Abstract
Purpose
Outdoor workers face elevated and prolonged heat exposures and have limited access to air-conditioned spaces. This study’s overarching research aim is to increase knowledge of municipal worker heat exposure and adaptation practices. The study’s sub-objectives are: (1) quantifying exposure misclassification from estimating personal heat exposure from the official weather station; (2) surveying worker’s knowledge and practices to adapt to extreme heat; and (3) relating heat exposure and adaptation practices to self-reported thermal comfort.
Methods
Participants wore a personal heat exposure sensor over 7 days from June 1st to July 3rd, 2015 in Tallahassee, Florida US. Next, participants confirmed the days that they wore the sensor and reported their daily thermal comfort and heat adaptations. Finally, participants completed an extreme heat knowledge, attitudes, and practices survey.
Results
Some participants (37%) experienced hotter and more humid conditions (heat index > 2) than the weather station. The most common heat adaptations were staying hydrated (85%), wearing a hat (46%), and seeking shade (40%). During work hours, higher temperatures increased the odds (odds ratio: 1.21, 95% confidence interval: 1.03–1.41, p = 0.016) of a participant feeling too hot. Shifting work duty indoors made workers to feel more comfortable (odds ratio: 0.28, 95% confidence interval: 0.11–0.70, p = 0.005).
Conclusion
In hot and humid climates, everyday, heat exposures continuously challenge the health of outdoor workers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The United States of America’s (US) summertime (May–September) rate of heat emergency department visits was 21.5/100,000 people per year over 2006–2010 based on the Agency for Healthcare Research and Quality’s Nationwide Emergency Department Sample (Hess et al. 2014). Certain groups are more vulnerable to heat-related illness including the poor, young children, older adults, people with pre-existing conditions (e.g., heart disease, poor blood circulation, diabetes, chronic obstructive pulmonary disease, and mental illness) or people taking medications that alter thermoregulation (Centers for Disease Control and Prevention and Environmental Protection Agency 2016; Gronlund. 2014; Uejio et al. 2011). Outdoor workers engaged in agriculture, construction, firefighting, manufacturing, military, or resource extraction also face heightened risks (Gubernot et al. 2014; Xiang et al. 2014). Such workers face prolonged heat exposures from outdoor conditions or indoor environments with limited air conditioning or ventilation. Physical labor will further strain the human body by increasing the heart and respiration rate, blood flow, and sweating. There are also economic costs of occupational heat morbidity and mortality, medical treatment, and lost productivity. Although nationwide cost estimates do not exist, these expenses costs the State of Washington $1.9 to 4.6 million USD per year (Washington State Department of Labor and Industries 2008).
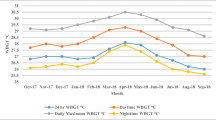
Located within the southeastern US, Florida’s climate can be classified as humid subtropical or tropical (southern Florida). Over the course of the year, the summer season (May–September) is hot and rainy, while the rest of the year (October–April) is warm or mild (winter) and relatively drier (Winsberg 2003). Over 2005–2012, the Florida summer season age-adjusted rates for occupational heat-related emergency department visits were 8.46 visits per 100,000 worker-years (Harduar Morano et al. 2016). Occupational heat-related illness rates were significantly higher in younger adults (age < 35) compared to older adults (age ≥ 35), males compared to females, minorities versus whites, and rural versus non-rural areas (Harduar Morano et al. 2016). Only one field study investigated occupational heat exposure in Florida (Mac et al. 2017). The present study focuses on the northern Florida city of Tallahassee, located in a region with high rates of occupational emergency department visits. Long-term (1981–2010) average monthly summer conditions are hot (average temperature range: 23.5–27.8 °C) and wet (average total rainfall range 88.1–196.3 mm).
This study’s overarching research aim is to increase knowledge of municipal worker heat exposure and adaptation practices. Our first sub-objective quantifies exposure misclassification error from estimating personal heat exposure (PHE) from the official airport weather station (Kuras et al. 2017). Our study’s airport weather station is located nine kilometers from the city center and may be cooler than urban outdoor worker microclimates. Furthermore, workers produce additional heat through exertional activity, cope with waste heat from machines, and/or less efficiently transfer heat through personal protective equipment. After work, laborer’s housing units may be insufficiently cooled and increase cumulative heat exposure and illness risks (Arcury et al. 2015; Quandt et al. 2013). More precise knowledge of PHE will inform occupational heat management strategies that are often based on airport readings.
For example, US institutions recommend decreasing the amount of physical labor and correspondingly increasing rest based on the magnitude and duration of heat exposure. Heat exposure is measured by Wet Bulb Globe Temperature (WBGT) which integrates temperature, humidity, solar radiation, and wind speed. Multiple institutions suggest that only light intensity work should be conducted on days when WBGT exceed 30 °C (American Industrial Hygiene Association 2003; American Conference of Governmental Industrial Hygienists 2014; National Institute for Occupational Safety and Health 2016). In the region, there is also evidence that injuries and heat-related illnesses increase at lower heat exposures (WBGT > 28 °C) (Garzon-Villalba et al. 2016). Managers may not implement the correct strategies if personal heat exposures are higher than airport readings suggest.
The study’s second sub-objective surveyed worker’s knowledge, attitudes, and practices to adapt to extreme heat. Extreme heat can be defined as weather that is much hotter than average for a particular place and time of year (Centers for Disease Control and Prevention and Environmental Protection Agency 2016). In high-income nations, most outdoor heat studies focus on agricultural as opposed to municipal workers (Xiang et al. 2014). Heat exposure, knowledge, and behavioral adaptations vary based on sociodemographics, the class of worker, form of compensation, and gender and job roles. For example, agricultural workers who were paid by the piece instead of a wage were less comfortable taking breaks and face heightened disease risks (Bethel and Harger 2014; Moyce et al. 2017; Spector et al. 2015). Gender and job roles may also structure heat exposure and knowledge (Moyce et al. 2017). In agriculture, men were more likely to pick, prune, irrigate, or operate machinery, while women primarily worked in packing/sorting activities (Stoecklin-Marois et al. 2013).
The final sub-objective examined the relationship between thermal comfort, heat exposure, and heat adaptation practices. A smaller number of studies evaluated the efficacy of interventions to reduce exposure or adapt to extreme heat. Heat-related illness training, providing water and shade, and self-adjustment of workload tended to decrease heat-related morbidity (Bates and Schneider 2008; Stoecklin-Marois et al. 2013). Temporary agricultural workers (H-2A visa) were less likely to use heat prevention strategies (change their work hours or activities, drink more water, take rest breaks in shaded areas) than domestic farmworkers (Mirabelli et al. 2010).
We hypothesize that heat exposure reduction strategies such as staying indoors or rescheduling heavy work may be the most effective at increasing thermal comfort.
Methodology
Study area and population
The study partnered with the city of Tallahassee to recruit participants who primarily worked outdoors or in locations without access to air conditioning. The study was conducted over June 1st to July 3rd, 2015 in Tallahassee, Florida US. Participants from five city departments volunteered in different periods: fleet, public works, and underground utilities (June 1–11), parks and recreation (June 4–18), and solid waste (June 25–July 3). The average daily temperature, relative humidity, and wind speed during these periods were: June 1–11 (25.7 °C, 75.4%, 1.6 km/h); June 4–18 (27.1 °C, 71.6%, 3.1 km/h); and June 25–July 3 (27.1 °C, 77.7%, 4.0 km/h).
Table 1 summarizes the number of participants in each department, their job titles, work location, and access to air-conditioned vehicles or break rooms. More than half of the participants (54%) volunteered from the solid waste department. The most common job title was “solid waste driver” (36%).
Data sources
Participants completed three tasks over a 7-day period (5 work days and two non-work days). The primary task was wearing a PHE sensor. For the second task, participants confirmed the days that they wore the sensor and reported their daily thermal comfort and heat adaptations. The final task was completing an extreme heat knowledge, attitudes, and practices survey. The Florida State University (IRB# 2015.15032) and Florida Department of Health Institutional Review Boards approved this project.
Outdoor heat exposure
The National Oceanic and Atmospheric Association National Center for Environmental Information (2016) provided the Tallahassee Regional Airport outdoor weather conditions. The weather station provided temperature and relative humidity measurements every 5 min and wind speed every hour. For a small fraction of observations (0.5%), missing weather data were linearly interpolated to provide a complete data record.
Personal heat exposure
Portable temperature and humidity sensors (iButton DS 1923) recorded date, time, temperature, and relative humidity every 5 min. Each lightweight sensor weighs 5 g has a circumference of 17.35 mm and height of 6.4 mm. The newly purchased sensor’s temperature and relative humidity accuracy were, respectively, ± 0.5 °C and ± 5% (Maxim Integrated 2017). A carabiner attached the iButton to the participant’s belt or shirt pocket during his/her waking hours. Participants were instructed to place the iButton next to their bed before they slept. Participants were excluded from the analysis if the iButton failed or was not worn during waking hours. Graphing heat exposure over time and the heat exposure logs determined if an iButton failed (e.g., no variation) or likely was not worn and stored in a car (e.g., consistently very high temperatures after work hours). The National Weather Service heat index was calculated from temperature and dewpoint (airport station) and temperature and relative humidity (iButton) using the weathermetrics R package (Anderson et al. 2013).
Personal heat exposure log
The participants completed a short log at the end of each day. Participants reported: whether or not they wore the iButton, time of arrival and departure from work, and hours spent outside. Finally, participants reported their daily thermal comfort (cold, neither cold nor hot, warm, hot, and very hot) and actions taken to reduce heat exposure (stayed indoors, used air conditioning at work, minimized outdoor work, sought out shade, changed daily work routines, or reschedule heavy work). One participant who did not submit a log was excluded from the analysis.
Social survey
The participants completed a survey gauging their knowledge, attitudes, and practices regarding extreme heat. Most of the structured survey questions were adapted from an analogous heat study (Hayden et al. 2011). The survey questions queried previous heat experiences, knowledge of heat warnings, behavior change in response to warnings, and practices to adapt to extreme heat. Participants only reported if they experienced any of the following symptoms during the preceding summer: headache, leg cramps, dry mouth, dizziness, fatigue, excess sweating, fainting, rapid heartbeat, or hallucinations. Respondents also reported basic demographic information (age, gender, race, occupation, and number of years worked outdoors). Finally, participants self-reported their height and weight which were converted to body mass index (body mass/square of body height).
Analysis
Relationships between outdoor weather and personal heat exposure
The study focused on personal and outdoor weather station associations (a) during working hours or (b) averaged across the entire day. Spearman’s rank correlation coefficient quantifies the strength and direction of the association between weather station and iButton temperatures and relative humidities. Correspondingly, scatterplots with a regression smoothing line graphically summarizes these relationship during working hours. For illustration, we also plot one participant’s iButton and weather station temperatures over the course of the work day. To smooth out variability, the temperatures are averaged over six working days (June 1–3, 8–10, 2015) at 5-min intervals.
Social survey, thermal comfort and adaptations
Descriptive statistics summarized participant’s survey answers. The study also analyzed participant’s self-reported daily thermal comfort recorded in the log sheets. The thermal comfort categories were collapsed to “hot” (hot or very hot) and “comfortable” (warm, neither hot nor cold, and cold). A generalized estimating equation repeated measurements analysis adjusted for potentially different subject-specific thermal comfort levels, with odds ratios (OR) and 95% confidence intervals (CI) reported. In other words, the analysis focuses on deviations from each participant’s average thermal comfort over the study period. This small pilot study focused on bivariate relationships between thermal comfort and either heat exposure, demographics, or heat adaptation strategies.
Results
Relationships between outdoor weather and personal heat exposure
Of the initial 50 participants, seven did not complete the study, four lost their iButtons, one iButton malfunctioned, and another four did not wear the sensor during non-work hours. This section focuses on the remaining participants (n = 34). The participants spent at least 40% of their working hours outdoors (Table 2). Parks and recreation, solid waste, and underground utilities spent 60–75% of their time outdoors.
Figure 1 plots the relationship between weather station and personal temperatures and relative humidities during work hours and averaged across each 24-h period. This section discusses both the strength and consistency of the correlation and the difference between mean weather station and personal heat exposure. Spearman’s rank correlation quantified the outdoor weather station and personal monitor associations. At work, there were significant associations between personal and airport temperatures (rho = 0.18, p = 0.02), and relative humidities (rho = 0.16, p = 0.04), but not heat indices (rho = 0.14, p = 0.08). The daily averaged personal and weather station relative humidities (rho = 0.21, p = 0.001) were significant, while temperatures (rho = 0.11, p = 0.10) and heat indices (rho = 0.11, p = 0.12) were not.
Scatterplots illustrating the temperature relationship between the weather station and personal exposures during work hours (a) and averaged across the entire day (c). Analogous relative humidity plots associate weather station and personal levels during work (b) and across the day (d). The plots overlay an ordinary least squares regression line to aid in interpretation
There were notable differences between the magnitude of weather station and personal temperatures. On average, personal temperatures were warmer and more variable than the weather station at work (0.6 °C; standard deviation 3.0 °C) and over the study day (0.2 °C; standard deviation 2.1 °C). In contrast, nearly, all personal humidities were below weather station levels at work (− 15.4%; standard deviation 11.8%) and over the study day (− 19.8%; standard deviation 7.1%). This difference likely reflects time spent in air conditioned and dehumidified environments at home and at work.
Stratified by department, the average fleet, parks and recreation, and solid waste worker heat exposure during working hours were similar to the weather station values (Table 2). The two public work participants always worked outdoors and experienced significantly hotter and humid conditions than the weather station (heat index difference: 5.2, standard deviation: 1.2). Notably, in every division, some participants experienced hotter and more humid conditions than airport readings. For example, 24% of the participant’s temperatures and 37% of the heat indices were respectively greater than 2 °C or 2 heat index units above the weather station.
Figure 2 plots one participant’s average iButton and weather station temperatures over the course of the work day at 5-min intervals. The participant reported working from 07:30 to 17:30. The participant experienced warmer temperatures (~ 26.5 °C) than the weather station during the evening and early morning. During this time, the participant is likely in an indoor temperature controlled environment. At work, the participant also experiences hotter temperature than the weather station. From 12:00–13:00, the participant may be eating lunch in a cooler microclimatic area.
Social survey results
Of the 49 surveys, 41 respondents answered every question and 8 respondents answered some of the questions. Table 3 summarizes demographic information for survey participants. The majority of respondents were male (92%). The most commonly reported race was black (59%) followed by white (39%). The median worker age was 44 years (standard deviation 11.1, range 21–66). According to their body mass index, the majority of respondents were either obese (44%) or overweight (38%).
During the summer, all of the respondents reported that they worked outside at some point during each day. Prior to 2015, the average number of years’ participants had been in their current job was 7.6 (n = 45, standard deviation = 9.1, range 0–32). Many participants reported that they had access to a building (40%) or vehicle with air conditioning at work (81%). Three participants did not have access to any air conditioning during their workday. Ninety-one percent of participants used central air conditioning to cool their homes, while the rest used window air-conditioning unit(s).
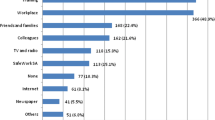
The most frequently reported method of protecting oneself from heat was to drink plenty of liquids (85%), followed by wearing a hat (46%), and seeking shade (40%) (Table 4). Thirty-four respondents (69%) heard a heat warning during the previous summer, and as a result, 56% who heard the warning changed their behavior. Twenty-one percent of participants reported that they had at least one symptoms of heat-related illness in the previous summer. Seven percent reported experiencing symptoms more than one time during the preceding summer.
Thermal comfort and adaptations
The thermal comfort analysis analyzed participants with PHE information who completed daily logs sheets. There were 35 participants who completed 209 log sheets. During a majority of the study days, participants (51%) felt “hot” during the workday, while they were relatively “comfortable” during the other periods. Separate Generalized Estimating Equations related heat exposure, demographics, or heat adaptation strategies to thermal comfort (Table 5).
During work hours, hotter and/or more humid conditions increased the odds of a participant feeling thermally hot. Interestingly, airport readings exhibited a more consistent relationship than personal measurements. Each unit change in weather station temperature (OR 1.21, 95% CI 1.03–1.41, p = 0.016) or heat index (OR 1.14, 95% CI 1.01–1.29, p = 0.027) significantly increased the odds of reporting “hot” conditions. The PHE measurements suggested a consistent but insignificant relationship for temperature (OR 1.09, 95% CI 0.95–1.25, p = 0.19) and heat index (OR 1.05, 95% CI 0.98–1.12, p = 0.14). There were no systematic relationships between daily averaged heat exposure metrics and thermal comfort.
Only one strategy significantly improved thermal comfort. Workers who were able to shift some work duties indoors were strongly protected against thermally uncomfortable conditions (OR 0.28, 95% CI 0.11–0.70, p = 0.005). All other strategies did not significantly alter thermal comfort. Sociodemographic characteristics also did not alter self-reported comfort.
Discussion
The study’s first objective quantified exposure misclassification from estimating PHE from outdoor weather stations. During the study period (early summer), the airport station provided a reasonable estimate of outdoor worker heat exposure. Workers likely experienced relatively hotter temperatures when working outdoors and cooler temperatures inside of air-conditioned vehicles or buildings. A shorter study of older adults (age > 65) in Baltimore, MD also found that PHE was similar to weather station observations (Basu and Samet 2002).
The weather station provides a somewhat accurate but imprecise measure of personal temperature exposures. By comparison, weather station humidity levels are almost uniformly higher than personal humidity readings. In the study area, temperature may be reasonably approximated by weather station observations. City managers would ideally manage heat exposure based on WBGT. Since the U.S. weather service does not collect and report WBGT, it may be approximated from temperature and relative humidity by conservatively presuming full sunlight and light wind conditions (Korey Stringer Institute 2017).
The most prevalent work-related heat adaption was drinking plenty of fluids. By comparison, increased hydration is a less common (43–58%) strategy used by the general public (Hayden et al. 2011; Sheridan 2007). US federal guidelines recommend outdoor workers drink ~ 0.25 L of cold (< 15 °C) water every 15 to 20 min (National Institute for Occupational Safety and Health 2016). During periods of prolonged outdoor work (> 2 h), some guidelines suggest that workers should also be provided with low calorie drinks containing electrolytes (Department of Defense (US) 2003; Montain and Cheuvront 2008). There is some evidence that workers that consume soda instead of water are more likely to report heat-related illness (Fleischer et al. 2013). Some workers (38–46%) wore a hat or light/loose-fitting clothing to cope with heat exposures. Agricultural workers who wore a hat or worked in dry clothing were less likely to experience heat-related illness symptoms (Arcury et al. 2015; Kearney et al. 2016). Work functions may constrain the types of clothing laborers could wear. Federal guidelines recommend employers provide protective clothing and equipment when heat exposure limits are surpassed.
Smaller proportions of workers could reschedule heavy work activities (27%) to cooler times of the day. This finding is comparable to agricultural workers in North Carolina (30–43%) but lower than agricultural workers in southern Georgia (62–64%) (Fleischer et al. 2013; Mirabelli et al. 2010). Road construction and repair crews may shift their work to the early morning to minimize traffic disruptions and air pollution and extreme heat exposures (Elrahman 2008). Future research should investigate the feasibility and trade-offs of shifting working hours to reduce heat exposure.
Sixty-eight percent of the present study’s participants recall hearing about the previous summer’s only extreme heat warning (August 22nd, 11:00–20:00 EDT). The worker’s heat warning awareness was slightly lower than other studies of the general public (80–93%) (Hayden et al. 2011; Sheridan. 2007). In New York city, older adults (age > 65), in fair or poor health, without air conditioning were also less aware of heat warnings (Lane et al. 2014). People working in hot conditions may not seek out weather information if they have limited agency to adapt to extreme heat. Consistent with other studies, about half of respondents (56%) who heard about a heat warning changed their behavior. About one in five workers reported experiencing one or more heat-related symptoms during the previous summer. This illness rate is lower than the rate reported by convenience samples of farmworkers (33–79%) (Arcury et al. 2015; Bethel et al. 2017; Fleischer et al. 2013; Kearney et al. 2016; Mirabelli et al. 2010; Spector et al. 2015).
In the present study, workers who could conduct their work indoors were less likely to report thermal discomfort. There are no U.S. federal workplace safety standards for outdoor heat exposure. State-level (California and Washington) regulations require heat-related illness training, providing potable water, rest, shade, and encourage hydration. Regulations that require training notably increased heat knowledge and adaptations in California but only modestly increased knowledge in Washington (Fleischer et al. 2013; Stoecklin-Marois et al. 2013). Some high-income nations (e.g., Japan, Australia, European Union members) also regulate occupational heat exposure (Xiang et al. 2014).
Individual health status and experience working in extreme heat may influence heat-related risks. Military members who were overweight and/or had lower fitness were more likely to experience heat-related illness (Bedno et al. 2014). Over 80% of the study, participants were overweight or obese based on BMI from self-reported height and weight. This proportion is even higher than the county-wide adult rate of 63% (Leon County Health Department 2011). Self-reported BMI can be considered a conservative estimate, since most studies suggest people under report their BMI (Connor Gorber et al. 2007). Thus, working outdoors does not necessarily translate into decreased obesity rates. Although this study did not find a relationship, there is evidence that workers with more experience may develop effective heat coping strategies (Moyce et al. 2017; Spector et al. 2015). Some participating departments were primarily composed of workers of one race. For example, almost all of the solid waste employees were Black. Our study, therefore, could not disentangle the effect of race from the city department.
We briefly review “best practices” for occupational hygienists to manage extreme heat exposure (National Institute for Occupational Safety and Health 2016).
-
Prior to working in a hot environment, employers should provide workers and supervisors with health and safety training which emphasizes:
-
Recognizing heat-related illness symptoms and first aid procedures such as:
-
Heat exhaustion symptoms: headache, nausea, dizziness, weakness, irritability, thirst, heavy sweating, elevated boy temperature, and decreased urine output.
-
Heat stroke symptoms: confusion, altered mental status, slurred speech, loss of consciousness, hot, dry skin or profuse sweating, seizures, and very high body temperature.
-
First aid: take worker to the clinic (heat exhaustion), emergency room (heat stroke), or call emergency medical service for evaluation and treatment. Someone must stay with the worker until help arrives. Remove the worker from a hot environment, rehydrate, and cool the worker down.
-
-
Encouraging hydration and consuming ~ 0.25 L of cold (< 15 °C) water every 15–20 min.
-
Certain populations are more sensitive to extreme heat such as older adults, people with chronic health conditions (e.g., diabetes, chronic obstructive pulmonary disease), and overweight or obese individuals.
-
Caffeine, alcohol, and prescription medications (e.g., some antidepressants, antihistamines, antipsychotic, high blood pressure, and overactive bladder drugs) also lower heat tolerance.
-
How to care for and use heat-protective clothing and equipment.
-
Training supervisors to monitor weather reports and weather advisories.
-
-
Establishing and enforcing the following policies will also help workers cope with heat:
-
Acclimatization plan to gradually increase worker exposure to hot environments over 1–2 weeks.
-
Limits on the duration and intensity of work based on the total workday heat exposure. Multiple institutions recommend similar heat thresholds (American Industrial Hygiene Association 2003; Tanaka 2007; American Conference of Governmental Industrial Hygienists 2014).
-
Medical monitoring program to prevent and identify heat-related illness early warning signs.
-
Elevated core body temperature is the best metric of heat-related illness and challenges to organ system functioning. PHE may improve upon outdoor weather station measurements, but is still an imperfect proxy of core body temperature (Byrne and Lim 2007; Kalkowsky and Kampmann. 2006). Core temperature measurement devices can be more intrusive and difficult to consistently use. The first study limitation is that it did not account for the iButton’s orientation (toward/away from the body) which may influence the sensor’s response time. This study presumes the sensor’s orientation introduced non-differential error that would be reduced by averaging exposure over the entire work day. Similarly, our study could have more accurately measured indoor/outdoor activity patterns. This information can be inferred from solar radiation monitors, which may be more accurate than self-reported information (Bernhard et al. 2015).
The social survey could also be improved by gathering more specific morbidity information. The survey should have asked participants to report the specific heat-related symptoms and the severity of illness they experienced during the previous summer. Future social surveys could be improved by explicitly asking about worker knowledge of occupational guidelines, the amount of water consumed, and rest to work ratios. To accommodate government and participant schedules, the study was conducted toward the beginning of summer. Repeating the study during the seasonally hottest period (late July–August) may further increase differences between weather station and personal temperatures and increase worker thermal discomfort.
Conclusion
This study documented municipal outdoor worker heat exposures and adaptations practices in consistently hot and humid Northern Florida, US. The first sub-objective quantified exposure misclassification from using an airport weather station to monitor personal heat exposure. Compared to individual exposures, the weather station recorded systematically higher humidities and somewhat similar temperatures. The second sub-objective surveyed workers knowledge, attitudes, and practices to adapt to extreme heat. Nearly all workers adapted to the heat by staying hydrated, while less than half reported wearing a hat or seeking out shade. The final sub-objective associated heat exposure and adaptation practices against self-reported thermal comfort. On hot days, a small proportion of participants (16%) could work indoors instead of outdoors and were more likely to be thermally comfortable. The study results increase knowledge of personal heat exposures and adaptation to strengthen heat management strategies.
References
American Conference of Governmental Industrial Hygienists (ed) (2014) TLVs® and BEIs®: Threshold limit values for chemical substances and physical agents and biological exposure indices. American Conference of Governmental Industrial Hygienists, Cincinnati, OH
American Industrial Hygiene Association (2003) The occupational environment: its evaluation, control, and management. American Industrial Hygiene Association Press, Fairfax
Anderson GB, Bell ML, Peng RD (2013) Methods to calculate the heat index as an exposure metric in environmental health research. Environ Health Perspect 121:1111–1119. https://doi.org/10.1289/ehp.1206273
Arcury TA, Summers P, Talton JW, Chen H, Sandberg JC, Spears Johnson CR, Quandt SA (2015) Heat illness among North Carolina Latino farmworkers. J Occup Environ Med 57:1299–1304. https://doi.org/10.1097/JOM.0000000000000552
Basu R, Samet JM (2002) Relation between elevated ambient temperature and mortality: a review of the epidemiologic evidence. Epidemiol Rev 24:190–202
Bates GP, Schneider J (2008) Hydration status and physiological workload of UAE construction workers: A prospective longitudinal observational study. J Occup Med Toxicol 3:21-6673-3-21. https://doi.org/10.1186/1745-6673-3-21
Bedno SA, Urban N, Boivin MR, Cowan DN (2014) Fitness, obesity and risk of heat illness among army trainees. Occup Med (Lond) 64:461–467. https://doi.org/10.1093/occmed/kqu062
Bernhard MC, Kent ST, Sloan ME, Evans MB, McClure LA, Gohlke JM (2015) Measuring personal heat exposure in an urban and rural environment. Environ Res 137:410–418
Bethel JW, Harger R (2014) Heat-related illness among Oregon farmworkers. Int J Environ Res Public Health 11:9273–9285. https://doi.org/10.3390/ijerph110909273
Bethel JW, Spector JT, Krenz J (2017) Hydration and cooling practices among farmworkers in Oregon and Washington. J Agromedicine doi. https://doi.org/10.1080/1059924X.2017.1318100
Byrne C, Lim CL (2007) The ingestible telemetric body core temperature sensor: a review of validity and exercise applications. Br J Sports Med 41:126–133. (doi: bjsm.2006.026344 [pii])
Centers for Disease Control and Prevention, Environmental Protection Agency (2016) Climate change and extreme heat: what you can do to prepare. EPA 430-R-16-061. Atlanta, GA
Connor Gorber S, Tremblay M, Moher D, Gorber B (2007) A comparison of direct vs. self-report measures for assessing height, weight and body mass index: a systematic review. Obes Rev 8:307–326 (doi: OBR347 [pii])
Department of Defense (US) (2003) Technical bulletin: heat stress control and heat casualty management. TB MED 507/AFPAM:28–152. Departments of the US Army, Navy, and Air Force, Washington, DC
Elrahman O (2008) Night-time road construction operations: synthesis of practice. Transportation Research and Development Bureau, New York State Department of Transportation, Albany, pp 1–13
Fleischer NL, Tiesman HM, Sumitani J, Mize T, Amarnath KK, Bayakly AR, Murphy MW (2013) Public health impact of heat-related illness among migrant farmworkers. Am J Prev Med 44:199–206
Garzon-Villalba XP, Mbah A, Wu Y, Hiles M, Moore H, Schwartz SW, Bernard TE (2016) Exertional heat illness and acute injury related to ambient wet bulb globe temperature. Am J Ind Med 59:1169–1176. https://doi.org/10.1002/ajim.22650
Gronlund CJ (2014) Racial and socioeconomic disparities in heat-related health effects and their mechanisms: a review. Curr Epidemiol Rep 1:165–173. https://doi.org/10.1007/s40471-014-0014-4
Gubernot DM, Anderson GB, Hunting KL (2014) The epidemiology of occupational heat exposure in the United States: a review of the literature and assessment of research needs in a changing climate. Int J Biometeorol 58:1779–1788. https://doi.org/10.1007/s00484-013-0752-x
Harduar Morano L, Watkins S, Kintziger K (2016) A comprehensive evaluation of the burden of heat-related illness and death within the Florida population. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph13060551
Hayden MH, Brenkert-Smith H, Wilhelmi OV (2011) Differential adaptive capacity to extreme heat: a phoenix, Arizona case study. Weather Clim Soc 3:269–280
Hess JJ, Saha S, Luber G (2014) Summertime acute heat illness in US emergency departments from 2006 through 2010: analysis of a nationally representative sample. Environ Health Perspect 122:1209–1215. https://doi.org/10.1289/ehp.1306796
Kalkowsky B, Kampmann B (2006) Physiological strain of miners at hot working places in German coal mines. Ind Health 44:465–473
Kearney GD, Hu H, Xu X, Hall MB, Balanay JA (2016) Estimating the prevalence of heat-related symptoms and sun safety-related behavior among Latino Farmworkers in Eastern North Carolina. J Agromedicine 21:15–23. https://doi.org/10.1080/1059924X.2015.1106377
Korey Stringer Institute (2017) Wet Bulb Globe temperature monitoring. https://ksi.uconn.edu/prevention/wet-bulb-globe-temperature-monitoring/. Accessed 7 Dec 2017
Kuras ER, Bernhard MC, Calkins MM, Ebi KL, Hess JJ, Kintziger KW, Jagger MA, Middel A, Scott AA, Spector JT, Uejio CK, Vanos JK, Zaitchik BF, Gohlke JM, Hondula DH (2017) Opportunities and challenges for personal heat exposure research. Environ Health Perspect
Lane K, Wheeler K, Charles-Guzman K, Ahmed M, Blum M, Gregory K, Graber N, Clark N, Matte T (2014) Extreme heat awareness and protective behaviors in New York City. J Urban Health 91:403–414
Leon County Health Department (2011) Leon County community health improvement plan 2012–2017, pp 1–18
Mac VV, Tovar-Aguilar JA, Flocks J, Economos E, Hertzberg VS, McCauley LA (2017) Heat exposure in Central Florida Fernery Workers: results of a feasibility study. J Agromedicine 22:89–99. https://doi.org/10.1080/1059924X.2017.1282906
Maxim Integrated (2017) iButton. https://www.maximintegrated.com/en/products/digital/ibutton.html. Accessed 28 Feb 2017
Mirabelli MC, Quandt SA, Crain R, Grzywacz JG, Robinson EN, Vallejos QM, Arcury TA (2010) Symptoms of heat illness among Latino farm workers in North Carolina. Am J Prev Med 39:468–471
Montain SJ, Cheuvront SN (2008) Fluid, electrolyte and carbohydrate requirements for exercise. In: Taylor NAS, Groeller H (eds) Physiological bases of human performance during work and exercise. Churchill Livingstone, New York, pp 563–576
Moyce S, Mitchell D, Armitage T, Tancredi D, Joseph J, Schenker M (2017) Heat strain, volume depletion and kidney function in California agricultural workers. Occup Environ Med. (doi: oemed-2016-103848 [pii])
National Institute for Occupational Safety and Health (NIOSH) (2016) Criteria for a Recommended Standard Occupational Exposure to Heat and Hot Environments Revised Criteria 2016:1–192
NOAA National Centers for Environmental Information (2016) Global Historical Climatology Network (GHCN). https://www.ncdc.noaa.gov/data-access/land-based-station-data/land-based-datasets/global-historical-climatology-network-ghcn
Quandt SA, Wiggins MF, Chen H, Bischoff WE, Arcury TA (2013) Heat index in migrant farmworker housing: implications for rest and recovery from work-related heat stress. Am J Public Health 103:e24-6. https://doi.org/10.2105/AJPH.2012.301135
Sheridan SC (2007) A survey of public perception and response to heat warnings across four North American cities: an evaluation of municipal effectiveness. Int J Biometeorol 52:3–15
Spector JT, Krenz J, Blank KN (2015) Risk factors for heat-related illness in Washington crop workers. J Agromedicine 20:349–359. https://doi.org/10.1080/1059924X.2015.1047107
Stoecklin-Marois M, Hennessy-Burt T, Mitchell D, Schenker M (2013) Heat-related illness knowledge and practices among California hired farm workers in the MICASA study. Ind Health 51:47–55
Tanaka M (2007) Heat stress standard for hot work environments in Japan. Ind Health 45:85–90 (doi: JST.JSTAGE/indhealth/45.85 [pii])
Uejio CK, Wilhelmi OV, Golden JS, Mills DM, Gulino SP, Samenow JP (2011) Intra-urban societal vulnerability to extreme heat: the role of heat exposure and the built environment, socioeconomics, and neighborhood stability. Health Place 17:498–507
Washington State Department of Labor and Industries (2008) Outdoor Heat Exposure. Concise Explanatory Statement. Economic Analyses. Heat-Related Illness Small Business Economic Impact Statement. http://www.lni.wa.gov/rules/AO06/40/0640CES.pdf. Accessed 17 July 2017
Winsberg MD (2003) Florida weather. University Press of Florida, Gainesville
Xiang J, Bi P, Pisaniello D, Hansen A (2014) Health impacts of workplace heat exposure: an epidemiological review. Ind Health 52:91–101. (doi: DN/JST.JSTAGE/indhealth/2012-0145 [pii])
Acknowledgements
We acknowledge Dr. Jon Powell, Jennifer Hill, and Katherine Estevez from the city of Tallahassee who helped facilitate this project. We thank employees who participated in the project and Dr. Mary Hayden who shared the extreme heat social survey. Finally, we thank anonymous reviewers whose comments notably improved the manuscript.
Funding
This publication was developed under Assistance Agreement No. (RD #83574901) awarded by the U.S. Environmental Protection Agency to Christopher K. Uejio. The manuscript was also supported by Centers for Disease Control and Prevention grants (EH12-1202; U38-EH000941) and The National Institute for Occupational Safety and Health grant (5U60OH010900-03). It has not been formally reviewed by the EPA. The views expressed in this document are solely those of the authors and do not necessarily reflect those of the EPA. EPA does not endorse any products or commercial services mentioned in this publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Uejio, C.K., Morano, L.H., Jung, J. et al. Occupational heat exposure among municipal workers. Int Arch Occup Environ Health 91, 705–715 (2018). https://doi.org/10.1007/s00420-018-1318-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00420-018-1318-3