Abstract
Purpose
The effort–reward imbalance (ERI) model includes extrinsic and intrinsic aspects of work stress. The single components, ERI and overcommitment (OC), are known to be associated with mental health. The aim of this study was to test whether OC is a mediator of the association between ERI and mental health.
Methods
Longitudinal analyses were conducted using data from the Third German Sociomedical Panel of Employees on German employees aged 40–54 years. The short version of the ERI questionnaire was used to measure ERI and OC at baseline (2013). Outcomes were mental health problems and self-rated mental health (5-Item Mental Health Inventory) in 2015. Multivariate regressions were conducted controlling for sociodemographics, health-related behaviour, job-related aspects, and mental health at baseline.
Results
A total of 912 men and 1148 women were included in the final analysis. Baseline OC was positively associated with follow-up mental health problems and negatively with self-rated follow-up mental health. While there was no direct effect of ERI on mental health, ERI affected mental health problems (b = 0.14; 95% CI 0.03 to 0.25) and self-rated mental health (b = − 1.15; 95% CI − 1.79 to − 0.57) indirectly through OC.
Conclusions
OC was associated with reduced mental health. There was no association between ERI and mental health that was independent of OC. OC could therefore be interpreted as a mediator between ERI and mental health. Future studies are needed to test the causality of this association.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Psychosocial working conditions are a major determinant of mental health (Bonde 2008; Netterstrøm et al. 2008; Siegrist 2008; Nieuwenhuijsen et al. 2010; Theorell et al. 2015; Rugulies et al. 2017). In the past decades, research has paid a lot of attention to extrinsic stressors such as work load, time pressure, or aspects of organisational structures as represented by the demand–control model (Karasek and Theorell 1990) or the model of organisational injustice (Elovainio et al. 2002). In this respect, the model of effort–reward imbalance (ERI) (Siegrist 1996) has to be distinguished from other theoretical concepts, as it incorporates person-related, intrinsic stressors alongside work-related, extrinsic factors in explaining health-adverse effects of working conditions.
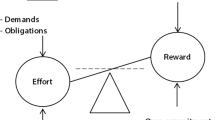
At the core of the ERI model (Siegrist 1996; Siegrist et al. 2009) lies the assumption that reciprocity is expected in the employer–employee relationship. Accordingly, the working contract is considered as an exchange of efforts delivered by the employee for rewards provided by the employer. Efforts are determined by work load, time pressure, and frequent interruptions at work. Ideally, these strains are balanced by rewards such as an adequate salary, esteem by colleagues and superiors, career opportunities, and job security. However, if efforts are regarded to outweigh the received rewards, negative emotions are elicited in those exposed. According to the model, feelings of being treated unfairly and a lack of adequate appreciation cause alterations in physiological strain reactions. If sustained over a long period, an ERI may thus manifest itself in adverse health conditions.
This extrinsic hypothesis has been investigated extensively for different health outcomes (Chandola et al. 2006; Rugulies and Krause 2008; Kivimäki and Siegrist 2016; Dragano et al. 2017; Rugulies et al. 2017). Regarding mental health, evidence is best for the association of ERI with depressive symptoms (Siegrist 2008; Theorell et al. 2015; Rugulies et al. 2017).
A distinctive feature of the ERI model is the integration of the concept of overcommitment (OC) as an intrinsic aspect alongside the extrinsic stressor (i.e. ERI). The model thus acknowledges individual differences in the perception and development of health-adverse working conditions. People who are overcommitted to their work are attributed an exaggerated motivation to expose themselves to demanding work (Siegrist et al. 2004). OC was hypothesised to be an independent predictor of adverse health (Siegrist et al. 2004) which could be confirmed for impaired mental health in several prospective studies (Siegrist and Li 2016).
Siegrist originally proposed strongest effects on health if ERI and OC are present simultaneously, linking ERI and OC in an interaction hypothesis (Siegrist et al. 2004). However, the latest systematic review by Siegrist and Li (2016) states that results concerning this interaction are inconsistent, with a majority of studies failing to support the hypothesis. With regard to the psychological content of the concept, the original elaboration leaves room for divergent interpretation. The concept of OC was introduced by Siegrist as a ‘personal pattern of coping with work demands’ (Siegrist and Marmot 2004, p. 1467) and can, therefore, be interpreted as a coping strategy when faced with extrinsic stressors such as ERI. Hence, it is logical to understand OC as a mediator between ERI and health, as it has recently been suggested in an editorial by Theorell (2017).
The ERI model has been tested in numerous studies but the intrinsic component of the ERI model has received far less attention in research compared to the extrinsic component (van Vegchel et al. 2005; Siegrist and Li 2016). Therefore, we lay our focus on the concept of OC. First, we tested separate associations of ERI and OC with mental health. Second, we examined whether OC was a mediator of the association of ERI with mental health.
Methods
Study design
Data were derived from the Third German Sociomedical Panel of Employees (GSPE-III) (Bethge et al. 2015). The GSPE-III is an ongoing, large-scale cohort study designed to identify occupational and personal risks affecting work ability and participation in working life in workers with health impairments as these are workers with a high risk to retire early. A total survey sample of 10000 was randomly drawn out of the register of the Federal German Pension Insurance Agency in 2013. Sampling was restricted to persons aged 40–54 who had previously received sickness benefits. Men and women were drawn separately to attain equal sample sizes. Data were collected by postal surveys, with the first survey taking place in 2013. A second survey in 2015 was only executed on participants of the baseline survey who expressed their explicit consent to follow-up. Exposure to ERI and OC as well as all covariates were assessed only at baseline. Indicators of mental health were assessed in both surveys. The study was approved by the ethics committee at Hannover Medical School and the data protection commissioner of the German Pension Insurance Agency.
Measures
Effort–reward imbalance and overcommitment
ERI and OC were assessed using the short measure (16-item) of the ERI questionnaire (Siegrist et al. 2009). Three of the items assess the efforts invested in terms of work load, time pressure, and disturbances/interruptions, and seven of the items assess rewards obtained in terms of salary, esteem, career opportunities, and job security. Responses are 4-point scaled. The effort–reward ratio (ERR) was calculated as the ratio of the total effort and reward scores using a correction factor to adjust for the different number of items (Siegrist et al. 2004). A higher ERR indicates a greater imbalance between efforts and rewards. OC was assessed with six 4-point scaled items. Higher OC scores indicate a greater commitment to work (Siegrist et al. 2009). We used continuous variables of ERR and OC in our analyses.
Mental health
Mental health problems (e.g. depression, anxiety, chronic sleep disturbances, emotional fatigue) diagnosed by a physician within the last 12 months were assessed by self-report and employed as a binary indicator (at least one diagnosis; no mental health problem) of reduced mental health (Ilmarinen 2007).
Self-rated general mental health was measured with the subscale of the German version of the 36-Item Short Form Health Survey (SF-36) (Morfeld et al. 2011). Participants were asked to indicate on a 6-point scale how often in the last 4 weeks they felt (1) nervous, (2) down in the dumps, (3) calm and peaceful, (4) downhearted, blue or (5) happy. Answers were summed up and transformed to build a final score with values between 0 and 100. Higher scores indicate better mental health.
Covariates
Besides sex and age, educational level, stable partnership (yes; no) and social support were included in all analyses as relevant variables. Level of education was categorised as low, medium, and high based on the highest graduation achieved in school education. Social support was assessed using the Oslo 3-Item Social Support Scale (Kroll and Lampert 2011). Furthermore, physical exercise (less than 2 h/week; at least 2 h/week), cigarette smoking (active smoker; non-smoker) and body mass index (BMI ≥ 30 kg/m2; BMI < 30 kg/m2) were included in the analyses as indicators of health-related behaviour. Physical job demands, determined by the frequency of having to handle heavy weights (Slesina 1987), and size of enterprise (< 50 employees; ≥ 50 employees) (The Commission of the European Communities 2003) were selected as relevant occupational confounders. The latter variable was dichotomised using 50 employees as a threshold to differ between small and medium-sized to large enterprises. Smaller enterprises may be characterised by closer relationships, but also have less occupational health support.
Statistical analysis
Characteristics of the study population were reported using descriptive statistics. Associations between ERI or OC and mental health were estimated by multivariate analyses, using logistic regression models for the binary outcome measure and linear regression models for self-rated mental health. Results are shown as unstandardised regression coefficients (b) or odds ratios (OR), respectively, with corresponding 95% confidence intervals (95% CI).
A three-model approach was used to test the associations between work stress characterised by ERI or OC and mental health. First, ERR and OC were introduced in separate models estimating the distinct total effects of the extrinsic and intrinsic components on the dependent variables. In the full model, independent effects of ERR and OC were estimated. All analyses were adjusted for baseline mental health, sociodemographic variables, health-relevant behaviour, and occupational variables. In supplementary analyses, we restricted our sample to people without baseline mental health problems and people with good baseline mental health (self-rated mental health at least 50 points). We also tested interactions of ERR and sex and OC and sex to clarify if gender affected the effect of either ERR or OC. In case of significant interaction terms stratified analyses were planned.
To test whether the effect of ERI on mental health was mediated by OC, mediation analyses were performed for the dependent variables. As recommended by Preacher and Hayes (2008), confidence intervals for direct and indirect effects of ERR were estimated using the bootstrap method (5000 samples). All calculations were performed using IBM SPSS Statistics Version 22.0. The SPSS Macro PROCESS Version 2.15 was used for the mediation analysis (Hayes 2013a).
Results
Participants
The flow of participants is shown in Fig. 1. The response rate at baseline was 33.3%. At follow-up 2 years later, 67.8% of questionnaires were returned. Unemployed participants or those with missing values on employment at baseline or follow-up were excluded from all further analyses. The sample eligible for longitudinal analysis comprised 912 men and 1148 women (see Fig. 1). There were small differences between responders and non-responders. Non-responders were more likely to be male and slightly older than baseline responders. Non-responders of follow-up had a lower educational level compared to participants.
Sample characteristics
The mean age of the sample was 48.1 years (SD = 4.0), and 55.7% of participants were women. The mean ERR was 1.37 (SD = 0.57), with men showing slightly higher levels of ERR (see Table 1). OC was equally distributed between men and women, with a mean score of 15.3 (SD = 4.0). At least one mental health problem diagnosed by a physician within the last 12 months was stated by 29.8% at baseline and by 28.4% at follow-up. Mean self-rated mental health was 64.8 (SD = 21.0) at baseline and 64.4 (SD = 20.7) at follow-up.
Predicting mental health
In separate analyses, OC and ERR were associated with higher OR for mental health problems (see Table 2). When introduced simultaneously in the fully adjusted model, only OC remained a significant predictor for mental health problems. The ERR was not associated with mental health problems when OC was included in the regression model.
Analyses restricted to people without baseline mental health problems (N = 1293) resulted in similar findings though the estimate of ERR was not significantly greater than 1 in the first model. Neither the effect of ERR nor OC was moderated by sex.
When introduced separately in regression analysis, OC was a significant predictor of self-rated mental health, whereas ERR was not (see Table 3). An increase in OC was associated with slightly reduced mental health at follow-up, independent of sociodemographic variables, health-related behaviour, occupational variables, and baseline mental health. Furthermore, OC remained a significant predictor in the fully adjusted model that included both components of the ERI model.
Analyses restricted to people with good baseline mental health (self-rated mental health at least 50 points, N = 1359) resulted in similar findings though the estimates were larger (results not shown). Neither the effect of ERR nor OC was moderated by sex.
OC mediating the effect of ERI on mental health
Results of the mediation analyses for both mental health outcomes supported the hypothesis that the association between ERI and mental health is mediated by OC (see Fig. 2). ERR and OC were positively associated, indicating that a greater ERI is associated with higher OC. In turn, higher OC was associated with a greater risk of developing mental health problems and reduced self-rated mental health. While there was no direct association between ERR and mental health, mediation analyses showed significant indirect effects of ERR on both mental health outcomes mediated by OC.
Discussion
This study used data from the GSPE-III to study the associations of work- and person-related work stress with mental health. Based on the ERI model, we hypothesised that ERI and OC are independent risk factors for reduced mental health. Furthermore, we hypothesised that OC mediated the association between ERI and mental health. To our knowledge, this has not been tested before.
To summarise the main findings, OC but not ERI proved to be an independent risk factor for reduced mental health. Moreover, mediation analysis showed that there was an indirect effect of ERI on mental health, mediated by the coping pattern of OC.
Our findings related to the adverse effect of OC are in line with studies that analysed the effects of OC on mental health. In prospective studies, OC was shown to be associated with reduced mental health functioning (Wahrendorf et al. 2012), clinically relevant anxiety and depression (Buddeberg-Fischer et al. 2008), sleep disturbances (Ota et al. 2009), and mental fatigue (Sembajwe et al. 2012).
Our finding of a lacking direct effect of ERI, however, may be surprising as many prospective studies have previously shown negative effects of ERI on various mental health outcomes (Kivimäki et al. 2007; Buddeberg-Fischer et al. 2008; Siegrist et al. 2012; Wang et al. 2012; Rugulies et al. 2013; Juvani et al. 2014). Possibly, the follow-up interval was too long to record significant effects of ERI on mental health. A small prospective study by Shimazu and de Jonge (2009) found significant effects of ERI on psychological distress and physical complaints in male blue-collar workers after 1 year but not after 2 years. In contrast, in a large Danish cohort study, high ERI predicted the onset of severe depressive symptoms even after a 5-year time interval (Rugulies et al. 2013).
It has to be considered, though, that all of the above-cited studies that reported significant effects of ERI on mental health differed from our study in one crucial feature: they did not include OC as a covariate in their analyses. Accordingly, in our study ERI was a significant predictor of mental health problems when OC was not included in the analysis. However, this association did not remain significant when OC was introduced into the analysis as a covariate, and there was a clear reduction of the association of ERI and mental health problems. Of course, OC could be recognised to be a confounder. However, according to Rothman et al. (2008), a factor that is considered to be a consequence of an exposure should not be viewed as a confounding variable.
Since our mediation model is based on the assumption of causality, the directions of the associations have to be questioned. We proposed ERI to be a predictor of OC on the grounds of theoretical thoughts. OC was described as a coping strategy (Siegrist and Marmot 2004) and can be understood therefore as a reactive behaviour aimed at overcoming certain stressors experienced by the individual. Our mediation model is supported by evidence concerning psychological recovery resources. The ability to psychologically detach from work-related problems is considered a relevant recovery resource (Sonnentag et al. 2010). There is a small number of studies that have found evidence for psychological detachment mediating associations between job stressors and well-being (Sonnentag and Fritz 2015). These findings support our mediation model because the concept of OC shows similarities to the stressor-detachment model with the highly overcommitted also being characterised by impaired psychological detachment from work-related problems.
The ERI questionnaire that was used in this study assesses OC with six items, of which five ask for abilities to withdraw from work obligations (Siegrist et al. 2004), for example ‘When I get home, I can easily relax and “switch off” work’ (Siegrist et al. 2009, p. 1012). Originally the concept of OC was depicted as an ‘excessive work-related commitment’ (Siegrist et al. 2004, p. 1485). However, the original questionnaire assessing OC has been modified to an extent that it now rather seems to capture an inability to withdraw from work (Schirmer 2015). It is reasonable that stress created by an ERI would impede detachment from work obligations, leading to higher scores of OC.
Contradictory findings have recently been published by Feldt et al. (2016), who found OC to be a significant predictor of ERI among a sample of predominantly young males working in technical fields. These results would encourage a reversal of predictor and mediator in our model. This idea stems from theoretical considerations that overcommitted behaviour contributes to a mismatch of efforts and rewards and thus increases the risk of experiencing ERI (Siegrist 2005).
As exposure was only assessed once at baseline, we could not test the direction of the associations. Thus, due to these relevant limitations in the study design we cannot draw any conclusions to the causality of our proposed model. It seems most likely that work- and person-related components of the model are associated in a reciprocal relationship. Therefore, future studies using at least a three-point study design are needed to gain a better understanding of the direction of associations.
A particular strength of this study is its prospective study design, which includes a large study sample. Moreover, the use of validated measures to assess work stress and analysis of continuous variables of ERI and OC facilitate the comparability of study results. Despite these strengths, the following limitations need to be considered when interpreting the study results.
First, the response rate in the baseline survey was rather low. Baseline responders and non-responders differed in sex and age, although these effects were very small. Due to limited data on baseline non-responders, a possible bias from selective participation cannot be ruled out.
Second, data on doctor-diagnosed mental health problems were collected using self-report questionnaires rather than validated diagnostic instruments. Therefore, it remains unclear whether participants’ statements are based on clinically verified diagnoses. Because the item was constructed as a summary measure, we also cannot discriminate among different kinds of mental health problems.
Third, assessments with self-report are prone to reporting bias caused by certain personality characteristics, such as a tendency to respond negatively. Since both risk factors and mental health indicators were assessed by self-report, this could result in overestimation of associations, especially when analysing cross-sectional data (Theorell and Hasselhorn 2005). Therefore, we report only results of longitudinal analyses. To control for the influence of reduced mental health, we adjusted for baseline mental health. Analyses were also conducted including only those without mental health problems or a higher mental health index at baseline. The results did not differ substantially from the results presented above including baseline mental health as a confounder (results are available on request).
Fourth, measurement of work stress was restricted to a single-point measurement at baseline. Therefore, we could not capture duration of and changes in exposure to work stress in the interval between the two surveys nor could we analyse the causality of our mediation model. Since it has been reported that exposure to continuous or increasing work stress is associated with greater adverse health effects than decreasing work stress (Buddeberg-Fischer et al. 2008; Feldt et al. 2013), results could have been influenced in both directions. On the one hand, participants experiencing a reduction in work stress due to job changes or reorganisation procedures in between surveys might report better mental health at follow-up. Given associations between exposure to work stress and mental health, this would cause reduced effect measures for the stated association. On the other hand, overestimation of effect sizes could be the consequence of an increase in work stress after baseline measurement.
Fifth, our study sample included workers with health impairments. Risk factors may differ in workers with already existing or earlier health impairments and healthy workers. Workers with health impairments may be in particular vulnerable to work stressors. Though this limits the generalisability of our findings, it does not compromise the relevance of our findings for occupational health physicians dealing with workers with health impairments. Our findings indicate that OC is a risk factor in these workers. Moreover, our sample was of a certain age group. It has been argued that the adverse health effects of work stress might be more pronounced at a younger age (Kivimäki et al. 2002; Chandola et al. 2008). Limited generalisation is further determined by drawing a study sample from the register of the Federal German Pension Insurance Fund. The study population is predominantly composed of non-manual workers with a higher educational level. The adverse health effects of work stress have been found to be stronger among manual compared to non-manual workers (Sverke et al. 2002). Stronger effects have also been reported for a lower occupational grade or a lower educational level (Wege et al. 2008; Rugulies et al. 2013).
Sixth, there was no significant total effect of ERI on self-rated mental health, and it could be argued that it is irrelevant to test OC as a mediator of this non-significant association. However, it has been stated that a total effect of the predictor on the outcome under study is not a prerequisite for mediation analysis (Hayes 2013b). Therefore, we did not consider it an obstacle for mediation analysis that there was no total effect of ERI on self-rated mental health.
Conclusion
In conclusion, OC was an independent predictor of impaired mental health, while ERI affected mental health only indirectly through OC. Although we cannot draw any conclusions on the causality of the association, these results support the interpretation of OC as a mediator between ERI and mental health. As research on the interplay of work- and person-related components of the ERI model is scarce, our study adds to the existing research by offering a new interpretation of the concept of OC. The results provide new perspectives for prevention programmes aimed at reducing work-related mental health problems. Recovery resources and skills that enable working people to detach from and limit their emotional involvement in work-related problems need to be part of effective prevention programmes.
Abbreviations
- BCa CI:
-
Bias-corrected bootstrap confidence interval
- BMI:
-
Body mass index
- ERI:
-
Effort–reward imbalance
- ERR:
-
Effort–reward ratio
- GSPE-III:
-
Third German Sociomedical Panel of Employees
- OC:
-
Overcommitment
- SF-36:
-
36-item Short Form Health Survey
References
Bethge M, Spanier K, Neugebauer T, Mohnberg I, Radoschewski FM (2015) Self-reported poor work ability—an indicator of need for rehabilitation? A cross-sectional study of a sample of German employees. Am J Phys Med Rehabil 94:958–966
Bonde JPE (2008) Psychosocial factors at work and risk of depression: a systematic review of the epidemiological evidence. Occup Environ Med 65:438–445
Buddeberg-Fischer B, Klaghofer R, Stamm M, Siegrist J, Buddeberg C (2008) Work stress and reduced health in young physicians: prospective evidence from Swiss residents. Int Arch Occup Environ Health 82:31–38
Chandola T, Brunner E, Marmot M (2006) Chronic stress at work and the metabolic syndrome: prospective study. BMJ 332:521–525
Chandola T, Britton A, Brunner E, Hemingway H, Malik M, Kumari M, Badrick E, Kivimaki M, Marmot M (2008) Work stress and coronary heart disease: what are the mechanisms? Eur Heart J 29:640–648
Dragano N, Siegrist J, Nyberg ST, Lunau T, Fransson EI, Alfredsson L, Bjorner JB, Borritz M, Burr H, Erbel R et al (2017) Effort–reward imbalance at work and incident coronary heart disease: a multicohort study of 90,164 individuals. Epidemiology 28:619–626
Elovainio M, Kivimäki M, Vahtera J (2002) Organizational justice: evidence of a new psychosocial predictor of health. Am J Public Health 92:105–108
Feldt T, Huhtala M, Kinnunen U, Hyvönen K, Mäkikangas A, Sonnentag S (2013) Long-term patterns of effort–reward imbalance and over-commitment: Investigating occupational well-being and recovery experiences as outcomes. Work Stress 27:64–87
Feldt T, Hyvönen K, Mäkikangas A, Rantanen J, Huhtala M, Kinnunen U (2016) Overcommitment as a predictor of effort–reward imbalance: evidence from an 8-year follow-up study. Scand J Work Environ Health 42:309–319
Hayes AF (2013a) Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. Guilford Press, New York
Hayes AF (2013b) Miscellaneous topics in mediation analysis. In: Little TD (ed) Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. Guilford Press, New York, pp 165–204
Ilmarinen J (2007) The work ability index (WAI). Occup Med 57:160
Juvani A, Oksanen T, Salo P, Virtanen M, Kivimäki M, Pentti J, Vahtera J (2014) Effort–reward imbalance as a risk factor for disability pension: the Finnish Public Sector Study. Scand J Work Environ Health 40:266–277
Karasek R, Theorell T (1990) Healthy work. Stress, productivity, and the reconstruction of working life. Basic Books, New York
Kivimäki M, Siegrist J (2016) Work stress and cardiovascular disease: reviewing research evidence with a focus on effort–reward imbalance at work. In: Siegrist J, Wahrendorf M (eds) Work stress and health in a globalized economy. Springer International Publishing, New York, pp 89–101
Kivimäki M, Leino-Arjas P, Luukkonen R, Riihimäki H, Vahtera J, Kirjonen J (2002) Work stress and risk of cardiovascular mortality: prospective cohort study of industrial employees. BMJ 325:857
Kivimäki M, Vahtera J, Elovainio M, Virtanen M, Siegrist J (2007) Effort–reward imbalance, procedural injustice and relational injustice as psychosocial predictors of health: complementary or redundant models? Occup Environ Med 64:659–665
Kroll LE, Lampert T (2011) Unemployment, social support and health problems: results of the GEDA study in Germany, 2009. Dtsch Ärztebl Int 108:47–52
Morfeld M, Kirchberger I, Bullinger M (2011) SF-36 deutsche Version des Short form-36 health survey. Hogrefe, Göttingen
Netterstrøm B, Conrad N, Bech P, Fink P, Olsen O, Rugulies R, Stansfeld S (2008) The relation between work-related psychosocial factors and the development of depression. Epidemiol Rev 30:118–132
Nieuwenhuijsen K, Bruinvels D, Frings-Dresen M (2010) Psychosocial work environment and stress-related disorders, a systematic review. Occup Med Oxf Engl 60:277–286
Ota A, Masue T, Yasuda N, Tsutsumi A, Mino Y, Ohara H, Ono Y (2009) Psychosocial job characteristics and insomnia: a prospective cohort study using the Demand-Control-Support (DCS) and Effort–Reward Imbalance (ERI) job stress models. Sleep Med 10:1112–1117
Preacher KJ, Hayes AF (2008) Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods 40:879–891
Rothman KJ, Greenland S, Lash TL (2008) Modern epidemiology, 3rd edn. Lippincott Williams & Wilkins, Philadelphia
Rugulies R, Krause N (2008) Effort–reward imbalance and incidence of low back and neck injuries in San Francisco transit operators. Occup Environ Med 65:525–533
Rugulies R, Aust B, Madsen IEH, Burr H, Siegrist J, Bültmann U (2013) Adverse psychosocial working conditions and risk of severe depressive symptoms. Do effects differ by occupational grade? Eur J Public Health 23:415–420
Rugulies R, Aust B, Madsen IE (2017) Effort–reward imbalance at work and risk of depressive disorders. A systematic review and meta-analysis of prospective cohort studies. Scand J Work Environ Health 43:294–306
Schirmer SM (2015) Validierung der “Overcommitmentskala” des Modells beruflicher Gratifikationskrisen. Dissertation, Philipps-Universität Marburg
Sembajwe G, Wahrendorf M, Siegrist J, Sitta R, Zins M, Goldberg M, Berkman L (2012) Effects of job strain on fatigue: cross-sectional and prospective views of the job content questionnaire and effort–reward imbalance in the GAZEL cohort. Occup Environ Med 69:377–384
Shimazu A, de Jonge J (2009) Reciprocal relations between effort–reward imbalance at work and adverse health: a three-wave panel survey. Soc Sci Med 1982 68:60–68
Siegrist J (1996) Adverse health effects of high-effort/low–reward conditions. J Occup Health Psychol 1:27
Siegrist J (2005) Social reciprocity and health: new scientific evidence and policy implications. Psychoneuroendocrinology 30:1033–1038
Siegrist J (2008) Chronic psychosocial stress at work and risk of depression: evidence from prospective studies. Eur Arch Psychiatry Clin Neurosci 258(Suppl 5):115–119
Siegrist J, Li J (2016) Associations of extrinsic and intrinsic components of work stress with health: a systematic review of evidence on the effort–reward imbalance model. Int J Environ Res Public Health 13:432
Siegrist J, Marmot M (2004) Health inequalities and the psychosocial environment-two scientific challenges. Soc Sci Med 1982 58:1463–1473
Siegrist J, Starke D, Chandola T, Godin I, Marmot M, Niedhammer I, Peter R (2004) The measurement of effort–reward imbalance at work: European comparisons. Soc Sci Med 1982 58:1483–1499
Siegrist J, Wege N, Pühlhofer F, Wahrendorf M (2009) A short generic measure of work stress in the era of globalization: effort–reward imbalance. Int Arch Occup Environ Health 82:1005–1013
Siegrist J, Lunau T, Wahrendorf M, Dragano N (2012) Depressive symptoms and psychosocial stress at work among older employees in three continents. Glob Health 8:27
Slesina W (1987) Arbeitsbedingte Erkrankungen und Arbeitsanalyse: Arbeitsanalyse unter dem Gesichtspunkt der Gesundheitsvorsorge. Enke, Stuttgart
Sonnentag S, Fritz C (2015) Recovery from job stress: the stressor-detachment model as an integrative framework. J Organ Behav 36:72–103
Sonnentag S, Binnewies C, Mojza EJ (2010) Staying well and engaged when demands are high: the role of psychological detachment. J Appl Psychol 95:965–976
Sverke M, Hellgren J, Näswall K (2002) No security: a meta-analysis and review of job insecurity and its consequences. J Occup Health Psychol 7:242–264
The Commission of the European Communities (2003) Commission Recommendation of 6 May 2003 concerning the definition of micro, small and medium-sized enterprises. http://eur-lex.europa.eu/legal-content/EN/ALL/?uri=CELEX:32003H0361. Accessed 23 May 2018
Theorell T (2017) On effort–reward imbalance and depression. Scand J Work Environ Health 43:291–293
Theorell T, Hasselhorn HM (2005) On cross-sectional questionnaire studies of relationships between psychosocial conditions at work and health—are they reliable? Int Arch Occup Environ Health 78:517–522
Theorell T, Hammarström A, Aronsson G, Träskman Bendz L, Grape T, Hogstedt C, Marteinsdottir I, Skoog I, Hall C (2015) A systematic review including meta-analysis of work environment and depressive symptoms. BMC Public Health 15:738
van Vegchel N, de Jonge J, Bosma H, Schaufeli W (2005) Reviewing the effort–reward imbalance model: drawing up the balance of 45 empirical studies. Soc Sci Med 1982 60:1117–1131
Wahrendorf M, Sembajwe G, Zins M, Berkman L, Goldberg M, Siegrist J (2012) Long-term effects of psychosocial work stress in midlife on health functioning after labor market exit—results from the GAZEL study. J Gerontol B Psychol Sci Soc Sci 67:471–480
Wang J, Patten SB, Currie S, Sareen J, Schmitz N (2012) A population-based longitudinal study on work environmental factors and the risk of major depressive disorder. Am J Epidemiol 176:52–59
Wege N, Dragano N, Erbel R, Jockel K-H, Moebus S, Stang A, Siegrist J (2008) When does work stress hurt? Testing the interaction with socioeconomic position in the Heinz Nixdorf Recall Study. J Epidemiol Community Health 62:338–341
Funding
This research was funded by the Federal German Pension Insurance Agency. The funders were not involved in the study design, the collection, analysis and interpretation of the data, the writing of the report, nor the decision to submit the paper for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was approved by the ethics committee at Hannover Medical School (1730–2013) and the data protection commissioner of the German Pension Insurance Agency. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hinsch, D.M., Spanier, K., Radoschewski, F.M. et al. Associations between overcommitment, effort–reward imbalance and mental health: findings from a longitudinal study. Int Arch Occup Environ Health 92, 559–567 (2019). https://doi.org/10.1007/s00420-018-1391-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00420-018-1391-7