Abstract
Purpose
The goal of this study is to describe characteristics of cataract surgery patients who previously underwent laser in situ keratomileusis/photorefractive keratectomy (LASIK/PRK) in comparison to non-LASIK/PRK cataract surgery patients including psychiatric comorbidities, as well as describe refractive prediction error after cataract surgery while accounting for axial length (AL) using the Barrett True-K and Barrett Universal II formulas.
Methods
This was a retrospective study of patients from the University of Colorado Cataract Outcomes Registry. The primary outcomes were refraction prediction error (RPE), mean absolute RPE, and median absolute RPE. Outcomes were stratified by five axial length groups. Univariate and multivariate models for RPE were stratified by the AL group.
Results
Two hundred eighty-one eyes with prior LASIK/PRK and 3101 eyes without are included in the study. Patients with prior LASIK/PRK were significantly younger: 67.0 vs 69.9 years, p < 0.0001. The LASIK/PRK group had significantly better mean pre-operative BCVA in comparison to the non-LASIK group, logMAR 0.204 vs logMAR 0.288, p = 0.003. The LASIK/PRK group had significantly lower rates of cardiovascular disease (18.5% vs 29.3%, p < 0.001), hypertension (49.1% vs 59.3%, p < 0.012), and type 2 diabetes (10.7% vs 26.0%, p < 0.001), and no significant difference in psychiatric disease. The absolute RPE was higher for the LASIK group for all ALs, but only significantly higher for eyes with AL less than 25 mm.
Conclusion
Patient eyes with prior LASIK/PRK surgery undergoing cataract surgery were significantly younger, had significantly less comorbidities, and a significantly better pre-operative BCVA. Using the Barrett formulas, absolute prediction error for eyes with longer ALs was not significantly worse for LASIK/PRK eyes than those without and the difference was smaller for eyes with longer AL.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.

Introduction
Commonly performed corneal refractive surgeries include photorefractive keratectomy (PRK) and laser in situ keratomileusis (LASIK), which has a 96% postoperative patient satisfaction rate [1]. LASIK offered a revolutionary breakthrough in ophthalmology due to the range of correction available, speed of recovery, and reliability of results [2]. Eventually, patients with prior corneal refractive surgery develop age-related cataracts which require surgical removal.
Patients with prior corneal refractive surgery have particularly increased demands for visual function and uncorrected visual acuity after their corneal refractive surgery and may have similar expectations following their cataract surgery [2, 3]. Despite the wide range of approaches and formulas that have been developed, intraocular lens (IOL) power calculations are less accurate in eyes with prior LASIK and PRK in comparison to previously unoperated eyes, causing an increased risk of refractive surprise [3,4,5,6]. Similarly, IOL power calculations in eyes with extremes of axial length (AL) but without prior refractive surgery are also less accurate making these patients prone to refractive surprise following cataract surgery as well [7, 8]. Previous studies that have assessed refractive outcomes after cataract surgery in patients with prior LASIK/PRK did not control for AL, which is an important confounder.
LASIK and other refractive surgeries have faced media scrutiny despite their proven level of safety and patient satisfaction as there have been anecdotal links to suicidality in unhappy patients [9]. However, psychiatric complications such as depression, suicidal ideation, psychosis, and attempted or completed suicide following or due to LASIK are rare [10]. To date, there is no scientific evidence that LASIK is a risk factor for depression [11]. However, the patient’s perceived postoperative visual result can be impacted by their psychological state [11]. Thus, patients with prior psychiatric diagnosis (such as depression, anxiety, bipolar depression, schizophrenia) may be at an increased risk of subjectively unsatisfactory visual outcomes after cataract surgery. This prompted interest in evaluating whether potentially differing rates of psychiatric disease in patients with and without prior LASIK/PRK may be linked to objectively different visual results following cataract surgery.
The objective of this study is to describe characteristics of cataract surgery patients (including prior psychiatric disorders) who previously underwent LASIK/PRK in comparison to non-LASIK/PRK cataract surgery patients, as well as describe Barrett formula refractive prediction error after cataract surgery while accounting for the important confounder of AL.
Patients and methods
This retrospective study included patient eyes that were part of the University of Colorado Department of Ophthalmology’s Cataract Outcomes Registry from March 2018 through December 2019. The Colorado Multiple Institutional Review Board approved this study (COMIRB#17–0629). Data were collected from patient’s electronic medical records, and the information was entered into a secure cataract outcomes database, described in detail elsewhere [12,13,14]. In brief, each cataract surgery patient had comprehensive review of their medical record. Demographic information, medical and psychiatric history, pre-operative and postoperative findings, and intra-operative and post-operative complications were collected. An additional administrative review of prior diagnosis codes of psychiatric diagnoses (including depression, anxiety, bipolar, post-traumatic stress disorder, schizophrenia, psychosomatic disorder) was performed using ICD-10 codes. Psychiatric diagnoses were identified according to the Diagnostic and Standard Manual of Mental Disorders, Fifth edition [15].
Preoperative biometry including axial length was obtained using the IOLMaster 700 optical biometer (Carl Zeiss Meditec AG), and cataract phacoemulsification surgery was performed using femtosecond laser or standard clear corneal incisions, per surgeon preference. Complex surgery was defined as surgery requiring the use of iris expansion device (Malyugin ring, iris hooks, or stretch pupilloplasty), capsular tension ring, or dye staining of the anterior capsule due to poor visualization. Postoperative refractions were collected at the visit with the best-corrected visual acuity (BCVA) between 3 and 26 weeks following cataract surgery. Refraction prediction for the IOL implanted in patients without prior LASIK/PRK was retrospectively calculated using the Barrett Universal II formula version 1.05 (https://calc.apacrs.org/barrett_universal2105/). Using the Barrett True-K No History formula version 2.5, refraction prediction for IOL implanted in patients with prior LASIK/PRK was calculated (https://calc.apacrs.org/Barrett_True_K_Universal_2105/). The myopic LASIK/PRK option within the calculator was used for those with myopic LASIK/PRK, and the hyperopic LASIK/PRK option was used for those with prior hyperopic LASIK/PRK. Refraction prediction error was calculated as actual postoperative refraction minus formula predicted refraction.
Exclusion criteria included patients less than 18 years of age, eyes with traumatic cataract, prior ocular surgery other than LASIK/PRK, prior radial keratotomy, combined ocular surgery, and eyes with post-operative BCVA of was worse than 20/40. Eyes with poor visual acuities were excluded to maximize the accuracy of utilized refractions as refraction accuracy decreases with visual acuity [16].
Statistical analysis
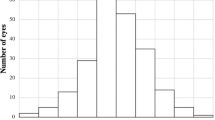
Information was collected from patients with one or both eyes included in the database. Frequencies and percentages for patient eyes with prior LASIK/PRK and non-LASIK/PRK eyes are presented. The two groups were compared using linear and logistic regressions with general estimating equations to account for intrasubject correlation. The primary outcome of refraction prediction error (RPE) was calculated as mean refraction prediction error (RPE) and standard deviation, mean (MAE) and median absolute refraction prediction error (MedAE), and standard deviation stratified by five axial length groups (< 23 mm, 23 to < 24 mm, 24 to < 25 mm, 25 to < 26 mm, and 26 + mm). Multivariable regression models were performed to adjust for factors that were significantly different between LASIK and non-LASIK patient eyes and associated with RPE. Univariate and multivariate models for RPE were stratified by axial length group. p values less than 0.05 were considered statistically significant. The SAS software (version 9.4, SAS Institute, Inc) was used for statistical analysis.
Results
Eyes (3382) were included in the study: 281 LASIK/PRK eyes and 3101 non-LASIK/PRK eyes. Patient characteristics and select clinical characteristics (including psychiatric diagnosis) are shown in Table 1. Patients with prior LASIK/PRK were significantly younger than non-LASIK/PRK patients: 67.0 ± 8.4 versus 69.9 ± 9.5 years, p < 0.0001. Black/African American and Hispanic patients had significantly lower rates of LASIK/PRK in comparison to Caucasian patients, both p < 0.0001. Patients with prior LASIK/PRK were more likely to have private insurance and less likely to have Medicare, Medicaid, or to be uninsured. Furthermore, patients with LASIK/PRK had significantly lower rates of cardiovascular disease (p = 0.001), type 2 diabetes (p < 0.0001), and treatment for chronic hypertension (p = 0.012). Overall, patients with LASIK/PRK had a slightly higher rate of any psychiatric diagnosis (18.2%) in comparison to patients with non-LASIK/PRK (16.4%), but the difference was not statistically significant (p = 0.58).
Table 2 presents the ocular characteristics in the LASIK/PRK versus non-LASIK/PRK groups. Eyes in the LASIK/PRK group had significantly better mean pre-operative BCVA, 0.204 ± 0.24 logMAR (Snellen equivalent: 20/32), in comparison to the non-LASIK/PRK group with a pre-operative best-corrected VA 0.288 ± 0.37 logMAR (Snellen equivalent: 20/39), p = 0.003. There were no significant differences in spherical equivalent of pre-operative refraction, and post-operative BCVA between the two groups. There was a significant difference in AL between the LASIK/PRK and non-LASIK/PRK groups: 25.4 ± 1.6 mm versus 24.1 ± 1.4 mm respectively, p < 0.0001. However, when stratified by the five AL groups, mean and median ALs were statistically similar between the LASIK/PRK and non-LASIK/PRK groups for each of the five defined AL groups
Table 3 shows ocular comorbidities, characteristics of surgery, and surgical complications. LASIK/PRK patient eyes were significantly less likely to have a history of pseudoexfoliation (0.4% versus 1.3%, p = 0.012) and diabetic retinopathy (0.7% versus 7.0%, p < 0.0001). Furthermore, for patients with diabetes, the rate of retinopathy was 2/30 (6.7%) in the LASIK/PRK patients versus 217/806 (27%) in the non-LASIK/PRK patients, p = 0.0008. In addition, LASIK/PRK eyes had significantly fewer complex surgeries in comparison to non-LASIK/PRK eyes, 7.8% and 15.2%, respectively, p = 0.0001. There was no significant difference in overall rate of surgical complications between the two groups
Refractive surprise using the Barrett Universal II and Barrett True-K formulas stratified by AL group is shown in Table 4. There were 721 eyes that were missing RPE and are not included. There were no significant differences in RPE between the LASIK/PRK and non-LASIK/PRK eyes in any of the axial length groups. However, absolute RPEs were higher in all of the LASIK/PRK groups in comparison to the non-LASIK/PRK groups, and significantly higher for three of our AL subgroups with smaller AL: 24 ≤ AL < 25 mm (0.662D versus 0.409D, p = 0.033), 23 ≤ AL < 24 mm (0.787D versus 0.400D, p = 0.027), and AL < 23 mm (1.079D versus 0.439D, p < 0.0001). Multivariable models for each of these AL groups were also adjusted (data not shown) for potential confounding variables of type 2 diabetes, baseline BCVA, and complex surgery. However, these potential confounders had very little effect on the main association and did not impact the significance.
Discussion
In this study, we compared the characteristics and visual outcomes of phacoemulsification cataract surgery in patients with prior LASIK/PRK and patients without history of LASIK/PRK. Patients with prior LASIK/PRK were significantly younger and had a significantly lower rate of cardiovascular disease, chronic hypertension, and diabetes. Furthermore, patients with prior LASIK/PRK had significantly better pre-operative BCVA, a significantly lower rate of complex cataract surgery, and a significantly higher MAE for refraction prediction error among eyes with axial lengths less than 25 mm using the Barrett formulas. There was no significant difference in rate of pre-operative psychiatric medical conditions between the two groups so further associations between psychiatric illness and visual outcomes were not pursued.
Our findings are similar to Manning et al., who reported that patients with prior LASIK/PRK were significantly younger and had better pre-operative BCVA in comparison to controls [3]. The LASIK/PRK patients in this study also had significantly less complex cataract cases in comparison to non-LASIK/PRK patients. It is possible that patients with prior refractive surgery have a lower tolerance for visual symptoms due to cataract and will seek help sooner in comparison to patients with no-prior refractive surgery [3]. Another explanation for the significantly younger age in LASIK/PRK patients is that due to a combination of photo-oxidative and acoustic stress, corneal surgery is cataractogenic [3]. Additionally, patients with prior LASIK/PRK may request cataract surgery earlier, not because of visual symptoms, but to reverse the lenticular myopic shifts (and subsequent ametropia) to maintain or restore their refractive status and spectacle independence gained following LASIK/PRK [3].
In our cohort, Black/African American and Hispanic patients had significantly lower rates of LASIK/PRK in comparison to Caucasian patients. To our knowledge, there are no reports evaluating racial disparities in refractive surgery nationally or worldwide. However, a recent study from Best et al. reported that racial disparities persist among the use of surgical procedures in the USA regardless of insurance status, hospital teaching status, and US census division [17]. Several reasons for this disparity have been proposed including decreased access to care and Black patients’ avoidance of seeking medical care out of fear of discrimination, amongst other social and systemic factors [17]. Thus, it is possible that the lower rate of LASIK/PRK in our cohort is a reflection of a nationwide racial disparity in surgical procedure use. The cohort of patients with prior LASIK/PRK in our study was more likely to have private insurance and less likely to have Medicaid, Medicare, or to be uninsured. Also, patients with LASIK/PRK in our cohort had significantly lower rates of cardiovascular disease, treatment for chronic hypertension, and type 2 diabetes. Previous studies have shown low socioeconomic status to be significantly associated with higher risk of developing cardiovascular disease and type 2 diabetes [18, 19]. Differences in cardiovascular disease and diabetes persisted even after adjustment for age and race/ethnicity which is likely reflective of differences in socioeconomic status of patients that can afford LASIK/PRK. Furthermore, for the patients with diabetes in our cohort, diabetic retinopathy was significantly higher in the non-LASIK/PRK group in comparison to the LASIK/PRK, which may also reflect unmeasured socioeconomic factor differences among patients who developed diabetes among each of the groups.
Prior studies have demonstrated that eyes with AL < 22 mm or > 24.5 or 25 mm have shown worse refractive outcomes after cataract surgery compared to eyes with more average AL [20, 21]. In our study, the three groups with the shortest axial lengths (< 23 mm, 23 to < 24 mm, and 24 to < 25 mm), patients with prior LASIK/PRK suffered larger refractive surprises using the Barrett True-K formula in comparison to non-LASIK/PRK patient eyes using the Barrett Universal II formula, p < 0.0001, p = 0.023, and p = 0.033, respectively. However, there was no statistical difference in MAE/MedAE between the LASIK/PRK and non-LASIK/PRK groups with longer axial lengths (25 mm or greater), and these groups also had the smallest magnitude difference in MAE and MedAE between groups. This finding is important, as existing reports on refractive errors in patients with prior corneal refractive surgery largely implicate the altered corneal curvature as a result of the prior refractive procedure as the reason for the higher rate of refractive error [4]. Our data demonstrates that when using the Barrett formulas for eyes with long axial length (> 25 mm), refraction prediction error is more similar between eyes that have and have not had prior LASIK/PRK. This suggests that long axial length and its association with unpredictable refractive predictions may be contributing more strongly to the refractive error than previously expected.
Because we did not find any significant difference in psychiatric history between the LASIK/PRK and the non-LASIK/PRK patients, we did not further pursue whether differences in objective visual outcomes between the two groups varied by psychiatric diagnosis state. Existing literature reports no association between LASIK and depression [11] or between patients getting PRK and increased anxiety/distress [22]. A cohort study by Chen et al. showed that patients with cataracts have a higher risk of developing depression, compared to non-cataract controls, after adjusting for cofounders [23]. In addition, the risk of depression is significantly lower in patients who undergo cataract surgery in comparison to those who do not undergo surgery [23].
While the retrospective nature of this study allowed for a larger sample size than might be otherwise unattainable, it is also a limitation. Another limitation is the sample sizes in some of our AL groups, which may have been too small to detect statistically significant differences. Furthermore, the data on medical and/or psychiatric comorbidities might be incomplete since we collected diagnosis from the patient chart retrospectively and it is possible patients may seek care with providers in other institutions and information may have not been in our electronic medical record system. Another limitation is our database did not collect information about socio-economic status, and therefore have no data on this parameter, but we do include data on insurance status. Thus, there may be some unmeasured difference in our two study groups that we cannot account for.
In conclusion, our study shows that patients with prior LASIK/PRK surgery undergoing cataract surgery are significantly younger and have significantly fewer comorbidities such as chronic hypertension, diabetes, and cardiovascular disease. These patients also have a significantly better pre-operative BCVA, but post-operative BCVA was similar to non-LASIK/PRK patients. For the AL groups less than 25 mm, patients with prior LASIK/PRK had higher Barrett True-K absolute refractive prediction errors following cataract surgery than those without prior LASIK/PRK when using the Barrett Universal II formula. However, for eyes in the longer AL groups, the difference in absolute prediction errors between LASIK/PRK eyes and non-LASIK/PRK eyes was smaller than for shorter eyes and the difference did not reach statistical significance. This is a novel finding in that refractive prediction errors using the Barrett formulas for these eyes with AL greater than 25 mm did not become significantly worse in the setting of prior LASIK/PRK as expected, indicating that LASIK/PRK may not affect refractive prediction accuracy as much in long eyes.
References
Eydelman M, Hilmantel G, Tarver ME, Hofmeister EM, May J, Hammel K, Hays RD, Ferris F 3rd (2017) Symptoms and satisfaction of patients in the Patient-Reported Outcomes With Laser In Situ Keratomileusis (PROWL) studies. JAMA Ophthalmol 135:13–22. https://doi.org/10.1001/jamaophthalmol.2016.4587
Hamilton DR, Hardten DR (2003) Cataract surgery in patients with prior refractive surgery. Curr Opin Ophthalmol 14:44–53. https://doi.org/10.1097/00055735-200302000-00008
Manning S, Barry P, Henry Y, Rosen P, Stenevi U, Lundstrom M (2015) Cataract surgery outcomes in corneal refractive surgery eyes: study from the European Registry of Quality Outcomes for Cataract and Refractive Surgery. J Cataract Refract Surg 41:2358–2365. https://doi.org/10.1016/j.jcrs.2015.04.034
Wang L, Koch DD (2021) Intraocular lens power calculations in eyes with previous corneal refractive surgery: review and expert opinion. Ophthalmology 128:e121–e131. https://doi.org/10.1016/j.ophtha.2020.06.054
Lundstrom M, Dickman M, Henry Y, Manning S, Rosen P, Tassignon MJ, Young D, Stenevi U (2018) Risk factors for refractive error after cataract surgery: analysis of 282 811 cataract extractions reported to the European Registry of Quality Outcomes for cataract and refractive surgery. J Cataract Refract Surg 44:447–452. https://doi.org/10.1016/j.jcrs.2018.01.031
Christopher KL, Patnaik JL, Miller DC, Lynch AM, Taravella MJ, Davidson RS (2021) Accuracy of intraoperative aberrometry, Barrett True-K with and without posterior cornea measurements, Shammas-PL, and Haigis-L formulas after myopic refractive surgery. J Refract Surg 37:60–68. https://doi.org/10.3928/1081597X-20201030-02
Zaldivar R, Shultz MC, Davidorf JM, Holladay JT (2000) Intraocular lens power calculations in patients with extreme myopia. J Cataract Refract Surg 26:668–674. https://doi.org/10.1016/s0886-3350(00)00367-9
Jung KI, Yang JW, Lee YC, Kim SY (2012) Cataract surgery in eyes with nanophthalmos and relative anterior microphthalmos. Am J Ophthalmol 153(1161–1168):e1161. https://doi.org/10.1016/j.ajo.2011.12.006
Eisenbeisz HC, Kudrna JJ, Greenwood M, Garry MT (2021) Corneal refractive surgery in the right patient at the right time. S D Med 74:358–362
Salimi A, Ing E, Nianiaris N (2020) Suicide and laser refractive surgery. J Ophthalmic Vis Res 15:432–434. https://doi.org/10.18502/jovr.v15i3.7464
Dell SJ, Schallhorn SC, Slade SG (2008) Linking Depression and LASIK. Cataract and Refractive Surgery Today 2008. https://crstoday.com/articles/2008-jun/crst0608_02-php/
Miller DC, Patnaik JL, Palestine AG, Lynch AM, Christopher KL (2020) Cataract surgery outcomes in human immunodeficiency virus positive patients at a tertiary care academic medical center in the United States. Ophthalmic Epidemiol: 1–8 https://doi.org/10.1080/09286586.2020.1866021
Manoharan N, Patnaik JL, Bonnell LN, SooHoo JR, Pantcheva MB, Kahook MY, Wagner BD, Lynch AM, Seibold LK (2018) Refractive outcomes of phacoemulsification cataract surgery in glaucoma patients. J Cataract Refract Surg 44:348–354. https://doi.org/10.1016/j.jcrs.2017.12.024
Fonteh CN, Patnaik JL, Grove NC, Lynch AM, Christopher KL (2022) Predictors of pseudophakic retinal tears at a tertiary care academic medical center. Ophthalmol Retina. https://doi.org/10.1016/j.oret.2022.01.010
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders, 5th edn. https://doi.org/10.1176/appi.books.9780890425596
Hoffer KJ, Aramberri J, Haigis W, Olsen T, Savini G, Shammas HJ, Bentow S (2015) Protocols for studies of intraocular lens formula accuracy. Am J Ophthalmol 160(403–405):e401. https://doi.org/10.1016/j.ajo.2015.05.029
Best MJ, McFarland EG, Thakkar SC, Srikumaran U (2021) Racial disparities in the use of surgical procedures in the US. JAMA Surg 156:274–281. https://doi.org/10.1001/jamasurg.2020.6257
Franks P, Winters PC, Tancredi DJ, Fiscella KA (2011) Do changes in traditional coronary heart disease risk factors over time explain the association between socio-economic status and coronary heart disease? BMC Cardiovasc Disord 11:28. https://doi.org/10.1186/1471-2261-11-28
Connolly V, Unwin N, Sherriff P, Bilous R, Kelly W (2000) Diabetes prevalence and socioeconomic status: a population based study showing increased prevalence of type 2 diabetes mellitus in deprived areas. J Epidemiol Community Health 54:173–177. https://doi.org/10.1136/jech.54.3.173
de Juan V, Martin R, Perez I, Herreras JM (2010) Influence of axial length in refractive outcome after cataract surgery. Arch Soc Esp Oftalmol 85:144–148
Mohammadi SF, Hashemi H, Mazouri A, Rahman AN, Ashrafi E, Mehrjardi HZ, Roohipour R, Fotouhi A (2015) Outcomes of cataract surgery at a referral center. J Ophthalmic Vis Res 10:250–256. https://doi.org/10.4103/2008-322X.170358
Kidd B, Stark C, McGhee CN (1997) Screening for psychiatric distress and low self-esteem in patients presenting for excimer laser surgery for myopia. J Refract Surg 13:40–44. https://doi.org/10.3928/1081-597X-19970101-11
Chen PW, Liu PP, Lin SM, Wang JH, Huang HK, Loh CH (2020) Cataract and the increased risk of depression in general population: a 16-year nationwide population-based longitudinal study. Sci Rep 10:13421. https://doi.org/10.1038/s41598-020-70285-7
Funding
This work was supported by the Research to Prevent Blindness grant to the Department of Ophthalmology, Grant Number UL1 TR002535.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of University of Colorado Department of Ophthalmology’s and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study. This study was approved by the Colorado Multiple Institutional Review Board (COMIRB#17–0629).
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fonteh, C.N., Patnaik, J.L., Grove, N.C. et al. Refractive outcomes using Barrett formulas and patient characteristics of cataract surgery patients with and without prior LASIK/PRK. Graefes Arch Clin Exp Ophthalmol 262, 2937–2944 (2024). https://doi.org/10.1007/s00417-024-06456-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-024-06456-3