Abstract
We demonstrated previously that the expression of the disaccharide, GalNAcβ1 → 4GlcNAc (LacdiNAc), on N-glycans of cell surface glycoproteins in MDA-MB-231 human breast cancer cells suppresses their malignant properties such as tumor formation in nude mice. Here, we report changes in the morphological appearance and adhesive properties of two kinds of clonal cells of MDA-MB-231 cells overexpressing β4-N-acetyl-galactosaminyltransferase 4. The clonal cells exhibited a cobble stone-like shape as compared to a spindle-like shape of the mock-transfected cells and the original MDA-MB-231 cells. This was associated with an increased expression of cell surface E-cadherin, a marker of epithelial cells, and a decreased expression of N-cadherin, vimentin, α-smooth muscle actin and ZEB1, markers of mesenchymal cells. In addition, the clonal cells showed a lower migratory activity compared to the mock-transfected cells by wound-healing assay. These results suggest that mesenchymal–epithelial transition may be occurring in these clonal cells. Furthermore, increased adhesion to extracellular matrix proteins such as fibronectin, collagen type I, collagen type IV, and laminin was observed. The clonal cells spread and enlarged, whereas the mock-transfected cells demonstrated poor spreading on laminin-coated plates in the absence of fetal calf serum, indicating that expression of LacdiNAc on cell surface glycoproteins results in changes in cell adhesive and spreading properties particularly to laminin.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the most common cancer among women, with the number of patients increasing worldwide (Bray et al. 2018). Breast cancer can be classified into five subtypes based on gene expression profiles (van ’t Veer et al. 2002). Targeted therapies for individual patient groups have raised survival rates; however, patients with certain subtypes, such as a triple-negative-type breast cancer, which lacks estrogen and progesterone receptors, as well as epidermal growth factor receptor 2, have the least effective therapies to date (Gupta et al. 2019; Hwang et al. 2019). Therefore, treatments for this type of breast cancer are urgently needed.
Epithelial–mesenchymal transition (EMT), a process in which cells lose epithelial cell characteristics and acquire those commonly expressed by mesenchymal cells, is closely associated with cancer progression. For instance, during EMT, epithelial cells lose their polarity, cell-to-cell and cell-to-substratum interactions, and, on the other hand, acquire migratory and invasive activities similar to mesenchymal cells (Thiery and Sleeman 2006; Lamouille et al. 2014). Likewise, a cellular morphological change caused by the reorganization of the actin cytoskeleton is a hallmark of EMT. This transition causes decreased expression of epithelial marker molecules such as E-cadherin, while the expression levels of mesenchymal cell markers including N-cadherin, α-smooth muscle actin (α-SMA) and vimentin increase (Thiery and Sleeman 2006). The expression of these EMT-marker proteins is regulated by several transcription factors such as Snail, Twist and ZEB1 (Lamouille et al. 2014). The EMT process itself is reversible, and referred to as “mesenchymal–epithelial transition” (MET). A number of studies have shown the occurrences of both EMT and MET in breast cancer cells (Blick et al. 2008; Sarrió et al. 2008; Wu et al. 2016), and treatments with some chemical reagents such as Luteolin (Lin et al. 2017) and Glypican-3 (Castillo et al. 2016) can suppress the progression of triple-negative type breast cancer, by inducing MET in the cells. Importantly, it should be noted that down-regulation of α2,6-sialyltransferase-I results in MET in the triple-negative-type breast cancer cell line MDA-MB-231 (Lu et al. 2014). Thus, expression of a certain glycosyltransferase and its glycan products is closely associated with EMT or MET in cancer cells (Xu et al. 2012; Li et al. 2016; Xu et al. 2017).
We previously showed that the disaccharide, GalNAcβ1 → 4GlcNAc (LacdiNAc) on the non-reducing termini of N-glycans of cell surface glycoproteins significantly decreases according to the progression stages of human breast cancers (Kitamura et al. 2003), suggesting that this disaccharide could be an important diagnostic marker for breast cancers. Furthermore, overexpression of LacdiNAc by transfection of the β4-N-acetylgalactosaminyltransferase 4 (β4GalNAcT4) cDNA in MDA-MB-231 breast cancer cells drastically suppressed malignant properties, such as colony formation, in vitro invasion and in vivo tumor formation (Hirano et al. 2015). Since LacdiNAc is abundantly expressed in the non-malignant regions of breast cancer specimens (Kitamura et al. 2003), this may suggest that its presence on N-glycans is important for the maintenance of normal mammary epithelial cells. The LacdiNAcylation occurs on both N-linked and O-linked glycoproteins in many human cancer tissues and cell lines, and the expression levels of this unique disaccharide appear to be regulated in a tissue-dependent manner (Hirano et al. 2014). For instance, increased expression of LacdiNAc is observed in prostate cancer (Fukushima et al. 2010), colon cancer (Huang et al. 2007), and ovarian cancer (Machado et al. 2011; Anugraham et al. 2017). In contrast, decreased expression was observed in neuroblastoma (Hsu et al. 2011), breast cancer (Kitamura et al. 2003), and gastric cancer (Adamczyk et al. 2018). Thus, the degree of the presence, or absence of LacdiNAc at cell surfaces may be useful as a biomarker for different kinds of cancer. However, the biological role this disaccharide may play in the process of tumor malignancy remains to be elucidated.
Here, we investigate the effects on the cellular properties of LacdiNAc expressed on MDA-MB-231 cells by transfection with the β4GalNAcT4 cDNA. We observed that overexpression of LacdiNAc results in MET-like changes in MDA-MB-231breast cancer cells.
Materials and methods
Cell culture
MDA-MB-231 human breast cancer cells were obtained from American Type Culture Collection (Manassas, VA), and clone 1 and clone 2 cells were obtained by transfection of the β4GalNAcT4 cDNA in MDA-MB-231 cells as described previously (Hirano et al. 2015). The stocked clonal cells were used occasionally after confirming the expression levels of β4GalNAcT4 gene and LacdiNAc on cell surface glycoproteins in the present study. Cells were cultured in Dulbecco’s modified Eagle’s medium (DMEM) containing 10% fetal calf serum (FCS) at 37 °C in a water-saturated 5% CO2 atmosphere. For transforming growth factorβ1 (TGFβ1)-treatment, cells were cultured in DMEM containing 10% FCS and 10 ng/ml human recombinant TGFβ1 (PeproTech Inc., Rocky Hill, NJ) for 3 days.
Western blot analysis
Proteins were extracted in a radio-immuno-precipitation assay (RIPA) buffer (pH 7.4) containing a complete protease inhibitor cocktail and PhosSTOP (Roche Diagnostics, Mannheim, Germany). Western blot analysis was performed as described previously (Hirano et al. 2003). Briefly, extracted proteins were subjected to SDS-polyacrylamide gel electrophoresis (SDS-PAGE) (10%), and transferred to polyvinylidene difluoride (PVDF) membrane. The blot was incubated in Tris-buffered saline (TBS) (pH 7.4) containing 1% skin milk and 0.05% Tween-20 with one of the following antibodies at indicated dilution: anti-E-cadherin (3195S; 1:500, Cell Signaling Technology), anti-N-cadherin (13116T; 1:500, Cell Signaling Technology), anti-vimentin (5741T; 1:500, Cell Signaling Technology), anti-α-SMA (CSB-PA004667; 1:500, CUSABIO, Houston, TX), anti-ZEB1 (3396T; 1:500, Cell Signaling Technology), anti-FAK (3285S; 1:500, Cell Signaling Technology), anti-pFAK (Tyr397)(8556S; 1:500, Cell Signaling Technology), anti-Akt (9272S; 1:1000, Cell Signaling Technology), anti-pAkt (Ser473) (9271S; 1:200, Cell Signaling Technology), anti-Smad2 (5339S; 1:500, Cell Signaling Technology), anti-pSmad2 (Ser465/467)(3108S; 1:100, Cell Signaling Technology), anti-mTOR (2983S; 1:500, Cell Signaling Technology), anti-pmTOR (Ser2448) (5536S; 1:500, Cell Signaling Technology) or anti-GAPDH (016-25523; 1:1000, Wako Pure Chemical Industry, Osaka, Japan). After washing, the blot was incubated with a horseradish peroxidase (HRP)-conjugated anti-rabbit IgG antibody (7074P2; 10,000, Cell Signaling Technology). The immunoreacted bands were visualized with a SuperSignal West Femto (Thermo Fisher Scientific. Waltham, MA) using ChemiDoc XRS Plus (BioRad laboratories Inc., Hercules, CA). The images were analyzed using Image Lab software (version 4.0) (BioRad laboratories Inc.) and expressed as relative values by taking that of the mock-transfected cells as 1.0.
Quantitative real-time PCR analysis
Total RNA preparations were obtained using an RNeasy Mini Kit (QIAGEN K. K., Tokyo). cDNA was synthesized using an iScript Reverse Transcription Supermix reagent (BioRad Laboratories Inc.). Real-time PCR was performed by mixing the indicated amounts of a Kapa SYBR FAST reagent (KAPA Biosystems, Woburn, MA), sets of primers described below, and the obtained cDNA. PCR conditions were as follows: 95 °C for 10 s, followed by 35 cycles of 95 °C for 5 s, and 60 °C for 20 s. Primers used for real-time PCR were Snail (forward 5′-TGACCTGTCTGCAAATGCTC-3′; reverse 5′-CAGACCCTGGTTGCTTCAA-3′), Slug (forward 5′-GGGGAGAAGCCTTTTTCTTC-3′; 5′-reverse TCCTCATGTTTGTGCAGGAG-3′), ZEB1 (forward 5′-TGCACTGAGTGTGGAAAAAGC-3′; reverse 5′-TTGCAGTTTGGGCATTCATA-3′), and GAPDH (forward 5′-CTGACTTCAACAGCGACACC-3′; reverse 5′-CTGTAGCCAAATTCGTTGTCAT-3′).
Flow cytometric analysis
For flow cytometric analysis, cells were detached from dishes with PBS containing 0.05 mM EDTA, then washed with PBS containing 5 mM EDTA and 5 mg/ml bovine serum albumin (BSA). The cells were then incubated with a monoclonal anti-E-cadherin antibody (60335-1; 1:100; Proteintech, Chicago, IL) on ice for 2 h and, after washing, incubated with Alexa 488-conjugated mouse IgG (Life Technologies, Waltham, MA) on ice for 1 h. For negative control, cells were incubated only with the secondary antibodies. Finally, the expression of E-cadherin was analyzed using a Cell Lab Quanta SC system (Beckman Coulter Inc., Brea, CA).
Immunocytochemical analysis
Immunocytochemical analysis was performed as described previously (Hirano et al. 2003). Briefly, glass coverslips placed in a four-well dish were coated with either laminin (mouse EHS tumor, Wako Pure Chemical Industry) or fibronectin (human plasma, Wako Pure Chemical Industry) solution (10 μg/ml) at 4 °C overnight, and washed with FCS-free media before use. Then 2 × 105 cells grown on the coverslips were fixed in 3% formaldehyde solution at 37 °C for 10 min, followed by permeabilization with PBS containing 0.05% saponin and 10% bovine serum albumin (BSA). Actin was detected by staining with ActinGreen 488 ReadyProbes reagent (Thermo Fisher Scientific) according to the manufacturer’s instructions. Cell nuclei were detected by staining with 4′-6-diamidino-2-phenylindole (DAPI). For double immunofluorescence, monoclonal anti-E-cadherin (60335-1; 1:200, Proteintech, Chicago, IL) and polyclonal anti-β-catenin (8084T; 1:200, Cell Signaling Technology) antibodies were used, followed by Alexa 488-conjugated (Fab)2 goat anti-mouse IgG and Alexa 546-conjugated (Fab)2 goat anti-rabbit IgG. For negative control, cells were incubated with non-specific mouse IgG and rabbit IgG (Wako Pure Chemical Industry) at the same concentrations as primary antibodies followed by the secondary antibodies as above. For the detection of LacdiNAc on cell surface glycoproteins, non-permeabilized fixed cells were incubated with fluorescein isothiocyanate (FITC)-conjugated Wisteria floribunda agglutinin (WFA) (F-3101-2; 1:1000, EY Laboratories Inc., San Mateo, CA). Immunofluorescence was observed with a FluoView Fv-10i microscope using a 60× objective lens (N.A. = 1.35) (Olympus, Tokyo, Japan).
Wound healing assay
Cells were cultured in a 24-well dish in medium containing 10% FCS until they reached confluence. Monolayer cells were scratched with a plastic tip, and the migration distances of the cells were measured at multiple times with phase-contrast microscopy (Olympus IX70).
Determination of cell adhesive properties to extracellular matrices
Adhesive properties of the cells to different kinds of ECM were determined using a CytoSelect 48-well cell adhesion assay kit (Cell Biolabs, Inc. San Diego, CA) according to the manufacturer’s instructions. Either 1 × 105 cells or 2 × 105 cells were grown on ECM-coated dishes in FCS-free media, and attached cells were detected by staining with crystal violet solution. The stainings were quantified by measuring absorbance at OD595 nm following solubilization.
Results
Enhanced expression of LacdiNAc on cell surface glycoproteins results in morphological changes of clone 1 and clone 2 cell lines
In a previous study, we showed that LacdiNAc is expressed on several cell surface glycoproteins of clone 1 and clone 2 cells isolated from MDA-MB-231 cells after transfection with β4GalNAcT4 cDNA. Moreover, we also found that malignant properties, such as colony formation in soft agar, in vitro invasion, and in vivo tumor formation in nude mice were markedly suppressed (Hirano et al. 2015). The cultured clonal cells appear to be enlarged and interact with each other to show a cobble-stone-like shape (Fig. 1b, c) compared to the mock-transfected cells, which appear as a spindle-like shape without cellular interaction (Fig. 1a). To further confirm this observation, the organization of cytoskeletal actin filaments was studied by immunocytochemistry. Actin-stress fibers, which are a hallmark of mesenchymal-like cells, were detected in the mock-transfected cells (arrows in Fig. 1d), whereas a cortical actin meshwork was detected in the transfected clonal cells (arrowheads in Fig. 1e, f). When both the mock-transfected cells and transfected cells were incubated with fluorescence-labeled WFA, which interacts with LacdiNAc (Nakata et al. 1993), in a buffer without saponin, no significant fluorescence was detected in the mock-transfected cells (Fig. 1g), while significant fluorescence was associated with cell surfaces of the transfected cells (Fig. 1h, i), in agreement with our previous results (Hirano et al. 2015). The fluorescence was diminished upon incubation of the transfected cells in the presence of 10 mM N-acetylgalactosamine as a haptenic sugar (data not shown). These results suggest that enhanced expression of LacdiNAc on cell surface glycoproteins may be associated with a morphological alteration from mesenchymal-like to epithelial-like in these transfected cells.
Morphological appearances of the mock-transfected and clone-transfected cells. Cells were observed by phase-contrast microscopy (a–c), and the insets show magnified views (scale bar in c indicates 100 μm). F-actin was detected by staining with fluorescence-labeled phalloidin (d–f). Arrows and arrowheads indicate actin-stress fibers and cortex actins, respectively (d–f). The LacdiNAc on cell surface glycoproteins was detected with FITC-labeled WFA (g–i). Cell nuclei were detected by staining with DAPI in all pictures. Scale bars in f and i indicate 20 μm
To further investigate the MET transformation in the transfected cells, expression levels of marker proteins of MET and EMT were analyzed by Western blot with the band intensities determined by densitometric analysis. The expression level of E-cadherin, a marker of epithelial cells, increased by 2.5- and 3.0-fold in clone 1- and clone 2-transfected cells, respectively, compared to the mock-transfected cells (Fig. 2a, b). The expression levels of N-cadherin, vimentin, α-SMA and ZEB1, markers of mesenchymal cells, were 0.25- and 0.28-, 0.49- and 0.56-, 0.79- and 0.60-, and 0.57- and 0.62-fold expressed in clone 1- and clone 2-transfected cells, respectively, compared to the mock-transfected cells (Fig. 2a, b).
Characteristic features of the mock-transfected cells and clone-transfected cells. a Immunoblot analysis of E-cadherin, N-cadherin, vimentin, α-SMA, ZEB1 and GAPDH in the mock-transfected cells and clone 1- and clone 2-transfected cells was performed as described in the text. b Average intensity of each band obtained in (a) is shown as mean ± SD of three independent experiments
The expression of E-cadherin at the cell surface was investigated by immunocytochemistry since E-cadherin plays an important role in cell-to-cell contact of epithelial cells (Wells et al. 2008). Although E-cadherin was detected mainly in the cytoplasm of all cells (Fig. 3a–c), β-catenin, which interacts with E-cadherin at the inner surfaces of plasma membranes (Wells et al. 2008), was detected in clone 1- and clone 2-transfected cells (Fig. 3e, f), indicating that some E-cadherin may be expressed at the cell surfaces of the two transfected clonal cell lines. Since limited expression of E-cadherin at the cell surface made immunocytochemical detection difficult, a flow cytometric analysis which provides more sensitive and quantitative aspects of molecules at cell surfaces was employed. The results demonstrated a significantly increased expression of E-cadherin at cell surfaces in clone 1- and clone 2-transfected cells compared to the mock-transfected cells (Fig. 3j).
Expression of E-cadherin in the mock-transfected cells and clone-transfected cells. a Immunocytochemical analysis of E-cadherin in green (a–c) and β-catenin in red (d–f) in the mock-transfected cells and clone 1- and clone 2-transfected cells, respectively. Cell nuclei were detected by staining with DAPI (blue in all images). Arrowheads indicate distribution of E-cadherin and β-catenin on cell surfaces of clone 1- and 2-transfected cells (h and i). A scale bar in i indicates 10 μm. j Flow cytometric analysis of E-cadherin in the mock-transfected cells and clone 1- and clone 2-transfected cells
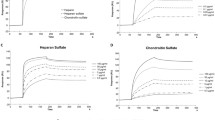
Since cells exhibiting mesenchymal cell-like properties show a high migratory activity (Thiery and Sleeman 2006; Lamouille et al. 2014), a wound-healing assay was used to compare the mock-transfected cells and the two kinds of clone-transfected cells (Fig. 4a), where the lengths of gaps between cells were determined (Fig. 4b). The results showed that after 12-h incubation, the gap length is reduced to 25% of the initial length in the mock-transfected cells, while they are only reduced to 64% and 58% of their initial lengths in clone 1- and clone 2-transfected cells (Fig. 4b), respectively. Thus, clone 1- and clone 2-transfected cells displayed reduced migratory activities compared to the mock-transfected cells. Taken together, these results suggest that the enhanced expression of LacdiNAc on cell surface glycoproteins may influence the MET process in clone 1- and clone 2-transfected cells.
Migratory activities of the mock-transfected cells and clone 1- and clone 2-transfected cells. a Wound healing assay was performed as described in the text, and gap lengths between cells at indicated times are shown by dotted lines in the images. b The quantified results obtained in (a) are shown as mean ± SD of each three-independent experiments by taking the value of an initial gap length as 1.0
TGFβ1 treatment induces EMT in mock-transfected cells and clone-transfected cells
Since TGFβ1 is known to induce EMT in various types of cells, including MDA-MB-231 breast cancer cells (Derynck and Zhang 2003; Lu et al. 2014), it was considered that TGFβ1 treatment may enhance EMT in the mock-transfected cells and induce EMT in clone 1- and clone 2-transfected cells. When the cells were treated with TGFβ1, the growth of the mock-transfected cells and two kinds of transfected clonal cells was inhibited by approximately 40% and 20%, respectively, as compared to non-treated cells (Fig. 5a). A morphological change to a more spindle-like shape was observed in the mock-transfected cells upon treatment with TGFβ1, while clone 1- and clone 2-transfected cells remained mostly in a cobble stone-like shape, with a small number of cells losing cell-to-cell contact and displaying a spindle-like appearance (Fig. 5a).
Effects of TGFβ1-treatment on the mock-transfected cells and clone-transfected cells. a Cells were grown in the presence or absence of 10 ng/ml TGFβ1 for 3 days, and the appearance of cells was observed by phase-contrast microscopy. Scale bar indicates 100 μm. b Gene expression levels of transcription factors were determined by quantitative real-time PCR. The expression levels were normalized against those of GAPDH. The results are shown as mean ± SD of each of three independent experiments. c Phosphorylation of Smad2, Akt, FAK and mTOR was examined by immunoblot analysis. The experiments were conducted in triplicate using GAPDH as a control, and representative data are shown
The expression levels of the transcription factors, Slug, Snail and ZEB1, that induce EMT, were determined by quantitative real-time PCR. As shown in Fig. 2, the expression level of ZEB1 protein in the clone-transfected cells decreased compared to the mock-transfected cells, and the transcript level of ZEB1 as well as Slug and Snail in clone 1- and clone 2-transfected cells also decreased compared to the mock-transfected cells (Fig. 5b). When cells were treated with TGFβ1, transcript levels of both Slug and Snail were increased approximately 1.3-fold in the mock-transfected cells and clone-transfected cells compared to the non-treated cells. In contrast, the transcript level of ZEB1 in the mock-transfected cells and clone-transfected cells was not changed significantly by TGFβ1 treatment (Fig. 5b). In addition, the expression level of E-cadherin in both the mock-transfected cells and clone-transfected cells decreased when treated with TGFβ1 (data not shown). These results indicate that TGFβ1 treatment can induce EMT-associated changes in both the clone-transfected cells and the mock-transfected cells.
A number of studies have demonstrated that TGFβ1 induces EMT through either the Smad signaling pathway or the non-Smad signaling pathway (Derynck and Zhang 2003; Colak and Dijke 2017). To investigate the signaling pathways that regulate EMT in response to TGFβ1 in these cells, the phosphorylation of downstream target molecules of the TGFβ-signaling cascades was examined by immunoblot analysis. A slight increase in the phosphorylation level of Smad2 was observed in all cells upon TGFβ1 treatment compared to the non-treated cells (Fig. 5c). This indicates that the Smad-signaling pathway can contribute to some extent to the induction of EMT in these cells. Since the non-Smad pathway activated by TGFβ1 treatment includes several signaling pathways in which PI3K, P38 and/or ERK-MAP kinases are involved (Colak and Dijke 2017), the phosphorylation of Akt was determined. The results showed that upon treatment with TGFβ1 levels of Akt are not changed significantly in the mock-transfected cells and transfected cells (Fig. 5c). Furthermore, the phosphorylation levels of mTOR and FAK were also not changed by TGFβ1-treatment in the mock-transfected cells and transfected cells (Fig. 5c). These results indicate that TGFβ1 can enhance EMT in the mock-transfected cells and induce EMT in clone-transfected cells through the Smad pathway and through non-Smad pathways other than those mediated by Akt and FAK.
LacdiNAcylation of cell surface glycoproteins promotes adhesion and spreading of clone-transfected cells on extracellular matrices
Since EMT has been reported to affect cell-to-substratum interaction (Lamouille et al. 2014), adhesive properties of the mock-transfected cells and clone-transfected cells toward several ECM proteins coated on plates (available commercially as an assay kit) were examined in the absence of FCS by staining the attached cells with crystal violet (Fig. 6a) followed by quantification of staining (Fig. 6b). The results showed that only a few cells attach to BSA-coated plates in both the mock-transfected cell and clone-transfected cells, while more clone 1- and clone 2-transfected cells adhere to fibronectin-, collagen type I-, collagen type IV-, or laminin-coated plates than the mock-transfected cells (Fig. 6a, b). In particular, clone 1- and 2-transfected cells showed much stronger adhesion to laminin-coated plates than the mock-transfected cells, with mean values of attached cells detected by staining of transfected cells (each 2 × 105 cells) were 1.99 and 2.92, respectively, while that of the mock-transfected cells was 0.48 (Fig. 6b).
Adhesive activities of the mock-transfected cells and clone-transfected cells toward ECMs. a Cells attached to BSA-, laminin-, collagen type-IV-, collagen type I- and fibronectin-coated plates were detected by staining with crystal violet. b Adhesive activities of cells to each ECM obtained in (a) were quantified as described in the text, and are presented each as mean ± SD of three independent experiments
Immunocytochemistry revealed that all cells exhibited a round shape on BSA-coated plates (Fig. 7a–c). Clone 1- and clone 2-transfected cells adhered and spread on laminin-coated plates with well-organized cortical actin filaments (Fig. 7e, f). In contrast, only a few mock-transfected cells adhered to laminin-coated plates without spreading (Fig. 7d). Both the mock-transfected cells and clone-transfected cells adhered to fibronectin-coated plates strongly even in the absence of FCS (Fig. 7g–i). These results indicate that the two kinds of clone-transfected cells acquire stronger adhesive and spreading activities, particularly to laminin, compared to the mock-transfected cells.
Morphological appearances of the mock-transfected cells and clone-transfected cells on ECM-coated plates. The mock-transfected cells and clone 1- and clone 2-transfected cells adhered to BSA- (a–c), laminin- (d–f) and fibronectin-coated (g–i) plates in the absence of FCS are shown. F-actin was detected by staining with fluorescence-labeled phalloidin, and cell nuclei were detected by staining with DAPI in all images. Scale bar in i indicates 20 μm
Discussion
The breast cancer cell line MDA-MB-231 is of the triple-negative type and highly metastatic, exhibiting a mesenchymal cell phenotype (Blick et al. 2008; Wu et al. 2016). Several studies have shown that certain chemicals and proteins can induce EMT or MET in MDA-MB-231 cells. For instance, anti-tumor drugs such as Sarasinoside A1 (Austin et al. 2013) and Luteolin (Lin et al. 2017) can induce MET in MDA-MB-231 cells, and it is assumed that these molecules suppress malignant properties of this type of breast cancer. In contrast, the enhanced expression of β1-integrin induces EMT in MDA-MB-231 cells (Hou et al. 2016). Interestingly, the increased expression of α2,6-sialyltransferase-I has been shown to enhance EMT in MDA-MB-231 cells (Lu et al. 2014). In a similar context as above, here we showed that the enhanced expression of the β4GalNAcT4 induces the increased expression of LacdiNAc in MDA-MB-231 cells, resulting in MET-like morphological and biochemical changes in the cells. These results extended our previous observations showing that increased expression of LacdiNAc on cell surface glycoproteins suppresses malignant phenotypes of MDA-MB-231cells (Hirano et al. 2015).
The mechanism accounting for the induction of MET in clone 1- and 2-transfected cells upon overexpression of LacdiNAc is not understood. It has been well documented that alterations of glycan structures of cell surface glycoproteins affect malignant properties of tumors (Varki 1993). In particular, changes of N-glycan structures on cell adhesion molecules such as integrins affect cell-to-cell and cell-to-substratum interactions, thus resulting in changes in cell adhesive and migratory properties (Asada et al. 1997; Gu and Taniguchi 2008; Gu et al. 2012). Integrin molecules are heterodimeric transmembrane receptors composed of α- and β-subunits, and bind selectively to extracellular matrices such as laminin and fibronectin (Miranti and Brugge 2002). They possess several potential N-glycosylation sites, and the β-propeller domain of the α5-subunit has been shown to be essential not only for the formation of heterodimers with a β1-subunit but also for biological functions including cell adhesion, spreading, and migration (Isaji et al. 2006). Furthermore, overexpression of β4-N-acetylglucosaminyltransferase 3 has been shown to suppress the invasive activity of Hela S3 cells and to inhibit α5β1-integrin-mediated cell spreading of GE11 cells (Isaji et al. 2004, 2006; Gu et al. 2012). In the present study, we also showed that enhanced expression of LacdiNAc on cell surface glycoproteins in MDA-MB-231 cells results in differences in adhesive properties of cells to laminin and fibronectin compared to the control cells. Since α5β1-integrin and α6β1-integrin bind to fibronectin and laminin, respectively (Alam et al. 2007), a difference in the glycosylation between α5- and α6-subunits, if any, might affect their adhesive properties to individual ECM molecules in two kinds of clone-transfected cells. Our preliminary studies show that the LacdiNAcylation occurs predominantly on β1-integrin in these clone-transfected cells (unpublished data), and we also assumed that altered glycosylation occurs to α5- and α6-subunits as well. Thus, further studies, including the detailed structural analysis of N-glycans of integrin molecules have to be addressed.
Biological roles of LacdiNAc in cancer cells have not been fully understood since expression levels and functions of this disaccharide appear to be in a tissue-dependent manner (Huang et al. 2007; Hsu et al. 2011; Che et al. 2014; Hirano et al. 2014). Furthermore, enhanced expression of LacdiNAc on cell surface glycoprotein receptors causes differential effects on cells. For instance, the overexpression of β4GalNAcT3, which also involves the synthesis of LacdiNAc as well as β4GalNAcT4 (Sato et al. 2003), in HCT116 colon cancer cells resulted in promotion of adhesive, migratory and invasive activities of the cells through LacdiNAcylated-integrin-activated signaling pathways (Huang et al. 2007). In contrast, enhanced expression of LacdiNAc on N-glycans of β1-integrin by transfection of the β4GalNAcT3 cDNA in SK-N-SH and SH-SY5Y neuroblastoma cells resulted in inhibition of the phosphorylation of FAK, Akt, and ERK molecules, thus causing the suppression of malignant properties of these cells (Hsu et al. 2011). As described above, the LacdiNAcylation of N-glycans of integrin molecules may affect the integrin-mediated-signaling pathways by activating or phosphorylating FAK and Akt in two kinds of clone-transfected cells. However, no significant difference in the phosphorylation levels of Akt, FAK and mTOR was observed between the mock-transfected cells and clonal cells in the presence or absence of TGFβ1 (Fig. 5c). Because the LacdiNAcylation of glycoproteins in the clonal cells occurred not only in β1-integrin but also in a few other glycoproteins including an epidermal growth factor receptor (unpublished data), the present LacdiNAcylation may affect several other signaling pathways whose molecular mechanisms have yet to be determined.
The expression of LacdiNAc on N-glycans has been shown to be associated with functional differentiation of bovine mammary epithelial cells (Sato et al. 1997; Furukawa et al. 2001), and progression of stages of several human cancers (Fukushima et al. 2010; Hsu et al. 2011; Che et al. 2014; Hirano et al. 2014). Furthermore, LacdiNAc on N-glycans has been shown to play an important role in the regulation of self-renewal of mouse embryonic stem cells (Sasaki et al. 2011). Thus, LacdiNAc on N-glycans can participate in many biological functions of mammalian tissues and cell lines. However, their detailed molecular mechanisms remain to be elucidated.
Taken together, the present study strongly indicates that the enhanced expression of LacdiNAc on cell surface glycoproteins results in MET-associated morphological and biological changes in clone 1- and clone 2-transfected breast cancer cells, and that these changes may contribute to the suppression of malignant properties in these cells.
References
Adamczyk B, Jin C, Polom K, Muñoz P, Rojas-Macias MA, Zeeberg D, Borén M, Roviello F, Karlsson NG (2018) Sample handling of gastric tissue and O-glycan alterations in paired gastric cancer and non-tumorigenic tissues. Sci Rep 8:242
Alam N, Goel HL, Zarif MJ, Butterfield JE, Perkins HM, Sansoucy BG, Sawyer TK, Languino LR (2007) The integrin-growth factor receptor duet. J Cell Physiol 213:649–653
Anugraham M, Jacob F, Everest-Dass AV, Schoetzau A, Nixdorf S, Hacker NF, Fink D, Heinzelmann-Schwarz V, Packer NH (2017) Tissue glycomics distinguish tumour sites in women with advanced serous adenocarcinoma. Mol Oncol 11:1595–1615
Asada M, Furukawa K, Segawa K, Endo T, Kobata A (1997) Increased expression of highly branched N-glycans at cell surface is correlated with the malignant phenotypes of mouse tumor cells. Cancer Res 57:1073–1080
Austin P, Freeman SA, Gray CA, Gold MR, Vogl AW, Andersen RJ, Roberge M, Roskelley CD (2013) The invasion inhibitor sarasinoside A1 reverses mesenchymal tumor transformation in an E-cadherin-independent manner. Mol Cancer Res 11:530–540
Blick T, Widodo E, Hugo H, Waltham M, Lenburg ME, Neve RM, Tompson EW (2008) Epithelial mesenchymal transition traits in human breast cancer cell lines. Clin Exp Metastasis 25:629–642
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Caner J Clin 68:394–424
Castillo LF, Tascón R, Lago Huvelle MR, Novack G, Llorens MC, Dos Santos AF, Shortrede J, Cabanillas AM, de Kier Bal, Joffé E, Labriola L, Peters MG (2016) Glypican-3 induces a mesenchymal to epithelial transition in human breast cancer cells. Oncotarget 7:60133–60154
Che MI, Huang J, Hung JS, Lin YC, Huang MJ, Lai HS, Hsu WM, Liang JT, Huang MC (2014) β1,4-N-acetylgalactosaminyltransferase III modulates cancer stemness through EGFR signaling pathway in colon cancer cells. Oncotarget 15:3673–3684
Colak S, Dijke P (2017) Targeting TGF-β-signaling in cancer. Trend Cancer 3:56–71
Derynck R, Zhang YE (2003) Smad-dependent and Smad-independent pathways in TGF-β family signalling. Nature 425:577–584
Fukushima K, Satoh T, Baba S, Yamashita K (2010) α1,2-Fucosylated and β-N-acetylgalactosaminylated prostate-specific antigen as an efficient marker of prostatic cancer. Glycobiology 20:452–460
Furukawa K, Kitamura N, Sato T, Hiraizumi S (2001) Differentiation-associated expression of β-N-acetylgalactosaminylated N-linked oligosaccharides in mammary epithelial cells. Adv Exp Med Biol 491:313–323
Gu J, Taniguchi N (2008) Potential of N-glycan in cell adhesion and migration as either a positive or negative regulator. Cell Adh Migr 2:243–245
Gu J, Isaji T, Xu Q, Kariya Y, Gu W, Fukuda T, Du Y (2012) Potential roles of N-glycosylation in cell adhesion. Glycoconj J 29:599–607
Gupta I, Sareyeldin RM, Al-Hashimi I, Al-Thawadi HA, Al Farsi H, Vranic S, Al Moustafa AE (2019) Triple negative breast cancer profile, from gene to microRNA, in relation to ethnicity. Cancers (Basel) 11:363
Hirano K, Zuber C, Roth J, Ziak M (2003) The proteasome is involved in the degradation of different aquaporin-2 mutants causing nephrogenic diabetes insibidus. Am J Path 163:111–120
Hirano K, Matsuda A, Shirai T, Furukawa K (2014) Expression of LacdiNAc groups on N-glycans among human tumor is complex. BioMed Res Int. https://doi.org/10.1155/2014/981627
Hirano K, Matsuda A, Kuji R, Nakandakari S, Shirai T, Furukawa K (2015) Enhanced expression of the β4-N-acetylgalactosaminyltransferase 4 gene impairs tumor growth of human breast cancer cells. Biochem Biophys Res Commun 461:80–85
Hou S, Isaji T, Hang Q, Im S, Fukuda T, Gu J (2016) Distinct effects of β1 integrin on cell proliferation and cellular signaling in MDA-MB-231 breast cancer cells. Sci Rep 6:18430
Hsu WM, Che MI, Liao YF, Chang HH, Chen CH, Huang YM, Jeng YM, Huang J, Quon MJ, Lee H, Huang HC, Huang MC (2011) B4GALNT3 expression predicts a favorable prognosis and suppresses cell migration and invasion via β1-integrin signaling in neuroblastoma. Am J Path 179:1394–1404
Huang J, Liang JT, Huang HC, Shen TL, Chen HY, Lin NY, Che MI, Lin WC, Huang MC (2007) β1,4-N-acetylgalactosaminyltransferase III enhances malignant phenotypes of colon cancer cells. Mol Cancer Res 5:543–552
Hwang SY, Park S, Kwon Y (2019) Recent therapeutic trends and promising targets in triple negative breast cancer. Pharmacol Ther 199:30–57
Isaji T, Gu J, Nishiuchi R, Zhao Y, Takahashi M, Miyoshi E, Honke K, Sekiguchi K, Taniguchi N (2004) Introduction of bisecting GlcNAc into integrin α5β1 reduces ligand binding and down-regulates cell adhesion and cell migration. J Biol Chem 279:19747–19754
Isaji T, Sato Y, Zhao Y, Miyoshi E, Wada Y, Taniguchi N, Gu J (2006) N-glycosylation of the β-propeller domain of the integrin α5 subunit is essential for α5β1 heterodimerization, expression on the cell surface, and its biological function. J Biol Chem 281:33258–33267
Kitamura N, Guo S, Sato T, Hiraizumi S, Taka J, Ikekita M, Sawada S, Fujisawa H, Furukawa K (2003) Prognostic significance of reduced expression of β-N-acetyl- galactosaminylated N-linked oligosaccharides in human breast cancer. Int J Cancer 105:533–541
Lamouille S, Xu J, Derynck R (2014) Molecular mechanisms of epithelial–mesenchymal transition. Nat Rev Mol Cell Biol 15:178–196
Li X, Wang X, Tan Z, Chen S, Guan F (2016) Role of glycans in cancer cells undergoing epithelial–mesenchymal transition. Front Oncol 6:33
Lin D, Kuang G, Wan J, Zhang X, Li H, Gong X, Li H (2017) Luteolin suppresses the metastasis of triple-negative breast cancer by reversing epithelial-to-mesenchymal transition via downregulation of β-catenin expression. Oncol Rep 37:895–902
Lu J, Isaji T, Im S, Fukuda T, Hashii N, Takakura D, Kawasaki N, Gu J (2014) β-Galactoside α2,6-sialyltranferase 1 promotes transforming growth factor-β-mediated epithelial-mesenchymal transition. J Biol Chem 289:34627–34641
Machado E, Kandzia S, Carilho R, Altevogt P, Conradt HS, Costa J (2011) N-Glycosylation of total cellular glycoproteins from the human ovarian carcinoma SKOV3 cell line and of recombinantly expressed human erythropoietin. Glycobiology 21:376–386
Miranti CK, Brugge JS (2002) Sensing the environment: a historical perspective on integrin signal transduction. Nat Cell Biol 4:E83–E90
Nakata N, Furukawa K, Greenwalt DE, Sato T, Kobata A (1993) Structural study of the sugar chains of CD36 purified from bovine mammary epithelial cells: occurrence of novel hybrid-type sugar chains containing the Neu5Acα2 → 6GalNAcβ1 → 4GlcNAc and the Manα1 → 2Manα1 → 3Manα1 → 6Man groups. Biochemistry 32:4369–4383
Sarrió D, Rodriguez-Pinilla SM, Hardisson D, Cano A, Moreno-Bueno G, Palacios J (2008) Epithelial-mesenchymal transition in breast cancer relates to the basal-like phenotype. Cancer Res 68:989–997
Sasaki N, Shinomi M, Hirano K, Ui-Tei K, Nishihara S (2011) LacdiNAc (GalNAcβ1-4GlcNAc) contributes to self-renewal of mouse embryonic stem cells by regulating leukemia inhibitory factor/STAT3 signaling. Stem Cell 29:641–650
Sato T, Taka J, Aoki N, Matsuda T, Furukawa K (1997) Expression β-N-acetylgalactosaminylated N-linked sugar chain is associated with functional differentiation of bovine mammary gland. J Biochem 122:1068–1073
Sato T, Gotoh M, Kiyohara K, Kameyama A, Kubota T, Kikuchi N, Ishizuka Y, Iwasaki H, Togayachi A, Kudo T, Ohkura T, Nakanishi H, Narimatsu H (2003) Molecular cloning and characterization of a novel human β1,4-N-acetylgalactosaminyl-transferase, β4GalNAc-T3, responsible for the synthesis of N, N′-diacetyl-lactosediamine, GalNAcβ1-4GlcNAc. J Biol Chem 278:47534–47544
Thiery JP, Sleeman JP (2006) Complex networks orchestrate epithelial-mesenchymal transitions. Nat Rev Mol Cell Biol 7:131–142
van ’t Veer LJ, Dai H, van de Vijver MJ, He YD, Hart AA, Mao M, Peterse HL, van der Kooy K, Marton MJ, Witteveen AT, Schreiber GJ, Kerkhoven RM, Roberts C, Linsley PS, Bernards R, Friend SH (2002) Gene expression profiling predicts clinical outcome of breast cancer. Nature 415:530–536
Varki A (1993) Biological roles of oligosaccharides: all of the theories are correct. Glycobology 3:97–130
Wells A, Yates C, Shepard CR (2008) E-cadherin as an indicator of mesenchymal to epithelial reverting transitions during the metastatic seeding of disseminated carcinomas. Clin Exp Metastasis 25:621–628
Wu Y, Sarkissyan M, Vadgama JV (2016) Epithelial–mesenchymal transition and breast cancer. J Clin Med 5(2):13. https://doi.org/10.3390/jcm5020013
Xu Q, Isaji T, Lu Y, Gu W, Kondo M, Fukuda T, Du Y, Gu J (2012) Roles of N-acetylglucosaminyltransferase III in epithelial-to-mesenchymal transition induced by transforming growth factor β1 (TGF-β1) in epithelial cell lines. J Biol Chem 287:16563–16574
Xu Q, Niu X, Wang W, Yang W, Du Y, Gu J, Song L (2017) Specific N-glycan alterations are coupled in EMT induced by different density cultivation of MCF 10A epithelial cells. Glycoconj J 34:219–227
Acknowledgements
We are grateful to Dr. Tomoya Isaji and Dr. Jianquo Gu at Tohoku Medical and Pharmaceutical University, Japan, for their generous gift of anti-β1-integrin antibody.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hirano, K., Takada, Y. & Furukawa, K. LacdiNAcylation of N-glycans in MDA-MB-231 human breast cancer cells results in changes in morphological appearance and adhesive properties of the cells. Histochem Cell Biol 153, 17–26 (2020). https://doi.org/10.1007/s00418-019-01822-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00418-019-01822-3