Abstract
To assess the potential role of IL-6 in sciatic nerve injury-induced activation of a pro-regenerative state in remote dorsal root ganglia (DRG) neurons, we compared protein levels of SCG-10 and activated STAT3, as well as axon regeneration in IL-6 knockout (IL-6ko) mice and their wild-type (WT) counterparts. Unilateral sciatic nerve compression and transection upregulated SCG-10 protein levels and activated STAT3 in DRG neurons not only in lumbar but also in cervical segments of WT mice. A pro-regenerative state induced by prior sciatic nerve lesion in cervical DRG neurons of WT mice was also shown by testing for axon regeneration in crushed ulnar nerve. DRG neurons from IL-6ko mice also displayed bilaterally increased levels of SCG-10 and STAT3 in both lumbar and cervical segments after sciatic nerve lesions. However, levels of SCG-10 protein in lumbar and cervical DRG of IL-6ko mice were significantly lower than those of their WT counterparts. Sciatic nerve injury induced a lower level of SCG-10 in cervical DRG of IL-6ko than WT mice, and this correlates with significantly shorter regeneration of axons distal to the crushed ulnar nerve. These results suggest that IL-6 contributes, at the very least, to initiation of the neuronal regeneration program in remote DRG neurons after unilateral sciatic nerve injury.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The primary sensory neurons of dorsal root ganglia (DRG) send off afferent axons with their peripheral branches in the peripheral nerves and central branches that run through the dorsal roots into the spinal cord. The bodies of primary sensory neurons react to peripheral nerve injury by upregulating a large spectrum of genes, transforming factors and regeneration-associated proteins that regulate the neuronal regeneration program (Mason et al. 2002; Liu et al. 2011; Bareyre et al. 2011; Mar et al. 2016; Martin et al. 2019). Under permissive extrinsic conditions, this results in promoting axonal regrowth distal to the peripheral nerve damage. Therefore, DRG neurons are frequently used as a reliable model for in vivo and in vitro studies of the intrinsic factors coordinating the neuronal regenerative program.
It has been found that axotomy induces a brisk transient increase of IL-6 synthesis in sensory neurons (Murphy et al. 1995). In our previous experiments we have found bilaterally increased levels of IL-6 and its receptor mRNA and protein not only in DRG neurons associated with the injured sciatic nerve, but also in remote cervical DRG (Dubový et al. 2013; Brázda et al. 2013). Unilateral sciatic nerve injury also induced bilateral activation of signal transducer and activator of transcription 3 (STAT3) through tyrosine-705 (Y705) phosphorylation in rat DRG neurons of both lumbar and cervical segments. Moreover, we detected increased IL-6 protein levels in the CSF following sciatic nerve injury and found activation of STAT3 in cervical DRG after intrathecal injection of IL-6 (Dubový et al. 2018a). It is well documented that activated STAT3 is a critical transforming factor of the neuronal pro-regenerative state (Smith et al. 2011; Bareyre et al. 2011; Zigmond 2012a). These published results suggest that IL-6 is a candidate molecule involved in initiating the pre-regenerative changes in remote DRG neurons after sciatic nerve lesion.
Superior cervical ganglion 10 (SCG-10) protein, also known as stathmin 2, is a neuron-specific member of the stathmin family (Sugiura and Mori 1995), that is significantly increased in most DRG neurons very early following a nerve lesion (Shin et al. 2014; Dubový et al. 2018b). SCG-10 immunostaining is also a good marker for regenerating sensory axons (Shin et al. 2012, 2014). Therefore, SCG-10 immunodetection is useful in monitoring the pro-regenerative state of DRG neurons and assessing axon regeneration distal to the nerve lesion.
In the results presented here, we used a mice model to confirm sciatic nerve injury-induced activation of a regenerative program in remote cervical DRG neurons. We compared SCG-10 protein levels and activation of STAT3 in lumbar and cervical DRG neurons of interleukin-6 knockout (IL-6ko) with wild-type (WT) mice to investigate if IL-6 is implicated in initiating the pro-regenerative program in remote cervical DRG neurons after sciatic nerve injury. In addition, the pro-regenerative state of cervical DRG neurons induced by sciatic nerve lesion was tested using an axon regeneration assay in crushed ulnar nerve.
Materials and methods
Mouse strains and surgical treatment
Thirty male mice (6–8 weeks old) of wild-type (WT) and 30 IL-6 knock out (IL-6ko) were used in all experiments. IL-6ko mice in the C57BL/6 genetic background were obtained from Jackson Labs. (Bar Harbor, ME) and C57BL/6J WT mice were purchased from the Masaryk University breeding facility as reference counterparts. Mice were housed in individually ventilated cages with a maximum of five animals per cage in 12 h light/dark cycles at a temperature of 22–24 °C under specific pathogen-free conditions in the animal facility of Masaryk University. Sterilized standard rodent food and water were available ad libitum. The experiments were approved by the Animal Care Committee of the Faculty of Medicine, Masaryk University, Czech Republic and Czech Governmental Animal Care Committee, in compliance with the Czech Animal Protection Act no. 246/1992. All surgical procedures were performed under anesthesia using a mixture of ketamine (100 mg/kg) and xylazine (20 mg/kg) administered intraperitoneally. Animals were randomly allocated to experimental groups. Seven WT and seven IL-6ko mice without any surgical treatment were used as naïve controls.
The left sciatic nerve of ten WT and ten IL-6ko mice was exposed in mid-thigh between the gluteus maximus and the anterior head of the biceps femoris, ligated with two ligatures and cut with a pair of sharp scissors (complete sciatic nerve transection, CSNT). The proximal nerve stump was buried in muscle to prevent the distal stump from reinnervation. The left sciatic nerve of a further ten WT and ten IL-6ko mice was exposed and three ligatures with 6-0 silk suture (Ethicon) were tied around the sciatic nerve to reduce its diameter (sciatic nerve constriction, SNC). The muscles and skin were closed with 5/0 sutures and animals were left to survive for 7 days.
Quantitative immunohistochemical analysis
Naïve, SNC- and CSNT-operated WT and IL-6ko mice (n = 3 for each group) were deeply anesthetized with a lethal dose of sodium pentobarbital (80 mg/kg body weight, i.p.) and perfused transcardially with 100 ml phosphate-buffered saline (PBS, pH 7.4) followed by 100 ml of Zamboni’s fixative (Zamboni and de Martino 1967). The L3–L4 and C6–C8 DRG from both sides were removed and immersed in Zamboni’s fixative at 4 °C overnight and then collected into samples of ipsilateral (L-DRGi) and contralateral (L-DRGc) lumbar as well as ipsilateral (C-DRGi) and contralateral (C-DRGc) cervical DRG for each group of mice.
The DRG samples were washed in 20% phosphate-buffered sucrose for 12 h, blocked in Tissue-Tek® OCT compound (Miles, Elkhart, IN) and cut to prepare serial longitudinal cryostat sections (10 µm). The sections were mounted on chrome-alum covered slides and processed under the same conditions for indirect immunohistochemical staining for SCG-10 and STAT3(Y705). Briefly, sections were washed with PBS containing 0.05% Tween 20 (PBS-T) and 1% bovine serum albumin (BSA) for 10 min, treated with 5% normal donkey serum in PBS-T for 30 min, then incubated with 25 µl of rabbit polyclonal antibody against SCG-10 (1:1000; LSBio, USA) or STAT3(Y705) (1:100; Santa Cruz, USA) in a humid chamber at room temperature (21 to 23 °C) for 12 h. SCG-10 and STAT3Y705 immunoreactions were visualized by treatment with FITC- or TRITC-conjugated and affinity-purified donkey anti-rabbit secondary antibodies (1:100; Millipore, USA), respectively. Sections were stained with Hoechst 33342 to detect cell nuclei, mounted in aqueous mounting medium (Vectashield; Vector Laboratories, USA) and analyzed using an epifluorescence microscope (Nikon Eclipse, Nikon, Czech Republic) equipped with a camera (DFC-480; Leica Microsystems) and a stabilized power supply for the lamp housing. The control sections were incubated either without the primary antibodies or by substituting the primary antibodies with the donkey IgG isotype.
Neuronal diameter and STAT3(Y705) nuclear immunofluorescence intensities were measured using a NIS-Elements image analysis system (Nikon, Czech Republic) as described previously (Dubový et al. 2002, 2018a). At least 60 neuronal profiles containing nuclei were measured for each animal group. The immunofluorescence intensities were expressed as mean intensity ± SD.
Western blot analysis
SCG-10 and STAT3(Y705) protein levels in DRG were analyzed by Western blot. Naïve, SNC- and CSNT-operated WT and IL-6ko mice (n = 4 for each group) were deeply anesthetized with a lethal dose of sodium pentobarbital (80 mg/kg body weight, i.p.) and DRG of both sides were removed under aseptic conditions from lumbar (L3–L4) and cervical (C6–C8) positions, washed in protease and phosphatase inhibitor cocktails (Roche, Germany), flash-frozen in liquid nitrogen and stored at − 80 °C until being analyzed further. The DRG samples were homogenized in TRIS-buffered saline (pH 7.2) with 0.1% Triton X-100 and a cocktail of protease and phosphatase inhibitors (LaRoche, Switzerland) and centrifuged at 10,000g for 5 min at 4 °C. Proteins were separated by SDS-polyacrylamide gel electrophoresis and transferred to nitrocellulose membranes by electroblotting (BioRad). After blocking with 5% bovine serum albumin (BSA) in TRIS-buffered saline (pH 7.2) for 2 h, the membranes were incubated with rabbit polyclonal antibody against SCG-10 (1:500; LSBio, USA) or STAT3(Y705) (1:100; Santa Cruz, USA) overnight. Blots were washed in TRIS-buffered saline (pH 7.2) and incubated with peroxidase-conjugated anti-rabbit IgG (1:1000; Sigma, USA) at room temperature for 1 h. Protein bands were visualized using the ECL detection kit (Amersham, USA) on the chemiluminometer reader LAS-3000 (Fuji, Japan) and analyzed using densitometry image software. Equal loading of proteins was confirmed by β-actin levels (Actin). The protein levels were compared to the value from naïve DRG, which was arbitrarily set as one.
In vivo assay of axon regeneration in crushed ulnar nerve
Mice that had undergone prior SNC or CSNT (n = 3 for each group of both WT and IL-6ko) for 7 days were re-anesthetized and the left ulnar nerve was exposed and crushed using a clamp with a defined force of 1.9 N for 5 s at two clicks at the same site (Ronchi et al. 2010) under a stereoscopic microscope. The left ulnar nerve was also crushed in a control group without any previous sciatic nerve injury (n = 3 for both WT and IL6ko). The distal margin of the crush injury was marked with a 10-0 epineurial stitch (Ethicon), the skin wound was closed with 5/0 sutures, and the animals were allowed to recover for 24 h.
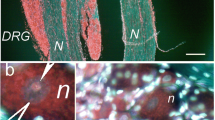
To investigate initiation of peripheral axon regeneration, the left ulnar nerves were removed following pericardial infusion with Zamboni fixative solution and nerve samples were fixed by immersion in Zamboni fixative solution overnight. After washing with 10% sucrose in PBS, 10 µm-thick longitudinal cryostat sections were cut and immunostained with rabbit polyclonal antibody against SCG-10 (1:1000; LSBio, USA) and FITC-conjugated, affinity-purified donkey anti-rabbit secondary antibody as described above. SCG-10 fluorescence intensity was analyzed along the length of the nerve distal to the crush; the regeneration index was determined by measuring the length of the longest SCG-10 decorated axons from the crush site (Abe et al. 2010). The length of SCG-10 immunopositive (SCG-10+) axons was measured in every third section by a person blind to the experimental conditions.
Statistical analyses
Statistical differences between data of STAT3 immunofluorescence intensities, Western blot and axon regeneration analysis of naïve DRG neurons and DRG neurons of SNC- or CSNT-operated mice were tested using a Mann–Whitney U test (p < 0.05). All statistical analyses were performed using STATISTICA 9.0 software (StatSoft, Inc., USA).
Results
Immunohistochemical and Western blot analysis of SCG-10 and STAT3 proteins in mouse DRG
Sections immunostained under the same conditions revealed weak SCG-10 immunoreactivity in both lumbar and cervical DRG neurons of naïve WT and IL-6ko mice (Figs. 1a, b, 2a, b). Unilateral SNC or CSNT of WT mice induced a substantial increase of SCG-10 immunofluorescence intensity in lumbar DRG neurons both ipsilateral (Fig. 1e, i) and contralateral (Fig. 1f, j) to the sciatic nerve lesions and bilaterally in cervical DRG (Fig. 1c, d, g, h). In contrast to WT mice, SNC or CSNT in IL-6ko mice induced increased SCG-10 immunofluorescence intensity only in lumbar DRG ipsilateral to the sciatic nerve lesions (Fig. 2e, i). However, the contralateral lumbar DRG neurons and the neurons of cervical DRG of both sides displayed only moderate SCG-10 immunofluorescence (Fig. 2c, d, f–h, j).
Representative pictures of cryostat sections through lumbar (L4) and cervical (C7) dorsal root ganglia (DRG) from naïve (a, b) WT mice and those with unilateral sciatic nerve compression (SNC; c–f) or complete sciatic nerve transection (CSNT; g–j) for 7 days. The sections of ipsilateral and contralateral lumbar (DRG-L4i, DRG-L4c) and cervical (DRG-C7i, DRG-C7c) DRG were incubated under the same conditions with rabbit polyclonal antibody against SCG-10 and FITC-conjugated donkey anti-rabbit secondary antibody. Unilateral SNC or CSNT of WT mice induced a substantial increase of SCG-10 immunofluorescence intensity in lumbar neurons both ipsilateral (e, i) and contralateral (f, j) to the sciatic nerve lesions and bilaterally in cervical DRG (c, d, g, h). Scale bars = 30 µm
Representative pictures of cryostat sections through lumbar (L4) and cervical (C7) dorsal root ganglia (DRG) from naïve (a, b) IL-6ko mouse and IL-6ko mice with unilateral sciatic nerve compression (SNC; c–f) or complete sciatic nerve transection (CSNT; g–j) for 7 days. The DRG sections were incubated under the same conditions with rabbit polyclonal antibody against SCG-10 and FITC-conjugated donkey anti-rabbit secondary antibody. SNC or CSNT in IL-6ko mice induced increased SCG-10 immunofluorescence intensity only in lumbar DRG ipsilateral to the sciatic nerve lesions (e, i). The contralateral lumbar DRG neurons (f, j) and the neurons of cervical DRG of both sides (c, d, g, h) displayed only moderate SCG-10 immunofluorescence. Scale bars = 30 µm
Alongside increased SCG-10 immunostaining intensity, higher STAT3 activation by phosphorylation at Tyr-705 (Y705) and its nuclear translocation was observed bilaterally in both lumbar and cervical DRG neurons 7 days after SNC or CSNT operated WT mice when compared with naïve ones (Figs. 3, 5). Sections of DRG from IL-6ko mice immunostained under the same conditions as those of WT mice revealed only moderate activation and nuclear translocation of STAT3(Y705), but distinct activation and nuclear translocation of STAT3(Y705) was observed in lumbar DRG neurons ipsilateral to the sciatic nerve lesions. Only CSNT induced the bilateral increase of nuclear STAT3(Y705) translocation in lumbar DRG neurons with significant enhancement on the contralateral side (Figs. 4, 5).
Representative pictures of cryostat sections through lumbar (L4) and cervical (C7) dorsal root ganglia (DRG) from naïve (a, b) WT mice and WT mice with unilateral sciatic nerve compression (SNC; c–f) or complete sciatic nerve transection (CSNT; g–j) for 7 days. The sections of ipsilateral and contralateral lumbar (DRG-L4i, DRG-L4c) and cervical (DRG-C7i, DRG-C7c) DRG incubated under the same conditions show immunofluorescence staining of STAT3 activated by Y705 phosphorylation and its nuclear translocation (arrowheads) bilaterally in lumbar (e, f, i, j) and cervical (c, d, g, h) DRG neurons 7 days after SNC or CSNT when compared with naïve ones (a, b). Scale bars = 30 µm
Representative pictures of cryostat sections through dorsal root ganglia (DRG) from naïve (a, b) IL6ko mice and those with unilateral sciatic nerve compression (SNC; c–f) or complete sciatic nerve transection (CSNT; g–j) for 7 days. The sections of ipsilateral and contralateral lumbar (DRG-L4i, DRG-L4c) and cervical (DRG-C7i, DRG-C7c) DRG were incubated under the same conditions with rabbit polyclonal antibody specific to Y705-phospho-STAT3 and TRITC-conjugated donkey anti-rabbit secondary antibody. Activated and nuclear translocation of STAT3 (arrowheads) was observed in lumbar DRG ipsilateral (e, i) and contralateral (less intense; f, j) to the sciatic nerve lesion. Scale bars = 30 µm
Results of STAT3(Y705) immunofluorescence intensity measured in the neuronal nuclei of lumbar (L-DRG) and cervical (C-DRG) dorsal root ganglia of naïve, WT and IL-6ko mice. DRG ipsilateral (i) and contralateral (c) to sciatic nerve compression (SNC) or complete sciatic nerve transection (CSNT) were collected after 7 days. *Significant difference (p < 0.05) compared to naïve control, †significant difference (p < 0.05) compared to IL-6ko (Mann–Whitney u test)
The in situ changes in SCG-10 and STAT3(Y705) proteins seen as alterations of immunofluorescence intensity in DRG neurons of unoperated WT and IL-6ko mice and following SNC or CSNT were confirmed by Western blot analysis (Fig. 6). Levels of SCG-10 protein increased bilaterally in both cervical and lumbar DRG of WT mice after SNC and CSNT when compared to DRG from naïve mice. Lumbar DRG ipsilateral to the sciatic nerve lesions showed a greater increase of SCG-10 levels than those from the contralateral side, but this was not statistically significant. The increases in SCG-10 protein levels in cervical DRG from both sides were approximately similar. SCG-10 protein was also bilaterally increased in both lumbar and cervical DRG of IL-6ko mice after SNC or CSNT when compared to naïve mice. Further, CSNT—but not SNC—induced a substantially bigger increase of SCG-10 levels in both lumbar and cervical DRG. Generally, the values of SCG-10 protein were significantly lower in DRG of IL-6ko than WT mice.
Results of Western blot analysis of SCG-10 and STAT3(Y705) protein levels in DRG of L3-L4 (L) and C6-C8 (C) segments collected from ipsilateral (i) and contralateral (c) sides of naïve, SNC- and CSNT-operated mice for 7 days. Upper panels show representative blots of SCG-10 and STAT3(Y705) from DRG of WT and IL6ko mice. Equal loading of proteins was confirmed by actin levels (Actin). Lower panels show densitometry of SCG-10 and STAT3(Y705) protein bands after normalization to actin; the intensities of the SCG-10 and STAT3(Y705) bands from naïve DRG were taken as 1. *Significant difference (p < 0.05) compared to naïve control, †significant difference (p < 0.05) compared to SNC, +significant difference (p < 0.05) compared to WT counterparts (Mann–Whitney u test)
Compared to naïve controls, SNC and CSNT induced a bilateral increase in STAT3(Y705) protein levels in both lumbar and cervical DRG of both WT and IL-6ko mice (Fig. 5). However, the extent of STAT3(Y705) increase in IL-6ko mice was not as strong as in WT. In contrast to WT mice, CSNT induced a more significant elevation of STAT3(Y705) protein than SNC (Fig. 6).
Axon regeneration assay in crushed ulnar nerve after prior sciatic nerve injury in wild-type and IL-6ko mice
We tested initiation of the pro-regenerative state in cervical DRG neurons of WT and IL-6ko mice by monitoring axonal regeneration in longitudinal sections of crushed ulnar nerves after SCG-10 immunostaining. The axon regeneration index was expressed as the longest SCG-10+ axon from the point of nerve crush. The length of SCG-10+ axons was greater in SNC- and CSNT-operated WT mice compared to control WT mice with only ulnar nerve crush (Fig. 7). These results indicate that prior sciatic nerve injury was able to induce increased regeneration capacity in cervical DRG of WT mice.
a Representative sections showing the maximal length of regenerated SCG-10+ axons (arrowheads) distal to the ulnar nerve crush (UNcrush) in WT and IL-6ko mice, unoperated and 7 days following sciatic nerve constriction (SNC) or complete sciatic nerve transection (CSNT). Dashed lines indicate the crush site. Scale bars = 300 µm. b The graph shows the mean length of regenerated SCG-10+ axons ± SD in the ulnar nerve 1 day after crush (UNcrush) in WT and IL-6ko mice without a sciatic nerve injury and 7 days following SNC or CSNT. *Significant difference (p < 0.05) compared to control, ‡significant difference (p < 0.05) compared to WT SNC + UNcrush, †significant difference (p < 0.05) compared to WT counterpart (Mann–Whitney u test)
Generally, the length of the longest SCG-10+ axons distal to ulnar nerve crush was significantly shorter in IL-6ko mice compared to those in WT controls. Besides, we found no significant differences in the length of SCG-10+ regenerated axons in the crushed ulnar nerve of IL-6ko mice with prior SNC or CSNT (Fig. 7).
Discussion
We described previously in a rat model that sciatic nerve lesion induced a temporary upregulation of IL-6 and its receptor not only in DRG of the lumbar (L4–L5) but also in remote DRG of cervical segments (Dubový et al. 2013). Downstream signaling of IL-6 is mediated via activation and nuclear translocation of STAT3 (Aaronson and Horvath 2002; Eulenfeld et al. 2012). Recently, we demonstrated activation and nuclear translocation of STAT3 bilaterally in DRG neurons of both lumbar and cervical segments after unilateral sciatic nerve injury. In addition, increased levels of IL-6 protein were detected in the cerebrospinal fluid (CSF) following sciatic nerve injury and activation of STAT3 was found in cervical DRG after intrathecal injection of IL-6 (Dubový et al. 2018a). Since IL-6 and activated STAT3 participate in initiating the axonal regeneration program (Qiu et al. 2005; Dziennis and Alkayed 2008; Smith et al. 2011; Bareyre et al. 2011; Zigmond 2012b; Quarta et al. 2014), we used IL-6ko mice and compared them to WT mice to see if IL-6 is a potential mediator of the pro-regenerative stage in DRG neurons non-associated with the injured sciatic nerve.
The induction of the regeneration-associated program can be indicated by increased SCG-10 that is also a marker for regenerated sensory axons of injured peripheral nerves (Shin et al. 2014). The DRG neurons of naïve WT and IL-6ko mice displayed a low basal level of SCG-10 that was significantly increased in the neuronal bodies of lumbar DRG ipsilateral to SNC or CSNT. In addition, both types of sciatic nerve lesion in WT mice induced a bilateral elevation of SCG-10 not only in lumbar (L3–L4), but also in cervical DRG (C6–C8). This initiation of the pro-regenerative state in cervical DRG neurons of WT mice by sciatic nerve lesion was also illustrated by STAT3 activation and axon regeneration distal to ulnar nerve crush compared to mice without and with prior SNC or CSNT. These results demonstrate for the first time that the pro-regenerative state of cervical DRG after prior sciatic nerve injury described in rats (Dubový et al. 2019) is also found in the mouse model.
In contrast to WT, sciatic nerve lesions in IL-6ko mice significantly increased SCG-10 and STAT3(Y705) levels only in lumbar DRG neurons ipsilateral to the sciatic nerve injury. However, contralateral DRG neurons and DRG neurons of cervical segments on both sides displayed lower levels of these two proteins. Corresponding to the expected lower activation of STAT3 in cervical DRG neurons of IL-6ko mice, the length of regenerated axons distal to ulnar nerve crush was significantly shorter in IL-6ko than WT mice. These results demonstrate that IL-6 deficiency leads to reduced initiation of the pro-regenerative state in cervical DRG neurons after prior sciatic nerve injury.
The results published regarding a role for IL-6 in activating DRG neurons to regenerate their central afferent branches following conditioning by a peripheral nerve injury are controversial (Cafferty et al. 2004; Cao et al. 2006). In addition, it has been demonstrated that in situ deactivation of IL-6 enhanced peripheral nerve regeneration (Koulaxouzidis et al. 2015). However, a pro-regenerative state in DRG neurons non-associated with the lesioned nerve can be initiated indirectly via CSF of the paraspinal subarachnoid space including DRG along the spinal cord (Joukal et al. 2016). A role for IL-6 in the initiation of the pro-regenerative state in cervical DRG via CSF of the subarachnoid space is also supported by the activation and nuclear translocation of STAT3 after intrathecal injection of IL-6 (Dubový et al. 2018a). Since DRG lack the blood-nerve barrier (Anzil et al. 1976), it is possible that remotely acting IL-6 may also be serum-derived.
Apart from lumbar DRG after CSNT, activation of STAT3 was lower in DRG after SNC of IL-6ko mice compared to WT mice suggesting the involvement of other neuropoietic cytokines including leukemia inhibitory factor (LIF). LIF may also have a role in initiating the pro-regenerative state in DRG neurons associated with peripheral nerve injury (Sun and Zigmond 1996; Cafferty et al. 2001). However, it is still unclear whether LIF upregulated in DRG neurons after nerve injury can be released into the subarachnoid space and subsequently diffuse into remote DRG as has been shown for IL-6.
Conclusion
Monitoring SCG10 and activated STAT3 levels in cervical DRG neurons after prior sciatic nerve lesions in WT and IL-6ko mice revealed a role for IL6 in activating the neuronal regeneration program in DRG neurons non-associated with the injured nerve. This was confirmed by significantly shorter regenerated axons distal to ulnar nerve crush following sciatic nerve lesions in IL-6ko mice compared to WT controls.
References
Aaronson DS, Horvath CM (2002) A road map for those who don’t know JAK-STAT. Science 296:1653–1655. https://doi.org/10.1126/science.1071545
Abe N, Borson SH, Gambello MJ et al (2010) Mammalian target of rapamycin (mTOR) activation increases axonal growth capacity of injured peripheral nerves. J Biol Chem 285:28034–28043. https://doi.org/10.1074/jbc.M110.125336
Anzil AP, Blinzinger K, Herrlinger H (1976) Fenestrated blood capillaries in rat cranio-spinal sensory ganglia. Cell Tissue Res 167:563–567. https://doi.org/10.1007/BF00215185
Bareyre FM, Garzorz N, Lang C et al (2011) In vivo imaging reveals a phase-specific role of STAT3 during central and peripheral nervous system axon regeneration. Proc Natl Acad Sci USA 108:6282–6287. https://doi.org/10.1073/pnas.1015239108
Brázda V, Klusáková I, Hradilová Svíženská I, Dubový P (2013) Dynamic response to peripheral nerve injury detected by in situ hybridization of IL-6 and its receptor mRNAs in the dorsal root ganglia is not strictly correlated with signs of neuropathic pain. Mol Pain 9:42. https://doi.org/10.1186/1744-8069-9-42
Cafferty WBJ, Gardiner NJ, Gavazzi I et al (2001) Leukemia inhibitory factor determines the growth status of injured adult sensory neurons. J Neurosci 21:7161–7170. https://doi.org/10.1523/JNEUROSCI.21-18-07161.2001
Cafferty WBJ, Gardiner NJ, Das P et al (2004) Conditioning injury-induced spinal axon regeneration fails in interleukin-6 knock-out mice. J Neurosci 24:4432–4443. https://doi.org/10.1523/JNEUROSCI.2245-02.2004
Cao Z, Gao Y, Bryson JB et al (2006) The cytokine interleukin-6 is sufficient but not necessary to mimic the peripheral conditioning lesion effect on axonal growth. J Neurosci 26:5565–5573. https://doi.org/10.1523/JNEUROSCI.0815-06.2006
Dubový P, Klusáková I, Svíženská I (2002) A quantitative immunohistochemical study of the endoneurium in the rat dorsal and ventral spinal roots. Histochem Cell Biol 117:473–480. https://doi.org/10.1007/200418-002-0411-5
Dubový P, Brázda V, Klusáková I, Hradilová-Svíženská I (2013) Bilateral elevation of interleukin-6 protein and mRNA in both lumbar and cervical dorsal root ganglia following unilateral chronic compression injury of the sciatic nerve. J Neuroinflamm 10:55. https://doi.org/10.1186/1742-2094-10-55
Dubový P, Hradilová-Svíženská I, Klusáková I et al (2018a) Bilateral activation of STAT3 by phosphorylation at the tyrosine-705 (Y705) and serine-727 (S727) positions and its nuclear translocation in primary sensory neurons following unilateral sciatic nerve injury. Histochem Cell Biol 150:37–47. https://doi.org/10.1007/s00418-018-1656-y
Dubový P, Klusáková I, Hradilová-Svíženská I, Joukal M (2018b) Expression of regeneration-associated proteins in primary sensory neurons and regenerating axons after nerve injury-an overview. Anat Rec 301:1618–1627. https://doi.org/10.1002/ar.23843
Dubový P, Klusáková I, Hradilová-Svíženská I et al (2019) A conditioning sciatic nerve lesion triggers a pro-regenerative state in primary sensory neurons also of dorsal root ganglia non-associated with the damaged nerve. Front Cell Neurosci 13:11. https://doi.org/10.3389/fncel.2019.00011
Dziennis S, Alkayed NJ (2008) Role of signal transducer and activator of transcription 3 in neuronal survival and regeneration. Rev Neurosci 19:341–362. https://doi.org/10.1515/REVNEURO.2008.19.4-5.341
Eulenfeld R, Dittrich A, Khouri C et al (2012) Interleukin-6 signalling: more than JAKs and STATs. Eur J Cell Biol 91:486–495. https://doi.org/10.1016/j.ejcb.2011.09.010
Joukal M, Klusáková I, Dubový P (2016) Direct communication of the spinal subarachnoid space with the rat dorsal root ganglia. Ann Anat 205:9–15. https://doi.org/10.1016/j.aanat.2016.01.004
Koulaxouzidis G, Reim G, Fluhr JW et al (2015) In situ deactivation of interleukin-6 enhances early peripheral nerve regeneration in a murine injury model. J Reconstr Microsurg 31:508–515. https://doi.org/10.1055/s-0035-1555114
Liu K, Tedeschi A, Park KK, He Z (2011) Neuronal intrinsic mechanisms of axon regeneration. Ann Rev Neurosci 34:131–152. https://doi.org/10.1146/annurev-neuro-061010-113723
Mar FM, Simões AR, Rodrigo IS, Sousa MM (2016) Inhibitory injury signaling represses axon regeneration after dorsal root injury. Mol Neurobiol 53:4596–4605. https://doi.org/10.1007/s12035-015-9397-6
Martin SL, Reid AJ, Verkhratsky A et al (2019) Gene expression changes in dorsal root ganglia following peripheral nerve injury: roles in inflammation, cell death and nociception. Neural Regen Res 14:939–947. https://doi.org/10.4103/1673-5374.250566
Mason MRJ, Lieberman AR, Grenningloh G, Anderson PN (2002) Transcriptional upregulation of SCG10 and CAP-23 is correlated with regeneration of the axons of peripheral and central neurons in vivo. Mol Cell Neurosci 20:595–615. https://doi.org/10.1006/mcne.2002.1140
Murphy PG, Grondin J, Altares M, Richardson PM (1995) Induction of interleukin-6 in axotomized sensory neurons. J Neurosci 15:5130–5138. https://doi.org/10.1523/JNEUROSCI.15-07-05130.1995
Qiu J, Cafferty WBJ, McMahon SB, Thompson SWN (2005) Conditioning injury-induced spinal axon regeneration requires signal transducer and activator of transcription 3 activation. J Neurosci 25:1645–1653. https://doi.org/10.1523/JNEUROSCI.3269-04.2005
Quarta S, Baeumer BE, Scherbakov N et al (2014) Peripheral nerve regeneration and NGF-dependent neurite outgrowth of adult sensory neurons converge on STAT3 phosphorylation downstream of neuropoietic cytokine receptor gp130. J Neurosci 34:13222–13233. https://doi.org/10.1523/JNEUROSCI.1209-13.2014
Ronchi G, Raimondo S, Varejão ASP et al (2010) Standardized crush injury of the mouse median nerve. J Neurosci Methods 188:71–75. https://doi.org/10.1016/j.jneumeth.2010.01.024
Shin JE, Miller BR, Babetto E et al (2012) SCG10 is a JNK target in the axonal degeneration pathway. Proc Natl Acad Sci USA 109:E3696–E3705. https://doi.org/10.1073/pnas.1216204109
Shin JE, Geisler S, DiAntonio A (2014) Dynamic regulation of SCG10 in regenerating axons after injury. Exp Neurol 252:1–11. https://doi.org/10.1016/j.expneurol.2013.11.007
Smith RP, Lerch-Haner JK, Pardinas JR et al (2011) Transcriptional profiling of intrinsic PNS factors in the postnatal mouse. Mol Cell Neurosci 46:32–44. https://doi.org/10.1016/j.mcn.2010.07.015
Sugiura Y, Mori N (1995) SCG10 expresses growth-associated manner in developing rat brain, but shows a different pattern to p19/stathmin or GAP-43. Devel Brain Res 90:73–91. https://doi.org/10.1016/0165-3806(96)83488-2
Sun Y, Zigmond RE (1996) Leukaemia inhibitory factor induced in the sciatic nerve after axotomy is involved in the induction of galanin in sensory neurons. Eur J Neurosci 8:2213–2220. https://doi.org/10.1111/j.1460-9568.1996.tb00744.x
Zamboni L, de Martino C (1967) Buffered picric acid-formaldehyde: a new, rapid fixative for electron microscopy. J Cell Biol 35:A148
Zigmond RE (2012a) gp130 cytokines are positive signals triggering changes in gene expression and axon outgrowth in peripheral neurons following injury. Front Mol Neurosci 4:62. https://doi.org/10.3389/fnmol.2011.00062
Zigmond RE (2012b) Cytokines that promote nerve regeneration. Exp Neurol 238:101–106. https://doi.org/10.1016/j.expneurol.2012.08.017
Acknowledgements
We thank Ms. Marta Lněníčková, Ms. Jitka Mikulášková, Mgr. Jana Vachová and Mr. Lumír Trenčanský for their skillful technical assistance.
Funding
This work was supported by Grant no. 16-08508S of The Czech Science Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval
All procedures performed in studies involving animals were in accordance with the ethical standards of the institution or practice at which the studies were conducted.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dubový, P., Hradilová-Svíženská, I., Klusáková, I. et al. Interleukin-6 contributes to initiation of neuronal regeneration program in the remote dorsal root ganglia neurons after sciatic nerve injury. Histochem Cell Biol 152, 109–117 (2019). https://doi.org/10.1007/s00418-019-01779-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00418-019-01779-3