Abstract
Objective
The aim of this study was to investigate the prevalence, risk factors, and prevention of occupational contact dermatitis (OCD), as well as risk factors and consequences of OCD among professional cleaners.
Methods
A systematic review following PRISMA guidelines was performed using Medline, EMBASE, and Cochrane Library.
Results
Thirty-nine studies containing over 109.000 participants were included in the review. The prevalence of OCD varied between 2.2% and 30.1%. Main occupational risk factors for developing OCD among cleaners included wet work and irritants in cleaning products (bleach, chlorine, ammonia, multi-use-cleaning) and skin contact to metal. The most common contact allergies included rubber, biocides, nickel/cobalt, and perfumes. Other risk factors were inconsistent use of protective gloves and low educational level. Consequences associated with OCD included significant impairment in quality of life, tendency to have unscheduled absence from work, sick leave, increased rate of disability, and recognized degree of injury. Only one prevention study has been published investigating the effect of an educative course in skin-protective behavior in cleaners. The study reported a higher degree of knowledge of skin protection, a decrease in the severity of hand eczema, and a shift toward fewer daily hand washings at follow-up after 3 months.
Conclusion
Our study proves that OCD is common in cleaners, and the main risk factors included wet work, irritants, and contact allergies, as well as inconsistent use of protective gloves and low educational level. More focus and a greater number of studies are needed on skin protection in this population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
For many years, occupational skin disease (OSD) has been the most frequently recognized work-related disease in many Western countries (Diepgen 2003). In Denmark, a total of 16,688 cases of suspected occupational diseases were reported in 2020, of these 13.5% (n = 2261) were suspected OSD (Arbejdsmarkedets erhverssikring 2020). Fifty-nine percent of the suspected OSD were later acknowledged as work related in 2020 (Arbejdsmarkedets erhverssikring 2020). Hand eczema (HE), also referred to as occupational contact dermatitis (OCD), constitutes 80–95% of all OSD (Halkier-Sorensen 1996). The lifetime prevalence has been estimated at 4.8% in the general working population in Norway, i.e., 1 in 20 working person may expect to develop OCD in the course of their working life. For health-care workers in Denmark and Hong Kong the figure is 21% and 22%, respectively (Vindenes et al. 2017; Ibler et al. 2012b; Luk et al. 2011). OCD most commonly affects the hands, starts at a young age, and often takes a chronic course (Carøe et al. 2010; Meding et al. 2005). The impairments caused by OCD include sick leave, loss of job, and early retirement. OCD is also known to be a significant financial burden to society (Carøe et al. 2010; Meding et al. 2005).
A number of risk factors for development of OCD have been identified. Wet work is a well-known risk factor (Carøe et al. 2010; Hamnerius et al. 2018; Nichol et al. 2019) and is defined as having wet hands for ≥ 2 h per working day, hand washing ≥ 20 times per working day, or wearing occlusive gloves for ≥ 2 h working day (Lund et al. 2020; Diepgen et al. 2015). The risk of OCD is, however, not negligible for those performing wet work < 2 h per day on average (Lund et al. 2020).
Professional cleaners are highly exposed to wet work and potential irritants and allergens. Thus, OCD has a high prevalence among workers in the cleaning industry (Gawkrodger et al. 1986; Hansen 1983), with a prevalence reported between 6 and 28% (Vindenes et al. 2017; Gawkrodger et al. 1986; Hansen 1983; Lammintausta 1983; Singgih et al. 1986; Nielsen 1996; Mirabelli et al. 2012). Prevention programs have therefore been suggested. However, there are no standards for prevention of OCD among cleaners and only limited data are available for this population. Primary prevention has shown to have a positive effect in the prevention of OCD among other professions such as health-care workers, hairdressers, and dairy industry workers (Held et al. 2001, 2002; Loeffler et al. 2006; Dulon et al. 2009; Schwanitz et al. 2003; Dickel et al. 2002). With respect to secondary prevention, several studies have reported positive effects of educational interventions in other occupations (Skudlik et al. 2012; Wilke et al. 2012; Ibler et al. , 2012a). The aim of this review was therefore to investigate the prevalence, risk factors, and contact allergy and prevention of CD or OCD in professional cleaners.
Method
For this study, we followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (MOCDr D et al. 2009). The medical databases included Pubmed, EmBase, and Cochrane Library. Literature was searched from November through December 2021 by using the following search terms: “hand dermatoses” OR “occupational dermatitis” OR “occupational eczema” OR “eczema” OR “hand eczema” OR “hand dermatose” OR “hand dermatitis” OR “contact dermatitis” AND “cleaner*” OR “hospital worker” OR “worker” AND “incidence OR “prevalence” OR “prevention”.
Inclusion and exclusion criteria
Only English language papers qualified for inclusion. Randomized clinical trials, original articles, posters, and case reports were included if they contained sufficient original data. Studies had to investigate the prevalence, risk factors, or prevention of CD or OCD among professional cleaners. If this could not be clarified based on the abstract, studies were full-text screened. There were no restrictions regarding country of origin, publication date, sex, or age. The reference lists of the included studies and review manuscripts were also searched for additional papers. In terms of studies investigating cleaning staff together with other professional workers (not providing specific information about cleaners), these were included, if they contained relevant and useful information based on the previous inclusion criteria. Studies were excluded if they did not report any outcomes related to dermatological aspects of occupational diseases.
Data extraction and quality assessment
The first step of this review was selection based on titles and abstracts of the retrieved articles. The second step was removal of duplicates and analysis of the abstracts for further selection. Finally, the selected papers were retrieved in full text and independently reviewed by two of the authors (FBS and TEM). The relevant literature was selected and presented in this review according to the inclusion criteria. The following data were extracted and presented in tables: author name and the date of publication, study setting country, study design, data on setting and participants, age, gender and number of participants, and outcome variables (Online Resource 1).
Definitions
Based on the definitions above, skin symptoms were defined as CD or OCD in the included studies. However, many of the studies did not distinguish between the two and just referred to the disease as CD. In the current review, we distinguish between the two.
Results
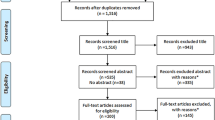
A total of 7844 articles were identified (Pubmed, n = 3704, EmBase n = 4116 and Cochrane Library n = 24). Of these, 1812 were unique papers and 61 were included for full-text assessment. Of these, 22 were excluded for reasons listed in the PRISMA flow diagram (not English, n = 10, no access, n = 4 and irrelevant to dermatology, n = 8) (Fig. 1). A total of 39 articles were included for this review (Online Resource 1). The included original articles were 14 questionnaire-based (Gawkrodger et al. 1986; Nielsen 1996; Mirabelli et al. 2012; Gupta et al. 2018; Lee et al. 2014; Stingeni et al. 1995; Lynde et al. 2009; Aydin Taş et al. 2021; Skoet et al. 2004; Falay Gür et al. 2022; Weisshaar et al. 2007; Garrido et al. 2021; Meding et al. 2016; Dietz et al. 2022), 5 retrospective (Santarossa et al. 2020; Brans et al. 2019; Nettis et al. 2002; Uter et al. 2010; Geier et al. 2003), 2 randomized (Held et al. 2002; Halkier-Sørensen and Thestrup-Pedersen 1993), 1 prospective one-group pre–post design and questionnaire (Clemmensen et al. 2015), 3 interview-based (Soder et al. 2007; Lammintausta et al. 1982; Lodi et al. 2000), 9 register-based (Carøe et al. 2010; Lammintausta 1983; Bensefa-Colas et al. 2014; Magnano et al. 2009; Feveile et al. 2009; Schwensen et al. 2013; Dietz et al. 2021; Liskowsky et al. 2011; Rui et al. 2012), 1 cross-sectional and retrospective (Melo et al. 2000), 1 questionnaire- and interview-based (Douwes et al. 2017), 1 observational based (Jungbauer et al. 2004), and 1 population-based study (Dietz et al. 2007) and 1 poster (Special Issue: 13th Congress of the European Society of Contact Dermatitis (ESCD), 14–17 September 2016 [Available from: ESCD Abstracts: Posters—2016—Contact Dermatitis-Wiley Online Library] 2016).
The prevalence, severity, and classification of CD
The prevalence of CD among cleaners was reported by five studies, and varied from 8.5% to 15.9% in two questionnaire-based studies (Gupta et al. 2018; Falay Gür et al. 2022), to 10.3% in a single retrospective study (Nettis et al. 2002), 11% in a single prospective one-group pre–post and questionnaire-based study (Clemmensen et al. 2015), and 14.8% in a single questionnaire and interview-based study (Douwes et al. 2017).
The prevalence of OCD among cleaners was reported by 11 studies. The prevalence varied from 2.2% to 20% in register-based studies (Carøe et al. 2010; Lammintausta et al. 1982; Schwensen et al. 2013; Dietz et al. 2021), 8.1–21.6% in questionnaire-based studies (Gawkrodger et al. 1986; Stingeni et al. 1995; Aydin Taş et al. 2021; Skoet et al. 2004), 30.1% in a single interviews-based study (Lodi et al. 2000), and 9.2–14.1% in retrospective studies (Santarossa et al. 2020; Nettis et al. 2002). OCD was reported most commonly in females (Aydin Taş et al. 2021; Skoet et al. 2004; Schwensen et al. 2013; Dietz et al. 2021; Dietz et al. 2007). However, the majority of the study population in most of these studies was female (Aydin Taş et al. 2021; Skoet et al. 2004; Schwensen et al. 2013; Dietz et al. 2021; Dietz et al. 2007).
A single study including 549 professional cleaners and 593 building workers (BW) reported a significantly higher incidence of “rash on the hands” among male and female cleaning workers compared to building workers (Lynde et al. 2009). Another study of 124 cleaners and kitchen workers, suspected to suffer from OSD, reported that 79.8% (n = 99) of these workers had skin lesions when examined by a dermatologist (Weisshaar et al. 2007). 86.3% (n = 107) were diagnoses with CD (Weisshaar et al. 2007), and with respect to the severity, severe CD was reported in 8.9% (n = 11) (Weisshaar et al. 2007).
Regarding severity of CD, a single study reported hospital cleaning workers to have the highest Hand Eczema Severity Index (HECSI) score (12.18 ± 9.40) defined as moderate CD compared to nursing auxiliaries (8.50 ± 5.68) and nurses (6.63 ± 6.95), although not significantly (Gupta et al. 2018). Another study including 49 hospital cleaning workers and 259 health-care workers (HCW) reported the severity of CD to be (11.53 ± 10.38) (defined as moderate) second highest in cleaners compared to physicians, nurses, clinical technicians, and caregivers (Falay Gür et al. 2022). A Danish study among “1000 cases of severe OCD seen and diagnosed at the Department of dermatology in hospital” reported the prevalence of severe OCD among cleaners to be 10.8% (Schwensen et al. 2013).
Regarding classification of CD, only seven studies (17% of all included studies) provided relevant information. One study from Italy included 396 cleaners, of which 14.1% (n = 56) was recognized with OCD, and allergic contact dermatitis (ACD) was found to be more common than irritant contact dermatitis (ICD) (ACD: 57.1% vs. ICD: 42.9%) (Santarossa et al. 2020). This was also supported by other studies from Denmark, Italy and Germany respectively (Carøe et al. 2010; Skoet et al. 2004; Brans et al. 2019; Lodi et al. 2000). However, in one study from Turkey, which included 245 hospital cleaning workers, ICD was reported in 87.2% and ACD in 12.8% based on patch test results (Aydin Taş et al. 2021). This was also the case in a study from Denmark, which included 67 cleaners with severe OCD of which ACD was more common than ICD (Schwensen et al. 2013).
Risk factors and contact allergies associated with OCD
The main irritants for cleaners were wet work and cleaning products. In particular bleach, detergents, and alkaline substances, chlorine, ammonia, and multi-use cleaning products (including those with hydrochloric acid) were implicated (Mirabelli et al. 2012; Stingeni et al. 1995; Lynde et al. 2009; Aydin Taş et al. 2021; Garrido et al. 2021; Halkier-Sørensen and Thestrup-Pedersen 1993). Regarding wet work, intense exposure was significantly more in cleaners than in health-care and building workers (Lynde et al. 2009; Halkier-Sørensen and Thestrup-Pedersen 1993). In an observational study of 41 office cleaners, the skin of the hands was exposed to wet-work activities in 50% of the time during 3 h of working (Jungbauer et al. 2004). A positive correlation was reported between hours per week spent with wet hands and skin symptoms (Nielsen 1996). Among 1107 cleaners, 81% (n = 896) had wet hands more than ¼ of their working hours (Nielsen 1996). Other irritants reported were gloves, mechanical irritation, soap, and metal (Carøe et al. 2010; Liskowsky et al. 2011; Rui et al. 2012).
The most common contact allergies included rubber additives, biocides, nickel/cobalt, perfumes, black rubber, and other allergens (Carøe et al. 2010; Uter et al. 2010; Geier et al. 2003; Liskowsky et al. 2011). Contact allergy to rubber additives included thiuram/thiuram mix, carbamate/carbamate mix, and mercaptobenzothiazole/mercapto mix (Carøe et al. 2010; Aydin Taş et al. 2021; Uter et al. 2010; Liskowsky et al. 2011). Cleaning has been reported as one of the most frequent occupations associated with nickel and/or chromium and/or cobalt reactions after a working period of 12 years from 2003 to 2015 (n = 170 cleaners) with a sensitization rate of 39% to metals alone or in combination (:Special Issue: 13th Congress of the European Society of Contact Dermatitis (ESCD), 14–17 September 2016 [Available from: ESCD Abstracts: Posters - 2016 - Contact Dermatitis -Wiley Online Library] 2016). In comparison, the prevalence of contact allergy to nickel, chromium, and cobalt in the general population has been reported to be 11.4%, 1.8% and 2.7%, respectively (Alinaghi et al. 2019). In another study investigating contact allergy in 236 cleaning workers, they found nickel, cobalt, thiuram mixture, methyldibromo glutaronitrile, and fragrance mixture I and II to be the most common reactions in patch testing (Aydin Taş et al. 2021).
Regarding preventive measures, only 26% of 1107 cleaners reported regular use of protective gloves during wet work, whereas 58% (n = 676) reported seldom use (Nielsen 1996). In another study among 693 cleaners, 27% (n = 187) reported glove use less than 1 day/week in the last 12 months, while 30% (n = 207) used gloves 1–3 days/week and 27% (n = 187) more than 4 days/week (Mirabelli et al. 2012). Low educational level was also reported to be a risk factor for OCD (Aydin Taş et al. 2021).
Consequences of OCD (quality of life (QoL), sick leave, disability, and loss of job)
Consequences associated with OCD were investigated in six studies. In a tertiary hospital setting, cleaners experienced significantly more impairment in quality of life (Qol) compared to nurses and nursing auxiliaries measured by the Dermatology Life Quality of Life (DLQI) (Gupta et al. 2018) (cleaning: 4.14 ± 3.17 vs. nurses: 1.95 ± 2.46 and nursing auxiliaries: 1.90 ± 1.52) (Gupta et al. 2018).
Sick leave due to OCD was investigated in a Finnish study of 40 cleaners with OCD and was reported by 22.5% (n = 9) (Lammintausta et al. 1982). In a German study of 124 cleaners and kitchen employees with OSD, 49.2% (n = 61) reported sick leave due to skin lesions (Weisshaar et al. 2007). The sick leave was reported to be mostly less than 8 weeks in a period more than 1 year (Weisshaar et al. 2007). Unscheduled absence from work was investigated in Canada. The study included 89 female cleaners and 470 female BW (Lynde et al. 2009). Female cleaners with rash on their hands were more likely to miss work (31%) than BW (5%). (However, the difference was not significant) (Lynde et al. 2009).
Exposure to cleaning agents and/or disinfectants was reported to contribute to the increased rate of disability pension in the cleaning trade among female cleaners in a Danish study including 193 cleaners (Bensefa-Colas, et al. 2014). Among women, 11% of the disability pension cases were attributable to exposure to cleaning agents and/or disinfectants (Feveile et al. 2009).
Having long-term work consequences due to OCD were investigated among 72 cleaners in a Danish study over a period of 9 years, of which 9.7% (n = 7) were awarded a degree of injury > 15% and 90.3% (n = 65) were awarded a degree of injury < 15% (Dietz et al. 2022), which is the percentage of injury the worker is awarded at recognition. A case can be recognized with or without the payment of economic compensation, which is only paid if the degree of injury is evaluated to be ≥ 5% (Dietz et al. 2022). The degree of injury is dependent on an individual evaluation of the workers’ degree of eczema (Dietz et al. 2022).
In a follow-up study after 2–11 years after being recognized with OCD, of the same population, 53.6% (n = 37) reported job loss due to OCD, and 31.4% (n = 22) reported that OCD had a negative impact on job choice (Dietz et al. 2022). Decrease in income was reported by 17.1% (n = 12), and 12.9% (n = 9) had experienced difficulty finding work because of OCD (Dietz et al. 2022).
Prevention of OCD
Three studies investigated primary (n = 2) (Held et al. 2002; Clemmensen et al. 2015) and secondary (n = 1) (Soder et al. 2007) prevention of OCD; however, only one of the studies included cleaners only (Clemmensen et al. 2015), one study included nursing, kitchen, and cleaning workers (Held et al. 2002), and one study included kitchen and cleaning workers (Soder et al. 2007). A primary prevention program investigated the effect of a 1-h group-based educative course in skin protective behavior based on an evidence-based skin protection program. At 3 months follow-up, the participants (who either suffered or did not suffer from HE) demonstrated significant improvement in the severity of CD measured by the Hand Eczema Severity Index (HECSI) and in the knowledge of skin protection as well as skin-protective behavior by means of fewer daily hand washing (Clemmensen et al. 2015). Another primary prevention study based on implementation of a skin care program led to significant improvement in skin care, skin-protective behavior, and skin symptoms in the intervention group (Held et al. 2002). However, no significant difference was found in self-reported skin symptoms between intervention groups and the control group (Held et al. 2002). In Germany, a secondary prevention program in 212 kitchen and cleaning workers with OCD proved effective in skin care habits, use of protective gloves, and reduced number of hand washings. The program was based on a 2-day course of teaching in basic skin care (Soder et al. 2007).
Discussion
This systemic review supports the impression that cleaners have an increased risk of OCD. In addition, it raises some key points for consideration.
Prevalence
In our systematic review study, prevalence of CD among cleaners varied from 8.5% to 15.9% (Gupta et al. 2018; Falay Gür et al. 2022; Nettis et al. 2002; Clemmensen et al. 2015; Douwes et al. 2017), which is not much different from an estimated prevalence of CD in the general population of 14.5% (Quaade et al. 2021). The prevalence of OCD overall varied between 2.2% and 30.1% (Carøe et al. 2010; Gawkrodger et al. 1986; Stingeni et al. 1995; Aydin Taş et al. 2021; Skoet et al. 2004; Santarossa et al. 2020; Nettis et al. 2002; Lammintausta et al. 1982; Lodi et al. 2000; Schwensen et al. 2013; Dietz et al. 2021). This may be explained by differences in the setting of the studies and geographic differences between countries reporting the data and demographic differences in the study populations. As an example, most studies from Denmark only included cases of OCD based on data from the Danish Labour Market Insurance register, possibly meaning that examination and assessment of the patients had been thorough and they were diagnosed by a specialist (Carøe et al. 2010; Skoet et al. 2004; Dietz et al. 2021). The remaining studies did not include patients with recognized cases of OCD, but only participants suspected to have OCD (Gawkrodger et al. 1986; Stingeni et al. 1995; Aydin Taş et al. 2021; Santarossa et al. 2020; Nettis et al. 2002; Lammintausta et al. 1982; Lodi et al. 2000). In addition, some studies did not distinguish between CD and OCD, and the prevalence of OCD may be higher in reality.
Occupational and other risk factors
Wet-work exposure was identified as risk factor for OCD in cleaners in our study, in accordance with studies of wet-work occupations (Meding et al. 2005, 2016; Carøe et al. 2018). However, it is important to notice that wet-work exposure in general is not a major risk factor for OCD, but the main risk determinants of wet-work exposure is the duration and frequency of exposure (Behroozy and Keegel 2014). Clear dose–response relationships for the associations between wet-work exposure and healing and improvement of HE have been reported. It has been shown that a shorter period of time with wet hands and a lower frequency of hand washing at work is related to higher rates of healing and improvement (Carøe et al. 2018). The nature of cleaning tasks requires cleaners to be in contact with water for a long time, which is difficult to prevent even by using technological improvement. Other factors when discussing wet-work exposure as risk factor for OCD include the importance of protective gloves to avoid contact with water, protective gloves being intact and dry inside along the way preventing them from getting wet, and using cotton gloves underneath, when protective gloves are used for more than 10 min. Benefits of regularly using hand moisturizers, which is associated with maintaining skin barrier function and prevention of dryness, should also be mentioned when discussing this topic (Halkier-Sørensen and Thestrup-Pedersen 1993).
Bleach, detergents, chlorine, ammonia, multi-use cleaning products, and other cleaning products were identified to be associated with OCD in cleaners (Mirabelli et al. 2012; Stingeni et al. 1995; Lynde et al. 2009; Aydin Taş et al. 2021; Garrido et al. 2021; Halkier-Sørensen and Thestrup-Pedersen 1993). However, this was not confirmed in a study from New Zealand including 424 cleaners, where only solvents/stain removers were found to be associated with OCD (Douwes et al. 2017). It might be possible that the differences in skin constitution, cleaning tasks, as well as having the opportunity to perform patch test, and use of protective gloves and skin protective behavior may partly explain the various results (Mirabelli et al. 2012; Aydin Taş et al. 2021; Douwes et al. 2017). None of the studies were observational, and behavioral differences in the cleaners may be assumed to influence the results. Not only using cleaning products, but also the frequency of using them has been identified as a major reason to develop OCD (Mirabelli et al. 2012). In addition, a higher occurrence of CD has been associated with outdoor cleaning, cleaning common areas of residential buildings, schools, and building sites (Mirabelli et al. 2012), which might reflect differences in cleaning needs and exposures.
Low educational level was identified as risk factor for developing OCD in cleaners. Several studies investigating cleaners have reported low educational level among the majority of the cleaning workers (Lee et al. 2014; Sejbaek et al. 2022). Health literacy reflects the personal, cognitive and social skills, which determine the ability of individuals to gain access to, understand, and use information to promote and maintain good health (Nutbeam 2000). Patients with low health literacy skills may have insufficient reading, written, or numeracy skills for effective functioning in the health context (Wittink and Oosterhaven 2018). Health literacy is in general correlated with education (Berkman et al. 2011; Kickbusch et al. 2013). Low health literacy is associated with increased morbidity and mortality and lower adherence (Berkman et al. 2011; Miller 2016). No studies have investigated health literacy among cleaners, but it may be speculated that many cleaners have low health literacy, which may affect their ability to prevent or manage OCD.
Consequences of OCD
Overall, cleaners with OCD experience significant, negative impacts in many domains of their lives. The negative impact is evident across many high-risk occupations such as nurses and hairdressers; however, it appears that cleaners have been overlooked, when discussing national action plan for effective prevention of OCD compared to other occupations. As an example, a prevention program was launched in 2011 in all hairdressing schools in Denmark (Dietz et al. 2021). However, no national action on prevention of OCD among cleaners has yet been implemented in Denmark. OCD associated impairment among cleaners is a matter of concern. This is aggravated by some general characteristics including low socio-economic status, limited level of education, pre-existing impairment of quality of life as well as classical medical elements such as pre-existing AD or OCD (Cvetkovski et al. 2005; Cvetkovski et al. 2006). Paying attention to personal and social consequences of having OCD in cleaners is important. Early treatment is important to reduce the risk of chronicity and has influence on job retention for many cleaners. This is a matter of concern, since many professional cleaners have limited opportunities due to low level of education.
OCD prevention programs
In this review, we only identified one single study investigating primary prevention of OCD among cleaners (Clemmensen et al. 2015). The intervention was based on educational skin protection program, and it showed increased knowledge of skin protection, improved skin protective behavior, and decreased severity of CD at 3 months follow-up (Clemmensen et al. 2015). Several secondary prevention programs have been investigated in other occupations with CD but not in cleaners (Ibler et al. 2012a; Mollerup et al. 2014; Fisker et al. 2018; Graversgaard et al. 2018; Gils et al. 2012), based on an educational intervention in skin care and individual counseling (Ibler et al. 2012a), educational videos and individual counseling (Mollerup et al. 2014), and integrated care provided by a multidisciplinary team (a dermatologist, a specialized nurse, and an occupational clinical physician) (Gils et al. 2012). All of the studies were randomized clinical studies with varying results. In the first randomized study from Denmark including 255 health-care workers, an improvement in clinical signs of hand eczema (HECSI), Qol (DLQI), self-evaluated severity, and skin-protective behavior was reported (Ibler et al. 2012a). In the second study, including 360 patients of different occupations with CD, greater reductions in clinical severity and improved behavior after 6 months was reported (Mollerup et al. 2014). However, the effect was dependent on baseline disease severity in the intervention group and no differences in quality of life or burden of disease was found between intervention and control group (Mollerup et al. 2014). In the third study from the Netherlands, an improvement of the HECSI score in the intervention group was reported after 26 weeks (Gils et al. 2012). However, no difference was found in the quality of life, patient’s global assessment of CD, or sick leave (Gils et al. 2012). Only two long-term follow-up studies have investigated secondary prevention of CD (Fisker et al. 2018; Graversgaard et al. 2018). The first study was based on a 2 h educational skin care program, which did not have any marked effect on sickness absence, health-related quality of life, and severity of CD after 1 year among 756 patients with CD (Fisker et al. 2018). In this study, the intervention was group based (not individual) and during the study period there was no repetition of content (Fisker et al. 2018). In the second long-term study, the impact of a secondary prevention program showed attenuation over time among 184 health-care workers, concluding that repeated information and education were needed to continue improvement (Graversgaard et al. 2018). A recent review investigating secondary and tertiary prevention strategies against OCD in Germany concluded that > 60% of patients remained in their occupation after 1 and 5 years following the secondary individual prevention programs (Ahlström et al. 2022). However, these conclusions were not based on randomized controlled trials and there were no control groups (Ahlström et al. 2022).
Despite the different findings regarding prevention programs of CD, the implementation of an effective nationwide prevention program may affect the prevalence of OCD among cleaners. New strategies are needed to educate cleaners in skin protection and prevention to reduce the risk of developing OCD. However, this should be practiced as early intervention, targeting cleaning apprentices and fully trained cleaners early in their work career. Based on studies investigating other occupations with wet work such as hairdressers, it has been reported that HE develops during the apprenticeship or within the first 5 years after graduation in almost half of the cases and these are often severe HE (Havmose et al. 1985; Lind et al. 2007).
Limitations
With regard to limitations, a high level of heterogeneity was observed in the included studies, which may be attributed to variations in the study populations in terms of gender, age, response rates, outcomes, geographic locations, availability of patch tests, and even study type and purpose of each particular study. In addition, some studies included in this review were performed many years ago and may not reflect the current situation regarding CD or OCD in cleaners. However, the decision to include these studies was based on the fact that they could help to describe the development over time.
Conclusion
In conclusion, this study finds that OCD is common among cleaners and associated with severe personal and social consequences. In general, using different cleaning products, the frequency of exposure, and location of cleaning may all possibly be important when discussing OCD among cleaners. However, other factors such as availability of gloves, moisturizer, and individual knowledge may also have an impact on the risk of developing OCD. Randomized studies investigating the effect of primary prevention programs are needed to prevent OCD among cleaners. Personal risk factors such as low educational background should be considered in the planning of future preventive strategies of HE.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
References
Ahlström MG, Dietz JB, Wilke A, Johansen JD, John SM, Brans R (2022) Evaluation of the secondary and tertiary prevention strategies against occupational contact dermatitis in Germany: a systematic review. Contact Dermatitis 87(2):142–153
Alinaghi F, Bennike NH, Egeberg A, Thyssen JP, Johansen JD (2019) Prevalence of contact allergy in the general population: a systematic review and meta-analysis. Contact Dermatitis 80(2):77–85
: Arbejdsmarkedets erhverssikring. Rapport for occupational injury statistics 2020 (in Danish) [Available from: https://www.aes.dk/dokument/aes-arbejdsskadestatistik-2020]. Accessed 1 Dec 2021
Aydin Taş T, Akiş N, Saricaoğlu H (2021) Occupational contact dermatitis in hospital cleaning workers. Dermatitis 32(6):388–396
Behroozy A, Keegel TG (2014) Wet-work Exposure: a main risk factor for occupational hand dermatitis. Saf Health Work 5(4):175–180
Bensefa-Colas L et al (2014) Occupational allergic contact dermatitis and major allergens in France: temporal trends for the period 2001–2010. Br J Dermatol 171(6):1375–1385
Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K (2011) Low health literacy and health outcomes: an updated systematic review. Ann Intern Med 155:97–107
Brans R, Schröder-Kraft C, Skudlik C, John SM, Geier J (2019) Tertiary prevention of occupational skin diseases: prevalence of allergic contact dermatitis and pattern of patch test results. Contact Dermat 80(1):35–44
Carøe T, Ebbehøj N, Agner T (2014) A survey of exposures related to recognized occupational contact dermatitis in Denmark in 2010. Contact Dermat 70:56–62
Carøe TK, Ebbehøj NE, Bonde JPE, Flachs EM, Agner T (2018) Hand eczema and wet work: dose-response relationship and effect of leaving the profession. Contact Dermat 78(5):341–347
Clemmensen KK, Randbøll I, Ryborg MF, Ebbehøj NE, Agner T (2015) Evidence-based training as primary prevention of hand eczema in a population of hospital cleaning workers. Contact Dermat 72(1):47–54
Cvetkovski RS et al (2005) Relation between diagnoses on severity, sick leave and loss of job among patients with occupational hand eczema. Br J Dermatol 152(1):93–98
Cvetkovski RS, Zachariae R, Jensen H, Olsen J, Johansen JD, Agner T (2006) Prognosis of occupational hand eczema: a follow-up study. Arch Dermatol 142(3):305–311
Dickel H, Kuss O, Schmidt A, Diepgen TL (2002) Impact of preventive strategies on trend of occupational skin disease in hairdressers: population based register study. Br Med J 324:1422–1423
Diepgen TL (2003) Occupational skin-disease data in Europe. Int Arch Occup Environ Health 76:331–338
Diepgen TL et al (2015) Guidelines for diagnosis, prevention and treatment of hand eczema. J Dtsch Dermatol Ges 13(1):e1-22
Dietz JB et al (2021) Degree of employment, sick leave, and costs following notification of occupational contact dermatitis-a register-based study. Contact Dermat 84(4):224–235
Dietz JB et al (2021) Incidence rates of occupational contact dermatitis in Denmark between 2007 and 2018: a population-based study. Contact Dermat 85(4):421–428
Dietz JB et al (2022) Occupational contact dermatitis among young people in Denmark—a survey of causes and long-term consequences. Contact Dermat 86(5):404–416
Douwes J et al (2017) Determinants of hand dermatitis, urticaria and loss of skin barrier function in professional cleaners in New Zealand. Int J Occup Environ Health 23(2):110–119
Dulon M, Pohrt U, Skudlik C, Nienhaus A (2009) Prevention of occupational skin disease: a workplace intervention study in geriatric nurses. Br J Dermatol 161:337–344
Falay Gür T, Savaş Erdogan S, Doğan B (2022) Investigation of the prevalence of hand eczema among healthcare professionals in Turkey: a cross-sectional study. J Cosmet Dermatol 21(4):1727–1735
Feveile H, Christensen KB, Flyvholm MA (2009) Self-reported occupational skin contact with cleaning agents and the risk of disability pension. Contact Dermat 60(3):131–135
Fisker MH et al (2018) Prevention of hand eczema: effect of an educational program versus treatment as usual - results of the randomized clinical PREVEX trial. Scand J Work Environ Health 44(2):212–218
Garrido AN, House R, Lipszyc JC, Liss GM, Holness DL, Tarlo SM (2021) Cleaning agent usage in healthcare professionals and relationship to lung and skin symptoms. J Asthma 25:1–9
Gawkrodger DJ, Lloyd MH, Hunter JA (1986) Occupational skin disease in hospital cleaning and kitchen workers. Contact Dermat 15:132–135
Geier J, Lessmann H, Uter W, Schnuch A (2003) Information Network of Departments of Dermatology (IVDK). Occupational rubber glove allergy: results of the information network of departments of dermatology (IVDK), 1995–2001. Contact Dermat 48(1):39–44
Graversgaard C, Agner T, Jemec GBE, Thomsen SF, Ibler KS (2018) A long-term follow-up study of the Hand Eczema Trial (HET): a randomized clinical trial of a secondary preventive programme introduced to Danish healthcare workers. Contact Dermat 78(5):329–334
Gupta SB et al (2018) Hand eczema in nurses, nursing auxiliaries and cleaners-a cross-sectional study from a tertiary hospital in western India. Contact Dermat 79(1):20–25
Halkier-Sorensen L (1996) Occupational skin diseases. Contact Dermat 35:1–120
Halkier-Sørensen L, Thestrup-Pedersen K (1993) The efficacy of a moisturizer (Locobase) among cleaners and kitchen assistants during everyday exposure to water and detergents. Contact Dermat 29(5):266–271
Hamnerius N, Svedman C, Bergendorff O, Björk J, Bruze M, Pontén A (2018) Wet work exposure and hand eczema among healthcare workers: a cross-sectional study. Br J Dermatol 178(2):452–461
Hansen KS (1983) Occupational dermatoses in hospital cleaning women. Contact Dermat 9:343–351
Havmose M, Thyssen JP, Zachariae C, Johansen JD (2022) Long-term follow-up of hand eczema in hairdressers: a prospective cohort study of Danish hairdressers graduating from 1985 to 2007. J Eur Acad Dermatol Venereol 36(2):263–270
Held E, Wolff C, Gyntelberg F, Agner T (2001) Prevention of work-related skin problems in student auxiliary nurses: an intervention study. Contact Dermat 44(5):297–303
Held E, Mygind K, Wolff C, Gyntelberg F, Agner T (2002) Prevention of work related skin problems: an intervention study in wet work employees. Occup Environ Med 59(8):556–561
Ibler KS et al (2012a) Skin care education and individual counselling versus treatment as usual in healthcare workers with hand eczema: randomised clinical trial. BMJ 345:e7822
Ibler KS, Jemec GBE, Flyvholm MA, Diepgen TL, Jensen A, Agner T (2012b) Hand eczema: prevalence and risk factors of hand eczema in a population of 2274 healthcare workers. Contact Dermat 67(4):200–207
Jungbauer FH, Van Der Harst JJ, Schuttelaar ML, Groothoff JW, Coenraads PJ (2004) Characteristics of wet work in the cleaning industry. Contact Dermat 51(3):131–134
Kickbusch I, Pelikan JM, Apfel F, Tsouros AD (2013) Health literacy: the solid facts. The World Health Organization, regional office for Europe, Copenhagen
Lammintausta K (1983) Hand dermatitis in different hospital workers who perform wet work. Derm Beruf Umwelt 31:14–19
Lammintausta K, Kalimo K, Aantaa S (1982) Course of hand dermatitis in hospital workers. Contact Dermat 8(5):327–332
Lee SJ, Nam B, Harrison R, Hong O (2014) Acute symptoms associated with chemical exposures and safe work practices among hospital and campus cleaning workers: a pilot study. Am J Ind Med 57(11):1216–1226
Lind M-L, Albin M, Brisman J et al (2007) Incidence of hand eczema in female Swedish hairdressers. Occup Environ Med 64:191–195
Liskowsky J, Geier J, Bauer A (2011) Contact allergy in the cleaning industry: analysis of contact allergy surveillance data of the information network of departments of dermatology. Contact Dermat 65(3):159–166
Lodi A, Mancini LL, Ambonati M, Coassini A, Ravanelli G, Crosti C (2000) Epidemiology of occupational contact dermatitis in a North Italian population. Eur J Dermatol 10(2):128–132
Loeffler H, Bruckner T, Diepgen T, Effendy I (2006) Primary prevention in health care employees: a prospective intervention study with a 3-year training period. Contact Dermat 54:202–209
Luk N-MT et al (2011) Hand eczema among Hong Kong nurses: a self-report questionnaire survey conducted in a regional hospital. Contact Dermat 65(6):329–335
Lund T, Petersen SB, Flachs EM, Ebbehøj NE, Bonde JP, Agner T (2020) Risk of work-related hand eczema in relation to wet work exposure. Scand J Work Environ Health 46(4):437–445
Lynde CB, Obadia M, Liss GM, Ribeiro M, Holness DL, Tarlo SM (2009) Cutaneous and respiratory symptoms among professional cleaners. Occup Med (lond) 59(4):249–254
Magnano M, Silvani S, Vincenzi C, Nino M, Tosti A (2009) Contact allergens and irritants in household washing and cleaning products. Contact Dermat 61(6):337–341
Meding B, Lantto R, Lindahl G et al (2005) Occupational skin disease in Sweden—a 12-year follow-up. Contact Dermat 53:308–313
Meding B, Anveden Berglind I, Alderling M, Lindahl G, Wrangsjö K (2016) Water exposure–challenging differences between occupations. Contact Dermat 74(1):22–28
Melo MDGM, Villarinho ALCF, Leite IDC (2019) Sociodemographic and clinical profile of patients with occupational contact dermatitis seen at a work-related dermatology service, 2000–2014. An Bras Dermatol 94(2):147–156
Miller TA (2016) Health literacy and adherence to medical treatment in chronic and acute illness: a meta-analysis. Patient Educ Couns 99(7):1079–1086
Mirabelli MC et al (2012) Occupational risk factors for hand dermatitis among professional cleaners in Spain. Contact Dermat 66(4):188–196
MOCDr D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred Reporting Items for Systematic Reviews and Meta-analyses: the PRISMA statement. PLoS Med 6:e1000097
Mollerup A, Veien NK, Johansen JD (2014) Effectiveness of the Healthy Skin Clinic–a randomized clinical trial of nurse-led patient counselling in hand eczema. Contact Dermat 71(4):202–214
Nettis E, Colanardi MC, Soccio AL, Ferrannini A, Tursi A (2002) Occupational irritant and allergic contact dermatitis among healthcare workers. Contact Dermat 46(2):101–107
Nichol K, Copes R, Kersey K, Eriksson J, Holness DL (2019) Screening for hand dermatitis in healthcare workers: comparing workplace screening with dermatologist photo screening. Contact Dermat 80(6):374–381
Nielsen J (1996) The occurrence and course of skin symptoms on the hands among female cleaners. Contact Dermat 4:284–291
Nutbeam D (2000) Health literacy as a public goal: a challenge for contemporary health education and communication strategies into the 21st century. Health Promot Int 15:259–267
Quaade AS, Simonsen AB, Halling AS, Thyssen JP, Johansen JD (2021) Prevalence, incidence, and severity of hand eczema in the general population—a systematic review and meta-analysis. Contact Dermat 84(6):361–374
Rui F, Bovenzi M, Prodi A et al (2012) Concurrent sensitization to metals and occupation. Contact Dermat 67:359–366
Santarossa M, Mauro M, Belloni Fortina A, Corradin MT, Larese Filon F (2020) Occupational contact dermatitis in Triveneto: analysis of patch test data of the north eastern Italian database from 1996 to 2016. Contact Dermat 82(6):370–379
Schwanitz HJ, Riehl U, Schlesinger T, Bock M, Skudlik C, Wulfhorst B (2003) Skin care management: educational aspects. Int Arch Occup Environ Health 76:374–381
Schwensen JF, Friis UF, Menné T, Johansen JD (2013) One thousand cases of severe occupational contact dermatitis. Contact Dermat 68(5):259–268
Sejbaek CS et al (2022) Professional cleaning and risk of asthma—a Danish nationwide register-based study. Scand J Work Environ Health 48(2):127–136
Singgih SIR, Latinga H, Nater JP, Woest TE, Kruyt- Gaspersz JA (1986) Occupational hand dermatoses in hospital cleaning personnel. Contact Dermat 14:14–19
Skoet R, Olsen J, Mathiesen B, Iversen L, Johansen JD, Agner T (2004) A survey of occupational hand eczema in Denmark. Contact Dermat 51(4):159–166
Skudlik C et al (2012) First results from the multicentre study rehabilitation of occupational skin diseases – optimization and quality assurance of inpatient management (ROQ). Contact Dermatitis 66:140–147
Soder S, Diepgen TL, Radulescu M, Apfelbacher CJ, Bruckner T, Weisshaar E (2007) Occupational skin diseases in cleaning and kitchen employees: course and quality of life after measures of secondary individual prevention. J Dtsch Dermatol Ges 5(8):670–676
: Special Issue: 13th Congress of the European Society of Contact Dermatitis (ESCD), 14–17 September 2016 [Available from: ESCD Abstracts: Posters - 2016 - Contact Dermatitis - Wiley Online Library]
Stingeni L, Lapomarda V, Lisi P (1995) Occupational hand dermatitis in hospital environments. Contact Dermat 33(3):172–176
Uter W, Hegewald J, Pfahlberg A, Lessmann H, Schnuch A, Gefeller O (2010) Contact allergy to thiurams: multifactorial analysis of clinical surveillance data collected by the IVDK network. Int Arch Occup Environ Health 83(6):675–681
van Gils RF, Boot CR, Knol DL, Rustemeyer T, van Mechelen W, van der Valk PG et al (2012) The effectiveness of integrated care for patients with hand eczema: results of a randomized, controlled trial. Contact Dermat 66(4):197–204
Vindenes HK, Svanes C, Lygre SHL, Hollund BE, Langhammer A, Bertelsen RJ (2017) Prevalence of, and work-related risk factors for, hand eczema in a Norwegian general population (The HUNT Study). Contact Dermat 77(4):214–223
Weisshaar E et al (2007) Secondary individual prevention of occupational skin diseases in health care workers, cleaners and kitchen employees: aims, experiences and descriptive results. Int Arch Occup Environ Health 80(6):477–484
Wilke A, Gediga G, Schlesinger T, John SM, Wulfhorst B (2012) Sustainability of interdisciplinary secondary prevention in patients with occupational hand eczema: a 5-year follow-up survey. Contact Dermat 67:208–216
Wittink H, Oosterhaven J (2018) Patient education and health literacy. Musculoskelet Sci Pract 38:120–127
Acknowledgements
This research has received funding from the Danish Working Environment Fund with grant number: 20205100702.
Funding
This research has received funding from the Danish Working Environment Fund with grant number: 20205100702.
Author information
Authors and Affiliations
Contributions
FS and TM: conceptualization, methodology, validation, formal analysis, investigation, resources, data curation, writing original draft, writing, review and editing, visualization, and project administration. OM, GJ and KI: conceptualization, methodology, investigation, resources, writing, original draft, writing, review and editing, visualization, project administration, and supervision.
Corresponding author
Ethics declarations
Conflict of interest
Dr Jemec reported receiving grants from AbbVie, LEO Foundation, Afyx, InflaRx, Janssen-Cilag, Novartis, UCB, CSL Behring, Regeneron, Sanofi, Boehringer Ingelheim, Union Therapeutics, and Toosonix and personal fees from Coloplast, Chemocentryx, LEO Pharma, Incyte, Kymera, and VielaBio. Dr. Ibler has been part of advisory boards and received personal fees from Astra Zeneca, Leo Pharma; Sanofi Genzymes and Eli Lilly. Dr Jemec and Ibler declare that none of the mentioned conflicts of interest had any influence in the content of this manuscript.
Ethical approval
Not applicable.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sedeh, F.B., Michaelsdóttir, T.E., Jemec, G.B.E. et al. Prevalence, risk factors, and prevention of occupational contact dermatitis among professional cleaners: a systematic review. Int Arch Occup Environ Health 96, 345–354 (2023). https://doi.org/10.1007/s00420-022-01937-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00420-022-01937-6