Abstract
Purpose
To determine the correlation of angiogenic growth factors and inflammatory cytokines with the clinical phenotype of ocular tuberculosis (OTB).
Methods
Vitreous fluid was analysed for cytokines in patients with OTB and non-OTB uveitis using multiplex fluorescent bead-based flow cytometric assay. The clinical phenotypes were recorded and correlated with vitreous biomarkers.
Results
Vitreous humour from OTB patients had elevated levels of interleukin-10 (IL-10), IL-17-A, interferon-gamma (IFN-γ), and tumour necrosis factor-alpha (TNF-α). Angiopoietin (Ang-2) levels were higher in the panuveitis phenotype. OTB posterior uveitis phenotype had relatively higher vascular endothelial growth factor (VEGF) levels and lower fibroblast growth factor (FGF) levels. Additionally, eyes with choroiditis and vasculitis had elevated levels of VEGF and Ang-2 with FGF downregulation. Both IFN-γ and IL-10 were upregulated in the choroiditis phenotype of OTB.
Conclusion
Angiogenic growth factors and inflammatory cytokines were altered in the vitreous humour of OTB patients. IFN-γ, VEGF, and IL-10 levels are increased in choroiditis and vasculitis phenotypes. Receiver operating characteristic (ROC) curve analysis further emphasized the importance of the IFN-γ assay in the diagnosis of OTB.
Similar content being viewed by others
Avoid common mistakes on your manuscript.

Introduction
Uveitis, an intraocular inflammation, is a leading cause of blindness worldwide [1]. Uveitis can be infectious, autoimmune, or idiopathic, depending on its aetiology. Ocular tuberculosis (OTB) is a chronic, granulomatous condition caused by Mycobacterium tuberculosis (MTB) that accounts for approximately 5–10% of uveitis cases [2, 3]. OTB-induced uveitis i.e. tubercular uveitis (TBU) is a painful devastating disease. Retinal and choroidal blood vessels are often involved, and vasculitis, serpiginous choroiditis, choroidal tubercles, or granuloma, and subretinal abscesses are the typical clinical presentation of the disease [4, 5]. Tubercular uveitis usually develops due to hypersensitivity reactions or hematogenous dissemination after a distant TB infection [6, 7]. Owing to a flared immune response, patients are often treated with corticosteroid therapy in addition to anti-TB treatment, indicating complex pathogenesis of OTB involving various chemokines and cytokines that mediate the inflammatory cascade [8, 9]. Pulmonary TB patients have been reported to have elevated serum angiogenic markers that increase with disease severity [10]. Angiogenesis signalling has been shown to play a critical role in TB granuloma formation as well as the dissemination of the MTB [11]. Infectious uveitis patients had elevated tumour necrosis factor-alpha (TNF-α), interferon-gamma (IFN-γ), interleukin-2 (IL-2), IL-4, IL-5, IL-18, and IL-10 cytokines in the aqueous humour compared to non-infectious uveitis [12]. Recently, Fukunaga et al. measured 33 inflammatory molecules from the vitreous fluid of uveitis patients with various aetiologies such as intraocular lymphoma, sarcoidosis, bacterial endophthalmitis, acute retinal necrosis, and found disease-specific patterns of biomolecules [13]. Several studies have reported cytokine changes in uveitis patients, and a few have further correlated with phenotypes of uveitis although there are still limited in OTB [14,15,16]. Ocular TB has protean manifestations that can vary from purely infective phenotypes, such as TB abscess or tuberculoma, to immune-mediated manifestations like serpiginous choroiditis or retinal vasculitis. Since retinal and choroidal blood vessels are often involved in TBU, understanding angiogenic biomarkers is key to pathophysiology. Furthermore, the uvea takes the brunt of inflammation due to extreme vascularity. We have previously reported the significance of vascular endothelial growth factor (VEGF) and fibroblast growth factor (FGF) as important mediators in MTB-infected retinal pigmented epithelial (RPE) cells and vitreous humour of patients with OTB [17]. In the present study, we measured the levels of key angiogenesis and inflammatory mediators in the vitreous humour samples of OTB and non-OTB uveitis patients and further correlated them with the clinical phenotype of OTB to assess their clinical implications.
Material and methods
This study was approved by the PGIMER Institute Ethics Committee and conducted in accordance with the tenets of the Declaration of Helsinki. After obtaining the informed consent, patients were enrolled at the uveitis clinic of Advanced Eye Centre, PGIMER, Chandigarh. The demographic details and clinical histories of all patients were recorded for analysis.
Subjects
The study included 48 patients with uveitis who underwent diagnostic pars plana vitrectomy (PPV) for different indications; 35 were subsequently diagnosed with OTB, and 13 were non-OTB uveitis controls. Patient vitreous humour samples were stored at − 80 °C as part of the ocular bio-repository bank maintained at our centre.
The patients were diagnosed and classified into confirmed and probable OTB according to the classification system of OTB by Gupta et al. 2015, which is based on clinical signs suggestive of OTB, ocular laboratory examinations including PCR for detection of MTB or MTB culture, immunological test (PPD and IGRA) along with radiologic features (CXR or CT) [4]. Confirmed OTB is the patients with clinical signs suggestive of OTB and confirmation of MTB from ocular fluids by PCR or microbiological culture. Probable OTB is patients with clinical signs suggestive of OTB and evidence of immunological test (PPD and IGRA) along with radiologic features ( chest CXR or CT) suggestive of TB. Patients with OTB showed no signs of extraocular TB or indications of TB in other body parts. The disease spectrum in the non-OTB uveitis group included idiopathic panuveitis (n = 1), pars planitis (idiopathic intermediate uveitis) (n = 2), retinal vasculitis (n = 4), vitreous haemorrhage (n = 2), choroiditis (n = 1), tractional retinal detachment (n = 1), acute retinal necrosis (n = 1), and toxocariasis (n = 1). No difference was observed in the age distribution among the groups, excluding age as a causative agent of immune responses. Furthermore, for cytokine profiling purposes, the patients were classified based on disease phenotype, i.e. the clinical presentation and anatomy of the disease, viz, anterior, posterior, and intermediate uveitis. The patients were followed up with an average duration of 11.4 months to establish the clinical significance of cytokine levels with OTB.
Angiogenic growth factors and inflammatory cytokines quantification
Angiogenesis growth factors: angiopoietin-2 (Ang-2), FGF, platelet-derived growth factors (PDGF-AA and PDGF-BB), VEGF, and granulocyte–macrophage colony-stimulating factor (GM-CSF) and inflammatory cytokines; IL-10, IFN-γ, TNF-α and IL-17A levels were quantified in the vitreous fluids using bead-based multiplex assay (LEGENDplex, BioLegend Inc, San Diego, CA, USA), quantified by flow cytometry (BD FACS LSR Fortessa). All kit reagents and standards ranging from 12.2 to 50,000 pg/ml were prepared according to the manufacturer’s instructions. Briefly, twenty-five microliters of each vitreous sample were used in the assay. The samples or standards were combined with conjugated fluorescent beads labelled with a particular analyte and detection antibody. The samples were incubated for 2 h in the dark at room temperature. Twenty-five microliters of streptavidin–phycoerythrin (SA-PE) reagent were added to the biotinylated detection antibodies, giving fluorescent signal intensities to the number of bound analytes. Beads were spun down and washed with wash buffer before being suspended into the final 200 µl of the buffer. All samples were analysed on BD FACS LSR Fortessa flow cytometer equipped with FACS DIVA 7.0 software (BD Biosciences, CA, USA). Unlabelled and PE beads were used as negative and positive controls, respectively. Setup beads were used to set the channel’s PMT voltages, and kit-provided standards were serially diluted to generate a standard curve for each analyte. FCS files were exported, and LEGENDplex™ data analysis software was used to analyse the data. The beads were segregated according to size and internal fluorescence intensity using a flow cytometer. Analyte-specific populations were separated and quantified using PE fluorescent signal. The exact concentration of analyte in the sample was calculated using a standard curve.
Statistical analysis
GraphPad Prism 8 was used for statistical analysis. Numerical data were represented as mean ± SEM in independent sample tests. The Kolmogorov–Smirnov test was used to check the normality of data. The Mann–Whitney was used to compare the groups, while a one-way ANOVA or Kruskal–Wallis test was performed to determine the significance level for more than two groups based on the normality distribution. A receiver operating characteristic (ROC) curve was generated to determine the optimal cut-off level, and the area under the curve (AUC) was assessed to check the diagnostic performance of the marker. p < 0.05 was recognized as statistically significant.
Results
The study included 48 patients with uveitis, of whom 35 were subsequently diagnosed with OTB, and 13 patients were non-OTB uveitis controls. The patients were further sub-classified into confirmed OTB (n = 15), probable OTB (n = 20), and non-OTB (n = 13) based on our previously published OTB classification system [4, 18]. There were 29 men and 19 women, with a male-to-female ratio of 1.5:1. The mean age of subjects with confirmed OTB was 37.92 ± 15.78 years, and probable OTB was 38.4 ± 15.7 years, and the non-OTB group was 44.9 ± 18.7 years. The disease spectrum in OTB included panuveitis (n = 16), intermediate uveitis (n = 3), choroidal granuloma (n = 1), retinal vasculitis (n = 7), and serpiginous choroiditis (n = 8). The detailed clinical parameters of all patients are provided in Table 1.
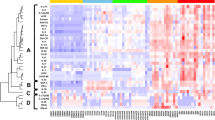
Overall, ten inflammatory and angiogenic growth factors in the vitreous fluid of patients with uveitis were analysed using flow cytometry. All the molecules viz Ang-2, FGF, PDGF-AA, PDGF-BB, VEGF, IL-10, IFN-γ, TNF-α, and IL-17A were detectable except, GM-CSF. Among angiogenic growth factors, levels of Ang-2 and VEGF were found to be elevated in the OTB group compared to the non-OTB group, but the data were not statistically significant; at the same time, inflammatory molecules IL-10, TNF-α, IFN-γ, and IL-17A were significantly augmented in OTB patients compared to non-OTB uveitis controls (Fig. 1). FGF levels were lower in patients with OTB than in the non-OTB uveitis controls. Furthermore, IL-10 and IFN-γ showed differential patterns among the confirmed OTB, probable OTB, and non-OTB uveitis control groups, with the highest levels in confirmed OTB, followed by probable OTB, and least in the non-TB uveitis control group, indicating their role in clinical stratification (Fig. 1).
Next, we analysed the relevance of molecules to the clinicopathological features of the disease, based on the anatomy of the disease, to establish their clinical importance. Ang-2 and FGF-2 levels were significantly higher in patients with panuveitis than those with intermediate or posterior uveitis. Surprisingly, FGF levels were reduced in posterior uveitis with a concomitant increase in VEGF compared to intermediate and pan-uveitis. No correlation was found between inflammatory mediators and disease anatomy (Fig. 2). We also examined the relationship between immune mediators with disease phenotypes to establish their prognostic significance. VEGF and Ang-2 were generally upregulated in serpiginous choroiditis and vasculitis disease phenotypes. However, FGF expression was found to be suppressed in these phenotypes. In addition, IL-10 and IFN-γ levels were elevated only in patients with serpiginous choroiditis (Fig. 3). Similarly, Ang-2 levels were higher in patients with longer disease duration (> 3 months) than in those with shorter disease duration; however, the difference was not statistically significant. Among the inflammatory molecules, IL-17A levels were significantly elevated with disease duration (Fig. 4). The mean values of all growth factors and inflammatory cytokines are listed in Table 2.
Angiogenesis growth factors and inflammatory cytokines in the vitreous samples of OTB patients based on anatomical locations of disease; intermediate, posterior, and pan-uveitis. One-way ANOVA or Kruskal–Wallis tests were used depending on the normality of the data. A p-value < 0.05 was considered significant
A ROC curve was plotted for each analyte to evaluate whether these molecules could serve as indicators for differentiating probable OTB, confirmed OTB, and non-OTB uveitis controls. All four inflammatory markers, IL-10 (p = 0.007), IL-17A (p = 0.018), IFN-γ (p = 0.011), and TNF-α (p = 0.022), had a good AUC with a significant p-value for differentiating the probable OTB group from the non-OTB group. Similarly, to distinguish confirmed OTB from the non-OTB uveitis control group, IL-10 and IFN-γ showed AUC of 0.783 and 0.828, respectively (p = 0.047, p = 0.022, respectively). At the cut-off value of 280.95 pg/ml, IFN-γ showed 73.3% sensitivity and 83.3% specificity in differentiating confirmed OTB from non-OTB. Similarly, IL-10 had a sensitivity of 53.3% and specificity of 83.3% at a cut-off value of 20.03 pg/ml for confirmed OTB from non-OTB uveitis control cases. For differentiation of probable OTB group from non-OTB uveitis controls, IFN-γ had a sensitivity of 85% and specificity of 66.7% at a cut-off value of 252.6 pg/ml, while for IL-10, sensitivity and specificity were 75% and 83.3%, respectively, at 19.94 pg/ml cut-off level (Fig. 5).
Discussion
OTB often involves inflammation of retinal and choroidal blood vessels. TBU diagnosis is challenging and usually requires 6–9 months of longer antitubercular therapy (ATT) and systemic corticosteroid treatment. The involvement of angiogenesis and inflammatory immune mediators in the pathophysiology of OTB and their association with OTB-induced uveitis phenotypes are poorly understood. In this study, the levels of inflammatory cytokines were higher in the OTB group than those in the non-OTB uveitis control group. Interestingly, IFN-γ levels were the highest in confirmed OTB patients, followed by probable OTB patients, and lowest in the non-OTB uveitis control group. These findings reemphasize the importance of IFN-γ in disease pathophysiology and the significance of the QuantiFERON-TB Gold test for the diagnosis of OTB. The IL-10 levels showed a differential pattern between OTB and non-OTB uveitis control groups. IL-10 is produced by macrophages, activated T cells, NK cells, dendritic cells, and B cells [19]. Animal studies have demonstrated that IL-10 is a protective cytokine in uveitis [20]. Many human studies have reported that elevated IL-10 levels in uveitis are mainly attributed to a feedback mechanism in tandem with inflammation [21]. Elevated IL-10 levels have also been linked to the ability of MTB to evade immune responses and chronic infections and mediate long-term infections [22]. IL-17A levels were also significantly higher in the OTB group than in the non-OTB uveitis control group and increased with disease duration. IL-17A, a member of the Th17 pathway, is a critical mediator of immunity, and protective and pathological roles have been shown for Th17 cells and IL-17A in mycobacterial infections [23]. MTB manipulates the Th17 pathway for survival, and dysregulated Th17 T-cell subsets have been reported in patients with pulmonary TB [24]. IL-17A is activated in the early stages of M. tuberculosis infection, and the IL-17R pathway is critical for immune surveillance, resulting in neutrophil recruitment [25, 26]. In an experimental autoimmune uveitis (EAU) model, Th17 cells were enough to induce uveitis which could be blocked with the treatment using an anti-IL17 antibody [27, 28]. In human subjects, increased levels of IL-17 have been found in autoimmune uveitis and are associated with active disease in patients with Bechet’s uveitis [29, 30]. A novel association has been reported between IL-17A locus polymorphisms and panuveitis, suggesting that IL-17A is a genetic risk factor for panuveitis [31]. IFN-γ has been well established and is central to MTB pathogenesis, increased concentrations of IFN-γ are a hallmark of TB infection. IFN-γ levels were higher in aqueous and serum samples of uveitis patients [32]. In OTB, IFN-γ levels were elevated in aqueous humour and positively correlated with disease activity [33]. The ROC curves in the present support the role of IL-10 and IFN-γ as promising diagnostic markers for OTB. Recently, Fukunaga et al. showed the value of inflammatory cytokines as diagnostic markers for different types of uveitis [13]. This differential pattern of IFN-γ and IL-10 could be of clinical interest as the diagnosis and management of OTB are challenging task.
Similar to our previous report, an elevated VEGF level trend was observed in the OTB group compared to that in the non-OTB uveitis controls. Interestingly, in this study, FGF was also reduced in the OTB group, consistent with our previous study, where we showed that MTB modulated VEGF and FGF for the growth and evasion of host defence mechanisms [17]. Furthermore, Ang-2 showed a differential pattern, depending on the anatomical location of the disease. FGF was reduced in posterior uveitis compared to that in intermediate and pan-uveitis.
VEGF and Ang-2 levels were also elevated, and FGF was downregulated in choroiditis and vasculitis presentation of tubercular uveitis. Since choroiditis and vasculitis phenotypes are vascular pathology-specific phenotypes of OTB, VEGF and Ang-2 angiogenic growth factors are augmented in these types. There have been multiple reports of patients with tubercular granulomas treated with anti-VEGF agents who showed clinical regression of the granuloma [34, 35]. A case of multiple bilateral tubercular granulomas with an exudative retinal detachment was reported with elevated levels of VEGF in the aqueous humour, treatment with weekly intravitreal anti-VEGF bevacizumab reduced VEGF levels and granuloma regression [36].
Among the inflammatory mediators, IL-10 and IFN-γ levels showed a sudden spike only in choroiditis. Furthermore, the ROC curve showed that IL-10 and IFN-γ cytokines can be used to differentiate OTB phenotypes with high sensitivity and specificity. This study further emphasizes the importance of the QuantiFERON assay for the diagnosis of OTB. Additionally, IL-10 and IFN-γ cytokine levels could be clinically helpful in differentiating OTB phenotypes from non-OTB patients, with good sensitivity and specificity.
In conclusion, the vitreous local environment of patients with OTB reveals the significance of several cytokines in OTB pathogenesis and clinical presentation of the disease. IL-10 and IFN-γ levels could be used as adjuvants to differentiate probable or confirmed OTB uveitis from non-OTB uveitis. Ang-2 might be useful for the prognosis of severe presentations of the disease such as choroiditis and vasculitis; however, further studies are required for validation.
References
Guo X, Chen Z, Xing Y (2021) Immune-mediated uveitis and lifestyle factors: a review. Ophthalmic Res 64:687–695. https://doi.org/10.1159/000518496
Gupta V, Gupta A, Rao NA (2007) Intraocular tuberculosis–an update. Surv Ophthalmol 52:561–587. https://doi.org/10.1016/j.survophthal.2007.08.015
Singh R, Gupta V, Gupta A (2004) Pattern of uveitis in a referral eye clinic in north India. Indian J Ophthalmol 52:121–125
Gupta A, Sharma A, Bansal R, Sharma K (2015) Classification of intraocular tuberculosis. Ocul Immunol Inflamm 23:7–13. https://doi.org/10.3109/09273948.2014.967358
Agarwal A, Aggarwal K, Gupta V (2019) Infectious uveitis: an Asian perspective Eye (Lond) 33:50–65. https://doi.org/10.1038/s41433-018-0224-y
Buckner CB, Leithiser RE, Walker CW, Allison JW (1991) The changing epidemiology of tuberculosis and other mycobacterial infections in the United States: implications for the radiologist. AJR Am J Roentgenol 156:255–264. https://doi.org/10.2214/ajr.156.2.1898796
Hernandez C, Cetner AS, Jordan JE, Puangsuvan SN, Robinson JK (2008) Tuberculosis in the age of biologic therapy. J Am Acad Dermatol 59:363–380. https://doi.org/10.1016/j.jaad.2008.05.033
Gupta V, Shoughy SS, Mahajan S, Khairallah M, Rosenbaum JT, Curi A, Tabbara KF (2015) Clinics of ocular tuberculosis. Ocul Immunol Inflamm 23:14–24. https://doi.org/10.3109/09273948.2014.986582
Kee AR, Gonzalez-Lopez JJ, Al-Hity A, Gupta B, Lee CS, Gunasekeran DV, Jayabalan N, Grant R, Kon OM, Gupta V, Westcott M, Pavesio C, Agrawal R (2016) Anti-tubercular therapy for intraocular tuberculosis: a systematic review and meta-analysis. Surv Ophthalmol 61:628–653. https://doi.org/10.1016/j.survophthal.2016.03.001
Kumar NP, Banurekha VV, Nair D, Babu S (2016) Circulating angiogenic factors as biomarkers of disease severity and bacterial burden in pulmonary tuberculosis. PLoS ONE 11:e0146318. https://doi.org/10.1371/journal.pone.0146318
Oehlers SH, Cronan MR, Scott NR, Thomas MI, Okuda KS, Walton EM, Beerman RW, Crosier PS, Tobin DM (2015) Interception of host angiogenic signalling limits mycobacterial growth. Nature 517:612–615. https://doi.org/10.1038/nature13967
Takase H, Futagami Y, Yoshida T, Kamoi K, Sugita S, Imai Y, Mochizuki M (2006) Cytokine profile in aqueous humor and sera of patients with infectious or noninfectious uveitis. Invest Ophthalmol Vis Sci 47:1557–1561. https://doi.org/10.1167/iovs.05-0836
Fukunaga H, Kaburaki T, Shirahama S, Tanaka R, Murata H, Sato T, Takeuchi M, Tozawa H, Urade Y, Katsura M, Kobayashi M, Wada Y, Soga H, Kawashima H, Kohro T, Aihara M (2020) Analysis of inflammatory mediators in the vitreous humor of eyes with pan-uveitis according to aetiological classification. Sci Rep 10:2783. https://doi.org/10.1038/s41598-020-59666-0
Curnow SJ, Murray PI (2006) Inflammatory mediators of uveitis: cytokines and chemokines. Curr Opin Ophthalmol 17:532–537. https://doi.org/10.1097/ICU.0b013e32801094b5
Sijssens KM, Rijkers GT, Rothova A, Stilma JS, Schellekens PA, de Boer JH (2007) Cytokines, chemokines and soluble adhesion molecules in aqueous humor of children with uveitis. Exp Eye Res 85:443–449. https://doi.org/10.1016/j.exer.2007.06.011
Ooi KG, Galatowicz G, Calder VL, Lightman SL (2006) Cytokines and chemokines in uveitis: is there a correlation with clinical phenotype? Clin Med Res 4:294–309. https://doi.org/10.3121/cmr.4.4.294
Singh N, Singh R, Sharma RK, Kumar A, Sharma SP, Agarwal A, Gupta V, Singh R, Katoch D (2020) Mycobacterium tuberculosis modulates fibroblast growth factor and vascular endothelial growth factor in ocular tuberculosis. Ocul Immunol Inflamm: 1–7 https://doi.org/10.1080/09273948.2020.1734212
Agrawal R, Agarwal A, Jabs DA, Kee A, Testi I, Mahajan S, McCluskey PJ, Gupta A, Palestine A, Denniston A, Banker A, Invernizzi A, Fonollosa A, Sharma A, Kumar A, Curi A, Okada A, Schlaen A, Heiligenhaus A, Kumar A, Gurbaxani A, Bodaghi B, Islam Shah B, Lowder C, Tappeiner C, Muccioli C, Vasconcelos-Santos DV, Goldstein D, Behra D, Das D, Makhoul D, Baglivo E, Denisova E, Miserocchi E, Carreno E, Asyari F, Pichi F, Sen HN, Uy H, Nascimento H, Tugal-Tutkun I, Arevalo JF, Davis J, Thorne J, Hisae Yamamoto J, Smith J, Garweg JG, Biswas J, Babu K, Aggarwal K, Cimino L, Kuffova L, Agarwal M, Zierhut M, Agarwal M, De Smet M, Tognon MS, Errera MH, Munk M, Westcott M, Soheilian M, Accorinti M, Khairallah M, Nguyen M, Kon OM, Mahendradas P, Yang P, Neri P, Ozdal P, Amer R, Lee R, Distia Nora R, Chhabra R, Belfort R, Mehta S, Shoughy S, Luthra S, Mohamed SO, Chee SP, Basu S, Teoh S, Ganesh S, Barisani-Asenbauer T, Guex-Crosier Y, Ozyazgan Y, Akova Y, Habot-Wilner Z, Kempen J, Nguyen QD, Pavesio C, Gupta V, Collaborative Ocular Tuberculosis Study G (2019) Standardization of nomenclature for ocular tuberculosis - results of collaborative ocular tuberculosis study (COTS) workshop. Ocul Immunol Inflamm: 1–11. https://doi.org/10.1080/09273948.2019.1653933
Verma R, Balakrishnan L, Sharma K, Khan AA, Advani J, Gowda H, Tripathy SP, Suar M, Pandey A, Gandotra S, Prasad TS, Shankar S (2016) A network map of Interleukin-10 signaling pathway. J Cell Commun Signal 10:61–67. https://doi.org/10.1007/s12079-015-0302-x
Broderick CA, Smith AJ, Balaggan KS, Georgiadis A, Buch PK, Trittibach PC, Barker SE, Sarra GM, Thrasher AJ, Dick AD, Ali RR (2005) Local administration of an adeno-associated viral vector expressing IL-10 reduces monocyte infiltration and subsequent photoreceptor damage during experimental autoimmune uveitis. Mol Ther 12:369–373. https://doi.org/10.1016/j.ymthe.2005.03.018
Sauer A, Villard O, Creuzot-Garcher C, Chiquet C, Berrod JP, Speeg-Schatz C, Bourcier T, Candolfi E (2015) Intraocular levels of interleukin 17A (IL-17A) and IL-10 as respective determinant markers of toxoplasmosis and viral uveitis. Clin Vaccine Immunol 22:72–78. https://doi.org/10.1128/CVI.00423-14
Redford PS, Murray PJ, O’Garra A (2011) The role of IL-10 in immune regulation during M. tuberculosis infection. Mucosal Immunol 4:261–270. https://doi.org/10.1038/mi.2011.7
Torrado E, Cooper AM (2010) IL-17 and Th17 cells in tuberculosis. Cytokine Growth Factor Rev 21:455–462. https://doi.org/10.1016/j.cytogfr.2010.10.004
Shen H, Chen ZW (2018) The crucial roles of Th17-related cytokines/signal pathways in M. tuberculosis infection. Cell Mol Immunol 15:216–225. https://doi.org/10.1038/cmi.2017.128
van de Veerdonk FL, Teirlinck AC, Kleinnijenhuis J, Kullberg BJ, van Crevel R, van der Meer JW, Joosten LA, Netea MG (2010) Mycobacterium tuberculosis induces IL-17A responses through TLR4 and dectin-1 and is critically dependent on endogenous IL-1. J Leukoc Biol 88:227–232. https://doi.org/10.1189/jlb.0809550
Lombard R, Doz E, Carreras F, Epardaud M, Le Vern Y, Buzoni-Gatel D, Winter N (2016) IL-17RA in non-hematopoietic cells controls CXCL-1 and 5 critical to recruit neutrophils to the lung of mycobacteria-infected mice during the adaptive immune response. PLoS ONE 11:e0149455. https://doi.org/10.1371/journal.pone.0149455
Peng Y, Han G, Shao H, Wang Y, Kaplan HJ, Sun D (2007) Characterization of IL-17+ interphotoreceptor retinoid-binding protein-specific T cells in experimental autoimmune uveitis. Invest Ophthalmol Vis Sci 48:4153–4161. https://doi.org/10.1167/iovs.07-0251
Zhang R, Qian J, Guo J, Yuan YF, Xue K (2009) Suppression of experimental autoimmune uveoretinitis by anti-IL-17 antibody. Curr Eye Res 34:297–303. https://doi.org/10.1080/02713680902741696
Jawad S, Liu B, Agron E, Nussenblatt RB, Sen HN (2013) Elevated serum levels of interleukin-17A in uveitis patients. Ocul Immunol Inflamm 21:434–439. https://doi.org/10.3109/09273948.2013.815786
Na SY, Park MJ, Park S, Lee ES (2013) Up-regulation of Th17 and related cytokines in Behcet’s disease corresponding to disease activity. Clin Exp Rheumatol 31:32–40
Mucientes A, Marquez A, Cordero-Coma M, Martin-Villa JM, Gorrono-Echebarria MB, Blanco R, Diaz Valle D, Benitez-del-Castillo JM, del Rio MJ, Blanco A, Olea JL, Cordero Y, Capella MJ, Gonzalez J, Diaz-Llopis M, Ortego-Centeno N, Adan A, Ruiz-Arruza I, Llorenc V, Fonollosa A, Martin J (2015) Specific association of IL17A genetic variants with panuveitis. Br J Ophthalmol 99:566–570. https://doi.org/10.1136/bjophthalmol-2014-306106
Lacomba MS, Martin CM, Chamond RR, Galera JM, Omar M, Estevez EC (2000) Aqueous and serum interferon gamma, interleukin (IL) 2, IL-4, and IL-10 in patients with uveitis. Arch Ophthalmol 118:768–772. https://doi.org/10.1001/archopht.118.6.768
Abu El-Asrar AM, Struyf S, Kangave D, Al-Obeidan SA, Opdenakker G, Geboes K, Van Damme J (2012) Cytokine and CXC chemokine expression patterns in aqueous humor of patients with presumed tuberculous uveitis. Cytokine 59:377–381. https://doi.org/10.1016/j.cyto.2012.04.030
Invernizzi A, Franzetti F, Viola F, Meroni L, Staurenghi G (2015) Optic nerve head tubercular granuloma successfully treated with anti-VEGF intravitreal injections in addition to systemic therapy. Eur J Ophthalmol 25:270–272. https://doi.org/10.5301/ejo.5000528
Matsou A, Dermenoudi M, Tzetzi D, Rotsos T, Makri O, Anastasopoulos E, Symeonidis C (2021) Peripapillary choroidal neovascular membrane secondary to sarcoidosis-related panuveitis: treatment with aflibercept and ranibizumab with a 50-month follow-up. Case Rep Ophthalmol 12:186–192. https://doi.org/10.1159/000512579
Agarwal M, Gupta C, Mohan KV, Upadhyay PK, Jha V (2020) Correlation of vascular endothelial growth factor with the clinical regression of tubercular granuloma. Indian J Ophthalmol 68:2037–2040. https://doi.org/10.4103/ijo.IJO_1261_20
Funding
This work was partially supported by the Department of Biotechnology Grant BT/PR13453/MED/30/1524/2015 and the Indian Council of Medical Research, grant 2015–1323 NCD II.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Research involving human participants
The study was approved by the PGIMER Institute Ethics Committee in accordance with the tenets of the Declaration of Helsinki.
Consent to participate
Written informed consent was obtained from each participant before enrolment in the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kumar, A., Singh, R., Sharma, R.K. et al. Correlation of angiogenic growth factors and inflammatory cytokines with the clinical phenotype of ocular tuberculosis. Graefes Arch Clin Exp Ophthalmol 261, 1369–1380 (2023). https://doi.org/10.1007/s00417-022-05943-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-022-05943-9