Abstract
Purpose
The study aims to observe the spontaneous remission of posterior vitreous detachment (PVD)-type vision degrading myodesopsia (VDM) during long-term follow-up.
Methods
We retrospectively reviewed VDM patients with PVD type that refused any treatment. The ratio and time of significant spontaneous remission of floater symptoms occurring were described. The associated factors with significant remission of floater symptoms were analyzed in the univariate and multivariate logistic regression analyses.
Results
In total, 179 patients with VDM were assessed. The mean age of all patients was 60.56 ± 0.47 years old, and the mean duration of follow-up was 23.89 ± 6.63 months. Of the patients, 40.78% have significant improvement in their floater symptoms after mean 16.55 ± 10.63-month follow-up. Myopia (OR = 0.280, 95% CI = 0.084–0.932, P = 0.038), the number of floaters > 3 (OR = 0.343, 95% CI = 0.172–0.683, P = 0.002), and floaters with string-like pattern (OR = 0.370, 95% CI = 0.166–0.824, P = 0.015) and blocky pattern (OR = 0.299, 95% CI = 0.090–0.993, P = 0.049) were negatively correlated with the significant spontaneous remission of VDM symptoms in the multiple binary logistic regression analysis.
Conclusions
Approximately 40% of VDM patients with PVD may experience significant spontaneous remission during long-term follow-up. Patients that are non-myopic and with fewer floaters are more likely to feel relief from VDM symptoms. Floaters with string-like or blocky patterns are less likely to undergo spontaneous remission.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction

Adults are increasingly afflicted with vision degrading myodesopsia (VDM) due to the aging of the population and the prevalence of myopia worldwide [1]. VDM may manifest as spots, cobwebs, shadows, and other assorted shapes as the eyes move [2, 3]. Although many studies show that YAG (yttrium–aluminum garnet) laser vitreolysis and vitrectomy for VDM are effective [4,5,6,7,8], the associated complications should be considered [9]. Observation is still the major process for VDM. While patients may become accustomed and neuroadapt to their floaters, especially the posterior vitreous detachment (PVD) type due to the Weiss ring migrating anteriorly and away from the visual axis gradually [10, 11]. However, the duration of symptoms and likelihood of spontaneous remission remain uncertain.
This study described the ratio and time of spontaneous remission of VDM patients with PVD type during long-term follow-up. Additionally, associated factors with significant spontaneous remission of VDM symptoms were explored.
Methods
Study population
This retrospective cohort study was conducted on patients with VDM of PVD type who refused any treatment process at He Eye Specialist Hospital. The study design adhered to the Declaration of Helsinki principles and was approved by He Eye Specialist Hospital’s Institutional Review Board. Written informed consent was waived due to the retrospective design. The patients whose initial visits occurred between January 2019 and December 2020 were collected. All patients were followed for at least 12 months after their floater symptoms first appeared. Exclusion criteria were (1) secondary vitreous floaters such as vitreous inflammation or hemorrhage and (2) patients undergoing other intraocular surgery that might disturb vitreous condition such as cataract or glaucoma surgeries during follow-up; however, pseudophakic eyes at the initial visits were included. If patients had floaters in both eyes, the eye with the more severe symptoms was chosen.
Ophthalmological examination
All patients underwent a slit-lamp examination, visual acuity, intraocular pressure, refractive status, vitreous and fundus examinations with a dilated pupil, and an ultrasound B scan. Some patients were examined with an ultrawide-field scanning laser ophthalmoscope (Optos® 200Tx, Optos®, Dunfermline, UK) to assist peripheral retinal screening at baseline. Optos images were not employed for floater evaluation in this study. Patients had a thorough fundus examination to look for Weiss ring or detached hyaloid. The Weiss ring should be visible under mydriasis at the optic nerve head and/or the posterior hyaloid was separated via B-scan ultrasound imaging [12]. All ultrasound B-scans were performed at baseline by one doctor (Q. L.).
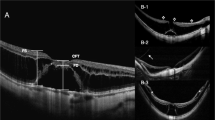
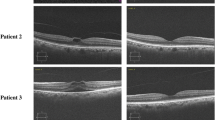
Data collection
The baseline demographic data collected from each patient’s record included age, sex, and laterality of involved eye. The sketch of floaters was shown to patients based on the drawing in previous articles [13, 14] (Fig. 1). The patterns of floaters were classified as spotty, string-like, lamelliform, blocky, and cloudy. All patients individually choose the pattern that closely resembled their visual floater symptoms. The number (≤ 3 or > 3) of floaters reported by patients were also recorded. Primary outcome measures included a subjective improvement (from 0 to 100%) and a five-level qualitative scale described by Delaney et al. [15] at the final visit. The significant remission was defined as the remission of 50% or greater.
Statistical analysis
Continuous values were described using the mean and standard deviation (SD), while categorical variables were represented using percentages. The Kaplan–Meier survival curve was generated for survival analysis. Multiple binary logistic regression and univariate analysis were utilized to identify risk factors related to significant spontaneous remission. For this investigation, the alpha level was set at 0.05 and the power of the statistic was established at 95%. SPSS (SPSS Inc., USA), version 27.0, was used to conduct all statistical analyses.
Results
This study included 179 patients, three of whom underwent retinal laser photocoagulation due to peripheral retinal tears on their initial visit but did not receive any treatment for floaters. In total 548 patients were not treated for floaters, and 367 patients with follow-up periods of less than 12 months or patients lost during follow-up were excluded, along with 2 patients who underwent cataract surgery during follow-up period (Fig. 2). The mean age of all patients was 60.56 ± 0.47 years, with a distinct female predominance (74.86%), and a mean follow-up duration was 23.89 ± 6.63 months. Among the total patients included in this study, 46.39% (n = 83) of the patients had Optos images assessment at baseline. Of the patients, 40.78% had significantly spontaneous remission in their floater symptoms after 16.55 ± 10.63 months (Table 1; Fig. 3). Of these patients, 40.67% experienced remission of floater symptoms within the first year. The Kaplan–Meier survival curve is shown in Fig. 4.
In the univariate analysis, age (OR = 1.036, 95% CI = 1.002–1.071, P = 0.040), myopia (OR = 0.235, 95% CI = 0.077–0.716, P = 0.011), number of floaters > 3 (OR = 0.374, 95% CI = 0.199–0.706, P = 0.002), and floaters with a string-like pattern (OR = 0.370, 95% CI = 0.166–0.824, P = 0.015) and cloudy pattern (OR = 0.087, 95% CI = 0.011–0.717, P = 0.023) correlated with significant spontaneous remission. In the multiple binary logistic regression analysis, myopia (OR = 0.280, 95% CI = 0.084–0.932, P = 0.038), the number of floaters > 3 (OR = 0.343, 95% CI = 0.172–0.683, P = 0.002), and floaters with string-like pattern (OR = 0.370, 95% CI = 0.166–0.824, P = 0.015) and blocky pattern (OR = 0.299, 95% CI = 0.090–0.993, P = 0.049) were negatively correlated with the significant spontaneous remission of VDM symptoms (Table 2). Significant spontaneous remission was observed in 53.4% and 52.0% of patients with spotty floaters and lamelliform floaters, respectively. Although only one patient with cloudy floaters had a significant spontaneous remission (Fig. 5).
There were four (2.23%) patients who complained of the floater symptoms becoming worse during follow-up (Fig. 3), including two patients with cloudy floaters, one patient with string-like floaters, and one patient with lamelliform floaters. No patients had additional complications associated with floaters, such as retinal detachment, retinal holes, or vitreous hemorrhage during follow-up.
Discussion
In this study, 75 percent of the patients were female suggesting that VDM is more prevalent among women. Interestingly, we discovered that previous prospective studies enrolled more female patients with floater (59–76%) [4,5,6,7]. Chuo et al. [16] discovered that the female had twice the change in posterior vitreous detachment (PVD) as the male patients, and that there was a clear and continuous link between PVD and a history of menopause, regardless of age and myopia. They postulated that perimenopausal hormone changes would affect the vitreous collagen or vitreoretinal interface because hormonal changes could affect glycosaminoglycan synthesis and metabolism [17, 18].
Though the YAG laser has been used for treating symptomatic floaters for nearly three decades [19], there is still some debate about its efficacy and safety [3, 7, 20,21,22,23,24]. In some prospective studies, the subjective efficacy of YAG laser vitreolysis for SVO was between 53 and 77% [4,5,6]. It is interesting to note that Shah and Heier [25] found the efficacy of YAG vitreolysis at 6 months (53%), sustained at 2.3 years (50%) in an observational extension study, but three of 35 patients undergoing YAG laser vitreolysis without retinal tears at the 6-month visit had retinal tear at the final visit (2.3 years). The other associated factors with YAG laser vitreolysis such as focal cataract, elevation of IOP, retinal hemorrhage, or retinal detachment were also reported previously [26]. Pars plana vitrectomy is another primary treatment option for VDM [10, 27,28,29]. While vitrectomy has been documented in reducing the symptoms of floaters and is considered to be an effective option but may lead to additional side effects [30, 31]. In 17,615 eyes undergoing vitrectomy for vitreous opacities in the Intelligent Research in Sight Registry, 12.4% eyes returned to the operating room for cataract surgery, and 3.7% eyes returned to the operating room for a non-cataract procedure within 1 year [32].
When complete PVD occurs, the projections of vitreous opacities on the retina are usually dark because of the elevated hyaloid near the retina [33]. During follow-up, the vitreous floaters usually move anterior and peripheral, which makes the shadows of floaters disperse and light [33], so the patients may feel the floater symptoms spontaneously improved. There are a few studies that have assessed spontaneous remission of floater symptoms so far. In this study, we found that 40 percent of patients reported their floater symptoms gradually going into significant spontaneous remission during long-term follow-up and that remission would occur in about 40% of patients within the first year. Even though the ratio of spontaneous remission in PVD-type floaters appears to be high in this study, we were unable to compare it to interventions like YAG laser vitreolysis and PPV surgery. In an interesting finding, a survey of websites about how to treat vitreous floaters found that the most common advice was observation (55.8%), followed by laser treatment (27.6%), no specific advice (11.3%), and vitrectomy (5.8%) [34]. Previously, it was assumed that floaters were usually stable if their symptoms persisted for longer than 3–6 months, so patients with floater symptoms that lasted at least 3–6 months were often chosen in previous intervention studies [4,5,6]. Based on the results of this study, the intervention treatment should be given to people who have had VDM symptoms for at least 1 year.
In this study, myopia was found to be an unfavorable factor associated with spontaneous remission of floater symptoms. The possible reason could be that the types of floaters in these myopic eyes are not only due to PVD but may also be accompanied by some collagen aggregates. Studies have shown that myopia is linked to the clumping of collagen in the vitreous, and these floaters usually constant and persistent [35]. Patients with a few floaters (≤ 3) have approximately triple the chance of significant spontaneous remission compared to patients with more floaters (> 3). Interestingly, we also found that patients with spotty and lamelliform floaters were easier to undergo spontaneous remission, and more than half the patients underwent significant spontaneous remission. The possible explanation is that fewer and smaller floaters are more likely to be overlooked by patients and possibly undergo neuroadaptation. Although large floaters, such as cloudy floaters, are difficult to neglect, in this study, only one patient with cloudy floaters experienced a significant spontaneous remission.
A pooled data analysis recently revealed that the presence of isolated floaters had a great risk of developing retinal tears (16.5% of total eyes), but that risk decreased to 3.9% at follow-up (4–8 weeks) [36]. van Overdam et al. [37] hypothesized that retinal tear forms more quickly following the onset of symptoms. In the present investigation, three patients with peripheral retinal tears at baseline were treated with retinal laser photocoagulation, and no additional retinal tears or detachments were discovered throughout the long-term follow-up. Consequently, observation is probably the safest strategy.
There are several limitations to the current study, including its retrospective design and single-center study. The visual function questionnaire was not used to evaluate the change in visual quality either. We identified a few factors associated with spontaneous remission of floaters and formulated a number of hypotheses, but we lacked objective measurements of floaters to determine if they were real position shifting, population reduction, or neural adaptation. But to the best of our knowledge, this is the first study to report the spontaneous remission of VDM.
In conclusion, approximately 40 percent of VDM patients with the PVD type may feel their floater symptoms improve significantly during long-term observation. Observation is advisable in patients with symptomatic floaters after acute PVD. Fewer and smaller floaters are more likely to get spontaneous remission in non-myopia patients.
Data availability
Raw data will be available upon request.
References
Webb BF, Webb JR, Schroeder MC et al (2013) Prevalence of vitreous floaters in a community sample of smartphone users. Int J Ophthalmol 6:402–405
Milston R, Madigan MC, Sebag J (2016) Vitreous floaters: etiology, diagnostics, and management. Surv Ophthalmol 61:211–227
Broadhead GK, Hong T, Chang AA (2020) To treat or not to treat: management options for symptomatic vitreous floaters. Asia Pac J Ophthalmol (Phila) 9:96–103
Shah CP, Heier JS (2017) YAG laser vitreolysis vs sham YAG vitreolysis for symptomatic vitreous floaters: a randomized clinical trial. JAMA Ophthalmol 135:918–923
Ludwig GD, Gemelli H, Nunes GM et al (2021) Efficacy and safety of Nd:YAG laser vitreolysis for symptomatic vitreous floaters: a randomized controlled trial. Eur J Ophthalmol 31:909–914
Lin T, Li T, Zhang X et al (2022) The efficacy and safety of YAG laser vitreolysis for symptomatic vitreous floaters of complete PVD or non-PVD. Ophthalmol Ther 11:201–214
Souza CE, Lima LH, Nascimento H et al (2020) Objective assessment of YAG laser vitreolysis in patients with symptomatic vitreous floaters. Int J Retina Vitreous 21(6):1
García BG, Orduna Magán C, Alvarez-Peregrina C et al (2020) Nd:YAG laser vitreolysis and health-related quality of life in patients with symptomatic vitreous floaters. Eur J Ophthalmol 7:11206721211008036
Ryan EH (2021) Current treatment strategies for symptomatic vitreous opacities. Curr Opin Ophthalmol 32:198–202
Schulz-Key S, Carlsson JO, Crafoord S (2011) Longterm follow-up of pars plana vitrectomy for vitreous floaters: complications, outcomes and patient satisfaction. Acta Ophthalmol 89:159–165
Shah CP, Fine HF (2018) Management of floaters. Ophthalmic Surg Lasers Imaging Retina 49:388–391
Wang MD, Truong C, Mammo Z et al (2021) Swept source optical coherence tomography compared to ultrasound and biomicroscopy for diagnosis of posterior vitreous detachment. Clin Ophthalmol 15:507–512
Tassignon MJ, Ní Dhubhghaill S, Ruiz Hidalgo I et al (2016) Subjective grading of subclinical vitreous floaters. Asia Pac J Ophthalmol (Phila) 5(2):104–109
van Overdam KA, Bettink-Remeijer MW, Klaver CC et al (2005) Symptoms and findings predictive for the development of new retinal breaks. Arch Ophthalmol 123(4):479–484
Delaney YM, Oyinloye A, Benjamin L (2002) Nd:YAG vitreolysis and pars plana vitrectomy: surgical treatment for vitreous floaters. Eye (Lond) 16:21–26
Chuo JY, Lee TY, Hollands H et al (2006) Risk factors for posterior vitreous detachment: a case-control study. Am J Ophthalmol 142:931–937
Smith TJ (1984) Dexamethasone regulation of glycosaminoglycan synthesis in cultured human skin fibroblasts. Similar effects of glucocorticoid and thyroid hormones. J Clin Invest 74:2157–2163
Smith TJ, Murata Y, Horwitz AL et al (1982) Regulation of glycosaminoglycan synthesis by thyroid hormone in vitro. J Clin Invest 70:1066–1073
Tsai WF, Chen YC, Su CY (1993) Treatment of vitreous floaters with neodymium YAG laser. Br J Ophthalmol 77:485–488
Su D, Shah CP, Hsu J (2020) Laser vitreolysis for symptomatic floaters is not yet ready for widespread adoption. Surv Ophthalmol 65:589–591
Katsanos A, Tsaldari N, Gorgoli K et al (2020) Safety and efficacy of YAG laser vitreolysis for the treatment of vitreous floaters: an overview. Adv Ther 37:1319–1327
Singh IP (2020) Modern vitreolysis-YAG laser treatment now a real solution for the treatment of symptomatic floaters. Surv Ophthalmol 65:581–588
Ivanova T, Jalil A, Antoniou Y et al (2016) Vitrectomy for primary symptomatic vitreous opacities: an evidence-based review. Eye (Lond) 30:645–655
Nguyen JH, Nguyen-Cuu J, Yu F et al (2019) Assessment of vitreous structure and visual function after neodymium:yttrium-aluminum-garnet laser vitreolysis. Ophthalmology 126:1517–1526
Shah CP, Heier JS (2020) Long-term follow-up of efficacy and safety of YAG vitreolysis for symptomatic weiss ring floaters. Ophthalmic Surg Lasers Imaging Retina 51:85–88
Hahn P, Schneider EW, Tabandeh H et al (2017) Reported complications following laser vitreolysis. JAMA Ophthalmol 135:973–976
de Nie KF, Crama N, Tilanus MA et al (2013) Pars plana vitrectomy for disturbing primary vitreous floaters: clinical outcome and patient satisfaction. Graefes Arch Clin Exp Ophthalmol 251:1373–1382
Mason JO 3rd, Neimkin MG, Mason JO 4th et al (2014) Safety, efficacy, and quality of life following sutureless vitrectomy for symptomatic vitreous floaters. Retina 34:1055–1061
Lin Z, Zhang R, Liang QH et al (2017) Surgical outcomes of 27-gauge pars plana vitrectomy for symptomatic vitreous floaters. J Ophthalmol 2017:5496298
Sommerville DN (2015) Vitrectomy for vitreous floaters: analysis of the benefits and risks. Curr Opin Ophthalmol 26:173–176
Appeltans A, Mura M, Bamonte G (2017) Macular hole development after vitrectomy for floaters: a case report. Ophthalmol Ther 6:385–389
Rubino SM, Parke DW 3rd, Lum F (2021) Return to the operating room after vitrectomy for vitreous opacities: intelligent research in sight registry analysis. Ophthalmol Retina 5:4–8
Serpetopoulos CN, Korakitis RA (1998) An optical explanation of the entoptic phenomenon of ‘clouds’ in posterior vitreous detachment. Ophthalmic Physiol Opt 18:446–451
Kalavar M, Hubschman S, Hudson J et al (2021) Evaluation of available online information regarding treatment for vitreous floaters. Semin Ophthalmol 36:58–63
Sebag J (2020) Vitreous and vision degrading myodesopsia. Prog Retin Eye Res 79:100847
Gishti O, van den Nieuwenhof R, Verhoekx J et al (2019) Symptoms related to posterior vitreous detachment and the risk of developing retinal tears: a systematic review. Acta Ophthalmol 97:347–352
van Overdam KA, Bettink-Remeijer MW, Mulder PG et al (2001) Symptoms predictive for the later development of retinal breaks. Arch Ophthalmol 119:1483–1486
Funding
This study was supported in part by the National Science Foundation of Liaoning Province, China (2020-MS-360), and Shenyang Young and Middle-aged Science and Technology Innovation Talent Support Program (RC210267). The funding organization had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Contributions
T. Z. L.: research design, interpretation of data, critical revision of the manuscript, and final approval of the version to be published. X. Y., C. S., Q. L.: data acquisition and analysis and drafting the manuscript. E. E. P.: critical revision of the manuscript and data analysis. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All research methods are in accordance with the tenets of the Declaration of Helsinki and approved by the ethics committee Board of the He Eye Specialist Hospital. Written informed consent was waived due to the retrospective design.
Consent for publication
All authors concur with the submission and agree for publication.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yang, X., Shi, C., Liu, Q. et al. Spontaneous remission of vision degrading myodesopsia of posterior vitreous detachment type. Graefes Arch Clin Exp Ophthalmol 261, 1571–1577 (2023). https://doi.org/10.1007/s00417-022-05948-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-022-05948-4