Abstract
Purpose
Human centrifugation, also called artificial gravity (AG), is proposed as a combined strategy against detrimental effects of microgravity in long-term space missions. This study scrutinized human short-arm centrifugation as countermeasure against musculoskeletal de-conditioning.
Method
Eleven healthy male subjects [mean age of 34 (SD 7) years] completed the cross-over trial, including three campaigns of −6° head-down tilt bed rest (HDT) for 5 days, with preceding baseline data collection and recovery phases. Bed rest without AG was used as control condition (Ctrl), and AG with 1 g at the center of mass applied once per day for 30 min in one bout (AG1×30) and in 6 bouts of 5 min (AG6×5, 3-min rest between bouts) as experimental conditions. End-points were muscle strength, vertical jump performance, and biomarkers of bone and protein metabolism.
Result
AG6×5 was better tolerated than AG1×30. Bone resorption markers CTX, NTX, and DPD all increased by approximately 25 % toward the end of bed rest (P < 0.001), and nitrogen balance decreased by approximately 3 g/day (P < 0.001), without any protection by AG (P > 0.4). Decreases in vertical jump height by 2.1 (SE 0.6) cm after Ctrl bed rest was prevented by either of the AG protocols (P = 0.039).
Conclusion
The present study yielded succinct catabolic effects upon muscle and bone metabolism that were un-prevented by AG. The preservation of vertical jump performance by AG in this study is likely caused by central nervous rather than by peripheral musculoskeletal effects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Physical de-conditioning is a well-known consequence of spaceflight and its ground-based analog of experimental bed rest (Pavy-Le Traon et al. 2007). This comprises a large variety of changes, of which muscle atrophy (Narici et al. 2003), bone loss (Vico et al. 2000), loss of aerobic (Capelli et al. 2006) and anaerobic (Ferretti et al. 2001; Rittweger et al. 2007) fitness, as well as orthostatic intolerance (Blaber et al. 2011) have been regarded as the greatest challenges for astronaut well-being and performance. Very recently, visual impairments, possibly related to changes in intra-cranial pressure, have been defined as another serious side effect of spaceflight (Mader et al. 2011).
The International Space Station (ISS) is dedicated to establish the capability of human long-term space missions. Promoting countermeasure development to safeguard crew health is one of its main goals. Fortunately, the past decade has seen substantial progress in countermeasure development during bed rest. For example, resistive exercise has been shown to combat muscle atrophy and bone loss in bed rest (Shackelford et al. 2004), and superposition of vibration seems to augment these benefits (Rittweger et al. 2010; Belavy et al. 2011). Regular aerobic exercise can maintain aerobic power and even maintain orthostatic tolerance in bed rest when combined with blood volume expansion (Shibata et al. 2010). It is promising that bone anti-resorptive treatment with alendronate has now proven to be effective in space (Leblanc et al. 2013), and it is hoped that the new advanced Resistive Exercise Device (aRED), a custom-made gravity-independent exercise device that has been built for the station, will result in improved muscular performance and bone status (Smith et al. 2012). However, independent of however successful these and future countermeasure developments may be, each of them addresses physiological systems in a piece-meal fashion, and they are very time-consuming on a practical level. Integrating multiple countermeasures into the crew time line during spaceflight is a genuine challenge. Moreover, there is currently no countermeasure for the visual impairment problem.
One would therefore wish for a combined countermeasure approach to combat all the known, and even yet unknown, negative health effects of microgravity. A simple idea therefore is to replace gravitational forces by centrifugal forces, hence the term artificial gravity (AG) (Bukley et al. 2007). The main rationale is that, physically speaking, molecules, cells, and even organs are unlikely to discern between the different forms of linear acceleration. It is obvious, though, that the centrifugal acceleration scales with ω 2 × r, where ω is angular velocity and r is the radius of the centrifuge. Thus, artificial gravity, in particular with short-arm centrifugation, induces different levels of acceleration along the body’s axis and thus differs from gravitational acceleration. The size-limitation in crewed spacecrafts enforces a short-arm (human centrifuge) with a radius below 2 m and with high rotation rate in order to generate centrifugal forces of required magnitude. Accordingly, the resulting Coriolis forces and cross-coupled angular velocities during head or body movements may induce disorientation, motion sickness, and other detrimental effects. Therefore, both the efficacy and the feasibility of short-term centrifugation (SAHC) protocols need to be investigated.
Based upon these principles, there had been an initiative to form an international multidisciplinary artificial gravity (IMAG) research project that would systematically investigate the feasible operational parameter space (radius, angular velocity, duty cycle, supplemental exercise, etc.) at multiple locations using HDT bed rest as a de-conditioning stimulus and standardized dependent measures to allow comparison of results between study centers. Unfortunately, the project was canceled after a single pilot study (Young and Paloski 2007). In summary, the pilot study, which treated subjects during 21 days of HDT de-conditioning with 1 h daily exposures to centrifugation (1g at the level of the heart, 2.5g at the feet), found moderate protection of muscle strength (Caiozzo et al. 2009) and cardiovascular function (Stenger et al. 2012), but no protection from increased markers of bone resorption (Smith et al. 2009).
The European Space Agency (ESA) has subsequently promoted the idea of investigating AG by installing two identical SAHCs in bed rest centers (Toulouse and Cologne). Two 5-day head-down tilt bed rest studies were planned in parallel. These studies were designed to further advance the experiences from IMAG, and the present study, named bed rest and artificial gravity 1 (BRAG1), aims at understanding whether partitioning AG into shorter intervals could be more effective than an un-interrupted bout of AG.
The 5-day bed rest format is based upon the rationale that biomarkers of bone and protein metabolism respond to unloading by bed rest within a few days, provided that there is a strict metabolic control of the bed rest study (Baecker et al. 2003). It therefore seems very straightforward to monitor these early responses as a necessary prerequisite for countermeasure effectiveness, and to thus use the 5-day bed rest format to screen different countermeasures in a much faster and efficient way than could be done using long-term bed rest only. Thus, we hypothesized that AG would counteract the elevation of bone resorption markers, the decay of protein catabolism, and the decline in neuromuscular functioning induced by 5 days of bed rest.
Method
Study design and setting
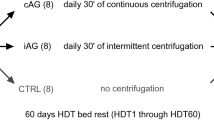
The definition of the AG protocol for the present study departed from the notion that a countermeasure that could be efficient with as little as 30 min of crew time per day should be appealing enough in order to consider implementation in future space vehicles. Fractioning physiological stimuli into a sequence of bouts is often able to enhance the effectiveness of the stimulus (Herbert et al. 1988), and Vernikos et al. (1996) had shown that standing or walking for 2 h per day, fractioned into eight daily bouts of 15 min during a 4-day bed rest, significantly reduced orthostatic intolerance when standing immediately after bed rest. Thus, to combine these rationales, the present study examined the effect of fractioning the centrifugation stimulus, and to compare the application of AG once daily for 30 min (AG1×30) and six times daily for 5 min each (AG6×5).
The study was designed as a controlled cross-over trial, i.e., each subject performed one campaign of bed without AG and two campaigns in which bed rest was combined with one of the two AG protocols, i.e., AG1×30 or AG6×5. In order to exclude effects of the sequence of conditions, permutations of the condition sequences were generated, and subjects were randomly assigned to one condition sequence.
The study was performed between March and July of 2010 at the French Space clinic (MEDES) on the premises of the University hospital Rangueil in Toulouse, France. The study was organized in three campaigns, each of which consisted of 5 days for baseline data collection (BDC-5 to BDC-1), 5 days of head-down tilt bed rest (HDT1 to HDT5), and 5 days of recovery (R + 0 to R + 4). The washout period between campaigns was 32 days.
All subjects who participated in this study were recruited from the local community by internet, newspaper, and advertisements. Twelve healthy males were included in the study after receiving a complete description of the experimental methods and after passing the medical and psychological screening criteria. Medical tests for selection included: medical history, clinical examination and psychological interview, chest-X-ray, electrocardiogram, ultrasound imaging of lower limb veins, a 10-min stand test, peak oxygen uptake measurement, bone densitometry and body composition by dual X-ray absorptiometry, and laboratory tests (hematology, blood chemistry, and urine drug screening analysis). In addition, the subjects had to pass a centrifuge tolerance test (AG6×5 protocol) in order to be eligible. Criteria for termination of these centrifuge runs are given below (subsection ‘application of short-arm centrifugation’). The study was approved by the local Ethics Committee (Comité de Protection des Personnes Sud-Ouest et Outre-Mer I). All volunteers signed a consent form and were aware of their right to withdraw from the experiment without prejudice at any time.
One subject (subject E) developed appendicitis during the second campaign, which was unrelated to the study. It was subsequently decided to withdraw that subject from the study, and all his data were excluded from the present analysis. The anthropometric data of the remaining eleven subjects are given in Table 1.
Head-down tilt bed rest
Six-degree head-down tilt bed rest was performed in conformity with ESA’s bed rest standardization plan (ESA 2009). Subjects followed a day–night cycle of 7 a.m. wake-up and lights-out at 11 p.m. During the HDT period, strict bed rest was followed, and all activities were conducted in the head-down tilt position (hygiene, toilet, eating, reading, etc.). Showering was performed in a dedicated head-down tilt shower-bed. As centrifugation was performed in horizontal position, subjects during Ctrl bed rest (i.e., campaigns without AG) were put to horizontal bed rest for 40 min per day, which was the anticipated duration of the average centrifugation protocol for AG1×30 and AG6×5. Transfer to the centrifuge was accomplished with a specific gurney, so that the subjects remained at −6° during the transport, and they rolled over from the gurney to the centrifuge nacelle without usage of their leg muscles. Subjects were allowed to change position in HDT position, but not to get up, sit, or stand at any time. During the HDT period, subjects were monitored by video in addition to close surveillance by MEDES staff to ensure compliance with the protocol. During the ambulatory and rehabilitation periods, the volunteers were not authorized to leave the research facility, except for specific testing sessions in the hospital next door. In that case, they were always accompanied by one member of the MEDES paramedical staff. During their free time, subjects were allowed leisure activities such as reading, games, or computer activities. Daytime sleeping or napping was not allowed.
As a major prerequisite for studying changes in bone and muscle metabolism by markers in blood and urine, the diet was controlled during the entire study and consisted of five different daily menus with three meals and two snacks. During the ambulatory periods (BDC and R), caloric intake was equal to 140 % resting metabolic rate, plus an additional allowance of +10 % to cover effects of thermogenesis (154 % total). During the HDT period, caloric intake was set to 110 % resting metabolic rate +10 % for thermogenesis (121 % total). Daily protein intake was set to 1.2 g per kg body mass, and fat was set to less than or equal 30 % of total caloric intake, and carbohydrates were set between 50 and 60 %. All of the food portions were individually weighed, and the subjects were required to eat all food items served to them. In case they did not, the dinner intake was augmented to balance the lunch leftovers. Smoking, alcohol, or caffeinated drinks were not allowed during the study.
Application of short-arm centrifugation
The SAHC used in this study provides nacelles for subjects to be supine with their feet directed outwards (see Fig. 1). A dummy was placed on an opposing arm for counterbalance. For each subject, the center of mass was calculated using a ratio of center of mass to height of 0.56 (Clauser et al. 1969). The nacelle was positioned, so that the calculated center of mass was located between 118 and 122 cm from the center of rotation. This small variation was inevitable due to variation in subjects’ height, which ranged from 167 to 190 cm and due to mechanical constraints. Accordingly, the rotation rates also ranged from 27.8 to 27.2 rpm, respectively, so that all subjects were exposed to 1 g at their estimated center of mass. During centrifugation, subjects were in complete darkness with their head placed on a headrest. They were instructed to stay calm, to not move the head, and to not contract their leg muscles. They could however crimp their toes every 10–20 s to prevent calf pain.
A centrifuge run was as follows: the centrifuge accelerated at 5° s−2 for 32–33 s until the target rotation rate was achieved. Rotation at constant velocity then lasted either 30 min for the AG1×30 protocol or 5 min for the AG6×5 protocol. The centrifuge then decelerated at 5° s−2 until a complete stop. For AG6×5, a 3-min rest period was used between two successive runs. The direction of centrifuge rotation (clockwise or counterclockwise) varied each day.
Medical monitoring included continuous heart rate, blood pressure, and respiration rate. Subjects wore headsets to communicate with the medical operator. The termination criteria were syncope, severe signs of orthostatic intolerance (self-reported sweating, dizziness, fainting), fast and persistent decrease in systolic blood pressure (>25 mmHg), abrupt changes in heat rate (>15 min−1), tachycardia (>150 min−1), irregular cardiac rhythm, or the subject’s request to stop.
Neuromuscular testing
Vertical jump tests were performed (outside the SAHC) as a measure of whole-body anaerobic power as described before (Rittweger et al. 2007). Briefly, subjects performed a countermovement jump on a Leonardo force plate with integrated software system in its version 4.2 (Novotec Medical, Pforzheim, Germany). This software system provides a user interface for standardized testing procedures. Three jumps were performed, and subjects were asked to ‘jump as high as possible with the head while keeping their hands posed on the hips. Jump tests were scheduled on days BDC-1, on R + 0 as the first thing after reambulation, and on day R + 4. All tests were performed and all data were collected as scheduled, except that subject K completed the jump test on day R + 1 instead day R + 0 during the AG1×30 campaign because of technical problems.
Isometric muscle strength was assessed on days BDC-4 and R + 1 with a Con-Trex MultiJoint System (CMV AG, Dübendorf, Switzerland) to assess the isometric maximal voluntary contraction (MVC) of six muscle groups. To ensure that torque was measured at, or as near as possible to, the optimum joint angle, MVCs were recorded at different joint angles for each muscle group: the knee extensors and flexors were tested at 90°, 80°, and 70°, the plantarflexors and foot dorsiflexors were measured at −20°, −10°, 0°, +10°, +20°, and +30°, and the elbow extensors and flexors were assessed at 30°, 60°, 90°, and 120°. For knee and elbow, full extension was set as 0°, and for the ankle 0° was defined as the angle when standing. At each joint angle, the subject was asked to perform a maximum extension followed 30 s after by a maximum flexion, and 30 s after by another pair of extension and flexion contractions until three complete sets of extension/flexion contractions have been recorded. In case the subject was still improving at the third contraction, successive contractions were recorded until no further improvement from the previous one was observed. Each contraction had to be maintained for 5–7 s. A 2-min rest was given between the successive set of three contractions at the next joint angle.
Biological samples
Blood samples were drawn from an antecubital vein in the morning at 7:00 after overnight fasting on days BDC-1, HDT5, and R + 4, and plasma was stored at −80 or −20 °C until enzyme-linked immuno assays (ELISA) were performed for bone-specific alkaline phosphatase (bAP, Tandem R. Ostase, Hybritech, Liége, Belgium) and n-terminal type1 pro-collagen (P1NP, Orion Diagnostica, Finland) were assessed by ELISA.
Urine was collected over 24-h periods, during which they were stored at 4 °C. From these collections, 10 mL samples were aliquoted and stored at −20 °C. From these aliquots, the C-Telopeptide (CTX) and N-Telopeptide (NTX) of the collagen cross-link were analyzed as markers of bone resorption by commercially available kits (NTX: Osteomark, TECOmedical, Bünde, Germany; CTX: Urine crosslaps, IDS, Frankfurt, Germany), and deoxypyridinoline (DPD) was analyzed by HPLC. Moreover, urinary N2 was analyzed by chemo-luminescence (Antek7000, Antek Instruments, U.S.) by an accredited laboratory (Central Biochemical Laboratory, Université de Lyon, Lyon, France). Protein intake was assessed using the nutrition software Nutrilog (Nutrilog SAS, Marans, France).
Data processing
Countermovement jumps were analyzed with the integrated Leonardo software in its version 4.2. The algorithm follows the principle outlined by Davies and Rennie before (Davies and Rennie 1968) and computes jump height and power by numerical integration of ground reaction force data. Accordingly, jump height (H Peak, in cm), peak power specific to body mass (P Peak, in W/kg), peak acceleration (A Peak, which is equivalent with peak force normalized for mass, in multiples of g), and countermovement depth (D CM, given in cm with negative values denoting downward movement from starting position) were identified as the variables h_max_E_pot, P_tot_max_rel, F_max_tot_rel, and h_min_E_Pot, respectively, in the database generated by the Leonardo software.
Isometric muscle strength tests were analyzed with the integrated Con-Trex software (Con-Trex human kinetics 1.7.4). For each muscle groups and tested angles, the isometric MVC torque was recorded and the highest value was chosen as the true MVC.
Protein intake was assessed by entering all ingredients for each recipe into the Nutrilog Edition Expert software, in its version 2.0 (Marans, France). All food and leftovers were weighed individually. Nitrogen balance was then calculated as the difference between nitrogen intake and the excretion in urine.
Statistical analyses
Statistical analyses were carried out using the R-environment in its version 2.13.1 for the 64-bit Windows platform (http://www.r-project.org). Data are given as best linear unbiased predictors (BLUP) and standard errors (SE) in the text, as means and SD in the Tables, and as means and their standard errors in the figures. The level for statistical significance was set to α = 0.05.
For muscle strength testing and for vertical jump testing, only the trials with greatest torque and with greatest jump height, respectively, were selected for statistical analyses. Where several data points were available from baseline data collection, they were lumped together to yield one single BDC value. Linear mixed effect (LME) models with time and intervention as fixed effects and subject ID as random effect were constructed in order to assess intervention effects. Variances were allowed to differ between participants and intervention, and LME models were optimized according to Akaike’s information criterion [see p. 353 and p. 652 in (Crawley 2007)]. Data were box-cox transformed where demanded by non-linear quantile–quantile plots or in case of heteroscedacity. Initially, all HDT days, as well as the recovery days, were tested against the lumped BDC days. Models were then further simplified in a step-wise manner when no significant intervention effects were found. Firstly, data representing HDT days were lumped together and so were data from all recovery days to yield the HDT phase and the REC phase (see Table 2 for the exact strategy for the lumping of days). When there were still no significant effects, AG1×30 and AG6×5 interventions were pooled to yield Ctrl vs. AG comparisons. The last step of model simplification was to delete any intervention effects from the model, so that pure-phase effects were analyzed as the simplest model.
Results
Centrifuge tolerance
All the 30 centrifuge sessions of the AG6×5 protocol were performed nominally by 10 out of the 11 subjects. On the second day of bed rest with centrifugation, one subject experienced nausea after his first 5-min centrifuge run, and consequently, the following 5 runs on that day were canceled. This subject no longer experienced nausea during the 5-min centrifuge runs on the subsequent days of this bed rest campaign.
The AG1×30 protocol was less well tolerated. Only 6 out of 11 subjects performed the full protocol nominally, and in 5 subjects, there was at least one of the 5 centrifuge runs interrupted because of a malaise. In total, there were 10 instances when a medical event occurred during centrifugation. One subject had a severe vasovagal syncope on his second centrifuge run during his third bed rest campaign. After recovery, this subject then continued the bed rest without centrifugation, but did not perform the tilt test at the end. Another subject (the same as the one described in the AG6×5 protocol above) experienced nausea and a drop in blood pressure during all 5 centrifugation runs of his third campaign, which prompted an interruption of the runs. These events occurred after more than 5 min of rotation and they occurred later and later each day. Yet, another subject experienced dizziness and sweating during two centrifuge runs on his first bed rest campaign. The centrifuge runs of the first session of the first bed rest campaign were also interrupted in two other subjects for the same reason.
Bone formation
Serum levels of bAP were increased on day HDT5 by +1.62 (SE 0.23) µg/L and by +0.95 (SE 0.23) µg/L on day R + 4 (P < 0.001 in both cases). By contrast, a decrease in serum levels of P1NP by 3.11 (SE 1.22) µg/L (P = 0.013) was found for day R + 4. No main effect of AG was found, nor was there a time × AG interaction (P > 0.3) for either bAP or P1NP.
Bone resorption
Urinary CTX excretion (see Fig. 2) was elevated during HDT by +618 (SE 58) µg/day and during Rec by +343 (SE 58) µg/day (both P < 0.001. NTX excretion was likewise increased during HDT by +149 (SE 13) mmol bone collagen equivalent (mmol BCE) per day, and during Rec by +58 (SE 11) mmol BCE/day (both P < 0.001). While there was no time × AG interaction for CTX excretion (P > 0.26), NTX depicted a trend (P = 0.093) to suggest an increase by AG of 45.0 (SE 33.3) mmol BCE/day. Urinary excretion of DPD depicted clear increases by +7.77 (SE 1.97) µg/day during HDT and by +1.01 (SE 1.97) µg/day during Rec (both P < 0.001). In addition, there was a significant HDT × AG1×30 interaction (P = 0.014) that indicated a sparing of the bed-rest-induced resorption by 6.89 (SE 2.80) µg/day. However, this significant effect disappeared when both AG conditions were lumped together (P = 0.062).
Bone resorption, identified here as 24-hour urinary excretion of the c-terminal cross-link (CTX), was increased over levels during baseline data collection (BDC) both during head-down tilt (HDT) bed rest (P < 0.001) and during four days of recovery (R + 1 to R + 3, P < 0.001) after the bed rest. This elevation CTX was comparable between the bed rest-only condition (Ctrl) and the two different artificial gravity (AG) regimens. This suggests that artificial gravity as applied in this study is no efficient countermeasure against bed-rest-induced bone loss. Triple asterisk denotes significant change from BDC (P < 0.001)
Nitrogen balance
Protein intake, which amounted to an average of 92.8 (SE 2.32) g/day, was inappreciably reduced by −0.26 (SE 0.03) g/day on day HDT2 (P = 0.033), but it was unaffected by AG (P = 0.84) or time × AG (P > 0.11). Urinary nitrogen excretion increased by +1.15, +3.16, and +2.33 (SE 0.58) g/day on days HDT2, HDT4, and HDT5, respectively (all P < 0.001), and by +1.37 (SE 0.58) g/day on R + 1 (P = 0.018). No main effect of AG was observed, but a HDT × AG6×5 interaction effect reversal of HDT-induced increases by −2.44 (SE 0.82) g/day. Moreover, trends for such reversing interaction effects were also found for HDT4 × AG1×30 (P = 0.061) and HDT5 × AG1×30 (P = 0.084). Nitrogen balance, i.e., the difference between intake and excretion of nitrogen, responded to HDT in a very similar way as nitrogen excretion (see Fig. 3): clear decreases by −1.19, −3.66, −2.81, and −1.40 (SE 0.58) g/day were observed on days HDT2, HDT4, and HDT5, respectively (P values between <0.001 and 0.042), suggesting that bed rest induced loss of protein mass. These effects were counteracted by AG, as shown by a HDT4 × AG6×5 interaction effect by +2.89 (SE 0.83) g/day (P < 0.001), and by trends for positive effects for HDT4 × AG1×30 (P = 0.061) by +1.56 (SE 0.83) g/day and for HDT5 × AG1×30 (P = 0.084) by +1.43 (SE 0.83) g/day.
Nitrogen Balance, computed as the difference between dietary intake and urinary excretion of nitrogen per 24 h, became reduced during days 2 (P = 0.042) and on days 4 and 5 (both P < 0.001) of head-down tilt (HDT) bed rest (all indicated as asterisks in the figure). This reduction was comparable between the control and intervention conditions, with the exception of day HDT4, where nitrogen balance was more positive for the AG6×5 condition (P < 0.001, indicated as +++ in the figure). This probably suggests that artificial gravity as applied in this study is not a fully effective countermeasure against bed-rest-induced muscle loss
Muscle strength
Muscle strength data, as well as P values for main effects of angle and time, and the time × AG interaction are listed in Table 3. There were no significant 3-way interactions time × AG × angle in any of the six different contraction types (P > 0.7 in all cases). The 2-way AG × angle interactions were all non-significant (P = 0.06 for plantar extension and P > 0.4 in all other cases). Likewise, 2-way time × angle interactions were all non-significant (P = 0.11 for knee extension and P > 0.4 in all other cases). Main effects for angle were found for all contraction types, except for elbow extension, and main effects for time were found for both contraction types of the arm, but for none in the leg (for P values, see Table 3).
Time × AG interactions, which relate to countermeasure effectiveness, were non-significant for arm contractions as well as for plantar extension, but they were significant for all other leg contractions (see Table 3). Contrast testing of these significant time × AG interactions indicated an increase in knee extensor strength by AG6×5 on day R + 1 by +18.0 (SE 8.6) Nm (P = 0.024). For knee flexion, both AG1×30 and AG6×5 enhanced muscle strength on day R + 1 by 25.6 (SE8.6) Nm and by 27.5 (SE 8.6) Nm, respectively (P = 0.013 and P = 0.0016, respectively). For plantar flexor strength, significant effects were observed for AG6×5 by −14.1 (SE 5.2) Nm (P = 0.013) and also for R + 1 × AG6×5 (P = 0.022) indicating an enhancement by +9.6 (SE 4.1) Nm on day R + 1.
Vertical jump performance
H Peak depicted significant effects of time (P < 0.001) and for time × AG interaction (P = 0.0066). Contrast testing revealed a clear decrease by −2.1 (SE 0.6) cm on day R + 0 (P < 0.001), and a weakly significant increase by +1.2 (SE 0.6) cm on day R + 4 (P = 0.046, see Table 4). This HDT-related reduction in jump height was mitigated by AG, as suggested by the R + 0 × AG interaction effect of +1.2 (SE 0.7) cm (P = 0.039). Similarly, a significant time effect was found for P Peak (P = 0.026) with a decrease by −1.55 (SE 0.47) W/kg on day R + 0 (P = 0.0012). Moreover, a significant time × AG effect (P = 0.035) and contrast testing demonstrate countermeasure effectiveness for P Peak by +1.23 (SE 0.58) W/kg (P = 0.034). A Peak likewise yielded significant time effects (P < 0.001), with decreases by −0.0589 (SE 0.0151) g on day R + 0 (P < 0.001) and by −0.031 (SE 0.015) g on day R + 4 (P = 0.039). However, there was no time × AG interaction (P = 0.26). Finally, there were significant effects of time (P < 0.001) and for the time × AG interaction (P = 0.0010) for DCM. Contrast testing suggested that DCM was decreased by −1.66 (SE 0.82) cm on day R + 0 (P = 0.045), but increased by +3.05 (SE 0.82) cm on day R + 4 (P < 0.001). These time effects were opposed by time × AG interactions that suggested effects of +2.89 (SE 1.17) cm for R + 0 × AG6×5 (P = 0.014), and of −3.22 (SE 1.17) cm for R + 4 × AG1×30 (P = 0.0062).
Discussion
The present study has examined the efficacy of 30 min of short-arm centrifugation per day with regards to the countermeasure efficacy for the musculoskeletal system. As a first of a series of planned studies, it focused upon mere ‘stance,’ without any additional exercise on the centrifuge, and it addressed the question of whether fractionation into 5-min bouts would yield better results.
Tolerance of centrifugation protocols
During centrifugation that generates 1g at the center of mass, the centrifugal force exerted at the legs is larger (up to 1.8g at the feet) than the 1g gravitational force experienced during standing in Earth. By the same token, the gravitational force is lower, by comparison, at the head, and thus the vestibular organ. Experience from this and past studies shows that longer duration of such centrifugation generates more fatigue in the legs and side effects due to the fluid shift in the direction of the centrifugal force. Centrifugation was interrupted in ten instances during the AG1×30 protocol, compared to only on such interruption during the AG6×5 protocol. Also, all of the interruptions in the AG1×30 protocol occurred after more than 5 min of centrifugation, later and later each day. This indicates that 5 min seems to constitute a reasonable exposure time for the g-gradient used here. Of note, there seemed to be a habituation effect with the repetition of the sessions. Such habituation of the physiological responses as well as the participant’s well-being to rotating environment has been described in several earlier studies (Guedry et al. 1964; Clement et al. 2001), and it could thus be that longer exposure times will be possible with prolonged centrifugation experience. On the other hand, all eight subjects of the IMAG study (see introduction) tolerated a slightly larger AG challenge for 1 h per day almost without any complication. This could potentially be explained by a more stringent screening, or by the allowance of moderate heel raises and shallow squats in the IMAG study.
Efficacy of AG protocols
Neither the clear-cut increases in the bone resorption markers CTX and NTX, nor the reduction of nitrogen balance in response to bed rest could be prevented by either of the AG protocols, although the significant sparing effect for DPD by AG1×30 on day HDT4 may suggest partial efficacy. There were some indications for a sparing in the bone resorption marker DPD. However, it has to be considered that DPD, which is a type-I collagen-linking compound, is also found in cartilage, and thus less specific for bone turnover than the collagen cross-links, and coefficients of variation from our lab are usually better for CTX and NTX than for DPD. Therefore, the present data are indicative of limited or poor countermeasure efficacy of this particular AG protocol for muscle and bone metabolism, and thus in concert with results from the IMAG study. Similarly, mere standing, with or without superimposed whole-body vibration, seems to be ineffective in a 1-g environment (Zange et al. 2008; Baecker et al. 2010). It therefore seems that some kind of exercise, perhaps as moderate as level walking (Vernikos et al. 1996), must be combined with the gravitational stimulus in order to achieve efficacy for muscle and bone. Of note, the AG level applied in this study was 1 g at the center of mass, meaning that ‘stance’ on the centrifuge will have required muscle forces that should be comparable to stance with terrestrial 1-g level. Therefore, it could also be a rationale to increase the g-level or daily exposure times in future AG application studies, or also to reduce the acceleration gradient.
As to the other outcome measures, they yielded mostly weak or even counter-intuitive results. Thus, bAP was mildly increased toward the end of bed rest, but the more direct marker of bone formation, P1NP, was decreased at the same time. It is generally the case that bone formation responses to bed rest are quite small and variable, and the important finding is that neither of the two AG protocols had a bearing on bone formation markers in this study. The study failed to provide any clear decrease in leg muscle strength (see Table 3, column ‘Time’). Such significant time effects, however, have been observed for the arm contractions, even though the effect was very small for elbow extension. Muscle strength testing is associated with sizeable practicing effects (Connelly et al. 2000), and it is thus very possible that such practice effects with repeated testing after 9 days in this study have blunted bed-rest-induced decreases in leg muscular strength. With this in mind, it seems well possible that the positive time × AG6×5 interaction for plantar flexion strength observed in this study is a meaningful reflection of countermeasure efficacy. In the IMAG study, by comparison, there was a very clear beneficial effect of AG against muscle atrophy, and plantar flexor muscle strength was even enhanced after 21 days of bed rest with AG countermeasure (Caiozzo et al. 2009). Thus, it seems very likely that a longer immobilization phase than 5 days is required in order to study countermeasure efficacy with regards to muscle size and strength.
Very clear and beneficial effects, however, were found in the present study for both AG protocols in relation to vertical jump performance. A succinct decline in peak acceleration, peak power, and jump height in the countermovement jump was paralleled by a decrease in countermovement depth in response to the bed rest only condition. Both AG prescriptions used in this study (AG1×30 and AG6×5) neutralized the bed-rest-induced effects upon peak power, jump height, and countermovement depth. The uniform response to bed rest in nitrogen balance across intervention conditions, as well as the short duration of the bed rest period of 5 days only, suggests that the decrement in jump performance, as well as AG’s countermeasure effect, is not mediated via muscle mass and strength. Of note, vertical jump performance is an ecological test of the human body to negotiate gravity, and it is as such strongly related to performance in tasks such as walking, chair-rising, and stair climbing (Runge et al. 2004). Thus, vertical jump performances is not a ‘pure’ muscle test, and it only loosely related to muscle strength after prolonged bed rest (Rittweger et al. 2007). Accordingly, jump height and peak power are reduced even when exercise during bed rest is effectively maintaining muscle strength (Buehring et al. 2011). It is useful at this point to also appreciate the mechanical complexity of vertical jumps, which requires dynamic balancing of a multi-fold inverted pendulum, as well as translation of rotational limb kinematics into vertical acceleration (Bobbert and van Soest 2001). Greater countermovement depth implies greater usage of hip and thigh muscles and less usage of the calf muscles (Vanrenterghem et al. 2004; Salles et al. 2011). Accordingly, increased countermovement depth will require more ‘confidence,’ and also more complex temporal coordination of task execution than the simple ankle strategy. It is therefore intriguing to argue that the preservation of jump performance by AG was mainly through central nervous, rather than via peripheral muscular effects. Daily ‘imprinting’ of gravitational information into the sensorimotor system offers a plausible rationale for such an explanation. This view is supported by the observations that the decline in jump performance outsizes the decline of isometric muscle strength and muscle size in long-term bed rest (Rittweger et al. 2007; Buehring et al. 2011), which may even imply that AG has a specific ability to ‘imprint’ gravitational information to the central nervous system.
Limitations
The main limitation of the present study consists in its short duration of only 5 days of head-down tilt bed rest. However, previous studies had yielded very clear responses of bone resorption markers and nitrogen metabolism after few days of bed rest, and there is thus a solid rationale for the choice of the 5-day bed rest format. The somewhat only elusive effects of bed rest upon muscle strength and upon bone formation markers are probably owed to the short bed rest duration. Also, it is possible that the washout period should be prolonged in future 5-day bed rest studies. The dynamics of recovery of the musculoskeletal system are probably more complicated than one would normally expect. Bone loss tends to continue for approximately 15 days after bed rest of 35–90 days duration (Rittweger et al. 2005, 2009, 2010), and the exact nature of these post-reambulation bone losses is currently unclear. On the other hand, the present study has yielded impressive results in the field of bone resorption, nitrogen metabolism, and jump performance. Of note, bed rest studies are equally challenging to budgets, researchers, and study participants, and shorter study durations will naturally relax some constraints. As such, short-term studies can identify initial responses to bed rest, and this provides very useful evidence on potential countermeasures. Moreover, short-term studies are unique in that they can help, in combination with mid-term and long-term studies, to identify the time course, and thus the hierarchy of bed-rest-induced de-conditioning for such measurements that cannot be taken continuously during the bed rest, but only before and after it. The discussion of nitrogen metabolism, muscle atrophy, and neuromuscular performance may serve as an example to this: the intriguing constellation of reduced jumping performance by bed rest, in the absence of any decline in knee extensor strength demonstrates the importance of central nervous de-conditioning, and this constellation of results would probably not have been picked by a longer bed rest format.
Conclusion
It seems unlikely that short daily exposures to short-arm centrifugation with 1g at the center of mass will have substantial sparing effects upon bed-rest-induced alterations in muscle and bone metabolism. There were, however, salient benefits upon vertical jump performance, and probably also upon calf muscle strength. These beneficial effects could be associated to central nervous mechanisms, and the question arises in how far those would be effective in mid-term and long-term studies. There was no apparent benefit of the non-fractioned 30-min AG exposure, but subjects could tolerate AG better when it was fractioned into 6 bouts of 5 min each. Future AG prescriptions should attempt to increase musculoskeletal forces either by including some kind of exercise, or by increasing the level of g-exposure.
Abbreviations
- AG:
-
Artificial gravity
- AG1×30 :
-
AG partitioned to 1 × 30 min
- AG6×5 :
-
AG partitioned to 6 times 5 min
- A Peak :
-
Peak acceleration during concentric phase of vertical jump
- aRED:
-
Advanced resistive exercise device
- bAP:
-
Bone-specific alkaline phosphatase
- BDC:
-
Baseline data collection
- CTX:
-
C-telopeptide of the collagen cross-link
- Ctrl:
-
Control
- DCM :
-
Countermovement depth during vertical jump test
- DPD:
-
Deoxypyridinoline
- ELISA:
-
Enzyme -linked immuno-sorbent assay
- HDT:
-
Head-down tilt
- LME:
-
Linear mixed effect
- ESA:
-
European space agency
- H Peak :
-
Peak jump height
- HPLC:
-
High-performance liquid chromatography
- MVC:
-
Maximal voluntary contraction
- NTX:
-
N-telopeptide of the collagen cross-link
- P1NP:
-
n-terminal type-1 pro-collagen
- P Peak :
-
Peak power during concentric phase of vertical jump
- SD:
-
Standard deviation
- SE:
-
Standard error
- R:
-
Recovery
References
Baecker M, Tomic A, Mika C, Gotzmann A, Platen P, Gerzer R, Heer M (2003) Bone resorption is induced on the second day of bed rest: results of a controlled crossover trial. J Appl Physiol 95:977
Baecker N, Frings-Meuthen P, Smith SM, Heer M (2010) Short-term high dietary calcium intake during bedrest has no effect on markers of bone turnover in healthy men. Nutrition 26(5):522–527. doi:10.1016/j.nut.2009.06.006
Belavy DL, Beller G, Armbrecht G, Perschel FH, Fitzner R, Bock O, Borst H, Degner C, Gast U, Felsenberg D (2011) Evidence for an additional effect of whole-body vibration above resistive exercise alone in preventing bone loss during prolonged bed rest. Osteoporos Int 22(5):1581–1591. doi:10.1007/s00198-010-1371-6
Blaber AP, Goswami N, Bondar RL, Kassam MS (2011) Impairment of cerebral blood flow regulation in astronauts with orthostatic intolerance after flight. Stroke 42(7):1844–1850. doi:10.1161/STROKEAHA.110.610576
Bobbert MF, van Soest AJ (2001) Why do people jump the way they do? Exerc Sport Sci Rev 29(3):95–102
Buehring B, Belavy DL, Michaelis I, Gast U, Felsenberg D, Rittweger J (2011) Changes in lower extremity muscle function after 56 days of bed rest. J Appl Physiol 111(1):87–94. doi:10.1152/japplphysiol.01294.2010
Bukley A, Paloski W, Clément G (2007) Physics of artificial gravity. In: Clement G, Bukley A (eds) Artificial gravity. Springer, Berlin, pp 33–58
Caiozzo VJ, Haddad F, Lee S, Baker M, Paloski W, Baldwin KM (2009) Artificial gravity as a countermeasure to microgravity: a pilot study examining the effects on knee extensor and plantar flexor muscle groups. J Appl Physiol 107(1):39–46. doi:10.1152/japplphysiol.91130.2008
Capelli C, Antonutto G, Kenfack MA, Cautero M, Lador F, Moia C, Tam E, Ferretti G (2006) Factors determining the time course of VO2(max) decay during bedrest: implications for VO2(max) limitation. Eur J Appl Physiol 98(2):152–160. doi:10.1007/s00421-006-0252-3
Clauser C, McConville J, Young J (1969) Weight, volume, and center of mass of segments of the human body. vol AMRL-TR-69–70. Aerospace Medical Research Laboratory, Aerospace Medical Division, Airforce Systems Command
Clement G, Deguine O, Parant M, Costes-Salon MC, Vasseur-Clausen P, Pavy-LeTraon A (2001) Effects of cosmonaut vestibular training on vestibular function prior to spaceflight. Eur J Appl Physiol 85(6):539–545
Connelly DM, Carnahan H, Vandervoort AA (2000) Motor skill learning of concentric and eccentric isokinetic movements in older adults. Exp Aging Res 26(3):209–228. doi:10.1080/036107300404868
Crawley MJ (2007) The R book. Wiley, Chichester
Davies CTM, Rennie R (1968) Human power output. Nature 217:770
ESA (2009) Standardization of bed rest study conditions (version 1.5); ESTEC contract number 20187/06/NL/VJ
Ferretti G, Berg HE, Minetti AE, Moia C, Rampichini S, Narici MV (2001) Maximal instantaneous muscular power after prolonged bed rest in humans. J Appl Physiol 90(2):431
Guedry FE Jr, Kennedy RS, Harris CS, Graybiel A (1964) Human performance during two weeks in a room rotating at three rpm. Aerosp Med 35:1071–1082
Herbert ME, Roy RR, Edgerton VR (1988) Influence of one-week hindlimb suspension and intermittent high load exercise on rat muscles. Exp Neurol 102(2):190–198
Leblanc A, Matsumoto T, Jones J, Shapiro J, Lang T, Shackelford L, Smith SM, Evans H, Spector E, Ploutz-Snyder R, Sibonga J, Keyak J, Nakamura T, Kohri K, Ohshima H (2013) Bisphosphonates as a supplement to exercise to protect bone during long-duration spaceflight. Osteoporos Int. doi:10.1007/s00198-012-2243-z
Mader TH, Gibson CR, Pass AF, Kramer LA, Lee AG, Fogarty J, Tarver WJ, Dervay JP, Hamilton DR, Sargsyan A, Phillips JL, Tran D, Lipsky W, Choi J, Stern C, Kuyumjian R, Polk JD (2011) Optic disc edema, globe flattening, choroidal folds, and hyperopic shifts observed in astronauts after long-duration space flight. Ophthalmology 118(10):2058–2069. doi:10.1016/j.ophtha.2011.06.021
Narici M, Kayser B, Barattini P, Cerretelli P (2003) Effects of 17-day spaceflight on electrically evoked torque and cross-sectional area of the human triceps surae. Eur J Appl Physiol 90(3–4):275–282
Pavy-Le Traon A, Heer M, Narici MV, Rittweger J, Vernikos J (2007) From space to Earth: advances in human physiology from 20 years of bed rest studies (1986-2006). Eur J Appl Physiol 101(2):143–194
Rittweger J, Frost HM, Schiessl H, Ohshima H, Alkner B, Tesch P, Felsenberg D (2005) Muscle atrophy and bone loss after 90 days of bed rest and the effects of flywheel resistive exercise and pamidronate: results from the LTBR study. Bone 36(6):1019–1029
Rittweger J, Felsenberg D, Maganaris CN, Ferretti JL (2007) Vertical jump performance after 90 days bed rest with and without flywheel resistive exercise, including a 180 days follow-up. Eur J Appl Physiol 100(4):427–436
Rittweger J, Simunic B, Bilancio G, Gaspare De Santo N, Cirillo M, Biolo G, Pisot R, Eiken O, Mekjavic IB, Narici M (2009) Bone loss in the lower leg during 35 days of bed rest is predominantly from the cortical compartment. Bone 44(4):612–618
Rittweger J, Beller G, Armbrecht G, Mulder E, Buehring B, Gast U, Dimeo F, Schubert H, de Haan A, Stegeman DF, Schiessl H, Felsenberg D (2010) Prevention of bone loss during 56 days of strict bed rest by side-alternating resistive vibration exercise. Bone PMID 19732856(46):137–147
Runge M, Rittweger J, Russo CR, Schiessl H, Felsenberg D (2004) Is muscle power output a key factor in the age-related decline in physical performance? A comparison of muscle cross section, chair-rising test and jumping power. Clin Physiol Funct Imaging 24:335–340
Salles AS, Baltzopoulos V, Rittweger J (2011) Differential effects of countermovement magnitude and volitional effort on vertical jumping. Eur J Appl Physiol 111(3):441–448. doi:10.1007/s00421-010-1665-6
Shackelford LC, LeBlanc AD, Driscoll TB, Evans HJ, Rianon NJ, Smith SM, Spector E, Feeback DL, Lai D (2004) Resistance exercise as a countermeasure to disuse-induced bone loss. J Appl Physiol 97(1):119–129
Shibata S, Perhonen M, Levine BD (2010) Supine cycling plus volume loading prevent cardiovascular deconditioning during bed rest. J Appl Physiol 108(5):1177–1186. doi:10.1152/japplphysiol.01408.2009
Smith SM, Zwart SR, Heer MA, Baecker N, Evans HJ, Feiveson AH, Shackelford LC, Leblanc AD (2009) Effects of artificial gravity during bed rest on bone metabolism in humans. J Appl Physiol 107(1):47–53. doi:10.1152/japplphysiol.91134.2008
Smith SM, Heer MA, Shackelford LC, Sibonga JD, Ploutz-Snyder L, Zwart SR (2012) Benefits for bone from resistance exercise and nutrition in long-duration spaceflight: evidence from biochemistry and densitometry. J Bone Miner Res 27(9):1896–1906. doi:10.1002/jbmr.1647
Stenger MB, Evans JM, Knapp CF, Lee SM, Phillips TR, Perez SA, Moore AD Jr, Paloski WH, Platts SH (2012) Artificial gravity training reduces bed rest-induced cardiovascular deconditioning. Eur J Appl Physiol 112(2):605–616. doi:10.1007/s00421-011-2005-1
Vanrenterghem J, Lees A, Lenoir M, Aerts P, De Clercq D (2004) Performing the vertical jump: movement adaptations for submaximal jumping. Hum Mov Sci 22(6):713
Vernikos J, Ludwig DA, Ertl AC, Wade CE, Keil L, O’Hara D (1996) Effect of standing or walking on physiological changes induced by head down bed rest: implications for spaceflight. Aviat Space Environ Med 67(11):1069–1079
Vico L, Collet P, Guignandon A, Lafage-Proust MH, Thomas T, Rehaillia M, Alexandre C (2000) Effects of long-term microgravity exposure on cancellous and cortical weight-bearing bones of cosmonauts. Lancet 355(9215):1607–1611
Young LR, Paloski WH (2007) Short radius intermittent centrifugation as a countermeasure to bed-rest and 0-G deconditioning: IMAG pilot study summary and recommendations for research. J Gravit Physiol 14(1):P31–P33
Zange J, Mester J, Heer M, Kluge G, Liphardt AM (2008) 20-Hz whole body vibration training fails to counteract the decrease in leg muscle volume caused by 14 days of 6 degrees head down tilt bed rest. Eur J Appl Physiol 105(2):271–277
Acknowledgments
This study was funded by ESA contract no. 22 127/08 and by a CNES framework agreement no. 70686. J Rittweger and J Zange were supported by internal funding from the German Aerospace Center (DLR) within the project ‘Artificial Gravity’. In addition, J. Rittweger used private funds to participate in the study in its planning phase (2006–2009). We are grateful to the staff of MEDES for their excellent work and support of this study. Special thanks go to Dr. Petra Frings-Meuthen and Gaby Kraus from the DLR Institute of Aerospace Medicine for the assessment of serum and urine markers of bone metabolism. Last but not least, we are deeply indebted to the study participants—without their selfless contribution, this work would not have been possible.
Conflict of interest
The authors have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Guido Ferretti.
Rights and permissions
About this article
Cite this article
Rittweger, J., Bareille, MP., Clément, G. et al. Short-arm centrifugation as a partially effective musculoskeletal countermeasure during 5-day head-down tilt bed rest—results from the BRAG1 study. Eur J Appl Physiol 115, 1233–1244 (2015). https://doi.org/10.1007/s00421-015-3120-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-015-3120-1