCAv) and the PCA (PCAv) were calculated as the mean of the peak-velocity envelope recorded from the transcranial Doppler ultrasound into LabChart. The breathing apparatus included a nose-clip, mouthpiece, personal bacteriological filter, and a gas sampling port to measure continuous CO2 and O2 percentages using a gas analyser, which was calibrated daily (ADI ML206). End-tidal pressures of CO2 and O2 (PETCO2 and PETO2) were measured and corrected for body temperature and pressure, saturated with water vapor (BTPS in Torr) using daily atmospheric pressure (~ 710 mmHg in Edmonton, Alberta, Canada). The mouthpiece was attached to a three-way valve and 6-L rebreathing bag as needed for the various rebreathing and breath-hold maneuvers (outlined in the following subsections).
Experimental protocol
Following instrumentation, participants underwent an initial baseline period of quiet breathing for 5-min. Due to the data collection overlap (Bruce et al. 2016), all participants then underwent an initial rebreathing protocol which was followed by multiple randomized breathing and breath holding protocols (outlined in Skow et al. 2015). The subsequent experimental protocols were separated by 3–5-min washout periods followed by a 2-min baseline period. For the purpose of this study, only the rebreathing and end-inspiratory voluntary-apnea protocols were utilized for comparison.
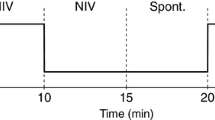
Rebreathing
Participants were coached to pre-fill a disposable 6-L rebreathing bag with expired air during normal breathing. After a period of room air breathing (2-min baseline), the three-way valve was switched to the rebreathing circuit, and the participants began breathing normally from the rebreathing bag. They continued to rebreathe until: (1) they voluntarily terminated the test with a hand signal; (2) their PETCO2 reached 65 Torr; (3) their PETO2 reached 45 Torr; or (4) the bag deflated. MAP, CBV, and end-tidal gases were sampled throughout.
End-inspiratory voluntary apneas
Following recovery, and a 2-min minimal baseline period during which end-tidal gases were obtained, participants were coached to initiate a voluntary maximal end-inspiratory apnea. They were instructed to avoid (1) hyperventilating before the apnea and (2) performing a Valsalva maneuvre, to avoid eliciting unwanted cardiovascular reflexes. At the termination of the apnea, participants exhaled into, and subsequently rebreathed from, the rebreathing circuit for two complete breaths to sample PETCO2 and PETO2 associated with the end of the VA. Mean arterial blood pressure and MCAv and PCAv were sampled throughout, and end-tidal gases were sampled prior to initiation of the apnea and again at the end of the VA.
Data analysis
Previously, Bruce et al. (2016) developed and characterized a method to quantify CBF during apneas, where (1) participants are not exchanging gases with the external environment, making end-tidal (PET) respiratory gas measures impossible and (2) PaCO2 and PaO2 are changing simultaneously. To circumvent these methodological challenges, (1) end-tidal PETCO2 and PETO2 were interpolated from the initial gas values prior to and those at the end of the apneas and (2) a stimulus index (SI) was calculated (PETCO2/PETO2), thus accounting for the simultaneous but inverse effects of these gas challenges on CBF (Bruce et al. 2016). This previously validated method allows for quantification of CVR during apneas (Bruce et al. 2016), where cerebrovascular chemostimuli (i.e., PaCO2 and PaO2) are changing simultaneously at the metabolic rate.
A 1-min mean baseline, at least 1-min prior to each intervention (e.g., rebreathing or voluntary apneas) was averaged to assess baseline cardiorespiratory variables. Given that PaCO2 and PaO2 change simultaneously during rebreathing and apneas, we calculated a SI as the ratio of PETCO2/PETO2 (Bruce et al. 2016). As end-tidal values cannot be measured during voluntary apneas, PETCO2 and PETO2 were interpolated (s−1) between values just prior to the apnea and those obtained at apnea termination (i.e., break point). These interpolated values were then used to calculate the second-by-second SI values throughout voluntary apneas, and we used the same SI ranges between the rebreathing and voluntary-apnea interventions, within individual. Subsequently, we analyzed all variables over a 10-s average bin at the maximal SI for both interventions. Lastly, we then plotted mean arterial pressure (MAP), PCAv, MCAv, MCAv conductance (MCAv CVC; MCAv/MAP), and PCAv CVC for both rebreathing and voluntary apneas over the same SI ranges. The slope of each response was calculated to represent the magnitude of the MAP, CVR, and CVC, which was compared between rebreathing and apnea interventions.
Statistical analysis
All baseline variables for both interventions were compared using a two-tailed paired t test. To compare the cerebrovascular responses to rebreathing and voluntary apneas, MAP, MCAv, PCAv, MCAv CVC, and PCAv CVC were plotted against the same SI range. The SI range length was determined by the shortest intervention between either the rebreathing or voluntary apnea, within-individual, since termination of both protocols was not time dependent. The magnitude (i.e., slope) of these responses was compared between interventions using two-tailed paired t tests. Additionally, to compare the cerebrovascular metrics at the end-point SI values of the interventions, two-tailed paired t tests were utilized. The effect size of the differences was assessed using Hedges’ g, calculated as the difference between sample means divided by the pooled and weighted standard deviation. Additionally, following the recruitment and analysis, since the proportion of sexes were roughly equal, we also tested for sex differences posteriori. Two-tailed unpaired t tests were used to test for potential sex differences between interventions for all variables. All statistical tests were performed using GraphPad Prism (v9.1.2), with significant differences assumed when P < 0.05).
Results
21 participants (11 females, 10 males; 25.2 ± 4.2 years old; body mass index of 23.2 ± 3.1 kg/m2) were included in the final data analysis out of the 23 originally recruited. One participant was excluded because we were unable to establish a matching SI range for comparison. A second participant’s data was omitted due to technical difficulties during data collection. Baseline resting hemodynamic and cerebral measurements are represented in Table 1. Of note, the cerebrovascular baseline variables were recovered prior to the subsequent voluntary-apnea trial, whereas blood gases and MAP remained mildly but significantly different. Regardless of small differences in baseline data between trials, our data demonstrate significant and large magnitude responses during interventions, outlined below.
We further compared the extent of each intervention on the hemodynamic and cerebrovascular parameters by comparing within-participant measurements at the end SI point of each protocol. Both MAP and CVR parameters were significantly higher during the voluntary apneas, while CVC and SI end points for both protocols were not significantly different (Table 1). However, not all of the parameters had sufficient time to return to baseline between interventions.
A representative single participant’s raw tracing demonstrating the quantification of hemodynamic responses to both interventions suggest elevated reactivity (measured via slope) during the voluntary-apnea protocol, compared to rebreathing (Fig. 1A–C).
A–C Representative cardiovascular and cerebrovascular responses to rebreathing (RB) and voluntary apneas (VA). D–F Hemodynamic slopes for all subjects. A–C Mean arterial pressure (MAP; mmHg) and middle cerebral artery velocity (MCAv; cm/s) responses to increasing stimulus index (SI; PETCO2/PETO2) within the same CO2 and O2 range (0.52–0.66) from a single representative participant. D–F Differences within all participants in mean arterial pressure slope (MAP slope; mmHg/SI), middle cerebral artery velocity slope (MCAv slope; cm/s/SI), and posterior cerebral artery velocity slope (PCAv Slope; cm/s/SI) between rebreathing (RB) and voluntary apneas (VA). A RB elicited a 76.9 mmHg/SI change and VA a 250.1 mmHg/SI change. B RB elicited a 111.9 cm/s/SI change and VA a 248.6 cm/s/SI change. C RB elicited a 51.5 cm/s/SI change and a VA 118.3 change. D–F RB slopes were significantly smaller than that of VA. Dots represent individual participant responses, with lines connecting each participant between interventions. Bars represent group means, whereas error bars represent standard deviation. Specific P values reported on each graph
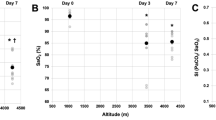
The mean slope of each hemodynamic and cerebrovascular response indicates a significant increase in MAP (n = 21; statistical power = 0.98), and MCAv (n = 21, statistical power = 0.97) and PCAv (n = 20; statistical power = 0.57; Fig. 1D–F; Table 2), during the VA protocol when compared to the RB. Conversely, MCAv and PCAv CVC (Fig. 2A, B; Table 2) were not significantly different, suggesting that the increased CVR may be a consequence of elevated MAP responses. Analysis performed posteriori of MAP, MCAv, PCAv, MCAv CVC, and PCAv CVC between sexes yielded no statistical significance (P ≥ 0.1; data not shown).
Cerebrovascular conductance (CVC) responses to rebreathing (RB) and voluntary apneas (VA). Comparisons between middle cerebral artery conductance slope (MCAv CVC; cm/s/mmHg/SI) and posterior cerebral artery conductance slope (PCAv CVC; cm/s/mmHg/SI) between rebreathing (RB) and voluntary apnea (VA). A–B RB slopes were not significantly different from VA. Dots represent individual participant responses, with lines connecting each participant between interventions. Bars represent group means, whereas error bars represent standard deviation. Specific P values reported on each graph
Discussion
We sought to characterize the differential effects of both rebreathing and voluntary apneas on blood pressure and its subsequent contribution to cerebral blood flow in both anterior and posterior cerebrovasculature. Compared to rebreathing, we found around a fourfold increase in MAP slope corresponding with larger blood flow velocity responses in both the anterior and posterior cerebral circulation during voluntary apneas compared to rebreathing, within similar ranges of chemostimuli. The elevated hemodynamic responses associated with VAs can be observed in both the MAP and CVR slopes (Fig. 1), and the end-point values for each intervention (Table 1). However, there were no differences between rebreathing and voluntary apneas in MCA and PCA CVC, suggesting the larger CVR observed with voluntary apneas were a result of the larger MAP response (Fig. 2). Our data highlight cerebrovascular hyperperfusion during apneas that exceeds that during similar blood gas perturbations associated with asphyxic rebreathing.
Cardiovascular responses are larger during voluntary apneas compared to rebreathing
The mean MAP was markedly increased during the voluntary apneas when compared to rebreathing within the same chemostimuli (i.e., SI) range. This observed hemodynamic response corroborated previous findings indicating that voluntary apneas further contribute to elevated sympathetic activation beyond the initial chemoreflex (Busch et al. 2019). Systemic blood pressure is directly modulated via increases in sympathetic outflow, which facilitates increases in both cardiac output and peripheral vasoconstriction, resulting in an increase in blood pressure (Fisher and Paton 2012). Breathing has a suppressive effect on sympathetic outflow (Hagbarth and Vallbo 1968), whereby increased pulmonary stretch receptor feedback during inspiration suppresses the SNS response to blood gas challenges (Hagbarth and Vallbo 1968; Steinback et al. 2010). During both voluntary and non-voluntary apneas, suppression of SNS activity is not present (Busch et al. 2019), which was illustrated by the increased MAP response during VA in our study. These increases in MAP translate to increased in CBF, independent of chemostimuli magnitude.
Elevated cerebrovascular responses may be a consequence of acute cardiovascular changes
The relative increases in both MCAv and PCAv between interventions followed the same trend as MAP, indicating a significantly larger increase in CBV during the VA protocol when compared to rebreathing. These findings further corroborate the observations of Battisti-Charbonney et al. (2011), where they found that before reaching the hypercapnic range (~ 45 mmHg), both increases in CO2 and decreases in O2 levels contribute to vasodilation within the cerebrovasculature (i.e., CVR). This vasodilation facilitates a linear increase in CBF proportionate to increasing CO2 during both hypoxic and normoxic rebreathing. However, upon reaching maximal vasodilation, cerebral blood flow reaches an asymptote and plateaus. Beyond this hypercapnic range, SNS activity is augmented via contribution from both the peripheral and central chemoreceptors, stimulating an enhanced systemic blood pressure that further contributes to the chemostimuli-induced CVR, driving cerebral blood flow beyond the plateau (Battisti-Charbonney et al. 2011).
Our comparison of CBF CVC was to further investigate the contribution of SNS mediated increases in blood pressure on CBF. The lack of significant differences in CVC in the two protocols suggest that the increased CVR observed during the VAs across the same SI ranges was indeed a consequence of elevated MAP when compared to rebreathing. Thus, cerebral vasodilation has no, or negligible, influence on CBF beyond maximal dilation of the cerebral vasculature, and that augmentation of MAP, via enhanced SNS activity, is necessary to further increase cerebral perfusion.
Methodological considerations
Previous literature has shown that both hypoxia and hypercapnia modify the metabolic rate. Hypoxia has been shown to contribute to an initial increase in oxidative metabolism (Vestergaard et al. 2016), while extreme hypercapnia has been shown to have a suppressive effect (Bain et al. 2017). Thus, the initial hypoxia-mediated increase in metabolism is likely offset by the suppressive effects associated with hypercapnia (Bain et al. 2017). However, most studies have explored prolonged exposure to blood gas challenges, whereas the mean response quantification duration for our VA intervention was ~ 68 s, normal for untrained individuals. Thus, we anticipate that the cerebral metabolic rate was likely unchanged during our short VA interventions, suggesting that the assumption of a constant metabolic rate and linear accumulation of chemostimuli is likely appropriate. However, to our knowledge, the relationships between hypoxia and hypercapnia and the metabolic rate has not been explored in shorter repetitive apneas, such as those associated with obstructive sleep apnea (OSA). Given the short duration of our apneas and the validation of the SI technique (Bruce et al. 2016), we suggest that quantifying a linear increase in chemostimuli (i.e., constant metabolic rate) is likely a sufficient method to assess CVR during short duration VA interventions.
Individuals who experience recurrent exposure to hypoxia and hypercapnia are known to experience altered functionality and plasticity of the peripheral chemoreceptors (carotid bodies; Kumar and Prabhakar 2012; Prabhakar et al. 2007). Sequential apneic events would more closely model the chronic apneic nature observed in patients with OSA and allow for observation of plasticity. Regardless, our data clearly show that, in healthy humans, VAs elicit larger MAPR and CVR when compared to rebreathing, suggesting that chemostimuli are only part of the stimuli leading to increases in CBF during VAs.
More refined techniques are required to further elucidate the exact mechanisms contributing to the observed increase in CBV. It is important to acknowledge that recent findings indicate that sympathetic nerve activity may affect CBV via increased cerebrovascular resistance (Tymko et al. 2020). We also used TCD which may underestimate the effect of sympathetic and PaCO2 related vasoconstriction on CBF (Ainlsie and Hoiland 2014; Verbree et al. 2014). TCDs operate under the assumption that conduit (MCA/PCA) diameter remains constant despite changes in PaCO2, and thus, velocity is proportional to flow (Ainslie and Hoiland 2014). However, PaCO2 has been shown to affect MCA diameter resulting in an overestimation during hypocapnia and an underestimation during hypercapnia (Ainlsie and Hoiland 2014, Coverdale et al. 2014; Verbree et al. 2014). In the future, MRI or duplex ultrasound could be used for a more accurate measurements during these inerventions. The study could also be further refined by giving adequate time between each protocol and measuring VA during normal tidal ventilation to avoid additional SNS stimulation from the unloading of low-pressure baroreceptors during maximal end-inspiratory VAs (Macefield and Wallin 1995; Macefield et al. 2006).
Potential clinical significance
Our findings assessing CBF responses to VAs in healthy individuals may have applications for understanding cerebrovascular control and disease risk in OSA. OSA is characterized by intermittent bouts of involuntary breathing cessation during sleep. These bouts can last from 10 to 50 s (Flemons et al. 1999), during which PaCO2 and PaO2 parallel the response of a voluntary apnea, resulting in subsequent changes in blood gases and increases in systemic blood pressure (Foster et al. 2007, 2010). Our data suggest these swings in blood pressure may contribute to cerebrovascular hyperperfusion, which may be damaging to downstream arterioles and capillaries via acute insult or remodeling (Urbano et al. 2008). In addition, transient hyperperfusion may result in greater washout of metabolically derived CO2 from the brainstem, reducing central respiratory chemoreceptor activation below an apneic threshold during sleep, potentially predisposing individuals to subsequent apneas (Ainslie and Duffin 2009; Dempsey 2005).
In the context of OSA, the intermittent apnea-related elevation in blood pressure and associated cerebral blood flow lead to repeated intermittent cycles of transient hypoxia and hyperperfusion (Bålfors and Franklin 1994; Urbano et al. 2008). Intermittent hypoxia is also believed to contribute to oxidative stress, contributing to impairment of cerebral autoregulation (Foster et al. 2007). Taken together, impaired cerebral autoregulation paired with the shearing stress from intermittent surges in blood pressure and cerebral blood flow may contribute to vascular damage and risk of ischemic stroke (Urbano et al. 2008). We believe that the lack of suppressive effect of dynamic ventilation on sympathetic activation during apneas is a major contributing factor to the observed lack of nighttime blood pressure reduction in OSA patients (Crinion et al. 2019), potentially exacerbating the cycle of hypertension and cardiovascular-related morbidity and mortality, contributing to elevated stroke risk (e.g., Javaheri et al. 2017).
Conclusions
We sought to compare superimposed chemostimuli and hemodynamic responses between rebreathing and voluntary-apnea interventions to determine whether apneic episodes result in larger elevations in CBF. The previously demonstrated elevated SNS activity associated with voluntary apneas likely contributes to markedly increased levels of systemic blood pressure and cerebral blood flow during apneas. Our findings suggest that the absence of dynamic ventilation during apneas further contribute to elevated systemic blood pressure, driving CBF beyond what localized vasodilation to chemostimuli permits.
Availability of data and material
The deidentified data from this study will be made available upon reasonable request by request to the corresponding author by a qualified researcher.
Code availability
Not applicable.
Abbreviations
- CBF:
-
Cerebral blood flow
- CBV:
-
Cerebral blood velocity
- MAP:
-
Mean arterial blood pressure
- MAPR:
-
Mean arterial blood pressure reactivity
- MCAv:
-
Middle cerebral artery blood velocity
- PCAv:
-
Posterior cerebral artery blood velocity
- P ETCO2/O2 :
-
Pressure of end-tidal CO2/O2
- SI:
-
Stimulus index (PETCO2/PETO2)
- CVR:
-
Cerebrovascular reactivity
- CVC:
-
Cerebrovascular conductance
- PaCO2/O2 :
-
Partial pressure of CO2/O2
References
Ainslie PN, Duffin J (2009) Integration of cerebrovascular CO2 reactivity and chemoreflex control of breathing: mechanisms of regulation, measurement, and interpretation. Am J Physiol Regul Integr Comp Physiol 296(5):R1473–R1495
Ainslie PN, Hoiland RL (2014) Transcranial Doppler ultrasound: valid, invalid, or both? J Appl Physiol 117:1081–1083
Bain AR, Ainslie PN, Barak OF, Hoiland RL, Drvis I, Mijacika T, Bailey DM, Santoro A, DeMasi DK, Dujic Z, MacLeod DB (2017) Hypercapnia is essential to reduce the cerebral oxidative metabolism during extreme apnea in humans. J Cereb Blood Flow Metab 37:3231–3242
Bålfors EM, Franklin KA (1994) Impairment of cerebral perfusion during obstructive sleep apneas. Am J Respir Crit Care Med 150:1587–1591
Battisti-Charbonney A, Fisher J, Duffin J (2011) The cerebrovascular response to carbon dioxide in humans. J Physiol 589:3039–3048
Bruce CD, Steinback CD, Chauhan UV, Pfoh JR, Abrosimova M, Vanden Berg ER, Skow RJ, Davenport MH, Day TA (2016) Quantifying cerebrovascular reactivity in anterior and posterior cerebral circulations during voluntary breath holding. Exp Physiol 101:1517–1527
Busch SA, Bruce CD, Skow RJ, Pfoh JR, Day TA, Davenport MH, Steinback CD (2019) Mechanisms of sympathetic regulation during apnea. Physiol Rep 7:1–14
Coverdale NS, Gati JS, Opalevych O, Perrotta A, Shoemaker JK (2014) Cerebral blood flow velocity underestimates cerebral blood flow during modest hypercapnia and hypocapnia. J Appl Physiol 117:1090–1096
Crinion SJ, Ryan S, Kleinerova J, Kent BD, Gallagher J, Ledwidge M, McDonald K, McNicholas WT (2019) Nondipping nocturnal blood pressure predicts sleep apnea in patients with hypertension. J Clin Sleep Med 15:957–963
Dempsey JA (2005) Crossing the apnoeic threshold: causes and consequences. Exp Physiol 90(1):13–24
Fisher JP, Paton JFR (2012) The sympathetic nervous system and blood pressure in humans: implications for hypertension. J Hum Hypertens 26:463–475
Flemons WW, Buysse D, Redline S, Oack A, Strohl K, Wheatley J, Young T, Douglas N, Levy P, McNicolas W, Fleetham J, White D, Schmidt-Nowarra W, Carley D, Romaniuk J (1999) Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. Sleep 22:667–689
Foster GE, Poulin MJ, Hanly PJ (2007) Intermittent hypoxia and vascular function: implications for obstructive sleep apnoea. Exp Physiol 92:51–65
Foster GE, Hanly PJ, Ahmed SB, Beaudin AE, Pialoux V, Poulin MJ (2010) Intermittent hypoxia increases arterial blood pressure in humans through a renin-angiotensin system-dependent mechanism. Hypertension 56:369–377
Hagbarth KE, Vallbo ÅB (1968) Discharge characteristics of human muscle afferents during muscle stretch and contraction. Exp Neurol 22:674–694
Javaheri S, Barbe F, Campos-Rodriguez F, Dempsey JA, Khayat R, Javaheri S, Malhotra A, Martinez-Garcia MA, Mehra R, Pack AI, Polotsky VY, Redline S, Somers VK (2017) Sleep apnea: types, mechanisms, and clinical cardiovascular consequences. J Am Coll Cardiol 69(7):841–858
Kumar P, Prabhakar NR (2012) Peripheral chemoreceptors: function and plasticity of the carotid body. Compr Physiol. https://doi.org/10.1002/cphy.c100069
Lucas SJE, Tzeng YC, Galvin SD, Thomas KN, Ogoh S, Ainslie PN (2010) Influence of changes in blood pressure on cerebral perfusion and oxygenation. Hypertension 55:698–705
Macefield VG, Gandevia SC, Henderson LA (2006) Neural sites involved in the sustained increase in muscle sympathetic nerve activity induced by inspiratory capacity apnea : a fMRI study. J Appl Physiol 100:266–273
Macefield VG, Wallin BG (1995) Effects of static lung inflation on sympathetic activity in human muscle nerves at rest andduring asphyxia. J Auton Nerv Syst 53(2–3):148–156. https://doi.org/10.1016/0165-1838(94)00174-i. PMID: 7560751
Prabhakar NR, Peng Y-J, Kumar GK, Pawar A (2007) Altered carotid body function by intermittent hypoxia in neonates and adults: Relevance to recurrent apneas. Respir Physiol Neurobiol 157:148–153
Skow RJ, Day TA, Fuller JE, Bruce CD, Steinback CD (2015) The ins and outs of breath holding: simple demonstrations of complex respiratory physiology. Adv Physiol Educ 39:223–231
Smirl JD, Hoffman K, Tzeng YC, Hansen A, Ainslie APN (2015) Methodological comparison of active- and passive-driven oscillations in blood pressure; implications for the assessment of cerebral pressure-flow relationships. J Appl Physiol 119:487–501
Steinback CD, Breskovic T, Frances M, Dujic Z, Shoemaker JK (2010) Ventilatory restraint of sympathetic activity during chemoreflex stress. Am J Physiol Regul Integr Comp Physiol 299:1407–1414
Tymko MM, Fraser GM, Matenchuk BA, Day TA, Boulé NG, Davenport MH, Steinback CD (2020) Determining whether sympathetic nervous activity influences cerebral blood velocity at rest: a novel approach. Clin Auton Res 30:357–359
Urbano F, Roux F, Schindler J, Mohsenin V (2008) Impaired cerebral autoregulation in obstructive sleep apnea. J Appl Physiol 105:1852–1857
Verbree J, Bronzwaer ASGT, Ghariq E, Versluis MJ, Daemen MJAP, Van Buchem MA, Dahan A, Van Lieshout JJ, Van Osch MJP (2014) Assessment of middle cerebral artery diameter during hypocapnia and hypercapnia in humans using ultra-high-field MRI. J Appl Physiol 117:1084–1089
Vestergaard MB, Lindberg U, Aachmann-Andersen NJ, Lisbjerg K, Christensen SJ, Law I, Rasmussen P, Olsen NV, Larsson HB (2016) Acute hypoxia increases the cerebral metabolic rate—a magnetic resonance imaging study. J Cereb Blood Flow Metab 36:1046–1058
Willie CK, Colino FL, Bailey DM, Tzeng YC, Binsted G, Jones LW, Haykowsky MJ, Bellapart J, Ogoh S, Smith KJ, Smirl JD, Day TA, Lucas SJ, Eller LK, Ainslie PN (2011) Utility of transcranial Doppler ultrasound for the integrative assessment of cerebrovascular function. J Neurosci Methods 196(2):221–237
Willie CK, Macleod DB, Shaw AD, Smith KJ, Tzeng YC, Eves ND, Ikeda K, Graham J, Lewis NC, Day TA, Ainslie PN (2012) Regional brain blood flow in man during acute changes in arterial blood gases. J Physiol 590:3261–3275
Willie CK, Tzeng YC, Fisher JA, Ainslie PN (2014) Integrative regulation of human brain blood flow. J Physiol 592:841–859
Acknowledgements
We are grateful to our participants for their time and effort in supporting our study.
Funding
Funding was provided by Natural Sciences and Engineering Research Council of Canada Discovery Grants (TAD: grant 04915; CDS: 06637).
Author information
Authors and Affiliations
Contributions
TAD, CDS and MHD, conception or design of the work; All co-authors, acquisition, analysis, or interpretation of data for the work; ALM, CDB, NDJS, CDS, TAD, drafting of the work or revising it critically for important intellectual content; All co-authors approved the final version of the manuscript and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All persons designated as authors qualify for authorship, and all those who qualify for authorship are listed.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
This study received ethical approval in advance from the University of Alberta Human Research Ethics Board (Protocol #00048741), was harmonized with the Mount Royal University Human Research Ethics Board (Protocol #102663) and abided by the Canadian Government Tri-Council Policy Statement (TCPS2) for Integrity in Research, and the Declaration of Helsinki, except for registration in a data base.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
The authors affirm that human research participants provided informed consent for publication of the deidentified, numerical data.
Additional information
Communicated by I. Mark Olfert.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Marullo, A.L., Bruce, C.D., Pfoh, J.R. et al. Cerebrovascular and blood pressure responses during voluntary apneas are larger than rebreathing. Eur J Appl Physiol 122, 735–743 (2022). https://doi.org/10.1007/s00421-021-04864-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-021-04864-5