Abstract
Despite commonly used for coronary artery bypass surgery, saphenous vein (SV) grafts have significantly lower patency rates in comparison to internal thoracic artery (ITA) grafts, which might be due to the structural characteristics of the vessel wall but also due to differences in oxidative stress adaptation and molecular signaling and regulation. This human post mortem study included a total of 150 human bypass grafts (75 SV grafts and 75 ITA grafts) obtained from 60 patients divided into five groups due to the time period of implantation: group 1: baseline group without grafting; group 2: 1 day; group 3: > 1 day–1 week; group 4: > 1 week–1 month; group 5: > 1 month–1 year. Pieces of 3 mm length were fixed with formaldehyde, dehydrated, wax embedded, cut into sections of 3 µm thickness, and histologically and immunohistochemically examined. Over the whole time period, we observed a lower neointima formation and a better preserved media in ITA grafts with a higher percentage of TNF-α, PDGFR-α, and VEGF-A in nearly all vessel wall layers, a higher amount of MMP-7, MMP-9, EGFR, and bFGF positive cells in SV grafts and a timely different peak not only between ITA and SV grafts but also within the various vessel wall layers of both graft types. Since most of the examined growth factors, growth factor receptors and cytokines are regulated by MAPKs, our results suggest an activation of different pathways in both vessel graft types immediately after bypass grafting.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Coronary artery bypass grafting (CABG) for the treatment of ischemic heart disease is one of the most frequently performed surgical procedures worldwide, and due to the technical advantages the saphenous vein (SV) is still the most used conduit, although long-term studies confirm that internal thoracic artery (ITA) grafts have a higher patency and better outcome than saphenous veins.
Nowadays, the majority of patients receive left ITA grafts to the left anterior descending (LAD) coronary artery and SV grafts or other conduits to the remaining vessels.
Although the ITA has patency rates of 90–95% 10–15 years after CABG, SV graft failure occurs in approximately 40% of grafts 10 years after surgery with significant atheroma in most of the remaining grafts (Schachner 2006).
Vascular remodeling in vessel grafts is thought to be a necessary response for environmental adaption and for compensation of the high wall shear stress (Muto el al. 2010). In short, it is characterized by the development of intimal hyperplasia, vessel wall thickening with deposition of vascular smooth muscle cells (VSMCs) and extracellular matrix especially in the intima.
Because of the arterial pressure and altered shear stress profile and oxidative stress within vessel grafts, endothelial cells (ECs) become activated and damaged or even lost.
Within 1 month after implantation, activated ECs, but also platelets and macrophages, release growth factors, such as platelet-derived growth factor (PDGF), transforming growth factor ß (TGF-ß), epidermal growth factor (EGF), and cytokines (IL-1, IL-6, and IL-8) causing a switch of VSMCs from the “contractile” to the “synthetic” phenotype (Mitra et al. 2006). To proliferate and migrate into the intima, VSMCs must be able to break down intercellular junctions, which is achieved by simultaneously expressing matrix metalloproteinases and their inhibitors. VSMCs in the intima continue to secrete extracellular matrix components, resulting in the narrowing of the bypass graft and eventually culminating in occlusion (Owens 2010).
Because vein graft adaptation after coronary bypass grafting presents similar physiologic characteristics as compared to injured arteries, it has been hypothesized that they share the same underlying mechanism. However, it is likely that vein and arterial graft adaptation have specific and distinct differences in their molecular pathways.
The aim of this human post mortem study was to investigate the molecular differences in SV and ITA grafts over a time period of 1 year after implantation in the coronary artery system.
Materials and methods
Tissue samples
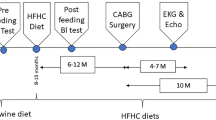
This study is a human postmortem study, examining 150 coronary artery bypass grafts (75 SV grafts and 75 ITA grafts) histologically and immunohistochemically from 60 patients. From each of the 60 patients, one piece of the ITA graft and the SV graft was harvested, additionally from 15 of the 60 patients one piece of native ITA and SV was examined. For the histological and immunohistochemical examination of vein and arterial segments, the informed consent was obtained from next of kin. The ethic regulations on research on human tissues were followed by the participating centers, consistent with the Declaration of Helsinki (1964) and its later amendments.
Histopathology, immunohistochemistry and morphometry
The grafts were divided into five groups (each containing 15 SV grafts and 15 ITA grafts) due to the time period of implantation: group 1: baseline group without grafting (native vessels); group 2: 1 day; group 3: > 1 day–1 week; group 4: > 1 week–1 month; group 5: > 1 month–1 year.
Immediately after autopsy of the heart, small pieces of 3 mm length of the proximal third of the vessels were fixed in formaldehyde, dehydrated, and wax embedded. Afterwards, sections of 3 µm thickness were routinely stained with hematoxylin and eosin (H&E), Elastica van Gieson staining for verifying elastic fibres, Masson’s trichrome staining for the assessment of vessel graft fibrosis and Alcian blue staining for the visualization of acid mucopolysaccharides.
For immunohistochemical investigations the following antibodies were used: anti-α-SMA (mouse monoclonal, Clone 1A4, Code M0851, prediluted, Dakocytomation, Glostrup, Denmark), anti-CD31 (mouse monoclonal, Clone JC70, prediluted, CellMarque™, California, USA), anti-CD3 (rabbit monoclonal, Clone 2GV6, prediluted, Ventana Medical Systems Inc., Arizona, USA), anti-CD20 (mouse monoclonal, CD20cy, Clone L26, Nr. M 0755, dilution 1:1000, DakoCytomation, Glostrup, Denmark), anti-CD163 (Clone MRQ-26, prediluted, Ventana Medical Systems Inc., Arizona, USA), anti-Ki67 (rabbit monoclonal, prediluted, Ventana Medical Systems Inc., Arizona, USA), Cleaved Caspase-3 antibody (rabbit polyclonal, Asp175, dilution 1:200, Cell Signaling Technology Europe B.V., Frankfurt am Main, Germany), anti-collagen IV (mouse monoclonal, Clone CIV22, Nr. M 0785, dilution 1:50, Dakocytomation, Glostrup, Denmark), matrix metalloproteinase-7 (MMP-7) antibody (rabbit polyclonal, ab232737, dilution 1:100, Abcam, Cambridge, UK), matrix metalloproteinase-9 (MMP-9) antibody (rabbit polyclonal, ab38898, dilution 1:1000, Abcam, Cambridge, UK), epidermal growth factor receptor (EGFR) antibody (mouse monoclonal, [EP38Y], ab52894, dilution 1:50, Abcam, Cambridge, UK), basic fibroblast growth factor (bFGF) antibody (rabbit polyclonal, ab8880, dilution 1:1000, Abcam; Cambridge, UK), tumor necrosis factor alpha (TNF-α) antibody (rabbit polyclonal, ab6671, dilution 1:300, Abcam, Cambridge, UK), platelet-derived growth factor receptor alpha (PDGFR-α) antibody (rabbit polyclonal, #3164, dilution 1:100, Cell Signaling Technology Europe B.V., Frankfurt am Main, Germany), platelet-derived growth factor receptor beta (PDGFR-ß) antibody (rabbit monoclonal; #4564, dilution 1:200, Cell Signaling Technology Europe B.V., Frankfurt am Main, Germany), vascular endothelial growth factor A (VEGF-A) antibody (mouse monoclonal, ab1316, dilution 1:1000, Abcam, Cambridge, UK), and transforming growth factor β (TGF-β) antibody (rabbit polyclonal, ab66043, dilution 1:100, Abcam, Cambridge, UK). Provided proof of validation is given on the technical specifications insert.
Immunohistochemistry was performed using the VENTANA BenchMark ULTRA (Ventana Medical Systems Inc., Arizona, USA). First the slides were entparaffinized with EZ Prep Concentrate (10X; Ventana Medical Systems Inc., Arizona, USA). All antibodies except anti-EGFR and anti-collagen IV received heat pretreatment at 95 °C with Ultra Cell Conditioning Solution (ULTRA CC1; Ventana Medical Systems Inc., Arizona, USA). Anti-EGFR and anti-collagen IV received pretreatment with Protease 1 (Ventana Medical Systems Inc., Arizona, USA) at room temperature. The incubation period was 32 min at room temperature for all antibodies except anti-CD31, anti-CD20, and anti-Ki-67, and 24 min at room temperature for anti-CD31, anti-CD20, and anti-Ki-67. At the same time, negative controls were incubated with blocking solution instead of the primary antibody. For visualization the ultraView Universal Alkaline Phosphatase Red Detection Kit (Ventana Medical Systems Inc., Arizona, USA) and ultraView Universal DAB Detection Kit (Ventana Medical Systems Inc., Arizona, USA) were used.
Intimal and media thickness was measured all 30 µm under light microscope (Zeiss Axioplan 2, Carl Zeiss AG, Jena, Germany) with a ProgRes® CF Scan CCD 12.5 M.P. Microscope Camera (JENOPTIK AG, Jena, Germany). Images were acquired with 20× (numerical aperture 0.50) and 60× (numerical aperture 0.75) objective lenses. The software for taking the pictures was the ProgRes® CarpturePro Camera Control Software. The image resolution was 1360 × 1024 Pixel (pixel size of 3.69 × 3.69 µm). Measurements were performed by the software ImageJ for Java (National Institutes of Health, USA). The mean value of each section was regarded as representative.
The degree of inflammation was assessed by a semiquantitative score as follows: 0—no inflammation, 1—mild inflammation, 2—moderate inflammation, 3—intense inflammation.
The occurrence of elastic fibres, vessel wall fibrosis, type IV collagen, and acid mucopolysaccharides was given as percentage of area in the intima, media, and adventitia, the endothelialization was visualized by CD31 and reported as percentage of the whole length of the vessel wall.
MMP-7, MMP-9, EGFR, bFGF, TNF-ɑ, PDGFR-α, PDGFR-ß, VEGF-A, TGF-ß, Ki-67, and caspase 3 positive cells were given as percentage of the whole cell population in the specific vessel wall layer (intima, media, and adventitia) counted in 10 high power fields (HPFs) at 40× magnification.
The number of neutrophil granulocytes, plasma cells, CD3 and CD20 positive lymphocytes, and CD163 positive macrophages was estimated as the percentage of the inflammatory infiltrate. The number of SMA positive cells was counted in 2 high-power fields at 40× magnification and extrapolated to 1mm2.
Statistical analysis
The quantitative data were expressed as mean ± standard error of the mean (SEM). The SPSS for Windows statistical software package (SPSS 22.0; Microsoft, Redmond, WA, USA) was used for analysis. The results of histological and immunohistochemical results of veins and arteries of each group were compared by Student’s t test. A p value of <0.05 was considered statistically significant.
Results
This study included a total of 150 human bypass grafts (75 SV grafts and 75 ITA grafts) obtained from 38 male and 22 female patients. All bypass grafts were patent at the time of harvest.
Intima thickness increased over time in both arterial and venous grafts, but ITA grafts revealed a significantly lower neointima formation compared to SV grafts at the end point of examination in group 5 (71.05 ± 59.74 µm vs. 265.83 ± 202.23 µm; p = 0.04) with a significantly lower number of SMA positive cells (104.28 ± 9.76/ mm2 vs. 478.57 ± 63.62/mm2, p = 0.04) and a thicker and better preserved media (245.21 ± 46.28 µm vs. 119.03 ± 31.57 µm; p = 0.0001) with a significantly higher number of SMA positive cells (850.00 ± 104.88/mm2 vs. 508.33 ± 102.06/ mm2, p = 0.0002; Figs. 1a + b, 2, 3, Supplementary Table 1).
Differences in intima and media thickness, endothelialization, inflammation, apoptosis and proliferation between ITA and SV grafts. a Lower neointima formation and better-preserved media in ITA grafts with b a higher amount of SMA positive cells in the media. c Surprisingly, low endothelialization after bypass grafting in both graft types. d Higher inflammation score in all vessel wall layers of SV grafts. e Similar apoptotic index in ITA and SV grafts with an earlier peak in ITA grafts. f Low Ki-67-proliferation index in both graft types with only a few positive macrophages, leukocytes, and endothelial cells
Elastica van Gieson staining. Significant increase of neointima formation in SV grafts and better preserved media in ITA grafts (white line—intima, black line—media; a–c: artery; d–f: vein; a + d: group 1; b + e: group 4; c + f: group 5; scale bars: lower magnification 200 µm, higher magnification 50 µm)
Growth factors, matrix metalloproteinases, and cytokines were mainly expressed by VSMCs, macrophages, and endothelial cells in both ITA and SV grafts.
We noticed a higher total percentage of MMP-7, MMP-9, EGFR, and bFGF in mostly all vessel wall layers of SV grafts (Supplementary Table 2), a higher percentage of TNF-ɑ, PDGFR-ɑ, and VEGF-A in ITA grafts, and a nearly similar distribution of TGF-β in both graft types. PDGFR-β showed an undulated course in both arteries and veins (Supplementary Table 3).
The peak of the expression was timely different in both vessel graft types and even different between the vessel wall layers within arterial or venous grafts.
The highest expression of MMP-9, EGFR, TNF-ɑ, and TGF-ß was observed on day 1 after implantation, the peak expression of MMP-7, bFGF, and PDGFR-α was noticed within 1 week after bypass grafting and the peak expression of PDGFR-ß and VEGF-A between 1 week and 1 month after CABG.
Slightly lower endothelialization in ITA grafts
After the endothelium was denuded and injured due to surgical procedure and distension pressure, we observed only a slight recovery and minimal endothelialization in arteries and veins with a slightly higher percentage of preserved endothelium and endothelialization in vein grafts, which showed an increase till 1 month and a decrease afterwards. Differences between ITA and SV grafts were not significant (Fig. 1c, Supplementary Table 1).
Significantly lower inflammation score in the media of ITA grafts
As expected, inflammation was more intense in the first month in in the two inner layers of arterial and venous bypass grafts, and the media of arterial grafts exhibited a clearly lower inflammation score (Fig. 1d). Inflammatory cells consisted mainly of neutrophil granulocytes, CD3 positive lymphocytes, macrophages, and some plasma cells. CD 20 positive B lymphocytes were completely absent.
Neutrophil granulocytes were predominantly seen within the first month after bypass surgery with a higher amount in the intima and media of venous conduits, later on the inflammatory infiltrate changed in favor of mononuclear cells.
The percentage of CD 163 positive macrophages was markedly higher than the amount of CD 3 positive lymphocytes (Supplementary Table 4).
Similar apoptotic index in ITA and SV grafts
Caspase 3, which is activated in apoptotic cells, was only expressed by VSMCs and endothelial cells of the intima and the vasa privata of the media and adventitia with a peak expression in the two inner layers of arteries on the first day (intima: 10.50 ± 7.37% vs. 7.14 ± 12.54%, p = n.s./media: 10.50 ± 6.66% vs. 5.71 ± 9.76%, p = n.s.) and in the intima and media of veins in the first week after bypass grafting (intima: 10.45 ± 6.97% vs. 6.11 ± 6.80%, p = n.s./media: 12.73 ± 9.00% vs. 5.63 ± 6.78%, p = n.s.; Fig. 1e, Supplementary Table 1).
Extremely low proliferation index in ITA and SV grafts
The Ki-67 proliferation index was extremely low with merely 1–3% in the whole vessel wall without any significant differences in arteries or veins (Fig. 1f, Supplementary Table 1). Surprisingly, we did not observe a positive staining of VSMCs, only some macrophages, lymphocytes and a few endothelial cells were positive.
Highest amount of elastic fibres in the media of ITA grafts in the baseline group and decelerated degeneration afterwards
The intima and media of arteries exhibited a significantly higher percentage of elastic fibres within the first week after bypass grafting and a minimal decrease of elastic fibres over the time (Figs. 2 and 4a, Supplementary Table 5). The number of elastic layers in arteries of all groups varied from 10 to 12.
When compared with arteries, veins had much thinner, fragmented fibres in the media, and thicker ones in the adventitia.
In arteries the internal elastic lamina (IEL) was one straight line, sometimes a double line, whereas veins showed multiple layers, and exhibited also more fragmentation and degeneration in group 5. Although the number of elastic lamellae in arteries did not significantly alter, ITA grafts showed also some degree of aging in group 5 with a higher amount of extracellular matrix between the particular elastic fibres.
Higher content of acid mucopolysaccharides and collagen type IV and lower fibrosis in ITA grafts (Supplementary Table 5)
Acid mucopolysaccharides were mainly expressed in the neointima and media of both vein and arterial grafts. The intima and media of arteries had a significantly higher content of mucopolysaccharides in groups 1, 2, and 3, and we observed a steadily increase in the mucopolysaccharide content in the neointima and media of both vessel types till 1 year after implantation (Figs. 4b, 5).
Alcian blue staining. A significantly higher percentage of acid mucopolysaccharides in the intima and media of ITA grafts in group 1 and a slightly increase of acid mucopolysaccharides in arteries and veins till 1 year after implantation (a–c: artery; d–f: vein; a + d: group 1; b + e: group 4; c + f: group 5; scale bars: lower magnification 200 µm, higher magnification 50 µm)
Collagen type IV, an important component of the basement membrane and extracellular matrix of the vascular system, was expressed by endothelial cells and VSMCs. Collagen type IV was abundant in the intima and media of arteries from the very beginning in group 1 (intima: 84.44 ± 6.85% vs. 56.67 ± 11.30%, p = 0.005; media: 81.56 ± 7.41% vs. 53.89 ± 7.74%, p = 0.003) with a significantly higher amount in the intima and media of ITA grafts over the whole time period (Figs. 4c, 6).
Collagen type IV staining. Significantly higher content of collagen type IV in intima and media of arteries in comparison to veins, but a slightly increase in SVs in the course of time (a–c: artery; d–f: vein; a + d: group 1; b + e: group 4; c + f: group 5; scale bars: lower magnification 200 µm, higher magnification 50 µm)
Fibrosis was seen in a significantly higher percentage in the neointima and media of vein grafts over the whole time period. We also observed an increase in fibrosis in the media and adventitia of vein grafts till group 5 as compared to arterial grafts (media: 48.00 ± 13.04% vs. 17.50 ± 6.46%, p = 0.004/ adventitia: 56.40 ± 13.22% vs. 39.60 ± 12.28%, p = n.s.) (Figs. 4d, 7).
Peak expression of MMP-7 and MMP-9 in SV grafts within 1 week after bypass surgery
Both members of the matrix metalloproteinase family reached their peaks of expression within 1 week after implantation and were higher in all vessel wall layers of veins. We noticed the highest amount of MMP-7 positive cells within 1 week in the intima of SV grafts (16.36 ± 12.06% vs. 3.86 ± 7.34%; p = 0.03; Fig. 8a) and the highest percentage of MMP-9 positive cells on day 1 after bypass surgery also in the intima of SV grafts (28.57 ± 24.62% vs. 4.00 ± 4.55%; p = 0.04; Fig. 8b). We also observed a higher amount of MMP-7 and MMP-9 positive cells in the intima of SV grafts in the baseline group, whereas the ITA grafts showed no expression of MMP-7 and MMP-9 in the intima and media.
Beyond 1 month after surgery, the levels of MMP-7 and MMP-9 declined in both arterial and venous grafts, MMP-9 was completely absent in the intima, and media of ITA grafts in group 5.
Higher percentage of EGFR in SV grafts and peak expression on day 1 after implantation
The total percentage of EGFR was generally higher in veins as compared to arteries throughout the whole time period and reached a peak on day 1 after bypass grafting in the intima and media (intima: 15.00 ± 4.14% vs. 2.50 ± 3.54%; p = 0.04/media: 40.00 ± 17.89% vs. 32.00 ± 3.17%; p = n.s). The expression of EGFR was elevated even in group 5 between 1 month and 1 year after bypass grafting (Fig. 8c).
Peak expression of bFGF in the media of SV grafts within the first week after surgery
bFGF, a heparin-binding protein and a key player in the process of proliferation and differentiation, showed its peak within the first week of implantation in the media of veins with a significantly higher percentage as compared to arteries (53.33 ± 22.91% vs. 15.63 ± 16.35%; p = 0.03) and a decreased percentage of bFGF positive cells afterwards (Fig. 8d).
SV grafts even showed a higher level of bFGF in the intima and media of the baseline group (intima: 22.86 ± 5.25% vs. 12.14 ± 3.80%, p = 0.002; media: 19.29 ± 5.62% vs. 12.00 ± 4.24%, p = 0.02).
Low percentage of TNF-α with the peak expression in all vessel wall layers of ITA grafts on day 1 after bypass surgery
TNF-α, an important cytokine inducing chemotaxis of inflammatory cells and fibroblasts and regulating the expression of growth factors, adhesion molecules, other cytokines and extracellular matrix degrading metalloproteinases, was found in a higher percentage in arteries compared to veins. It had its peak expression in all layers of ITA grafts on day 1 after bypass grafting (intima: 7.50 ± 15.00% vs. 1.43 ± 3.78%; p = n.s./media: 20.00 ± 17.80% vs. 1.67 ± 4.08%; p = n.s/ adventitia: 5.00 ± 4.08% vs. 0.71 ± 1.89%; p = n.s; Fig. 9a).
Higher expression of VEGF-A in ITA grafts with the highest level within 1 month after implantation
VEGF-A, a signal protein that stimulates vasculogenesis and angiogenesis, exhibited a higher level in arteries than in veins throughout the whole vessel wall with a peak in all vessel wall layers between 1 week and 1 month after implantation (intima: 19.00 ± 13.42% vs. 10.00 ± 3.13%; p = n.s/media: 21.60 ± 13.52% vs. 12.13 ± 0.00%; p = n.s./adventitia: 22.00 ± 10.95% vs. 10.00 ± 0.05%, p = n.s.). After 1 month, there was no expression of VEGF-A in the intima and media of venous grafts, which was significantly lower in comparison to arterial grafts (Figs. 9b, 10).
VEGF-A staining. Higher expression of VEGF-A in ITA grafts with the highest level between 1 week till 1 month after implantation and a significantly higher percentage in arterial grafts in group 5 (> 1 month–1 year after implantation). No expression of VEGF-A in the intima and media of the baseline groups (a–c: artery; d–f: vein; a + d—group 1; b + e—group 4; c + f—group 5; scale bars: lower magnification 200 µm, higher magnification 50 µm)
Peak expression of PDGFR-α in ITA grafts within 1 week after implantation and undulated course of PDGFR-ß in ITA and SV grafts
We found a distinct higher percentage of PDGFR-α in comparison to PDGFR-ß, and surprisingly, PDGFR-α was expressed in a higher percentage in arteries with the peak expression in the intima and media within the first week (intima: 31.25 ± 6.41% vs. 16.54 ± 9.87%; p < 0.001/media: 32.50 ± 7.07% vs. 18.08 ± 9.47; p < 0.001; Figs. 9c, 11).
PDGFR-α staining. Higher percentage of PDGFR-α in ITA grafts with the peak expression within 1 week after implantation and a higher level even in the baseline group of ITA grafts (a–c: artery; d–f: vein; a + d—group 1; b + e—group 4; c + f—group 5; scale bars: lower magnification 200 µm, higher magnification 50 µm)
PDGFR-β had an undulated course in both arteries and veins with the highest level in arteries within 1 week after surgery throughout the whole vessel wall, veins had their peak level in the media between 1 week and 1 month after surgery (Fig. 9d).
Similar distribution of TGF-β in ITA and SV grafts
TGF-ß, also a multifunctional cytokine, showed the peak expression on day 1 in the intima of veins (61.43 ± 26.7% vs. 52.50 ± 18.93%; p = n.s.) and media of arteries (62.50 ± 12.58% vs. 50.00 ± 18.26%; p = n.s.) with a nearly similar distribution in arteries and veins and was even present in a relatively high percentage in group 5 between 1 month and 1 year after bypass grafting. (Fig. 9e).
Discussion
The ITA has proven to provide superior long-term results, a higher patency and lower patient mortality than SV grafts.
One year after bypass grafting, we observed a significantly lower neointima formation with a reduced amount of SMA positive cells and a better preserved media with a higher amount of SMA positive cells in ITA grafts. That may be due to structural differences of both graft types, but also due to molecular differences between SV and ITA grafts.
The ITA belongs structurally to elastic arteries with a strong medial layer consisting of collagen, elastic fibres and circumferentially arranged VSMCs. This special structure of the ITA wall is responsible for the vessel tone, the alteration of the arterial diameter, and the perfect adaption to different arterial pressures after bypass grafting.
Over time we observed a degeneration of elastic fibres and the IEL especially in SV grafts. More gaps, fenestrations, and discontinuities in the IEL represent a problem, because they allow activated VSMCs of the media to migrate into the intima.
The switch of the venous VSMCs from the contractile to the secretive phenotype due to hypoxia, endothelial dysfunction, and inflammation (Wadey et al. 2018), and the migration of VSMCs from the media to the intima are crucial events in the progression of neointima formation. After the switch, they are responsible for the expression of different growth factors and cytokines, such as PDGF, TGF-β, VEGF, TNF-ɑ, and endothelin-1 (de Vries and Quax 2018) and are also able to produce various components of the extracellular matrix.
Whether or not myofibroblasts contribute to the neointima formation is still a matter of controversial discussion. Some believe that in response to the vessel graft injury and trauma after bypass grafting fibroblasts in the adventitia can change their phenotype into myofibroblasts and are then able to migrate through the media into the intima, where they deposit extracellular matrix. Alternatively, the role of myofibroblasts could be limited to structural changes of the adventitia. Anyway, the presence of myofibroblasts is extremely difficult to determine, because they express α-SM actin and can hardly be differentiated from VSMCs.
However, regarding the extracellular matrix, the total content of acid mucopolysaccharides in our study was significantly higher in arterial grafts from the very beginning with a steadily increase in the percentage till 1 year after bypass surgery in both arteries and veins. The major component present in the ITA is heparan sulfate while the dominant glycosaminoglycan in the SV is dermatan sulfate, which leads to increased attachment and adsorption of LDL and VDL, and maybe; therefore, the SV graft is more predisposed to neointimal thickening than the ITA graft (Wadey et al. 2018).
The ITA is also characterized by an extraordinary high amount of collagen type IV, not only as a component of the IEL, but especially in the extracellular matrix (ECM) of the intima and media, which can be one of several important supporting factors to avoid intimal hyperplasia and vessel graft occlusion after bypass surgery. Collagen type IV is produced by VSMCs with a higher release in the quiescent contractile cell type (Adiguzel et al. 2009), can prolongate the switch from the contractile to the synthetic phenotype, and is able to delay the proliferation and migration of VSMCs (Foglieni et al. 2008; Guo et al. 2018; Otsuka et al. 2013).
The starting point of vessel wall modifications after CABG is unquestionably the endothelial denudation caused by stretch, distension pressure and graft handling, leading to heightened oxidative stress. Unexpectedly, in the first month, we observed a very low endothelialization in arteries as compared to veins.
Intact and healthy endothelial cells normally produce the vasorelaxant prostacyclin (PGI2) and endothelium-derived nitric oxide (NO), which prevent platelet activation, adhesion, and aggregation (Borović et al. 2013) and subsequently vessel wall thrombosis and occlusion. Although we observed a lower endothelialization in ITA grafts, the remaining arterial endothelial cells may release a higher percentage of the antithrombotic endothelium-dependent relaxation factor (EDFR) than saphenous veins (Foglieni et al. 2008; Otsuka et al. 2013).
However, the loss of the endothelial cell layer exposes extracellular matrix components in ITAs and SVs and prepare the milieu for adhesion of granulocytes, monocytes, lymphocytes, and platelets, which are able to express and release various cytokines and growth factors.
During the first week of implantation, we could see that the inflammation in general and especially leukocytes play major roles in vessel graft adaption. After endothelial injury, platelet activation subsequently leads to inflammation and to the attachment of leukocytes.
Leukocytes become activated by the binding of P-selectin to P-selectin glycoprotein ligand-1 (PSGL-1) and are then able to invade and cross the vessel wall, which is also mediated by monocyte chemoattractant protein 1 (MCP-1), intercellular adhesion molecule 1 (ICAM-1), and macrophage-1 antigen (Mac-1).
Regarding the inflammatory infiltrate, we observed a very high amount of neutrophil granulocytes in the inner two layers of SV grafts within the first week after bypass surgery, and these neutrophils contain primary granules, which include elastase, myeloperoxidase, cathepsins, and defensins as well as secondary and tertiary granules with lactoferrin and MMP-9 inside.
Among the first released substances after vessel graft implantation were the matrix metalloproteinases MMP-7 and MMP-9, which were delivered immediately after implantation of the vessel wall with a significantly higher percentage in SV grafts. Both matrix metalloproteinases reached a peak expression in both vessel graft types within 1 week after surgery, although the percentage of MMP-7 was much lower in comparison to MMP-9. MMP-7, and MMP-9 are both involved in extracellular matrix (ECM) degradation by freeing smooth muscle cells from cell–matrix contacts, which is necessary for VSMC migration into the neointimal layer and also facilitates the entry of monocytes into the vessel wall (Sharony et al. 2006). A growth factor that plays also an important role for the enhancement of cell migration is EGF and indirectly EGFR by activation of c-Jun N-terminal kinase (JNK) (Huang et al. 2003).
EGFR was expressed in a higher percentage in all vessel wall layers of SV grafts with the peak expression in the intima and media on day 1 after surgery. It is involved in fibroblast and VSMC proliferation and is also known as a negative regulator of the apoptotic pathway.
Other important cell types within the inflammatory infiltrate were monocytes and macrophages. Monocytes cannot only enter the subendothelial space from the luminal side, where they become macrophages, but can also migrate from the periadventitial tissue and vasa privata of the media and adventitia into the vessel graft wall. Interestingly, we noticed a high amount of CD163 positive macrophages in the adventitia of both conduit types even 1 month to 1 year after surgery.
CD163 positive macrophages have been reported to be responsible for hypoxia inducible factor-alpha (HIF-α) and VEGF-A expression, increased intraplaque vascular cell adhesion protein-1 (VCAM-1) release, and inflammatory cell recruitment (Guo et al. 2018).
CD163 is also able to mediate the attachment of monocytes to endothelial cells, and is expressed in endothelial progenitor cells (EPCs), which are associated with neovascularization and angiogenesis (Pioli et al. 2004; Frings et al. 2002).
Activated macrophages are able to produce TNF-ɑ, which was surprisingly found in a higher percentage in all vessel wall layers of ITA grafts with the peak expression on day 1 after CABG. On the one hand, it is able to induce the production of inflammatory mediators such as ICAM-1 and MCP-1; on the other hand, it stimulates VSMC and fibroblast migration, promotes matrix degradation (Jiang et al. 2007), and regulates various different growth factors (PDGF, VEGF, FGF).
TNF-α modulates also the release of TGF-β, an important profibrotic factor. Although the percentage of fibrosis was much higher in all vessel wall layers of SV grafts, leading to a much stiffer und less flexible vessel graft wall, we noticed a similar distribution of TGF-β in both graft types with a lower expression in the baseline groups and the peak expression in the intima and media on day 1 after surgery in both arteries and veins.
TGF-ß was primarily produced by activated macrophages, lymphocytes, VSMCs, and endothelial cells. In SMC culture, TGF-β is reported to be the most potent stimulator of collagen synthesis (Rekhter 1999) and fibrosis and is linked to increased mRNA expression of collagen type I and collagen type III. TGF-β has also been shown to modulate matrix metalloproteinases (Simionescu et al. 2005) and VEGF (Padua and Massague 2009).
Another growth factor, which promotes fibroblast, endothelial and VSMC proliferation, (Bourassa 1994) and is also involved in tissue repair and regeneration, bFGF, was present in a higher percentage in veins as compared to arteries, especially in the first month after surgery. It was mainly released by endothelial cells and VSMCs.
PDGF is another important mediator of VSMC proliferation and migration in both human arteries and veins (Muto 2010), plays a significant role in angiogenesis and stimulates the synthesis of types I and III collagen in VSMC culture. Although PDGF is synthesized, stored, and released by platelets upon activation, it is also produced by other cells including VSMCs, activated macrophages, and endothelial cells.
We observed PDGFR-α in a higher percentage in ITA grafts with the highest expression within the first week after implantation, PDGFR-β revealed an undulated course without any preference of the vessel type.
A further growth factor, VEGF-A, was nearly absent in both baseline groups and exhibited a clearly higher level in all vessel wall layers of ITA grafts with the peak expression from 1 week to 1 month after CABG. It is mainly produced by VSMCs, macrophages, and endothelial cells. It is responsible for the migration and chemotaxis of macrophages and granulocytes, increased matrix metalloproteinase activity, and the creation of blood vessels.
VEGF is reported to be a negative regulator of neointimal formation in vein graft animal models (Kudo et al. 2007), which may be due to an accelerated reendothelialization of the damaged vessel or an increased NO production.
Normally, VEGF protects cells from apoptosis, but it has been shown, that cross talks between TGF-β1 and VEGF signaling converts VEGF/flk-1-activated p38MAPK into a proapoptotic signal, leading to apoptosis of the affected cell (Ferrari et al. 2006).
Although there were no significant differences concerning the percentage of caspase 3 between arteries and veins, a time-dependent caspase activation with the peak expression in the intima and media of arteries on day 1 and in veins within 1 week after implantation could be seen. Even in group 5, the apoptotic index was high in both vessel graft types.
Prolonged cell death may be responsible for the ongoing release of growth factors, which can in turn again activate VSMCs to migrate, secrete components of extracellular matrix, and release cytokines.
According to the current knowledge, VSMCs do not only migrate, but also proliferate (Angelini et al. 1991; Mehta et al. 1997; Motwani and Topol 1998; Wadey et al. 2018) and reenter the cell cycle after bypass grafting, but no Ki-67 positive VSMCs in the arterial and vein graft wall were found, which may be partly due to the advanced age of the vessel conduits. The results of our study implicate that rather migration and the switch from the quiescence to the secretive state in response to appropriate stimuli than proliferation may play a crucial role for the neointimal thickening.
Inhibition of almost all above-mentioned growth factors lead to a lower degree of intimal hyperplasia in animal models, but human studies so far have been disappointing.
TGF-ß1 antagonists reduced collagen content and expression in a rat vein graft model (Wolff et al. 2006) and in ex vivo organ culture of human SVs (Ranjzad et al. 2009), antisense bFGF adenovirus limited neointimal hyperplasia by an ERK-dependent mechanism in a rabbit vein graft model (Yamashita et al. 2003), and PDGFR inhibitor reduced cell proliferation also in a rabbit vein graft model (Kimura et al. 2008).
The majority of growth factor receptors are cell membrane-type tyrosine kinases that trigger downstream signal cascades, including the mitogen-activating protein kinase (MAPK) pathway, which upon stimulation, phosphorylate their specific substrates. This process can either lead to survival or apoptosis of the affected cell.
However, different receptor expression levels, collateral signaling pathways and the presence or absence of adaptor proteins make it difficult to exactly identify that specific pathway or cross-talk, which is initially responsible for the start of the development of intimal hyperplasia and therefore determine the differing fate and outcome of SV and ITA grafts. If it would be possible to block one specific target molecule at the very beginning of the signaling cascade via genetic vectors, occlusive vessel graft disease, and reoperations could be avoided.
A limitation to this study is the non-consideration of gender- and age-dependent differences between ITA and SV grafts. In addition, we did also not include serum parameters and the medication prior to death. Furthermore, tissue samples were obtained only from the proximal third of the vessel grafts to compare the two vessel graft types, and also studies from the middle, and the distal third of the vessels would be necessary to expand the overall picture. Furthermore, the specimens were obtained at autopsy 6–12 h after death and it is questionable, if autolysis has already influenced the biological reactivity of the tissue.
In conclusion, we observed a significantly lower intimal hyperplasia and a largely preserved media 1 year after bypass grafting in comparison to SV grafts and a more flexible and elastic structure due to higher amounts of elastic fibres, which form a barrier for migration of VSMCs, macrophages, lymphocytes, and other inflammatory cells.
We noticed a higher percentage of TNF-α, PDGFR-α, and VEGF-A in nearly all vessel wall layers of arterial grafts and a higher amount of MMP-7, MMP-9, EGFR, and bFGF in SV grafts.
Furthermore, we observed a timely different expression of growth factors and cytokines in ITA and SV grafts. The highest percentage of MMP-9, TGFβ, TNF-α, and EGFR was found on day 1 after implantation, the peak expression of MMP-7, bFGF, and PDGFR-α was noted within 1 week after bypass grafting and the peak expression of PDGFR-β, and VEGF-A between 1 week and 1 month after CABG.
The results of the present study indicate, that the main transformation of the vessel graft wall take place in the first days and weeks after bypass grafting, but subsequently vessel wall degeneration, tissue damage, and inflammation may lead to a continuous stimulation for the migration of VSCMs even months and years after implantation leading to an accelerated development of neointima formation in SV grafts.
Because most of the before-mentioned growth factors, growth factor receptors, and cytokines are regulated by MAPKs, our results suggest an activation of different pathways in both vessel graft types immediately after coronary artery bypass grafting.
References
Adiguzel E, Ahmad PJ, Franco C, Bendeck MP (2009) Collagens in the progression and complications of atherosclerosis. Vasc Med 14:73–89
Angelini GD, Soyombo AA, Newby AC (1991) Smooth muscle cell proliferation in response to injury in an organ culture of human saphenous vein. Eur J Vasc Surg 5:5–12
Borović ML, Borović S, Marinković-Erić J, Todorović V, Puškaš N, Kočica M, Radak Đ, Lačković V (2013) A comprehensive morphometric analysis of the internal thoracic artery with emphasis on, gender and left-to-right specific differences. Histol Histopathol 28:1299–1314
Bourassa MG (1994) Long-term vein graft patency. Curr Opin Cardiol 9:685–691
de Vries MR, Quax PHA (2018) Inflammation in vein graft disease. Front Cardiovasc Med 5:3
Ferrari G, Pintucci G, Seghezzi G (2006) VEGF, a prosurvival factor, acts in concert with TGF-beta1 to induce endothelial cell apoptosis. ProcNatl Acad Sci U S A 103:17260–17265
Foglieni C, Maisano F, Dreas L, Giazzon A, Ruotolo G, Ferrero E, Li Volsi L, Coli S, Sinagra G, Zingone B, Alfieri O, Becker AE, Maseri A (2008) Mild inflammatory activation of mammary arteries in patients with acute coronary syndromes. Am J Physiol Heart Circ Physiol 294:2831–2837
Frings W, Dreier J, Sorg C (2002) Only the soluble form of scavenger receptor CD163 acts inhibitory on phorbol ester-activated T-lymphocytes, whereas membrane bound protein has no effect. FEBS Lett 526:93–96
Guo L, Akahori H, Harari E, Smith SL, Polavarapu R, Karmali V, Otsuka F, Gannon RL, Braumann RE, Dickinson MH, Gupta A, Jenkins AL, Lipinski MJ, Kim J, Chhour P, de Vries PS, Jinnouchi H, Kutys R, Mori H, Kutyna MD, Torii S, Sakamoto A, Choi CU, Cheng Q, Grove ML, Sawan MA, Zhang Y, Cao Y, Kolodgie FD, Cormode DP, Arking DE, Boerwinkle E, Morrison AC, Erdmann J, Sotoodehnia N, Virmani R, Finn AV (2018) CD163+ macrophages promote angiogenesis and vascular permeability accompanied by inflammation in atherosclerosis. J Clin Invest 128:1106–1124
Huang C, Rajfur Z, Borchers C, Schaller MD, Jacobson K (2003) JNK phosphorylates paxillin and regulates cell migration. Nature 424:219–223
Jiang Z, Shukla A, Miller BL, Espino DR, Tao M, Berceli SA, Ozaki CK (2007) Tumor necrosis factor-α and the early vein graft. J Vasc Surg 45:169–176
Kimura S, Egashira K, Nakano K, Iwata E, Miyagawa M, Tsujimoto H, Hara K, Kawashima Y, Tominaga R, Sunagawa K (2008) Local delivery of imatinib mesylate (STI571)-incorporated nanoparticle ex vivo suppresses vein graft neointima formation. Circulation 118(14 Suppl):S65–S70
Kudo FA, Muto A, Maloney SP, Pimiento JM, Bergaya S, Fitzgerald TN, Westvik TS, Frattini JC, Breuer CK, Cha CH, Toshiya N, Tellides G, Sessa WC, Dardik A (2007) Venous identity is lost but arterial identity is not gained during vein graft adaptation. Arterioscler Thromb Vasc Biol 27:1562–1571
Mehta D, Izzat MB, Bryan AJ, Angelini GD (1997) Towards the prevention of vein graft failure. Int J Cardiol 62(Suppl 1):S55–63
Mitra AK, Gangahar DM, Agrawal DK (2006) Cellular, molecular and immunological mechanisms in the pathophysiology of vein graft intimal hyperplasia. Immunol Cell Biol 84:115–124
Motwani JG, Topol EJ (1998) Aortocoronary saphenous vein graft disease: pathogenesis, predisposition, and prevention. Circulation 97:916–931
Muto A, Model L, Ziegler K, Eghbalieh SDD, Dardik A (2010) Mechanisms of vein graft adaption to the arterial circulation: insights into the neointimal algorithm and management strategies. Circ J 74:1501–1512
Otsuka F, Yahagi K, Sakakura K, Virmani R (2013) Why is the mammary artery so special and what protects it from atherosclerosis. Ann Cardiothorac Surg 2:519–526
Owens CD (2010) Adaptive changes in autogenous vein grafts for arterial reconstruction: clinical implications. J Vasc Surg 51:736–746
Padua D, Massague J (2009) Roles of TGF beta in metastasis. Cell Res 19:89–102
Pioli PA, Goonan KE, Wardwell K, Guyre PM (2004) TGF-B regulation of human macrophage scavenger receptor CD163 is Smad3-dependent. J Leukoc Biol 76:500–508
Ranjzad P, Salem HK, Kingston PA (2009) Adenovirus-mediated gene transfer of fibromodulin inhibits neointimal hyperplasia in an organ culture model of human saphenous vein graft disease. Gene Ther 16:1154–1162
Rekhter MD (1999) Collagen synthesis in atherosclerosis: too much and not enough. Cardiovasc Res 41:376–384
Schachner T (2006) Pharmacologic inhibition of vein graft neointimal hyperplasia. J Thorac Cardiovasc Surg 13:1065–1072
Sharony R, Pintucci G, Saunders PC, Grossi EA, Baumann FG, Galloway AC, Mignatti P (2006) Matrix metalloproteinase expression in vein grafts: role of inflammatory mediators and extracellular signal-regulated kinases-1 and -2. Am J Physiol Heart Circ Physiol 290:H1651–1659
Simionescu A, Philips K, Vyavahare N (2005) Elastin-derived peptides and TGF-beta1 induce osteogenic responses in smooth muscle cells. Biochem Biophys Res Commun 334:524–532
Wadey K, Lopes J, Bendeck M, George S (2018) Role of smooth muscle cells in coronary artery bypass grafting failure. Cardiovasc Res 114:601–610
Wolff RA, Malinowski RL, Heaton NS, Hullett DA, Hoch JR (2006) Transforming growth factor-beta1 antisense treatment of rat vein grafts reduces the accumulation of collagen and increases the accumulation of h-caldesmon. J Vasc Surg 43:1028–1036
Yamashita A, Hanna AK, Hirata S, Dardik A, Sumpio BE (2003) Antisense basic fibroblast growth factor alters the time course of mitogen-activated protein kinase in arterialized vein graft remodeling. J Vasc Surg 37:866–873
Funding
No funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All performed procedures were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments.
Informed consent
Informed consent was obtained from next of kin.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Steger, C.M., Hartmann, A. & Rieker, R.J. Molecular differences between arterial and venous grafts in the first year after coronary artery bypass grafting. Histochem Cell Biol 154, 405–419 (2020). https://doi.org/10.1007/s00418-020-01896-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00418-020-01896-4