Abstract
Purpose
This pilot pre-and post-intervention study investigated the effects of a short-term aquatic exercise programme on physiological outcomes, symptoms and exercise capacity in women with chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME).
Methods
Eleven women (54.8 ± 12.4 year) volunteered for the 5-week program; an initial 20-min aquatic exercise session then two self-paced 20-min sessions per week for 4 weeks. Pre- and post-intervention outcomes were physiological measures, 6 min Walk Test (6MWT), perceived exertion (RPE), hand grip strength, Sit-to-Stand, Sit-Reach test, Apley’s shoulder test, FACIT questionnaire, and 24-h post-test tiredness and pain scores (0–10 visual analogue scale). Heart rates, RPE, 24- and 48-h post-session tiredness/pain scores were recorded each session.
Results
6MWT distance increased by 60.8 m (p = 0.006), left hand grip strength by 6 kg (p = 0.038), Sit-Reach test by 4.0 cm (p = 0.017), right shoulder flexibility by 2.9 cm (p = 0.026), FACIT scores by 8.2 (p = 0.041); 24-h post-test tiredness and pain decreased by 1.5 and 1.6, respectively (p = 0.002). There were significant post-intervention increases in exercising heart rates (6MWT 4- and 6-min time points), oxygen saturation at 2-min, and reduced RPE at 4-min. Weekly resting and exercising heart rates increased significantly during the study but RPE decreased; immediately post- and 24-h post-session tiredness decreased significantly. There were no reports of symptom exacerbation.
Conclusions
Five weeks of low-moderate intensity aquatic exercise significantly improved exercise capacity, RPE and fatigue. This exercise mode exercise may potentially be a manageable and safe physical activity for CFS/ME patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic Fatigue Syndrome or Myalgic Encephalomyelitis (CFS/ME) is characterised by disabling fatigue for more than 6 months with no other apparent cause, and any four of the following symptoms: post-exertional malaise (PEM), headaches, impaired concentration and memory, swollen and painful lymph nodes, sore throat, muscle and joint pain, and unrefreshing sleep (Carruthers et al. 2011). The pathogenesis of CFS/ME remains unclear; viral, neuroendocrine and/or psychological events such as trauma or extreme emotional stress can contribute to the development of this debilitating illness (Carruthers et al. 2011). CFS/ME is often complicated by co-conditions such as fibromyalgia syndrome (FMS), occurring in up to 70% of CFS/ME patients (Cook et al. 2006; IOM 2015; McManimen and Jason 2017), postural orthostatic tachycardia syndrome (POTS) which occurs in 20–34% of patients (Benarroch 2012; Hoad et al. 2008), cognitive and neurological symptoms.
The recovery from CFS/ME is uncertain (IOM 2015). Earlier studies reported that full recovery occurs in less than 10% of diagnosed patients (Moss-Morris et al. 2005; Taylor and Kielhofner 2005). The frequency of those who do return to employment or education varies from 8 to 52% (Stormorken et al. 2017), but the majority of those considered to have “recovered” rarely return to pre-illness health and physical function (Adamowicz et al. 2014; Andersen et al. 2004; Taylor and Kielhofner 2005). Current management of CFS/ME includes alleviation of symptoms through rest, specialist medical care (including medications), relaxation therapy, cognitive behavioural therapy counselling, graded exercise therapy (GET) and adaptive pacing (Larun et al. 2017), but not all individuals respond to such treatments (McManimen and Jason 2017; Moss-Morris et al. 2005). Individuals with CFS/ME who remain sedentary are likely to become physically deconditioned and may be more at risk of developing lifestyle illnesses such as cardiovascular disease, type 2 diabetes and cancer. However, the most appropriate modes of exercise for CFS/ME patients remain uncertain, as PEM and symptom exacerbation are common in patients who attempt physical activity (McManimen and Jason 2017).
Aquatic exercise and hydrotherapy are recommended modalities of treatment for pathologies such as FMS (Bidonde et al. 2014; Busch et al. 2011; Mannerkorpi et al. 2009; Wilson et al. 2012), the arthritides (Becker 2009), multiple sclerosis (MS) (Becker 2009; Castro-Sanchez et al. 2012; Plecash and Leavitt 2014; Verhagen et al. 2012), and chronic obstructive pulmonary disease (COPD) (Becker 2009; McNamara et al. 2015), yet there has been little research to date with CFS/ME patients. Two studies combined strength training and 45-min hydrotherapy sessions 5 days per week (Gordon and Lubitz 2009), and strength or aerobic training plus hydrotherapy (Gordon et al. 2010). The studies utilised a 4-week hospital in-patient programme, resulting in significant improvements in strength, aerobic capacity and depression in adolescents with CFS/ME although the authors did not discuss the contribution of the hydrotherapy component to the overall results. Swimming has been suggested as a possible mode for GET (Wallman et al. 2004), but there is no further mention of aquatic exercise or hydrotherapy in the CFS/ME literature.
The therapeutic value of aquatic exercise relies on the hydrodynamic properties of water, such as buoyancy, relative density, resistance, viscosity, turbulence, and hydrostatic pressure and flow (Macias-Hernandez et al. 2015). Water temperature also enhances physiological and sensory effects (Honda and Kamioka 2012; Macias-Hernandez et al. 2015). Hydrotherapy and aquatic exercise provide physiological benefits such as pain reduction through the blockage of nociceptive signals (Assis et al. 2006; Castro-Sanchez et al. 2012; Honda and Kamioka 2012); increased blood flow (Becker 2009; Honda and Kamioka 2012); muscle relaxation and reduced fatigue (Bidonde et al. 2014; Busch et al. 2011); reduced peripheral oedema, which may also assist in pain reduction (Gabrielsen et al. 2000; Honda and Kamioka 2012); reduced sympathetic nervous system (SNS) activity and orthostatic intolerance, and enhanced autonomic function (Becker 2009); and reduced mechanical loading on joints (Castro-Sanchez et al. 2012). Aquatic exercise may also enhance physical function (strength and aerobic capacity) (Assis et al. 2006; Becker 2009; Kanitz et al. 2015; Meredith-Jones et al. 2011). Increased aerobic capacity can be attributed to enhanced cardiac output and stroke volume, and lower heart rate (HR), as increased venous pressure and vasodilation force blood from lower extremities to the thoracic cavity and heart (Becker 2009; Torres-Ronda and del Alcazar 2014). Central and peripheral adaptions also contribute to increases in peak oxygen consumption with water-based training, comparable to land-based aerobic exercise (Becker 2009). There is further evidence that cool water exercise provides thermal conductivity benefits for patients with thermal instability (Torres-Ronda and del Alcazar 2014). Joint and muscle pain, fatigue, thermal regulation, orthostatic intolerance, and autonomic dysregulation are also common in CFS/ME (Benarroch 2012; McManimen and Jason 2017), thus aquatic exercise might potentially be beneficial.
There is substantial evidence that the mechanical properties of water combined with the physiological benefits of exercise provide symptom relief and enhanced physical capacity for a range of musculoskeletal and neurological conditions (Bidonde et al. 2014; Macias-Hernandez et al. 2015). We hypothesized that self-paced, low-intensity aquatic exercises could reduce pain and fatigue, and increase joint range of motion (ROM), strength and exercise capacity in individuals with CFS/ME. This 5-week pilot study investigated the physiological responses of CFS/ME patients to aquatic exercise, to determine the clinical application of aquatic exercise as a safe and effective rehabilitation exercise modality.
Methods
The pilot study was approved by the Southern Cross University Human Research Ethics Committee (HREC ECN-16-212), and was a pre- and post-intervention study with the participants acting as their own controls. The study was conducted in late 2016, with a 6-week period of advertising and recruitment (August 15th–October 3rd). Participant screening and initial health and exercise assessments were completed between October 10th and 25th. Participants completed the 5 weeks of the exercise intervention (October 28th–November 25th), with post-intervention health and exercise assessments during the following week (November 28th–30th). We phoned all participants 2 weeks later for a follow-up discussion about their health and well-being.
Participants
Participants were recruited from the local area by advertising through the media and university. We recruited patients who had a diagnosis of CFS/ME from their medical practitioner, according to the updated International Consensus Criteria (Carruthers et al. 2011) or the 1994 Centres for Disease Control criteria (Fukuda et al. 1994). Potential participants contacted the researchers by phone and email and were offered the Participant Information Sheet and Informed Consent to Participate. The researchers discussed the project by phone with all potential participants, who were invited to attend the university laboratory for further screening [medical history, cardiovascular risk screening (Exercise and Sports Science Australia 2011)], health questionnaire and assessments. The inclusion criteria were: between the ages of 18–80 years; a medical diagnosis of CFS/ME, post-viral fatigue syndrome or infectious mononucleosis; not participating in a physical activity program or regular exercise; able to communicate in English; able to commit the time to participate in the research; informed consent. Informed consent was obtained from all individual participants included in the study. The exclusion criteria were: any cardiovascular, pulmonary, metabolic, renal, endocrine, autoimmune, neurological, inflammatory condition, infectious disease or mental illness that made exercise participation a risk for participants; any diagnosed medical condition other than CFS/ME that caused severe fatigue; musculoskeletal injuries that prevented exercise participation; being a non-swimmer; an allergy to chlorine or other pool chemicals; being pregnant. Participants who had diagnosed FMS concurrent with CFS/ME were not excluded from the study.
Physical assessments
Participants underwent a series of physiological and exercise assessments prior to, and after, the 5-week exercise intervention. Physical characteristics (age, height, weight, resting HR, and blood pressure), time since symptom onset (TSSO) and time since diagnosis (TSD) were recorded. Primary outcomes consisted of (1) exercise outcome measures: a 6-min Walk Test (6MWT) which included distance completed (m), exercising HR (bpm), oxygen saturation (%) and 0–10 Rate of Perceived Exertion (RPE) (Borg 1982) every 2 min; handgrip strength (kg) (Camry, CA USA), 60 s Sit to Stand (repetitions/60 s), Sit-Reach test and Apley’s Shoulder test (cm); and (2) a pre- and post-intervention Functional Assessment of Chronic Illness Therapy-Fatigue (FACIT Version 4) questionnaire (Cella 1997; Webster et al. 2003), which consists of 13 statements (e.g., “I feel fatigued”, “I feel weak all over”, “I need to sleep during the day”, “I am able to do my usual daily activities”), each requiring one of the following answers: “Not at all”; “A little bit”; “Somewhat”; “Quite a bit”; “Very much”.
Secondary outcomes included tiredness and pain, which were assessed 24 and 48 h after the pre- and post-intervention testing sessions using a 0–10 Visual Analogue Scale (VAS), with participants phoning, texting or emailing their scores to the research team. Other secondary measures were: tiredness, pain and 0–10 RPE which were assessed after each exercise session (immediately post-exercise, 24- and 48-h post-session). Heart rates and RPE prior to, and during, each exercise session were also secondary outcomes. There were no changes to the pilot study outcomes after the intervention had commenced.
Exercise intervention
The aquatic exercise intervention consisted of an initial session lasting between 15 and 20 min, depending on each participant’s physical ability and symptoms. The remaining 4 weeks of the intervention consisted of twice-weekly aquatic sessions with 48–72 h recovery between sessions. The exercise sessions were conducted in a climate controlled indoor deep water pool with a temperature of 27 °C. Participants were instructed in the use of HR monitors (Polar T31, Oulu Finland) and the 0–10 RPE scale, and were asked to keep their exertion levels below 6/10 or “moderately hard”. Pre-exercise HR and RPE were recorded, as were HR and RPE during every 10 min of exercise. Participants were fitted with buoyancy belts and the majority of exercises conducted in deep water, with access to a ramp and chest deep water platform available if required. All participants completed a variety of gentle intensity ROM, strengthening and aerobic water exercises that were performed to music.
Sessions started with a duration of 15 min but gradually increased in time for participants who could increase their exercise capacity. All exercises were self-paced. The warm up and cool down exercises included low-intensity water walking followed by upper and lower limb stretching through all planes of movement. Both the warm up and cool down went for 5 min each. Strength exercises used water resistance, pool noodles and kickboards, and included arm and shoulder circling, bicep curls, triceps push-backs, upper cuts, wrist flexion/extension, pool noodle rows and push-ups, knees to chest, jumping jacks, and squats (in deep water or using the pool platform). Each exercise went for 20–30 s. Short sets of aerobic exercises included water walking, pool noodle cycling, “skiing” using arms and legs, noodle side-stroke, breaststroke swimming, and kicking. Simple floating was also used as a relaxation exercise or a “time out” if the participant felt tired. The aerobic and strength component lasted for approximately 5–10 min, depending on each participant’s levels of energy. Stretching formed part of the cool down and included all muscle groups.
The researcher who led the exercise sessions was an accredited clinical Exercise Physiologist and qualified aquatic instructor experienced in adapted aquatic programming. Final-year exercise science students assisted participants in the pool with instruction and support if needed. 24- and 48-h post-session fatigue, pain and other symptoms were recorded by participants and texted or phoned in to the research team, with participants noting if the symptoms changed or remained the same. Participants were asked to not increase their time in the water, or intensity of exercise if they were symptomatic; they were asked to reduce exercise time or intensity if they felt more symptomatic during a session, and any changes in participant health, well-being or symptoms were recorded by the supervisors. Changes in symptoms 24- and 48-h post each exercise session were also sent in to researchers during the 4-week block. Participants returned to the laboratory in the week following the final aquatic session for post-intervention physiological assessments and a final interview with two members of the research team (qualitative research results not available in this publication).
Data collection and analysis
Participant characteristics were collated from the initial interviews including demographic data such as the TSSO and TSD of CFS/ME symptoms. The primary analysis of the exercise intervention and assessment data with intention-to-treat included all participants regardless of dropout or level of adherence. Intervention compliance for each participant was calculated as the number of completed exercise sessions divided by the nine sessions of the intervention; scores were totalled and expressed as a percentage. Physiological data are presented as mean ± standard deviation. Pre- and post-intervention exercise assessment, pain, tiredness, and fatigue data were recorded and transferred to SPSS (V24, ©IBM) spreadsheets for analysis using a two-tailed paired samples t test. The scores for the FACIT questionnaire were totalled for each participant out of 52 points, pre- and post-intervention, with a score of < 30/52 denoting severe fatigue, and higher scores meaning less fatigue.
Data from each exercise session [resting and training HR (at 10-, 20-min and recovery time points), training RPE (at 5-, 10-, 20-min and recovery time points), pain and tiredness (immediately post-exercise, and 24- and 48-h post-exercise session)] were averaged for each week and recorded in Excel spreadsheets. Data were analysed using a general linear model with repeated measures analysis of variance (ANOVA), with time (week) and training session (time point values) interactions analysed. A Bonferroni adjustment was used to detect significant differences between training session time points for each outcome measure. Statistical significance was set at ˂ 0.050 for both t test and ANOVA analyses. The magnitude of the change between pre- and post-intervention values was reported using a modified Cohen’s effect size (ES) with the following descriptors applied to ES thresholds: 0.0–0.2 trivial, 0.2–0.6 small, 0.6–1.2 moderate, 1.2–2.0 large, > 2.0 very large (Batterham and Hopkins 2006).
Results
The participant characteristics and demographic data are shown in Table 1. Of the eleven participants, seven also had COPD or respiratory problems, six had diagnosed FMS, four reported recurring neurological symptoms (vertigo, migraines), three had thermal instability, and one had POTS. There were no significant post-intervention changes in resting physiological outcomes although there was a trend to increase with HR (p = 0.065 ES 0.34).
Exercise tests
There were significant post-intervention increases in 6MWT distance (p = 0.006 ES 1.23), 6MWT 4-min (p = 0.023 ES 0.57) and 6-min HR (p = 0.018 ES 0.96). RPE decreased at 4-min (p = 0.028 ES 0.44); with a trend to decrease in RPE at 6-min (p = 0.057 ES 0.67) (Table 2). Oxygen saturation at the post-intervention 2-min time point also increased significantly (p = 0.029 ES 0.63).
There were significant improvements in left hand grip strength (p = 0.038 ES 0.79) while right-hand grip strength showed a trend (p = 0.051 ES 0.61); right shoulder ROM (p = 0.026 ES 0.51) while left shoulder ROM showed a trend (p = 0.074 ES 0.45); the Sit-Reach test scores (p = 0.017 ES 0.44); FACIT (p = 0.041 ES 1.00); 24-h post-test tiredness (p = 0.002 ES 0.73) and 24-h post-test pain (p = 0.002 ES 0.92). Immediate post-test tiredness and pain showed trends to decrease post-intervention (p = 0.093 ES 0.48 and p = 0.096 ES 0.54 respectively).
Aquatic exercise sessions
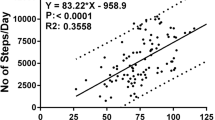
Intervention compliance was 86.9%. Several participants had days where they felt their symptoms were worse or they had other commitments, so did not attend the exercise session. However, there were no adverse events reported during or after training. The weekly changes in the averaged mean RPE, HR, pain and tiredness are shown in Figs. 1, 2, 3 and 4. There was a significant weekly decrease in mean RPE between Week 1 and 5 (p = 0.009 ES 0.48) with a trend decrease between Week 1 and 3 (p = 0.089 ES 0.44). RPE at 10 min of exercise decreased significantly between Week 1 and 4 (p = 0.040 ES 0.61), and Week 1 and 5 (p = 0.031 ES 0.54), with trend decreases between Week 1 and 2 (p = 0.088 ES 0.51) and Week 1–3 (p = 0.050 ES 0.59). RPE at 20 min decreased significantly from Week 1–2 (p = 0.049 ES 0.46) and Week 1–5 (p = 0.020 ES 0.49), with trend decreases from Week 1–3 (p = 0.058 ES 0.46) and Week 1–4 (p = 0.080 ES 0.40). Recovery RPE also decreased between Week 2 and 3 (p = 0.026 ES 0.46) and Week 2 and 5 (p = 0.013 ES 0.63).
There were significant weekly increases in resting HR between Week 1 and 2 (p = 0.003 ES 0.60), week 1 and 3 (p = 0.001 ES 0.75), week 1 and 4 (p = 0.014 ES 0.55), and week 1 and 5 (p = 0.004 ES 0.81). There were also significant increases in HR at the 10-min exercise time point from Week 2–5 (p = 0.013 ES 0.69), week 3–4 (p = 0.042 ES 0.44), and week 3–5 (p = 0.014 ES 0.57) with a trend between week 2 and 4 (p = 0.053 ES 0.59). Within-week changes included significant increases in week 1 between resting and 10-min HR (p = 0.006 ES 1.22), resting and 20-min HR (p = 0.013 ES 1.12) and resting and recovery HR (p = 0.030 ES 0.99); in week 4 between resting and 10-min HR (p = 0.009 ES 1.33), and resting and 20-min HR (p = 0.017 ES 1.00); in Week 5 between resting and 10-min HR (p = 0.039 ES 0.89). There was a significant decrease between 20-min and recovery HR in week 3 (p = 0.049 ES 0.62), and a trend decrease in week 5 between 10-min and recovery HR (p = 0.071 ES 0.81).
Mean tiredness scores decreased between week 1 and 2 (p < 0.001 ES 0.80), week 1 and 3 (p = 0.004 ES 0.47), week 1 and 4 (p = 0.004 ES 0.55) and week 1 and 5 (p = 0.002 ES 0.53). There were also significant decreases in immediate post-session tiredness between week 1 and 2 (p = 0.007 ES 0.59), week 1 and 3 (p = 0.006 ES 0.73), week 1 and 4 (p = 0.015 ES 0.73) and week 1 and 5 (p = 0.044 ES 0.52). Twenty four-hour post-tiredness decreased significantly between week 1 and 2 (p = 0.041 ES 0.48), week 1 and 4 (p = 0.040 ES 0.53) and week 1 and 5 (p = 0.030 ES 0.64). Forty eight-hour post-tiredness showed a trend decrease between Week 1 and 2 (p = 0.062 ES 0.45). There were no significant differences between post-session, 24- or 48-h post-session pain scores each week, nor were there any differences between weeks for these time points.
Discussion
This pre- and post-intervention pilot study investigated the effects of 5 weeks of self-paced, low-intensity aquatic exercises on physiological outcome measures and symptoms in women with CFS/ME. To our knowledge, this is the first study to examine the isolated effects of aquatic exercise with CFS/ME patients. Previous studies by Gordon and Lubitz (2009) and Gordon et al. (2010) included daily hydrotherapy with resistance training or aerobic training for adolescents with CFS/ME who attended a 4-week in-hospital rehabilitation programme. The authors noted significant improvements in aerobic capacity, strength, depression, and quality of life, but while stating the benefits of strength and aerobic training, did not report the contribution made by hydrotherapy to the results. Aquatic exercise is a recommended management modality for patients with FMS, osteoarthritis, and other musculoskeletal conditions (Becker 2009; Bidonde et al. 2014), so it is surprising that this type of exercise has not been previously used with CFS/ME patients, given that up to 70% of these patients have a concurrent diagnosis of FMS, and many have problems with orthostatic intolerance (IOM 2015; McManimen and Jason 2017).
Our most surprising finding was the extent of the improvements in aerobic capacity, measured by increased walking distance. The likely explanations for this result include: (1) increased cardiovascular function (cardiac output, stroke volume, perfusion) due to redistributed blood flow, especially with repeated bouts of exercise (Becker 2009); (2) enhanced oxygen consumption due to peripheral vascular adaptions in response to exercising in water which has a density three times that of air (Becker 2009).This results in a training effect at a relatively lower exercise intensity than on land (Becker 2009), which may partly explain why our cohort increased their aerobic fitness in such a short time. Our cohort was physically deconditioned pre-intervention and such individuals have less lean muscle mass, capillary density, and mitochondrial density (Becker 2009). Therefore, exercise-induced increases in muscle mass would contribute to enhanced peripheral oxygen extraction. Another consideration is that the increased hydrostatic pressure of water also reduces the partial pressure of oxygen, which contributes to the work of breathing by approximately 60% (Meredith-Jones et al. 2011). This cardiorespiratory challenge may improve the strength of the diaphragm and intercostal muscles to enable individuals to increase their ventilation rate during exercise, and therefore, their oxygen uptake and aerobic capacity. Improved cardiorespiratory capacity with water-based exercise has been reported in older adults (Bocalini et al. 2013; Kieffer et al. 2012), neurological patients (Becker 2009; Castro-Sanchez et al. 2012; Salem et al. 2011), and FMS patients, (Bidonde et al. 2014; Gusi et al. 2006; Jentoft et al. 2001; Mannerkorpi et al. 2009), who have the greater overlap with CFS/ME patients in terms of symptoms and fatigue. There are important clinical implications with such improvements because decreases in VO2max with ageing and/or chronic medical conditions contribute significantly to reduced physiological functional capacity, risk of other chronic conditions, and greater morbidity (Becker 2009).
It was interesting to note that while 6MWT distance and exercising HR during the test increased, RPE decreased significantly at the 4-min time point of the test, with a trend to decrease at the 6-min time point. In other words, the participants were able to exercise harder, but their perception of effort was actually lower than during their pre-intervention 6MWT. This result is similar to findings by Wallman et al. (2004), where RPE decreased after a 12-week graded exercise programme. However, we found significant results after only 5 weeks, which suggests that substantial changes in both perceptual and physiological outcomes are possible with short-term training.
Our participants increased hand grip strength significantly and clinically (> 20% increase) during the 5 weeks, with the right-hand final mean value just below, and the left-hand value equalling, the relevant age norm for Australian women (Massy-Westropp et al. 2011). This result supports findings in other aquatic exercise studies (Bocalini et al. 2008; Jentoft et al. 2001; Kieffer et al. 2012). The physiological adaptation is likely due to neural and hypertrophic mechanisms in response to the increased resistance of the upper limbs moving through all planes of motion in water (Bento and Rodacki 2015; Kieffer et al. 2012). Water density provides resistance to movement in all directions (Baena-Beato et al. 2014; Meredith-Jones et al. 2011), which will activate agonist and antagonist muscle groups with all movement phases. This was especially relevant for the shoulder, arm and wrist exercises we used, which involved flexion/extension of the main joints, and forearm pronation/supination. Previous research has shown that it is necessary to activate the antagonist muscle group late in the ROM to decelerate the moving limb and to resist increasing lift forces caused by the buoyancy of water (Meredith-Jones et al. 2011). However, lower limb strength, assessed by the Sit-to-Stand functional test, did not improve. Possibly the muscle movement patterns used during this test (i.e., a squat) were not specific to those used in our aquatic exercises (e.g., water walking and cycling), which were predominantly done as open-chain exercises in deep water. The Sit-to-Stand is a closed-chain, weight-bearing exercise and the buoyancy effects of water training may not have been as effective at increasing the hamstring and quadriceps muscle strength needed for land-based squatting (Bento and Rodacki 2015), although muscle strength needed for walking improved. Our cohort also increased their shoulder and trunk flexibility, possibly because the exercises were performed through as full a ROM as possible for each participant, and because stretching was conducted as part of the cool down. Enhanced trunk, shoulder and upper limb flexibility with aquatic exercise have also been reported in other studies (Baena-Beato et al. 2014; Bergamin et al. 2013; Bocalini et al. 2008).
FACIT scores and 24-h post-exercise test tiredness were significantly lower post-intervention, with a trend decrease immediately post-exercise test. Weekly post-exercise tiredness scores also decreased, with the most significant reductions being in immediately post-exercise session scores throughout the study. Weekly 24- and 48-h post-exercise session tiredness showed the greatest reductions in the initial 3 weeks of the study. Possibly the most substantial physiological adaptations to exercise occurred then, and therefore, participants did not feel so tired or fatigued post-exercise. The rate of adaptation to aquatic exercise has not really been researched, but the cohort reported less tiredness and RPE as the study progressed and their exercise capacity increased. It is important to note that despite the improvements in the FACIT and tiredness scores, participant still considered themselves fatigued at the end of the study; the FACIT scores show a reduction in fatigue post-intervention but not the disappearance of this symptom. This decrease in fatigue, however, could result in an increased ability to perform activities of daily living as a follow-on effect of this exercise modality. There still needs to be longer-term research to investigate the optimal frequency and duration of aquatic exercise for CFS/ME patients, without symptom exacerbation.
The 24-h post-exercise test pain score was significantly lower after the 5-week intervention with a trend decrease in the immediate post-test score. It is possible that the aquatic intervention resulted in an increase in pain threshold for the participants, or reduced sensations and perceptions of pain due to the combined hydrostatic mechanisms of water immersion (Becker 2009; Gabrielsen et al. 2000; Honda and Kamioka 2012). The comparison of weekly post-exercise pain scores, with a time effect, showed a trend towards decreased pain 24-h post-exercise session but no significant pain reduction immediately post-exercise or 48-h post-exercise. The small sample size in our study may be a contributing factor since there is moderate quality evidence that aquatic exercise and hydrotherapy may reduce pain in fibromyalgia, lower back pain and MS (Bidonde et al. 2014; Verhagen et al. 2012; Salem et al. 2011); further studies are needed to assess the benefits for CFS/ME.
We had reasonable adherence to the intervention, considering that PEM and symptom exacerbation are the main reasons CFS/ME patients do not engage in physical activity (McManimen and Jason 2017). It is likely that the emphasis we placed on patient self-pacing, the lack of symptom exacerbation and perception of the aquatic exercise as “fun” contributed to the relatively high attendance (Brass and Federoff 2007; McNamara et al. 2015).
Limitations of the study
This pilot study had a small sample size and whilst we reported many positive results, we are cautious about extrapolating our findings to the larger CFS/ME community. The small number of participants reflects the difficulty of recruiting CFS/ME patients in a rural area where distance and travel were barriers to participation. The lack of randomisation and a control group were also weaknesses of the study, again associated with the difficulty of recruiting large numbers of participants. However, there is support for our findings from other studies with similar cohort sizes, utilising similar aquatic programmes (Jentoft et al. 2001; Gusi et al. 2006; Mannerkorpi et al. 2009; Kieffer et al. 2012; Salem et al. 2011). More robust, randomised controlled studies are warranted.
Conclusion
In summary, the 5-week aquatic exercise intervention provided symptomatic and physiological benefits that increased participant exercise capacity. Further studies are needed to provide evidence for optimal frequency, duration and intensity of aquatic exercise sessions, and if there are longer-term benefits such as behaviour change and sustained reduction in symptoms. This mode of self-paced exercise may potentially benefit CFS/ME patients.
Abbreviations
- ANOVA:
-
Analysis of variance
- BPM:
-
Beats per minute
- CFS:
-
Chronic fatigue syndrome
- COPD:
-
Chronic obstructive pulmonary disease
- ES:
-
Effect size
- FACIT:
-
Functional assessment of chronic illness therapy-fatigue
- FMS:
-
Fibromyalgia syndrome
- HR:
-
Heart rate
- ME:
-
Myalgic encephalomyelitis
- MS:
-
Multiple sclerosis
- PEM:
-
Post-exertional malaise
- POTS:
-
Postural orthostatic tachycardia syndrome
- ROM:
-
Range of motion
- RPE:
-
Rate of perceived exertion
- SD:
-
Standard deviation
- 6MWT:
-
6-min walk test
- SNS:
-
Sympathetic nervous system
- SPSS:
-
Statistical package for the social sciences
- TSD:
-
Time since diagnosis
- TSSO:
-
Time since symptom onset
- VAS:
-
Visual analogue scale
References
Adamowicz J, Caikauskaite I, Friedberg F (2014) Defining recovery in chronic fatigue syndrome: a critical review. Qual Life Res 23(9):2407–2416
Andersen M, Permin H, Albrecht F (2004) Illness and disability in Danish chronic fatigue syndrome patients at diagnosis and 5-year follow-up. J Psychosom Res 56(2):217–229
Assis M et al (2006) A randomized controlled trial of deep water running: clinical effectiveness of aquatic exercise to treat fibromyalgia. Arthritis Rheum 55:57–65. https://doi.org/10.1002/art.21693
Baena-Beato P, Artero EG, Arroyo-Morales M, Robles-Fuentes A, Gatto-Cardia MC, Delgado-Fernández M (2014) Aquatic therapy improves pain, disability, quality of life, body composition and fitness in sedentary adults with chronic low back pain. Controll Clin Trial Clin Rehabilit 28:350–360
Batterham A, Hopkins W (2006) Making meaningful inferences about magnitudes. Int J Sports Physiol Perform 1:50–57
Becker B (2009) Aquatic therapy: scientific foundations and clinical rehabilitation applications. Phys Med Rehabilit 1:859–872. https://doi.org/10.1016/j.pmrj.2009.05.017
Benarroch E (2012) Postural tachycardia syndrome: a heterogeneous and multifactorial disorder. Mayo Clin Proc 87:1214–1225
Bento P, Rodacki A (2015) Muscle function in aged women in response to a water-based exercises program and progressive resistance training. Geriatr Gerontol Int 15:1193–1200
Bergamin M, Ermolao A, Tolomio S, Berton L, Sergi G, Zaccaria M (2013) Warer-versus land-based exercise in elderly subjects: effects on physical performance and body composition. Clin Interv Aging 8:1109–1117
Bidonde J et al (2014) Aquatic exercise training for fibromyalgia (review). Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD011336
Bocalini D, Serra A, Murad N, Levy R (2008) Water- versus land-based exercise effects on physical fitness in older women. Geriatr Gerontol Int 8:265–271
Borg E (1982) Psychophysical bases of perceived exertion. Med Sci Sports Exerc 14:377–381
Brass J, Federoff L (2007) Psychological benefits of water aerobics for fibromyalgia patients. Int J Aquat Res Educ 1:255–268
Busch A et al (2011) Exercise therapy for fibromyalgia Curr. Pain Headaches Rep 15:358–367. https://doi.org/10.1007/s11916-011-0214-2
Carruthers B et al (2011) Myalgic encephalomyelitis: international consensus criteria. J Intern Med 270:327–338. https://doi.org/10.1111/j.1365-2796.2011.02428.x
Castro-Sanchez A, Mataran-Penarrocha G, Lara-Palomo I, Saavedra-Hernandez M, Arroyo-Morales M, Moreno-Lorenzo C (2012) Hydrotherapy for the treatment of pain in people with multiple sclerosis: a randomized controlled trial. Evid Based Complement Altern Med. https://doi.org/10.1155/2012/473963
Cella D (1997) Manual of the functional assessment of chronic illness therapy (FACIT) measurement system. Center on outcomes, research and education (CORE). Evanston Northwestern Healthcare and Northwestern University, Evanston
Cook D, Nagelkirk P, Poluri A, Mores J, Natelson B (2006) The influence of aerobic fitness and fibromyalgia on cardiorespiratory and perceptual responses to exercise in patients with chronic fatigue syndrome. Arthritis Rheum 54:3351–3362. https://doi.org/10.1002/art.22124
ESSA (2011) Adult pre-exercise screening tool Version 1. Exercise and Sports Science Australia
Fukuda K, Straus SE, Hickie I, Sharpe MC, Dobbins JG, Komaroff A (1994) The chronic fatigue syndrome: a comprehensive approach to its definition and study. Int Chronic Fatigue Syndr Study Group Ann Intern Med 121:953–959
Gabrielsen A, Videbaek R, Johansen L, Warberg J, Christensen N, Pump B, Norsk P (2000) Forearm vascular and neuroendocrine responses to graded water immersion in humans. Acta Physiol Scanda 169:87–94
Gordon B, Lubitz L (2009) Promising outcomes of an adolescent chronic fatigue syndrome inpatient programme. J Paediatr Child Health 45:286–290
Gordon B, Knapman L, Lubitz L (2010) Graduated exercise training and progressive resistance training in adolescents with chronic fatigue syndrome: a randomized controlled pilot study. Clin Rehabilit 24:1072–1079. https://doi.org/10.1177/0269215510371429
Gusi N, Tomas-Carus P, Hakkinen A, Hakkinen K, Ortega-Alonso A (2006) Exercise in waist-high warm water decreases pain and improves health-related quality of life and strength in the lower extremities in women with fibromyalgia. Arthritis Rheum 55(1):66–73
Hoad A, Spickett G, Elliot J, Newton J (2008) Postural orthostatic tachycardia syndrome is an under-recognized condition in chronic fatigue syndrome. Q J Med 101:961–965
Honda T, Kamioka H (2012) Curative and health enhancement effects of aquatic exercise: evidence based on interventional studies. Open Access J Sports Med 3:27–34
IOM (Institute of Medicine) (2015) Beyond myalgic encephalomyelitis/chronic fatigue syndrome: redefining an illness. The National Academics Press, Washington, DC
Jentoft E, Kvalvik A, Mengshoel A (2001) Effects of pool-based and land-based aerobic exercise on women with fibromyalgia/chronic widespread muscle pain. Arthritis Care Res 45:42–47
Kanitz A et al (2015) Effects of two deep water training programs on cardiorespiratory and muscular strength responses in older adults. Exp Gerontol 64:55–61. https://doi.org/10.1016/j.exger.2015.02.013
Kieffer HS, Lehman M, Veacock D, Korkuch L (2012) The effects of a short-term novel aquatic exercise program on functional strngth and performance of older adults. Int J Exerc Sci 5:321–333
Larun L, Brurberg KG, Odgaard-Jensen J, Price JR (2017) Exercise therapy for chronic fatigue syndrome. Cochrane Database Systematic Rev https://doi.org/10.1002/14651858.CD003200.pub7
Macias-Hernandez S, Vazquez-Torres L, Morones-Alba J, Coronado-Zarco R, Soria-Bastida M, Cruz-Medina E, Nava-Bringas T (2015) Water-based Tai Chi: theoretical benefits in musculoskeletal diseases. Current evidence. J Exerc Rehablit 11:120–124
Mannerkorpi K, Nordeman L, Ericsson A, Arndorw M, GAU study group (2009) Pool exercise for patients with fibromyalgia or chronic widespread pain: a randomized controlled trial and subgroup analyses. J Rehabilt Med 41:751–760
Massy-Westropp NM, Gill TK, Taylor AW, Bohannon RW, Hill CL (2011) Hand grip strength: age and gender stratified normative data in a population-based study. BMC Res Notes 4:127
McManimen S, Jason L (2017) Post-exertional malaise in patients with ME and CFS with comorbid fibromyalgia SLR. Neurol Neurosurg 3:22–27
McNamara R, McKeough Z, McKenzie D, Alison J (2015) Acceptability of the aquatic environment for exercise training by people with chronic obstructive pulmonary disease with physical comorbidities: additional results from a randomised controlled trial. Physiotherapy 101:187–192. https://doi.org/10.1016/j.physio.2014.09.002
Meredith-Jones K, Waters D, Legge M, Jones L (2011) Upright water-based exercise to improve cardiovascular and metabolic health: a qualitative review. Complement Ther Med 19:93–103. https://doi.org/10.1016/j.ctim.2011.02.002
Moss-Morris R, Sharon C, Tobin R, Baldi J (2005) A randomized controlled graded exercise trial for chronic fatigue syndrome: outcomes and mechanisms of change. J Health Psychol 10:245–259. https://doi.org/10.1177/1359105305049774
Plecash A, Leavitt B (2014) Aquatherapy for neurodegenerative disorders. J Huntingdon’s Dis 3:5–11. https://doi.org/10.3233/JHD-140010
Salem Y, Scott A, Karpatkin H, Concert G, Haller L, Kaminsky E, Weisbrot R, Spatz E (2011) Community-based aquatic programme for individuals with multiple sclerosis: a pilot study. Disabil Rehabil 33(9):720–728
Stormorken E, Jason L, Kirkevold M (2017) From good health to illness with postinfectious fatigue syndrome: a qualitative study of adults’ experiences of the illness trajectory. BMC Fam Pract 18:49–64
Taylor R, Kielhofner G (2005) Work-related impairment and employment-focused rehabilitation options for individuals with chronic fatigue syndrome: a review. J Ment Health 14(3):253–267
Torres-Ronda L, del Alcazar X (2014) The properties of water and their application for training. J Hum Kinet 44:237–248
Verhagen A, Cardoso J, Biema-Zeinstra S (2012) Aquatic exercise and balneotherapy in musculoskeletal conditions. Best Pract Res Clin Rheumatol 26:335–343
Wallman K, Morton A, Goodman C, Grove R, Guilfoyle A (2004) Randomised controlled trial of graded exercise in chronic fatigue syndrome. Med J Aust 180:444–448
Webster K, Cella D, Yost K (2003) The functional assessment of chronic illness therapy (FACIT) measurement system: properties, applications, and interpretation. Health Qual Life Outcomes 1:1–7
Wilson B, Spencer H, Kortebeine P (2012) Exercise recommendations in patients with newly diagnosed fibromyalgia. Phys Med Rehabilit 4:252–255. https://doi.org/10.1016/j.pmrj.2011.11.012
Acknowledgements
The authors acknowledge that this study was supported in part by an internal seed grant from Southern Cross University.
Author information
Authors and Affiliations
Contributions
SC and SB conceived and designed the research. All authors conducted data collection. SB analysed the data and created the tables. SC created the figures. All authors developed, read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Additional information
Communicated by Fabio Fischetti.
Rights and permissions
About this article
Cite this article
Broadbent, S., Coetzee, S. & Beavers, R. Effects of a short-term aquatic exercise intervention on symptoms and exercise capacity in individuals with chronic fatigue syndrome/myalgic encephalomyelitis: a pilot study. Eur J Appl Physiol 118, 1801–1810 (2018). https://doi.org/10.1007/s00421-018-3913-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-018-3913-0