Abstract
Purpose
The left ventricle (LV) ejects blood into the proximal aorta. Age and hypertension are associated with stiffening and dilation of the aortic root, typically viewed as indicative of adverse remodeling. Based on analytical considerations, we hypothesized that a larger aortic root should be associated with lower global afterload (effective arterial elastance, EA) and larger stroke volume (SV). Moreover, as antihypertensive drugs differ in their effect on central blood pressure, we examined the role of antihypertensive drugs for the relation between aortic root size and afterload.
Methods
We studied a large group of patients (n = 1250; 61 ± 12 years; 78 % males; 64 % hypertensives) from a single-center registry with known or suspected coronary artery disease. Aortic root size was measured by echocardiography as the diameter of the tubular portion of the ascending aorta. LV outflow tract Doppler was used to record SV.
Results
In the population as a whole, after adjusting for key covariates in separate regression models, aortic root size was an independent determinant of both SV and EA. This association was found to be heterogeneous and stronger in patients taking a calcium channel blocker (CCB; 10.6 % of entire population; aortic root size accounted for 8 % of the explained variance of EA).
Conclusion
Larger aortic root size is an independent determinant of EA and SV. This association was heterogeneous and stronger in patients on CCB therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Arterial afterload is influenced by the physical properties of the aortic root including its size. Both aging and disease states such as hypertension have been shown to be related to increasing aortic root size in cross-sectional (Vasan et al. 1995), longitudinal (Lam et al. 2010) and post-mortem studies (Virmani et al. 1991). This is associated at molecular level by inflammatory activity (Lindeman et al. 2009) and degradation of elastin fibers in the vessel wall with replacement by collagen (Wang and Lakatta 2002). As this causes central arteries to lose elasticity, the concomitantly observed aortic dilation has been attributed to the exhaustion of strain reserve: the repetitive pulsatile hemodynamic stress is no longer accommodated by distensibility (AlGhatrif and Lakatta 2014; O’Rourke and Nichols 2005; Safar et al. 2003). Hemodynamic stress may also contribute to aortic root dilatation. This has been shown in athletes and is reportedly more common not only in high-intensity sports (Pelliccia et al. 2010) but also in children with complete heart block where aortic dilation appears to regress after pacemaker insertion, in parallel with a reduction in stroke volume achieved by the increase in heart rate (Altit et al. 2014). Whether this process is driven purely by altered hemodynamic load, or if aortic wall inflammation plays a role, is unknown (Davey et al. 2011; Hans et al. 2012).
Windkessel models are applied to conceptualize afterload as divided into its constituent components in the frequency domain (Frank 1899). A widely used model is the 3-element windkessel which constitutes an electrical analog to the circulation and incorporates (a) a capacitor with electric charge storage properties to account for the distensibility of elastic arteries, (b) a peripheral resistive element which is the resistance at steady state flow, i.e., the zero harmonic, localized to the distal circulation and (c) characteristic impedance (ZC), a proximal resistive force acting on the high-frequency impedance spectrum. Based on non-windkessel theories, an analytical argument can be made that a larger aortic root should contribute to a lower afterload: first, the Moens-Korteweg equation posits that the diameter of the aorta is positively related to the aortic elastance-wall thickness product (i.e., a measure of aortic stiffness) and inversely related to the square of the local pulse wave velocity. Second, the water hammer equation posits that pulse wave velocity is positively related to ZC. Taken together, these equations connect a larger aortic root size with lower ZC, which should translate into lower afterload and larger stroke volume (SV), especially when preload and/or contractile reserves are limited. However, this view runs contrary to the traditional paradigm that large artery dilation is a feature of adverse remodeling, and there are few reports from the real world to support this notion (Gardin et al. 2006; Lam et al. 2013; Mitchell et al. 2008).
Different classes of antihypertensive drugs exhibit differences in their effect on central blood pressure, an important finding considering the role central pressure appears to play for the clinical course of the patient (Mancia et al. 2014). While the exact physiology of central pressure remains controversial, its determinants are likely to include not only cardiac output and systemic vascular resistance (SVR) but also factors controlled by properties of the proximal aorta including its stiffness, the pulse wave velocity and the magnitude of reflected arterial waves (Izzo 2004; O’Rourke 1990). Whether the size of the aortic root plays a role for the effects of antihypertensive drugs on central hemodynamics is unknown.
We wished to test the hypothesis that a larger aortic root is associated with lower LV afterload and consequently a larger SV. We postulated that the association between aortic root size and LV afterload is influenced by antihypertensive drugs.
Methods
Patients and data sources
Individuals were identified for inclusion into the present retrospective analysis from a registry of patients undergoing coronary arteriography for acute coronary syndrome at National Heart Centre Singapore, using unique personal national identification numbers to link records to echocardiographic data available in the local clinical echocardiography database. Inclusion criteria were (a) registry enrollment between 3 August 2007 and 30 December 2010 and (b) echocardiography having been performed in close conjunction with the angiography (±1 week). Exclusion criteria were (a) having neither Singapore citizenship nor permanent resident status and (b) any valvular heart disease that invalidates subsequent hemodynamic analysis: specifically, regurgitation of either mitral or aortic valve greater than mild in severity or aortic stenosis of any degree. We included only the first study for patients that had undergone multiple angiograms or ultrasound scans. Individual case sheets and electronic health records were reviewed in cases with missing data including clinical characteristics and blood test results. The registry, which contains demographic and clinical information, is managed by Singapore Cardiac Databank and was audited in November 2015 against source documents and found to be 97.5 % accurate. As this was a retrospective study utilizing existing data, the local institutional ethics review board approved the protocol with waiver of informed consent.
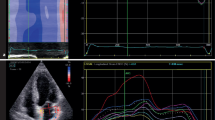
Echocardiograms
Echocardiograms were performed using routine clinical image acquisition (GE Vivid System E5, E7 and Vivid i, Chalfont, United Kingdom; Philips IE33 and CX50, Eindhoven, The Netherlands; Siemens Acuson Sequoia 512 and Aspen, Malvern PA, USA; Toshiba Artida, Otawara, Japan; all transducers 1–5 MHz; lab staffed by 25 sonographers, 10 physicians; Agfa HealthCare IMPAX Cardiovascular Suite, Greenville SC, USA), adhering to applicable guidelines (Lang et al. 2005). The size of the aortic root was recorded at three locations: (a) as the widest diameter at the level of the sinus of Valsalva, (b) at the sinotubular junction and (c) and as the largest diameter of the tubular portion of the ascending aorta as measured from inner edge to inner edge in the parasternal long-axis acoustic window (Fig. 1; Lang et al. 2005). It was decided pre-hoc to use ascending aortic diameter for the purpose of all data analyses in this study and aortic dilation was defined as an indexed diameter ≥2.1 cm/m2 as recommended elsewhere (Evangelista et al. 2010). LV outflow tract diameter was measured 0.5–1.0 cm below the aortic valve in a focused and zoomed-in parasternal long-axis view in mid-systole as the distance between basal septum and anterior mitral valve leaflet, and SV was obtained by multiplying LV outflow tract area (Lang et al. 2005) by the pulsed-wave Dopper velocity–time integral. LV end-diastolic volume (LVEDV) was obtained by dividing SV by LV ejection fraction (LVEF) and LV end-systolic volume (LVESV) was calculated by subsequently subtracting SV from LVEDV, a method validated in a porcine model against 3D echocardiography and post-mortem LV volumes (Hart et al. 2002). Arterial elastance (EA), which was introduced as an estimate of global afterload (Sunagawa et al. 1985) and subsequently validated against impedance measurements in the time domain (Kelly et al. 1992), was obtained by dividing LV end-systolic pressure [LVESP; estimated as 0.9 brachial systolic blood pressure (SBP)] by SV. End-systolic LV elastance (ELV) was used as a pre-load independent measure of LV contractility and calculated by dividing LVESP by LVESV (Sagawa et al. 1977), under the assumptions that end-systolic volume is linearly related to pressure and that V0 is negligible, both of which are reasonable under physiological loading conditions (Burkhoff et al. 2005; Kass and Kelly 1992). Arterial compliance (CA) was calculated by dividing SV by brachial pulse pressure, assuming a linear association between arterial volume and pressure (Chemla et al. 1998). Mean arterial pressure (MAP) was derived from brachial blood pressure as diastolic blood pressure (DBP) +PP/3. SVR was calculated as MAP divided by cardiac output. All chamber size data were indexed to body surface area (BSA) prior to any analyses (Asanoi et al. 1989; Najjar et al. 2004) and are shown in their indexed form throughout the article. Heart rate and brachial artery blood pressure were recorded immediately before echocardiography. The coefficient of variation for measurements of aortic root size, LVEF and SV, analyzed in 50 randomly selected studies as the standard deviation of differences divided by the mean, was 4.3, 7.6 and 8.6 %, respectively.
Statistics
Logarithmic transformation was applied to skewed variables as appropriate. Correlations were analyzed using Pearson’s or Spearman’s correlation coefficients; T tests or Mann–Whitney U tests were applied for un-paired comparisons, as appropriate. We used multiple regression to analyze central hemodynamics as done elsewhere (Sahlén et al. 2012), using multivariable models to analyze predictors of SV, including a priori the principal determinants of SV as covariates: heart rate, LVEDV (preload), EA (afterload) and ELV (contractility). In similar analysis of predictors of EA (i.e., lumped afterload), we included a priori the elements from a 2-element windkessel model of the arterial circulation as covariates (SVR, CA) as well as root size which acted as a proxy for proximal arterial function (i.e., the third element of a 3-element windkessel model). The impact of vasoactive drugs (antihypertensive or statins) (Koh 2000) was investigated by interaction analyses applied to pre-hoc defined subgroups [treatment with calcium channel blockers (CCB), β-adrenergic receptor blockers, diuretics, long-acting nitrates, angiotensin-converting enzyme (ACE) inhibitors and statins] using centered interaction variables while adjusting for arterial blood pressure. Assumptions for linear regression were checked as follows: linearity of relationships between covariates and the dependent variable were analyzed in component residual plots, residuals were inspected for normality, homoskedasticity and the independence of errors was assessed using the Durbin-Watson statistic, multicollinearity was excluded by calculating variance inflation factors, outliers were identified by calculating leverage values and double-checked against original data post hoc to ensure data veracity. Overall regression model predictive accuracy was assessed as adjusted R 2. The relative importance of regressors was estimated by quantifying the variance attributable to each one using an established method for partitioning the R 2 statistic by averaging sequential sums of squares over all orderings of regressors (Chevan and Sutherland 1991; Grömping 2006). Cohen’s d statistic was calculated as an index of effect size, as the difference between subgroup means divided by pooled standard deviation. Statistical significance was considered present for a two-tailed p value of <0.05. All statistics were analyzed using R v. 3.1.2. Data are presented as mean ± standard deviation (SD) or median (inter-quartile range) as appropriate.
Results
Study population
The original dataset comprised n = 1411 patients of whom n = 161 patients were excluded due to valvular heart disease, leading to a final dataset for analyses comprising n = 1250 patients. Basic characteristics are shown in Table 1. In a majority of patients, the indication for coronary angiography was ST-elevation myocardial infarction (n = 711; 57 %; Table 2). Table 3 shows hemodynamic parameters for the entire study population including indices of LV preload (LVEDV), afterload (EA) and contractility (ELV). There were 133 patients on CCB of whom 90.2 % were documented to be hypertensive.
Clinical and pathophysiological correlates of aortic root dilation
Patients with aortic root dilation (n = 1129 %) were older and more commonly hypertensive as shown in Table 1. Among 793 hypertensives, 11.3 % had aortic root dilation (n = 90) vs. 4.6 % (n = 21) of 457 non-hypertensives (Chi2 = 15.2, p < 0.001). As shown in Fig. 2, patients with aortic root dilation had lower EA, larger LVEDV and larger SV than patients with normal aortic root size. They had similar number of diseased vessels on angiography (Table 2) and similar ELV to patients with normal aortic root size (Fig. 2), indicating preserved contractility. Patients with aortic root dilation had higher pulse pressure (56.6 vs. 51.6 mmHg, p < 0.01) but similar CA to patients with normal aortic root size (0.8 vs. 0.8 mmHg mL m−2, p = ns), in keeping with their SV being larger (Fig. 2). Their LVEF was higher (52.4 vs. 49.6 %, p = 0.03). There was a trend to greater use of CCB in patients with aortic root dilation (16 vs. 10 %) which was statistically non-significant (p = 0.07).
Favorable associations between aortic root dilation (x-axes) and both stroke volume and its principal determinants (y-axes). Panels show stroke volume (a), effective arterial elastance (LV afterload; b) end-systolic LV elastance (LV contractility; c) end-diastolic volume (LV preload; d) and heart rate (e). Patients with normal vs. dilated aortic root are shown in blue vs. red (color figure online)
Correlations with SV are shown in Table 4 (Model 1). In multivariable analysis, aortic root size remained a significant predictor (p = 0.002), accounting for 2.4 % of the total explained variance of SV after adjusting for HR, LVEDV, ELV, SVR and CA (Table 4; Model 2). Effect size of aortic dilatation on SV was small–moderate in magnitude (Cohen’s d = 0.39).
Effect of antihypertensive therapy on the association between aortic root size and EA
Determinants of EA in multivariable analysis are shown in Table 5 (Model 3). There were significant interactions between the association between aortic root size and EA and the use of CCBs (p < 0.001) as well as use of β-adrenergic receptor blockers (p = 0.04), but not diuretics (p = 0.10), long-acting nitrates (p = 0.10), ACE-inhibitors (p = 0.41) or statins (p = 0.11).
There was a strong association between aortic root size and EA in patients taking a CCB (n = 133, p < 0.001) in whom increased aortic root size accounted for almost 8 % of the overall explanatory power of the model (total R 2 = 0.86). In contrast, in patients not taking a CCB (n = 1117) the association between aortic root size and EA was statistically non-significant in subgroup analysis (p = 0.44; Table 5; Models 4a, 4b). In contrast, the association with aortic root size was weak in patients on β-adrenergic receptor blockers (0.9 % of overall explanatory power attributable to aortic root size). Further subgroup analysis showed that patients taking vs. not taking a CCB had similar SVR (2.07 ± 0.54 vs. 2.13 ± 0.54 mmHg s m2 mL−1, p = 0.51) and CA (0.69 ± 0.24 vs. 0.76 ± 0.27 mL m−2 mmHg−1, p = 0.07) but larger SV (40.5 vs. 36.9 mL m−2, p = 0.003).
Discussion
The present study aimed to characterize the role of aortic root enlargement for LV afterload and SV. We found that a larger aortic root was associated with lower LV afterload (EA) and preload (LVEDV), similar contractility (ELV) and consequently larger SV. Moreover, we found a significant interaction effect indicating heterogeneity of the association between aortic root size and afterload as patients on CCB therapy exhibited a particularly strong association: 8 % of total explained EA was attributable to aortic root size in this subgroup.
Aortic root size, afterload and stroke volume
A principal end-point of the current analysis was EA, effective arterial elastance, which represents global afterload, i.e., a ‘lumped’ measure of the input impedance that opposes ventricular outflow (Kelly et al. 1992; Sunagawa et al. 1985). Aortic root size was positively associated with higher age but inversely associated with EA. Patients with aortic dilation had similar contractility (ELV) but greater preload (LVEDV) and larger SV. This is in keeping with analytical considerations suggesting that aortic dilation should have a beneficial effect on afterload and SV. As expected, the proportion of afterload attributable to aortic properties was small in numerical terms: the amount of variance explained by the regression model that was attributable to aortic diameter, after adjusting for other determinants of afterload, was 3.6 % (Table 5). This figure is analogous to previously published in vivo determinations of afterload by members of our group where ZC (derived from central flow and non-invasively determined central blood pressure waveforms) accounted for 3.5–5.0 % of total arterial resistance (Johnson et al. 2013; Sahlén et al. 2011). Invasive estimates of the proportion attributable to ZC have been performed mainly in individuals that were healthy or at least free of vascular disease and have been in the range 4–7 % (Kelly et al. 1992; Murgo et al. 1981). Non-invasive measurements have yielded estimates in the range 8–11 % in apparently healthy middle-aged subjects (Segers et al. 2007) and approximately 14–17 % in patients with hypertension and heart failure (Desai et al. 2009).
Mitchell et al. recorded ZC in 167 clinical trial participants with systolic hypertension studied off antihypertensive therapy. Patients with high pulse pressure were found to have higher pulse wave velocity, smaller aortic root diameter, greater aortic wall stiffness and higher ZC, suggesting a mismatch between pulsatile flow and diameter in patients with inappropriately small aortic root (Mitchell et al. 2008). While the population studied by Mitchell et al. was different to that of the present study (mean MAP >40 mmHg higher, 100 % were hypertensive), we are able to confirm and extend their findings by demonstrating that the aortic root diameter is indeed an independent determinant of global LV afterload and forward stroke volume. In contrast to what Mitchell et al. found, we found a small but significant increase in pulse pressure in patients with aortic root dilatation (+5 mmHg) which is likely to be attributable to a larger SV, which in turn is determined by several important differences in central hemodynamics of which the aortic root diameter is in fact one. Future research will need to demonstrate how this differs from the hyperdynamic circulatory state that causes systolic blood pressure elevation mainly in younger hypertensives (Fouad et al. 1978).
Contrary to the view that pulsatile load drives aortic root dilation, longitudinal data from the Framingham Heart Study have shown that individuals that develop aortic root dilation actually have lower baseline pulse pressure and higher diastolic blood pressure (Lam et al. 2010). This suggests aortic remodeling may conceivably be an adaptive response to an age-related increase in pulse pressure and that individuals with blunting of this response may exhibit a smaller aortic root and associated higher LV afterload (Mitchell et al. 2003). A positive association between SV and aortic root size has also been observed in other populations including the Losartan Intervention For Endpoint reduction (LIFE) trial (Bella et al. 2002; Cipolli et al. 2009; Palmieri et al. 2001).
Mechanistically, aortic root dilation occurs either due to hemodynamic stress (Altit et al. 2014) or due to local enzymatic processes in the aortic wall including inflammation and activation of neutrophil-derived proteases (Lindeman et al. 2009). It is conceivable that the role of hemodynamically driven, ‘appropriate’ dilation in elderly individuals may receive insufficient recognition, possibly due to the association between atherosclerotic vessel inflammation and dilation of other arterial segments in the body (Ito et al. 2008). A strength of the present report is, therefore, the fact that the population under study did consist almost exclusively of patients with established coronary artery disease and presumably poor endothelial function with ongoing enzymatic activation of arterial walls. Longitudinal investigations in this field do exist, as based on Framingham Heart Study and Cardiovascular Health Study, but were limited by the fact that they predominantly included community-dwelling individuals. As such, they may not have been able to conclusively demonstrate whether hypertensive subjects with unfavorable aortic root characteristics are at increased risk of heart failure (Gardin et al. 2006; Lam et al. 2013). Future research will need to collect longitudinal data on both characteristic impedance and aortic wall stiffness in an appropriately selected group of patients at risk of heart failure to answer this important question.
Impact of aortic root size on antihypertensive therapy
In a predefined interaction analysis, we noted that the association between aortic root size and afterload was heterogeneous and larger among patients taking CCB therapy, the proportion of explained variance attributable to aortic size in that subgroup being 8 %. Other antihypertensive drugs did not demonstrate an interaction of this magnitude although a directionally similar association was found for β-adrenergic receptor blockers.
Central arterial stiffness is a strong predictor of cardiovascular events (28) and there is growing awareness that antihypertensive drugs differ between classes in their ability to alter central hemodynamics and reduce aortic blood pressure (Cushman et al. 2001; Millar et al. 1999). Previous data have shown that CCB therapy reduces central blood pressure more than diuretics (Matsui et al. 2009) and that the vasodilating β-adrenergic receptor blocker nebivolol produces a greater reduction in central pressure (Dhakam et al. 2008) than the β1-receptor-selective agent atenolol (Mackenzie et al. 2009). The largest published study in this field was the Conduit Artery Functional Evaluation (CAFE) study which compared central blood pressure between patients on a CCB-based vs. a β-adrenergic receptor blocker-based antihypertensive regimen. Patients on CCB therapy were found have a central systolic pressure 12 mmHg lower than brachial pressure vs. a peripheral-to-central difference of only 8 mmHg in β-adrenergic receptor blocker-treated patients (Williams et al. 2006). While the present study did not evaluate the exact physiological basis for an effect of CCB therapy, it is known that the main mechanism for blood pressure reduction with CCB therapy is inhibition of voltage-dependent L-type calcium channels of vascular smooth muscle cells (SMC) (Berkels et al. 2003). Animal experiments specifically examining aortic tissue have shown that depolarization-induced contraction does control both basal and active tension of aortic SMCs via activation of L-type calcium channels (Fransen et al. 2012) which in turn may be inhibited by administering CCBs (Michiels et al. 2014). Murine aortic SMCs have also been demonstrated to be more sensitive to the vasodilator effect of nitric oxide in the presence of the L-type CCB nifedipine (Van Hove et al. 2009). Whether the production of nitric oxide per se is also favorably influenced by CCBs is still unknown, however, as the impact of antihypertensive drugs on endothelial function varies significantly between different vascular territories (Virdis et al. 2011). A putative mechanism to explain the significantly greater role played by aortic root size in patients on CCB therapy may be alterations in aortic root resistive or viscoelastic properties over and above the impact on blood pressure (which we adjusted for in multivariable analysis). However, in contrast to other arterial segments where viscoelasticity has been shown to change with drug administration (Safar et al. 1983; Safar et al. 1987; Vatner et al. 1980), animal experiments evaluating aortic properties have yielded conflicting results with an effect of aortic SMC tone on vessel elasticity being observed in some (Armentano et al. 1995; Barra et al. 1993) but not all reports (Niederhoffer et al. 1997; Van Gorp et al. 1996).
Limitations
This study has several limitations: (a) all patients had acute coronary syndrome, i.e., there was no normal control group; (b) some important but less common cardiac co-morbidities (congenital heart disease, cardiomyopathy) are not available through our data sources which remains a potential source of error; (c) CCBs were treated as a class; while the large majority of patients can be assumed to take non-dihydropyridine CCBs, the exact drugs used as well as duration were unfortunately not available to us. (d) While 90 % of CCB-treated patients were documented to have hypertension, it is conceivable that CCB therapy was prescribed for another indication (coronary spasm, refractory chest pain) in the remainder. (e) While we did find the association between aortic root size and afterload heterogeneous across subgroups taking vs. not taking CCB therapy, we did not record central pressure and flow nor directly analyze aortic wall stiffness. (f) We used a method for estimating ELV that assumes that aortic volume and pressure are linearly related and that V0 is zero. However, this is likely to play a minor role under normal physiological circumstances (Burkhoff et al. 2005; Kass and Kelly 1992) and obtaining true ELV based on invasively determined pressure–volume loop data is unlikely to alter the findings of the study which mainly focused on SV and EA. (g) The data in the present study were acquired in a predominantly Chinese population which may influence the external validity of findings (Virmani et al. 1991). (h) Differences between the multiple echocardiographs and transducers used may represent a source of error in image acquisition and (i) scaling was done to BSA in a ratiometric, non-allometric, fashion.
Conclusions
We used non-invasive hemodynamic analyses to investigate a large group of well-characterized patients. The size of the aortic root was independently associated with SV (positively) and EA (inversely). This suggests that dilation of the aortic root, as seen in elderly individuals and hypertensive patients, may in fact be favorable, possibly by mitigating the adverse impact of concomitant aortic wall stiffening. The association between aortic root size and afterload was heterogeneous, and stronger in patients taking CCBs. Future research will need to elucidate the nature of this association and externally validate findings outside ACS patients.
Abbreviations
- ACE:
-
Angiotensin-converting enzyme
- AR:
-
Aortic regurgitation
- BSA:
-
Body surface area
- CA :
-
Arterial compliance
- CAFÉ:
-
Conduit artery functional evaluation
- CCB:
-
Calcium channel blocker
- EA :
-
Arterial elastance
- ELV :
-
End-systolic LV elastance
- LIFE:
-
Losartan for endpoint reduction trial
- LV:
-
Left ventricle
- LVEDV:
-
Left ventricular end-diastolic volume
- LVEF:
-
Left ventricular ejection fraction
- LVESP:
-
Left ventricular end-systolic pressure
- LVESV:
-
Left ventricular end-systolic volume
- MAP:
-
Mean arterial pressure
- SD:
-
Standard deviation
- SMC:
-
Smooth muscle cell
- SV:
-
Stroke volume
- SVR:
-
Systemic vascular resistance
- ZC :
-
Characteristic impedance
References
AlGhatrif M, Lakatta EG (2014) The reality of aging viewed from the arterial wall. In: Safar ME, O’Rourke MF, Frohlich ED (eds) Blood pressure and arterial wall mechanics in cardiovascular diseases. Springer-Verlag, London, p 146
Altit G, Sarquella-Brugada G, Dahdah N et al (2014) Effect of dual-chamber pacemaker implantation on aortic dilatation in patients with congenital heart block. Am J Cardiol 114:1573–1577
Armentano RL, Barra JG, Levenson J, Simon A, Pichel RH (1995) Arterial wall mechanics in conscious dogs. Assessment of viscous, inertial, and elastic moduli to characterize aortic wall behavior. Circ Res 76:468–478
Asanoi H, Sasayama S, Kameyama T (1989) Ventriculoarterial coupling in normal and failing heart in humans. Circ Res 65:483–493
Barra JG, Armentano RL, Levenson J, Fischer EI, Pichel RH, Simon A (1993) Assessment of smooth muscle contribution to descending thoracic aortic elastic mechanics in conscious dogs. Circ Res 73:1040–1050
Bella JN, Wachtell K, Boman K et al (2002) Relation of left ventricular geometry and function to aortic root dilatation in patients with systemic hypertension and left ventricular hypertrophy (the LIFE study). Am J Cardiol 89:337–341
Berkels R, Taubert D, Rosenkranz A, Rosen R (2003) Vascular protective effects of dihydropyridine calcium antagonists. Involvement of endothelial nitric oxide. Pharmacology 69:171–176
Burkhoff D, Mirsky I, Suga H (2005) Assessment of systolic and diastolic ventricular properties via pressure-volume analysis: a guide for clinical, translational, and basic researchers. Am J Physiol Heart Circ Physiol 289:H501–H512
Chemla D, Hebert JL, Coirault C et al (1998) Total arterial compliance estimated by stroke volume-to-aortic pulse pressure ratio in humans. Am J Physiol 274:H500–H505
Chevan A, Sutherland M (1991) Hierarchical partitioning. Am Stat 45:90–96
Cipolli JA, Souza FA, Ferreira-Sae MC et al (2009) Sex-specific hemodynamic and non-hemodynamic determinants of aortic root size in hypertensive subjects with left ventricular hypertrophy. Hypertens Res 32:956–961
Cushman WC, Materson BJ, Williams DW, Reda DJ (2001) Pulse pressure changes with six classes of antihypertensive agents in a randomized, controlled trial. Hypertension 38:953–957
Davey DL, Bratton SL, Bradley DJ, Yetman AT (2011) Relation of maternal anti-Ro/La antibodies to aortic dilation in patients with congenital complete heart block. Am J Cardiol 108:561–564
Desai AS, Mitchell GF, Fang JC, Creager MA (2009) Central aortic stiffness is increased in patients with heart failure and preserved ejection fraction. J Card Fail 15:658–664
Dhakam Z, Yasmin McEniery CM, Burton T, Brown MJ, Wilkinson IB (2008) A comparison of atenolol and nebivolol in isolated systolic hypertension. J Hypertens 26:351–356
Evangelista A, Flachskampf FA, Erbel R et al (2010) Echocardiography in aortic diseases: EAE recommendations for clinical practice. Eur J Echocardiogr 11:645–658
Fouad FM, Tarazi RC, Dustan HP, Bravo EL (1978) Hemodynamics of essential hypertension in young subjects. Am Heart J 96:646–654
Frank O (1899) Die Grundform des arteriellen Pulses. Erste Abhandlung, mathematische Analyse. Z Biol 37:483–526
Fransen P, Van Hove CE, van Langen J et al (2012) Contribution of transient and sustained calcium influx, and sensitization to depolarization-induced contractions of the intact mouse aorta. BMC Physiol 12:9
Gardin JM, Arnold AM, Polak J, Jackson S, Smith V, Gottdiener J (2006) Usefulness of aortic root dimension in persons > or = 65 years of age in predicting heart failure, stroke, cardiovascular mortality, all-cause mortality and acute myocardial infarction (from the Cardiovascular Health Study). Am J Cardiol 97:270–275
Grömping U (2006) Relative Importance for Linear Regression in R. J Stat Software 17:1–27
Hans CP, Koenig SN, Huang N et al (2012) Inhibition of Notch1 signaling reduces abdominal aortic aneurysm in mice by attenuating macrophage-mediated inflammation. Arterioscler Thromb Vasc Biol 32:3012–3023
Hart JP, Cabreriza SE, Gallup CG, Hsu D, Spotnitz HM (2002) Validation of left ventricular end-diastolic volume from stroke volume and ejection fraction. ASAIO J 48:654–657
Ito S, Akutsu K, Tamori Y et al (2008) Differences in atherosclerotic profiles between patients with thoracic and abdominal aortic aneurysms. Am J Cardiol 101:696–699
Izzo JL Jr (2004) Arterial stiffness and the systolic hypertension syndrome. Curr Opin Cardiol 19:341–352
Johnson J, Hakansson F, Shahgaldi K, Manouras A, Norman M, Sahlén A (2013) Impact of tachycardia and sympathetic stimulation by cold pressor test on cardiac diastology and arterial function in elderly females. Am J Physiol Heart Circ Physiol 304:H1002–H1009
Kass DA, Kelly RP (1992) Ventriculo-arterial coupling: concepts, assumptions, and applications. Ann Biomed Eng 20:41–62
Kelly RP, Ting CT, Yang TM et al (1992) Effective arterial elastance as index of arterial vascular load in humans. Circulation 86:513–521
Koh KK (2000) Effects of statins on vascular wall: vasomotor function, inflammation, and plaque stability. Cardiovasc Res 47:648–657
Lam CS, Xanthakis V, Sullivan LM et al (2010) Aortic root remodeling over the adult life course: longitudinal data from the Framingham Heart Study. Circulation 122:884–890
Lam CS, Gona P, Larson MG et al (2013) Aortic root remodeling and risk of heart failure in the Framingham Heart study. JACC Heart Fail 1:79–83
Lang RM, Bierig M, Devereux RB et al (2005) Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 18:1440–1463
Lindeman JH, Abdul-Hussien H, van Bockel JH, Wolterbeek R, Kleemann R (2009) Clinical trial of doxycycline for matrix metalloproteinase-9 inhibition in patients with an abdominal aneurysm: doxycycline selectively depletes aortic wall neutrophils and cytotoxic T cells. Circulation 119:2209–2216
Mackenzie IS, McEniery CM, Dhakam Z, Brown MJ, Cockcroft JR, Wilkinson IB (2009) Comparison of the effects of antihypertensive agents on central blood pressure and arterial stiffness in isolated systolic hypertension. Hypertension 54:409–413
Mancia G, Fagard R, Narkiewicz K et al (2014) 2013 ESH/ESC Practice Guidelines for the Management of Arterial Hypertension. Blood Press 23:3–16
Matsui Y, Eguchi K, O’Rourke MF et al (2009) Differential effects between a calcium channel blocker and a diuretic when used in combination with angiotensin II receptor blocker on central aortic pressure in hypertensive patients. Hypertension 54:716–723
Michiels CF, Van Hove CE, Martinet W, De Meyer GR, Fransen P (2014) L-type Ca2 + channel blockers inhibit the window contraction of mouse aorta segments with high affinity. Eur J Pharmacol 738:170–178
Millar JA, Lever AF, Burke V (1999) Pulse pressure as a risk factor for cardiovascular events in the MRC Mild Hypertension Trial. J Hypertens 17:1065–1072
Mitchell GF, Lacourciere Y, Ouellet JP et al (2003) Determinants of elevated pulse pressure in middle-aged and older subjects with uncomplicated systolic hypertension: the role of proximal aortic diameter and the aortic pressure-flow relationship. Circulation 108:1592–1598
Mitchell GF, Conlin PR, Dunlap ME et al (2008) Aortic diameter, wall stiffness, and wave reflection in systolic hypertension. Hypertension 51:105–111
Murgo JP, Westerhof N, Giolma JP, Altobelli SA (1981) Effects of exercise on aortic input impedance and pressure wave forms in normal humans. Circ Res 48:334–343
Najjar SS, Schulman SP, Gerstenblith G et al (2004) Age and gender affect ventricular-vascular coupling during aerobic exercise. J Am Coll Cardiol 44:611–617
Niederhoffer N, Marque V, Lartaud-Idjouadiene I, Duvivier C, Peslin R, Atkinson J (1997) Vasodilators, aortic elasticity, and ventricular end-systolic stress in nonanesthetized unrestrained rats. Hypertension 30:1169–1174
O’Rourke M (1990) Arterial stiffness, systolic blood pressure, and logical treatment of arterial hypertension. Hypertension 15:339–347
O’Rourke MF, Nichols WW (2005) Aortic diameter, aortic stiffness, and wave reflection increase with age and isolated systolic hypertension. Hypertension 45:652–658
Palmieri V, Bella JN, Arnett DK et al (2001) Aortic root dilatation at sinuses of valsalva and aortic regurgitation in hypertensive and normotensive subjects: the Hypertension Genetic Epidemiology Network Study. Hypertension 37:1229–1235
Pelliccia A, Di Paolo FM, De Blasiis E et al (2010) Prevalence and clinical significance of aortic root dilation in highly trained competitive athletes. Circulation 122:698–706
Safar ME, Bouthier JA, Levenson JA, Simon AC (1983) Peripheral large arteries and the response to antihypertensive treatment. Hypertension 5:Iii63–Iii68
Safar ME, Toto-Moukouo JJ, Bouthier JA et al (1987) Arterial dynamics, cardiac hypertrophy, and antihypertensive treatment. Circulation 75:I156–I1161
Safar ME, Levy BI, Struijker-Boudier H (2003) Current perspectives on arterial stiffness and pulse pressure in hypertension and cardiovascular diseases. Circulation 107:2864–2869
Sagawa K, Suga H, Shoukas AA, Bakalar KM (1977) End-systolic pressure/volume ratio: a new index of ventricular contractility. Am J Cardiol 40:748–753
Sahlén A, Abdula G, Norman M et al (2011) Arterial vasodilatory and ventricular diastolic reserves determine the stroke volume response to exercise in elderly female hypertensive patients. Am J Physiol Heart Circ Physiol 301:H2433–H2441
Sahlén A, Shahgaldi K, Aagaard P, Manouras A, Winter R, Braunschweig F (2012) Altered ventriculo-arterial coupling during exercise in athletes releasing biomarkers after endurance running. Eur J Appl Physiol 112:4069–4079
Segers P, Rietzschel ER, De Buyzere ML et al (2007) Noninvasive (input) impedance, pulse wave velocity, and wave reflection in healthy middle-aged men and women. Hypertension 49:1248–1255
Sunagawa K, Maughan WL, Sagawa K (1985) Optimal arterial resistance for the maximal stroke work studied in isolated canine left ventricle. Circ Res 56:586–595
Van Gorp A, Van Ingen Schenau DS, Willigers J et al (1996) A technique to assess aortic distensibility and compliance in anesthetized and awake rats. Am J Physiol 270:H780–H786
Van Hove CE, Van der Donckt C, Herman AG, Bult H, Fransen P (2009) Vasodilator efficacy of nitric oxide depends on mechanisms of intracellular calcium mobilization in mouse aortic smooth muscle cells. Br J Pharmacol 158:920–930
Vasan RS, Larson MG, Levy D (1995) Determinants of echocardiographic aortic root size. The Framingham Heart Study. Circulation 91:734–740
Vatner SF, Pagani M, Manders WT, Pasipoularides AD (1980) Alpha adrenergic vasoconstriction and nitroglycerin vasodilation of large coronary arteries in the conscious dog. J Clin Invest 65:5–14
Virdis A, Ghiadoni L, Taddei S (2011) Effects of antihypertensive treatment on endothelial function. Curr Hypertens Rep 13:276–281
Virmani R, Avolio AP, Mergner WJ et al (1991) Effect of aging on aortic morphology in populations with high and low prevalence of hypertension and atherosclerosis. Comparison between occidental and Chinese communities. Am J Pathol 139:1119–1129
Wang M, Lakatta EG (2002) Altered regulation of matrix metalloproteinase-2 in aortic remodeling during aging. Hypertension 39:865–873
Williams B, Lacy PS, Thom SM et al (2006) Differential impact of blood pressure-lowering drugs on central aortic pressure and clinical outcomes: principal results of the Conduit Artery Function Evaluation (CAFE) study. Circulation 113:1213–1225
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Additional information
Communicated by Keith Phillip George.
Rights and permissions
About this article
Cite this article
Sahlén, A., Hamid, N., Amanullah, M.R. et al. Impact of aortic root size on left ventricular afterload and stroke volume. Eur J Appl Physiol 116, 1355–1365 (2016). https://doi.org/10.1007/s00421-016-3392-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-016-3392-0