Abstract
Purpose
The impact of organizational change at work on cardiovascular disease (CVD) among employees is poorly understood. We examined the longitudinal associations between different types of work-unit organizational changes and risk of CVD among employees.
Methods
We used multilevel mixed-effects parametric survival models to assess the risk of incident ischemic heart disease and stroke (72 events) during 2014 according to organizational changes in 2013 among 14,788 employees working in the same work unit from January through December 2013. We excluded employees with pre-existing CVD events between 2009 and 2013. Data on organizational changes defined as mergers, split-ups, relocations, change in management, employee layoffs, and budget cuts were obtained from work-unit managers (59% response).
Results
There was an excess risk of CVD in the year following change in management (HR 2.04, 95% CI 1.10–3.78) and employee layoff (HR 2.44, 95% CI 1.29–4.59) in the work unit relative to no change. Exposure to any organizational change also suggested increased risk of CVD (HR 1.48, 95% CI 0.91–2.43). Including perceived stress as mediator in the regression models attenuated the point risk estimates only slightly, indicating no important mediation through this psychosocial factor.
Conclusions
Work-unit organizational change may be associated with excess risk of incident CVD among the employees relative to stable workplaces.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Organizational changes in workplaces have become a part of many employees’ lives. Such changes seem to be motivated by a combination of rapid technological developments (e.g., digitalization of workflows) as well as globalization processes (e.g., flexibility of labor) and increasing concentration of capital (Smaglik 2005; Gaynor et al. 2012; Eurofound 2015). Public-sector workplaces are no exception against these forces. During the last two decades, all public-sector hospitals in Denmark were required by the government to increase annual treatment rates by 1.5–2.0% without parallel budget adjustments (Danish Ministry of Finance 2017). This has led to numerous organizational changes (e.g., mergers, downsizing, and implementation of new technology) attempting to maximize efficiency.
Increasingly, there are indications that organizational changes are extracting a cost in terms of employee health and psychological well-being (Dahl 2011; Bamberger et al. 2012; Jong et al. 2016; Jensen et al. 2018). The existing epidemiological literature on organizational changes and health status is mainly based in Nordic studies and focuses on single types of changes (e.g., downsizing) (Jong et al. 2016). The majority of these studies show deleterious health effects among employees remaining after the changes (Vahtera et al. 1997; Bamberger et al. 2012; Kjekshus et al. 2014; Jong et al. 2016), although inconsistent evidence exists (Theorell et al. 2003; Østhus and Mastekaasa 2010). The Finnish 10-town study demonstrated a doubled risk of cardiovascular mortality among permanent employees related to major downsizing (i.e., > 18% staff reduction). Interestingly, this excess risk of cardiovascular mortality has been observed soon after downsizing (Vahtera et al. 2004) and company closure (Drivas et al. 2013), indicating a triggering effect. No studies have yet focused on cardiovascular disease (CVD) following other specific types of organizational changes, as there are reports of higher long-term sickness-absence rates following mergers, split-ups, reallocation of employees, and the establishment or shutting down of work units (Ingelsrud 2014; Jensen et al. 2018).
Researchers have argued in favor of a causal relation between perceived stress and CVD (Rod et al. 2009), and a meta-analysis found a 1.3-fold increased risk of coronary heart disease related to high perceived stress in the general population (Richardson et al. 2012). In addition, there are indications of increased use of psychotropic medications for stress-related mental disorders following various types of organizational changes (Dahl 2011), such as downsizing (Kivimäki et al. 2007) and change in management (Jensen et al. 2019). One study found common stressful work-related events (e.g., pressure of deadlines and perceived competition) to trigger heart attacks, whereas no higher risk due to self-reported events of being laid-off/quitting (Möller et al. 2005). Moreover, levels of blood pressure and mental distress have been found to be elevated shortly before and after reorganization involving change in management with strongest effects among employees reporting most future job uncertainty (Pollard 2001).
In sum, organizational changes may be associated with a higher risk of CVD that is potentially mediated through work stress. Yet, there is a need for studies examining these complex associations and distinguishing between different types of organizational changes.
We sought to investigate the prospective short-term relations between work-unit organizational changes and CVD among public healthcare employees in the Capital Region of Denmark.
Methods and materials
Data sources and population
This study used data from the “Well-being in Hospital Employees (WHALE)” cohort (Hvidtfeldt et al. 2017) to examine work-unit organizational change observed from 1 January through 31 December 2013 with follow-up on CVD among employees from baseline at 1 January through 31 December 2014. The source population was established when all 37,720 employees (nested in 2696 work units nested in 14 institutions) in the Capital Region of Denmark were invited to take part in a work-environment survey in March 2014 (84% response). The vast majority of the surveys were administered by working email, and paper versions were distributed to employees with no working email (e.g., cleaning staff). The employees received up to three reminders on completing the survey.
We extracted complete sociodemographic and occupational information at baseline from company registers. Complete data on cause of death, date of hospital admission for ischemic heart disease (ICD-10 codes: I20–I25) and stroke (I61, I63–I64), and personal gross income were obtained via linkage to national registers.
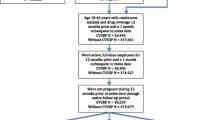
We included employees aged ≥ 18 years with ≥ 18.5 weekly working hours in the same work unit (or its derived unit if changes had occurred). We included employees from a work unit if ≥ 3 employees and ≥ 30% of the staff remained in the same unit throughout the period of observation on organizational changes. For example, if work units A and B (each with three employees) merged into work-unit C, we included all six employees in the study population. We excluded smaller work units (fewer than three employees) as well as individuals with a personal history of ischemic heart disease or stroke between 2009 and 2013 and employees working in a department in Spain. The final study population with complete data on work-unit organizational changes, cardiovascular events, and covariates included 14,788 employees nested in 1283 work units nested in 13 institutions (Fig. 1 and Supplementary material 1).
Work-unit organizational changes
From April through June 2016, we collected data on work-unit-level organizational changes by distributing an email survey to every manager in the source population. In this survey, each manager was asked to provide semi-annual information (yes/no) on the work unit that they managed regarding the occurrence of mergers, split-ups, relocation, change in management, employee layoff(s), and budget cuts in 2013 (59% response). At the work-unit level (level 2), we created an indicator variable (yes/no) for each of the six types of organizational changes occurring throughout 2013. In addition, we created an indicator variable for any of these changes in the same period.
Cardiovascular disease
Employees were followed from baseline at 1 January 2014 to first-time hospital admission or death due to CVD (i.e., event), death not due to CVD (i.e., censoring), or end of study by 31 December 2014, whichever came first.
Covariates
The following employee-level variables were included as potential confounders of the relation between work-unit organizational changes and CVD: age, sex, occupational group, seniority, full-time employment, manager status, contractual employment, personal gross income, and days of sickness absence in 2012. We also included the number of employees within work units as a potential work-unit-level confounder. Since different types of organizational changes were partially overlapping, we included a priori selected work-unit level variables as potential confounders (Supplementary materials 2–3). For example, confounders for the association between employee layoff and CVD included mergers, change in management, and budget cuts. This approach was consistent with a previous study from our research group (Jensen et al. 2019).
Employee perceived stress was measured with the item “To what degree have you been stressed for the last 6 months?” from the work-environment survey using a 5-point scale ranging 1=”Not at all” to 5=”Very high degree”. Non-respondents in the study population (14%) were included in the analyses.
Statistical analyses
Hazard ratios (HR) and 95% confidence intervals (CI) from multilevel mixed-effects parametric survival models assessed the relations between work-unit organizational changes in 2013 and days to CVD through 2014. Employees (level 1) were nested within work units (level 2), which again were nested within institutions (level 3) to account for clustering in the hierarchical structure of the data.
We fitted models with a Weibull distribution, because we expected the effect of organizational changes on subsequent CVD to decrease monotonically during follow-up (George et al. 2014). Employees that experienced organizational change would likely establish stressful new workflows as standard during the following year. We assessed the proportion of variance explained by the organizational higher levels, as this could be a target of intervention. This was done by rerunning the Weibull models but with Accelerated-Failure Time (AFT) parametrization to calculate the Intra-class Correlation Coefficient (ICC) using the following formula for work unit j and institution k:
In addition, ρ is the ancillary parameter from the Weibull model (Canette 2016). Using AFT parametrization does not change the fitted Weibull model–only the interpretation of the output (George et al. 2014). The \({\text{ICC}}\, \times \, 1 0 0\) can be interpreted as the percentage of total variance in CVD explained by each higher organizational level (Snijders and Bosker 2012). This could be any factor differing between work units (e.g., organizational changes, medical specialties) and between institutions (e.g., local policies on working environment).
We used a six-step sequential modeling strategy as follows:
Model 1: A null model with a random intercept for the work-unit level. Assesses the proportion variation in CVD explained by factors at the work-unit level.
Model 2: As model 1, but nesting the work-unit level within the institutional level (null multilevel model with three levels). Assesses the proportion of variance in CVD explained by factors at the work-unit (nested within institutions) and the institutional level.
Model 3: As model 1, but entering only the indicator variable for any work-unit organizational change (random-intercepts model with two levels). Assess the crude association between any organizational change and risk of CVD for future comparison.
Model 4: As model 3, but entering work-unit-level organizational change variables in the fixed part (random-intercepts model with two levels). Assesses the risk of CVD explained by the organizational change indicators conditioned on employee-level confounders and latent work-unit-level factors.
Model 5: As model 4, but nesting the work-unit level within the institutional level (random-intercepts model with three levels). Risk estimates of CVD additionally conditioned on latent institutional-level factors.
Model 6: As model 5, but entering work-unit level confounder(s) when modeling each type of change (random-intercepts model with three levels). Allows interpretation of the relative risk of CVD associated with each change conditioned on employee-level factors, confounding work-unit-level changes, and latent work-unit and institutional-level factors.
The mediating roles of perceived stress were assessed by comparing the risk estimates from each regression model with and without the perceived-stress variable. A reduced risk estimate when included was taken as evidence of mediation (Baron and Kenny 1986).
A significance level of 0.05 was used throughout. The statistical analyses were performed in STATA version 14.2 software (Stata Corporation, College Station, TX, USA).
Results
The descriptive statistics and data structure of the study population are shown in Table 1 and Supplementary material 1. The study population predominantly comprised females, nursing-care workers, and employees with permanent employment, where about half of the work units (and employees) were exposed to any organizational changes. All 72 CVD events of ischemic heart disease (n = 49) and stroke (n = 23) in 2014 were recorded as hospital admission. During follow-up through 2014, seven employees died due to other reasons than CVD and were thus censored.
Table 2 shows the risk of CVD related to all employee-level confounders, exposure to any work-unit organizational change, and perceived stress. There were indications of a higher risk of CVD following any organizational changes (HR 1.48, 95% CI 0.91–2.43), although this finding was poorly supported in the data (model 5). Models 1–2 show that the work-unit level and the institutional level accounted for about 20% and 5%, respectively, of the total variance in CVD. Models 3–5 show that the HR estimate for any organizational change relative to no change decreased slightly from 1.48 to 1.45 when accounting for perceived stress as mediator in the regression model. Despite weak statistical evidence, the direction of the HR-point estimate indicated a higher risk of CVD among employees reporting a very high degree of perceived stress relative to those reporting no stress at all.
In Table 3, model 6 (main model) shows that there was higher risk of CVD following change in management (HR 2.04, 95% CI 1.10–3.78) and employee layoff (HR 2.44, 95% CI 1.29–4.59). When adjusting for other confounding work-unit organizational changes the HR-point estimates of all change indicators increased (models 5–6). Including perceived stress as a potential mediator in model 6 attenuated the HR-point estimates only slightly.
Sensitivity analyses
To assess the impact of missing data on organizational changes, we conducted a sensitivity analysis where all eligible employees with missing data on changes were assigned to the reference category of “no changes”. Similar results were found for any change (HR 1.57, 95% CI 1.07–2.30) compared to those in Table 2 (HR 1.48, 95% CI 0.91–2.43), indicating no impact of missing data on changes.
Extending follow-up on CVD to also include incidents in 2015 diminished the association according to any organizational changes (HR 1.03, 95% CI 0.72–1.48), suggesting that the detrimental effects were short-term.
We assessed if the marked risk directions of the highest categories of seniority and income were due to residual age-confounding by stepwise adding age2 and age3 in models 3–5 (Table 2). Including neither age2 nor age2 and age3 changed the point estimates for HR meaningfully, suggesting no residual confounding by age.
Study participation required working in the same work unit through 2013, but some laid-off employees could be included in the study population if their termination period extended into 2014. Employment termination periods ranged 3–6 months depending on seniority. To assess if the employee-layoff effects were attributed to poor health status among those laid-off, we restricted model 6 for “employee layoff” to changes occurring only in the first semester of 2013 (i.e., exposure and covariates at level 2) while keeping the follow-up period through 2014 unaltered. An employee laid-off in the first semester of 2013 would terminate the employment in the last semester 2013 and thus not be included for follow-up. Results from this sensitivity analysis supported the excess risk of CVD following employee layoff (HR 2.04, 95% CI 0.99–4.21) relative to no changes.
Discussion
Change in management and employee layoff in the work unit were associated with higher risk of incident cardiovascular events among the employees remaining during these changes relative to no changes. Exposure to any changes seemed also to be a risk factor for CVD, although there was some uncertainty regarding this finding. Mergers, split-ups, relocation, and budget cuts were not statistically significantly associated with CVD in the data. The HR-point estimates of all change indicators decreased only slightly when adjusting for perceived stress, indicating that this psychosocial factor was not an important mediator of the association in the present study.
Previous findings and potential mechanisms
Our finding of a 2.4-fold higher risk of CVD in the year after employee layoff in the work unit is consistent with the 5.1-fold higher cardiovascular mortality in the first 4 years following major downsizing among employees who kept their job reported in a Finnish study (Vahtera et al. 2004). In the same study, minor downsizing (8–18% staff reduction) was not associated with a higher risk of cardiovascular mortality (although estimates pointed in this direction) (Vahtera et al. 2004), indicating some sensitivity towards the proportion of laid-off employees. Supporting this a study found 4.8 times higher mortality from ischemic heart disease following closure of an entire company among male ex-employees, although no association was found with cerebrovascular mortality (Drivas et al. 2013). As termination periods extended up to 6 months in our study, some employees laid-off in 2013 may be included in the study population with follow-up in 2014. However, a sensitivity analysis showed that employee layoff only occurring in the first semester of 2013 was related to a similarly high risk of CVD through 2014 (HR 2.0 vs. HR 2.4), suggesting that the present employee-layoff effects were attributed to the employees who kept their job in 2013. We also found that employees experiencing a change in management had a doubled risk of subsequent CVD relative to employees experiencing no changes. To the extent of our knowledge, this is the first epidemiological study to demonstrate an association between this type of organizational change and CVD, although there is some prior evidence of associations with other adverse outcomes (Greubel and Kecklund 2011; Ingelsrud 2014; Jensen et al. 2018). A new management may give rise to concerns about future job situation and new stressful work procedures, which could potentially explain why change in management was related to cardiovascular events, although we had no data to support this. The HR estimate of any changes pointed to a higher risk of CVD, but this result was inadequately supported in the data. We were unable to detect associations with CVD for mergers, split-ups, relocation, and budget cuts, which may be due to lack of statistical power as these types of changes were least frequent in the data.
Hypertension, e.g., due to episodic stressful events at work, may burst blood vessels or disrupt arterial plaque deposits that can clog blood supply and lead to ischemic heart disease or stroke. Organizational changes inducing excess negative emotions (e.g., distress, anger, and frustration) could be regarded such workplace stressor (Kivimäki and Steptoe 2018). However, we found no convincing indications of perceived stress mediating the association between changes and CVD. This could be due to using a single-item perceived-stress measure, which introduce poor discrimination between the variable categories as indicated by the HR-point estimates and the broad confidence intervals in Table 2. In combination with the few CVD events, the present study may have been statistically underpowered to detect mediation of the CVD effects through perceived stress. A previous study demonstrated that half of the effects of major downsizing on medically certified sickness absence were mediated by changes in physical demands, job control, and job insecurity (Kivimäki et al. 2000), suggesting that these psychosocial factors may also play an important role in mediating CVD effects. Working in the public sector of Denmark is generally considered as a secure employment. The relatively low unemployment rate in the capital region decreased from 6.0 to 5.3% between 2013 and 2014 (Statistics Denmark 2019), suggesting that fear of long-term unemployment would not have been a factor following organizational changes among many of the employees examined. However, we lacked data on job insecurity to test this.
Table 2 suggests that the work-unit level was an important contributor to variation in CVD events. However, this contribution diminished when adjusting for all confounders in the regression model, indicating the homogeneity in characteristics of the work units. For example, “service/technical workers” strongly predicted CVD and since work units were mostly comprised by the same occupational groups, this may likely have contributed to the drop in the work-unit-level ICC when adjusting for “occupational groups” in Table 2.
Strengths and limitations
Limitations are highlighted in the following. First, the potential impacts of organizational changes on CVD before and during the changes were not examined. We started follow-up at 1 January 2014 to ascertain that the outcome of CVD occurred after potential exposure to changes in 2013, as there were no data on change initiation–only change occurrence. Excluding CVD events in 2013 may have contributed to underestimating the associations. Second, we did not have data to account for organizational changes during the follow-up period. This may have underestimated the results, as the reference category of work units not changed through 2013 would be more likely to be reorganized in 2014 than work units changed recently. Third, the reorganization itself could layoff managers and, therefore, cause missing data on changes, as these were collected retrospectively via email. Indeed, the email addresses were not changed if the managers remained employed within the Capital Region of Denmark. A sensitivity analysis suggested no impact of missing data on changes in line with a previous analysis comparing baseline characteristics between employees with and without data on changes from the WHALE cohort (Jensen et al. 2018). The CVD rates of employees with (n = 14,788, 0.49%) and without data on changes (n = 10,673, 0.36%) were comparable (p = 0.12). Fourth, power analysis showed that the main analysis was statistically powered to detect an HR of 1.94 (n = 14,788, power = 0.8, type-I rate = 5%) in keeping with effect sizes from the previous studies (Vahtera et al. 2004; Drivas et al. 2013). Due to few CVD events, the analyses of specific types of changes may be underpowered with a risk of type-II statistical error as evidenced by broad 95% CIs, although exposure to change in management and employee layoff were both “statistically significantly” associated with CVD. Since the hypothesis was addressing short-term effects of organizational changes an extension of the follow-up period will not increase the power. Finally, the presented associations may have been inflated by excess job insecurity and job demand control prior to the changes, but there were no data to adjust for these potential confounders in the regression models.
This study has several strengths. First, data on changes, CVD, and perceived stress originated from independent sources and, thus, common-method bias is not an issue (Podsakoff et al. 2003). Second, organizational changes were measured at the work-unit level, ensuring that the employees did experience the potential reorganization. Third, we included only those employees, who worked in the same work unit during the observation of changes, which, again, ensured that the employees were affected by the changes. Fourth, we accounted for clustering on two higher levels in the organizational structure, which allowed us to assess variance explained by latent institutional and work-unit-level factors. Finally, we consider it as a strength of the study that we assessed the relative risk of CVD following various and frequently occurring types of changes. This also allowed us to establish a purer reference group of no changes as compared to many prior studies examining a single type of change.
In conclusion, this study demonstrated a higher risk of CVD among the employees who kept their job during change in management and employee layoff in the work unit relative to no organizational changes. This risk direction was also indicated for exposure to any changes. Exposure to mergers, split-ups, relocation, and budget cuts may also be associated with CVD, but further studies with stronger statistical power are needed to support this. Inferences to other workplace contexts should be made cautiously because of the few cardiovascular events observed as well as the age and sex composition of the study population. We recommend that organizational changes, especially change in management and employee layoff in the work unit, should be considered as risk factors for health by decision makers, managers, and employees. Future studies with should assess potential mediation of CVD effects through perceived stress and other psychosocial factors (e.g., job demand control and job insecurity) using multiple items from a validated questionnaire (e.g., Cohen’s Perceived Stress Scale, Cohen et al. 1983; Danish Psychosocial Questionanire, Clausen et al. 2019). These factors should be measured before and after the organizational changes to assess changes in psychosocial work environment. In addition, further research should evaluate possible differential effects by occupational groups as well as the circumstances under which organizational changes induce beneficial or adverse effects to identify possible targets of intervention.
References
Baron RM, Kenny DA (1986) The moderator-mediator variable distinction in social the moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol 51:1173–1182. https://doi.org/10.1037/0022-3514.51.6.1173
Bamberger SG, Vinding AL, Larsen A et al (2012) Impact of organisational change on mental health: a systematic review. Occup Environ Med 69:592–598. https://doi.org/10.1136/oemed-2011-100381
Canette I (2016) In the spotlight: intraclass correlations after multilevel survival models. In: Stata News. https://www.stata.com/stata-news/news31-2/intraclass-correlations/ Accessed 27 Sep 2019.
Cohen S, Kamarck T, Mermelstein R (1983) A global measure of perceived stress. J Health Soc Behav 24:385–396
Clausen T, Madsen IE, Christensen KB et al (2019) The Danish Psychosocial Work Environment Questionnaire (DPQ): development, content, reliability and validity. Scand J Work Environ Health 45:356–369. https://doi.org/10.5271/sjweh.3793
Dahl MS (2011) Organizational change and employee. Stress 57:240–256. https://doi.org/10.1287/mnsc.1100.1273
Drivas S, Rachiotis G, Stamatopoulos G et al (2013) Company closure and mortality in a Greek bus company. Occup Med 63:231–233. https://doi.org/10.1093/occmed/kqs235
de Jong T, Wiezer N, de Weerd M et al (2016) The impact of restructuring on employee well-being: a systematic review of longitudinal studies. Work Stress 30:91–114. https://doi.org/10.1080/02678373.2015.1136710
Danish Ministry of Finance (2017) Sygehusene fritages for produktivitetskrav i 2018. https://www.fm.dk/nyheder/pressemeddelelser/2017/10/sygehusene-fritages-for-produktivitetskrav-i-2018 Accessed 29 Nov 2018.
Eurofound (2015) ERM annual report 2014: restructuring in the public sector. Publications Office of the European Union, Luxembourg
Greubel J, Kecklund G (2011) The impact of organizational changes on work stress, sleep, recovery and health. Ind Health 49:353–364. https://doi.org/10.2486/indhealth.MS1211
Gaynor M, Laudicella M, Propper C (2012) Can governments do it better? Merger mania and hospital outcomes in the English NHS. J Health Econ 31:528–543. https://doi.org/10.1016/j.jhealeco.2012.03.006
George B, Seals S, Aban I (2014) Survival analysis and regression models. NIH Public Access 21:686–694. https://doi.org/10.1007/s12350-014-9908-2.Survival
Hvidtfeldt UA, Bjorner JB, Jensen JH et al (2017) Cohort profile: the well-being in hospital employees (WHALE) study. Int J Epidemiol 46:1758–1759. https://doi.org/10.1093/ije/dyx073
Ingelsrud MH (2014) Reorganization increases long-term sickness absence at all levels of hospital staff: panel data analysis of employees of Norwegian public hospitals. BMC Health Serv Res 14:411. https://doi.org/10.1186/1472-6963-14-411
Jensen JH, Flachs EM, Skakon J et al (2018) Dual impact of organisational change on subsequent exit from work unit and sickness absence: a longitudinal study among public healthcare employees. Occup Environ Med 75:479–485. https://doi.org/10.1136/oemed-2017-104865
Jensen JH, Bonde JP, Flachs EM et al (2019) Work-unit organisational changes and subsequent prescriptions for psychotropic medication: a longitudinal study among public healthcare employees. Occup Environ Med 76:143–150. https://doi.org/10.1136/oemed-2018-105442
Kivimäki M, Steptoe A (2018) Effects of stress on the development and progression of cardiovascular disease. Nat Rev Cardiol 15:215–229. https://doi.org/10.1038/nrcardio.2017.189
Kivimäki M, Vahtera J, Pentti J, Ferrie JE (2000) Factors underlying the effect of organisational downsizing on health of employees: longitudinal cohort study. BMJ 320:971–975
Kivimäki M, Honkonen T, Wahlbeck K et al (2007) Organisational downsizing and increased use of psychotropic drugs among employees who remain in employment. J Epidemiol Community Heal 61:154–158. https://doi.org/10.1136/jech.2006.050955
Kjekshus LE, Bernström VH, Dahl E, Lorentzen T (2014) The effect of hospital mergers on long-term sickness absence among hospital employees: a fixed effects multivariate regression analysis using panel data. BMC Heal Serv Res 14:50. https://doi.org/10.1186/1472-6963-14-50
Möller J, Theorell T, De Faire U et al (2005) Work related stressful life events and the risk of myocardial infarction. Case-control and case-crossover analyses with the Stockholm heart epidemiology programme (SHEEP). J Epidemiol Community Health 59:23–30. https://doi.org/10.1136/jech.2003.019349
Østhus S, Mastekaasa A (2010) The impact of downsizing on remaining workers’ sickness absence. Soc Sci Med 71:1455–1462. https://doi.org/10.1016/j.socscimed.2010.06.045
Pollard TM (2001) Changes in mental well-being, blood pressure and total cholesterol levels during workplace reorganization: the impact of uncertainty. Work Stress 15:14–28. https://doi.org/10.1080/02678370110064609
Podsakoff PM, MacKenzie SB, Lee JY, Podsakoff NP (2003) Common method biases in behavioral research: a critical review of the literature and recommended remedies. J Appl Psychol 88:879–903. https://doi.org/10.1037/0021-9010.88.5.879
Rod NH, Grønbæk M, Schnohr P et al (2009) Perceived stress as a risk factor for changes in health behaviour and cardiac risk profile: a longitudinal study. J Intern Med 266:467–475. https://doi.org/10.1111/j.1365-2796.2009.02124.x
Richardson S, Shaffer JA, Falzon L et al (2012) Meta-analysis of perceived stress and its association with incident coronary heart disease. Am J Cardiol 110:1711–1716. https://doi.org/10.1016/j.amjcard.2012.08.004
Smaglik P (2005) Job movements. Nature 433:901. https://doi.org/10.1038/nj7028-901a
Snijders T, Bosker R (2012) Multilevel analysis. An introduction to basic and advanced multilevel modeling, vol 2. SAGE Publications, Thousand Oaks
Statistics Denmark (2019) Fuldtidsledige efter område, personer, pct, højeste fuldførte uddannelse, alder og køn. http://www.statistikbanken.dk/AUL08 Accessed 27 Mar 2019.
Theorell T, Oxenstierna G, Westerlund H et al (2003) Downsizing of staff is associated with lowered medically certified sick leave in female employees. Occup Environ Med 60:E9. https://doi.org/10.1136/oem.60.9.e9
Vahtera J, Kivimäki M, Pentti J (1997) Effect of organisational downsizing on health of employees. Lancet 350:1124–1128. https://doi.org/10.1016/S0140-6736(97)03216-9
Vahtera J, Kivimäki M, Pentti J et al (2004) Organisational downsizing, sickness absence, and mortality: 10-town prospective cohort study. BMJ 328:555. https://doi.org/10.1136/bmj.37972.496262.0D
Acknowledgements
This work was supported by the Danish Working Environment Research Fund [13-2015-03]. JHJ thanks University Copenhagen, Julie Von Müllens Fond, Else and Mogens Wedell-Wedellsborgs Fond, and the Graduate School of Public Health (at University of Copenhagen) for their financial contribution to his stay as a visiting researcher in Department of Social and Behavioral Sciences at Harvard T.H. Chan School of Public Health during this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no potential conflict of interest.
Ethical standards
The Capital Region of Denmark approved the data handling for the present study [BFH-2016-020]. This study complies with the standards of the Regional Ethics Committee. The Regional Ethics Committee stated that ethical approval or informed consent were not required for this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Jensen, J.H., Flachs, E.M., Skakon, J. et al. Work-unit organizational changes and risk of cardiovascular disease: a prospective study of public healthcare employees in Denmark. Int Arch Occup Environ Health 93, 409–419 (2020). https://doi.org/10.1007/s00420-019-01493-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00420-019-01493-6