Abstract
Purpose
To provide a review of the salient histological and imaging features in neovascular age-related macular degeneration (AMD) that will be integrated in order to have a better comprehension of the pathogenesis and clinical aspects of this disease.
Methods
A literature review of histology and imaging features in neovascular AMD was conducted.
Results
Histology has granted a detailed characterization of neovascular AMD ex vivo. In details, histological features in these eyes have offered important insights into the pathogenesis of neovascular AMD. In addition, histology donated a detailed characterization of the different types of macular neovascularization (MNV) that may complicate AMD. The introduction of optical coherence tomography angiography (OCTA) has enormously amplified our knowledge of neovascular AMD through in vivo assessment of the anatomical and pathological characteristics of this disease. New insights elucidating the morphological features of the choriocapillaris confirmed that this vascular structure plays a crucial role in the pathogenesis of neovascular AMD. OCTA also offered a detailed visualization of MNV complicating neovascular AMD.
Conclusions
New imaging technologies offer a remarkable chance to build a bridge between histology and clinical findings in neovascular AMD.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.

Introduction
Age-related macular degeneration (AMD) represents a predominant cause of reduced visual acuity among older subjects in developed countries [1]. A severe vision loss may be the result of exudation of macular neovascularization (MNV) in most of the AMD cases (85%). However, the development of geographic atrophy (GA) is also a recognized causal factor (15% of cases). The late form of AMD is characterized by the development of one of these complications [1].
AMD may be complicated by the development of a type 1, type 2, or type 3 MNV. Fluorescein angiography (FA) has been historically considered a fundamental imaging modality in the identification and follow-up of patients with neovascular AMD, showing leakage of the dye on late phases of the angiographic sequence. Type 1 MNV may be difficult to delineate on FA, associated with some hyperfluorescent pinpoints; therefore, the term “occult” was applied. In details, FA may display a poorly delineated area of stippled hyperfluorescence in presence of type 1 MNV. Conversely, type 2 MNV typically exhibits a well-defined or “classic” pattern with FA. On FA images, type 2 MNV appears as a well-demarcated area of hyperfluorescence with leakage in the mid- and late-phase frames. In presence of type 3 MNV, FA shows a focal hyperfluorescent area in front of the RPE with occult leakage, similarly to type 1 MNV.
The detection of type 1 MNV had been significantly improved with indocyanine green angiography (ICGA). In contrast to FA, ICGA uses an alternative dye that is significantly (99%) bound to plasma lipoproteins and employs a longer excitation wavelength. As a consequence, this imaging modality grants a better visualization of the choroidal vessels and neovascularizations below the RPE. Using ICGA, type 1 MNV may be visualized as well-demarcated areas of fluorescence, presenting as a hyperfluorescent plaque that emerges relatively late in the angiogram. In type 3 MNV, ICGA may reveal a hot spot with staining and leakage.
Structural optical coherence tomography (OCT) and OCT angiography have significantly improved our capability to characterize neovascular AMD [2,3,4]. Since these imaging techniques have overcome significant limitations of previous dye-based techniques for the assessment of the retina and choroid, structural OCT and OCTA have assumed the role of key technological tools for the evaluation of patients with neovascular AMD. In particular, OCTA has granted a detailed visualization of different types of MNV and new insights into the pathogenesis of neovascular AMD, as this imaging modality offers a unique visualization of the choriocapillaris (CC), which represents the innermost portion of the choroid. The OCTA technology and analysis of CC images is not discussed in detail, since there are recent reviews discussing these aspects in-depth [3, 5]. Of note, there is a debate on the best strategy that should be employed to analyze CC images (e.g., image averaging and/or compensation, threshold to binarized images). Therefore, a correct interpretation of OCTA images in neovascular AMD eyes should be also weighed with the image analysis employed to elaborate images. In this review, we will integrate findings of OCTA studies with histologic features previously described in neovascular AMD.
Pathologic mechanisms leading to macular neovascularization
AMD is a complex disorder with a multifactorial etiology. Although its pathogenesis involves many elements, different approaches proved that AMD is ultimately featured by a damage of the unit comprised by the photoreceptors, RPE, Bruch’s membrane, and CC. Dysfunction of this unit may lead to the development of drusen with progressive photoreceptor, RPE, and CC damage.
Histopathological studies displayed that the number of CC non-functional capillary vessels (i.e., empty vessels without blood flowing inside—also known as ghost vessels) is greater in eyes with drusen [6]. Moreover, the CC dropout was demonstrated to be dependent on the AMD stage, with the late stage featured by the greatest amount of non-functional capillary vessels [6].
The causative relationship between the CC and RPE impairments has been evaluated in a histopathological study [7]. In this study, the authors analyzed postmortem eyes from 11 subjects, including 5 and 3 patients with GA and neovascular AMD, respectively, and 3 age-matched controls without ocular disorders. This analysis showed that RPE is primarily affected in GA (i.e., there are no regions with CC loss and overlying healthy RPE), while a CC impairment may occur in regions with viable RPE in the eyes with neovascular AMD. In these regions with vascular dropout, the RPE may be relatively hypoxic, causing an increase in VEGF secretion by the RPE and resulting stimulation of MNV growth. Finally, fractures in Bruch’s membrane allow the transit of neovessels from the CC into the sub-RPE or subretinal space.
The damage of the unit comprised by the photoreceptors, RPE, Bruch’s membrane, and CC as the key factor of AMD pathogenesis and MNV development has been recently supported by imaging studies. Previous important studies employing structural OCT and OCTA demonstrated that eyes with early/intermediate AMD are characterized by significant impairment of the photoreceptors [8] and CC [9,10,11]. Notably, dysfunction of these two units seems to be strictly correlated.[12].
Significant changes in the CC were displayed in eyes with exudative neovascular AMD. Using OCTA, the CC was studied in eyes with type 1 MNV [13, 14]. These studies displayed that many cases were characterized by the presence of a ring-shaped hypoperfused CC area surrounding the MNV (“dark halo”). The latter OCTA feature has been suggested to be dependent on a mechanical compression of the CC or may be secondary to a “steal” phenomenon [13].
OCTA was also employed to investigate the CC in eyes with type 3 MNV [15, 16], as several pieces of evidence suggested that outer retinal ischemia may be extremely relevant in driving the occurrence of this form of MNV [17]. Using OCTA analysis, the CC was compared between eyes affected by type 3 MNV and fellow eyes without MNV [15]. Furthermore, the latter fellow eyes were compared with the fellow eyes of AMD patients with unilateral type 1 or 2 MNV. The latter study demonstrated that eyes with type 3 MNV had an overall reduction in CC perfusion. Of note, also the fellow non-neovascular eyes (with type 3 MNV in the other eye) had a greater CC impairment than non-neovascular AMD fellow eyes from patients with unilateral type 1 or type 2 MNV. These OCTA findings corroborate the hypothesis that choroidal ischemia may have a fundamental role in the occurrence of type 3 MNV. Twenty-six type 3 MNV eyes were compared with 26 eyes with intermediate AMD [16]. The latter OCTA study demonstrated that eyes with type 3 MNV are characterized by a significant greater hypoperfusion of the CC.
Non-exudative neovascular AMD
The presence of an exudative neovascular lesion defines the exudative (or wet) neovascular form of AMD. Nonetheless, it should be noted that MNV may exist without characteristics of exudation, an entity referred to as “non-exudative neovascular AMD” [18, 19].
Non-exudative (or quiescent) MNV is defined as a treatment-naïve type 1 MNV imaged with dye-based angiography or OCTA and without evidence of exudation. Querques and Souied [18] first described this entity as a late-speckled hyperfluorescent lesion on fluorescein angiography (FA) or hyperfluorescent area seen on late-phase ICGA and associated with the absence of fluid on structural OCT.
Although dye-based angiographies may detect non-exudative MNV, OCTA represents a fast and non-invasive imaging modality with a high sensitivity in identifying non-exudative MNV lesions [19]. Using OCTA, non-exudative MNV may be detected in up to 30% of all subjects with intermediate AMD. This result agrees with previous results employing ICGA that demonstrated the presence of asymptomatic MNV in approximately 25% of eyes with drusen [20].
Using structural OCT and OCTA, eyes with non-exudative MNV were followed for 1 year after enrollment [21]. This study proved that the 1-year incidence of exudation was 21.1% and 3.6%, in eyes with and without non-exudative MNV, respectively. A subsequent study demonstrated the 2-year risk of exudation in eyes with non-exudative neovascular AMD was 13.6 times greater in comparison with eyes without non-exudative neovessels [22]. These studies demonstrated that the progression to frank exudation is significantly increased for eyes with documented non-exudative MNV [20]. Hence, OCTA may be considered a useful imaging tool to monitor intermediate AMD eyes and to define appropriate follow-up intervals.
OCTA analysis may also provide imaging biomarkers associated with an increased risk of exudation [23]. Specifically, non-exudative MNVs with a lower vascular density at baseline and slower growth over time were less inclined to exudation during follow-up.
Although non-exudative MNV may cause retinal damage through exudation, an increasing evidence seems to suggest that choroidal neovessels may compensatorily nourish hypoxic and micronutrient-insufficient outer retinal cells. In 2004, the first histological clues by Grossniklaus and Green [24] suggested that type 1 MNV may be favorable for the health of the outer retina and RPE. Specifically, they suggested that type 1 MNV supports overlying RPE and outer retina by recapitulating the morphology of native CC. Successively, a direct clinicopathological correlation (histology of eyes imaged during life) corroborated this theory [25]. In details, a white woman with treatment-naïve non-exudative neovascular AMD in one eye and exudative neovascular AMD in the fellow eye was examined postmortem after 9 years of follow-up visits with multimodal imaging. Multimodal imaging displayed that non-exudative MNV remained stable within a shallow irregular RPE detachment. Histologically, MNV invaded half of the macular region and vessels were demonstrated to cross twenty-two Bruch’s membrane’s fractures. Noteworthy, small non-exudative neovessels were morphologically equivalent to native CC. Furthermore, these neovessels had fenestrations, presumably secondary to VEGF, secreted by hypoxic RPE. Importantly, outer retinal cells were conserved over the non-exudative MNV.
Exudative neovascular AMD
Exudative neovascular AMD may be characterized by the pathological proliferation and exudation of type 1, type 2, or type 3 MNV.
Type 1 and type 2 MNV
Type 1 MNV is characterized by pathologic angiogenesis located between the RPE and Bruch’s membrane. This type of MNV represents the most common subtype of neovascular AMD. Conversely, type 2 MNV depicts the least common phenotype of exudative neovascular AMD, accounting for 9–17% of all newly diagnosed cases. Type 2 MNV is featured by the growth of pathologic choroidal vessels in the subretinal space (Figs. 1 and 2).
Multimodal imaging of an immature type 1 macular neovascularization associated with age-related macular degeneration. A Multicolor image shows areas of RPE alteration and mottling in the macula associated with a hemorrhage. B Blue fundus autofluorescence shows areas of reduced autofluorescence secondary to RPE atrophy. C The structural optical coherence tomography B-scan demonstrates the presence of a fibrovascular pigment epithelial detachment associated with intraretinal and subretinal fluid, and subretinal hyperreflective material. D Flow within a neovascular lesion (red arrowheads) is seen on the en face OCTA image segmented at the RPE-RPE fit level, as visualized on the corresponding E OCTA B-scan. F, G The OCTA image segmented at the level of the choriocapillaris demonstrates a region of hypoperfusion surrounding the MNV (highlighted with green arrowheads)
Multimodal imaging of type 3 macular neovascularization associated with age-related macular degeneration. A Multicolor image shows areas of RPE alteration and mottling in the macula. B The structural optical coherence tomography B-scan demonstrates the presence of a hyperreflective intraretinal lesion connected with the RPE/sub-RPE space in a region with RPE detachment (red arrowhead). C Flow within hyperreflective intraretinal material (green arrowheads) is seen on the corresponding OCTA B-scan image
Histopathological studies have provided a detailed characterization of neovascularizations in AMD. In details, type 1 and type 2 MNVs may appear as a neovascular sprout originating from the choroid and located in the sub-RPE or subretinal space through breaks in Bruch’s membrane. As these neovessels mature, they may progress in a more arranged vascular system stemming from a choroidal feeder vessel [26]. Noteworthy, the endothelial cells in the arborizing neovessels lack the barrier function of more mature endothelial cells. As a consequence, these neovessels may leak fluid into the sub-RPE, subretinal, and intraretinal locations. Histopathological data also reported that neovessels occurring in AMD are associated with the presence of other components that include fibroblasts, myofibroblasts, lymphocytes, and macrophages [27]. Furthermore, proteins and lipids may leak with fluid from neovessels and precipitate within the retina [26]. In some eyes, progression of the fibrous component may result in the maturation of a macular scar, which occurs with regression and/or condensation of the vascular component [28].
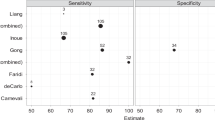
Thirty-three eyes with type 1 MNV were evaluated using OCTA [29]. This study demonstrated that 75% of eyes had a highly organized vascular complex on OCTA images. Furthermore, a large main feeder vessel was recognized in 72% of these cases. In the end, the authors identified two defined patterns: (i) the “medusa” pattern with neovessels branching outward from the core of the lesion, and (ii) the “sea fan” pattern featured by vessels branching from one side of the MNV. OCTA is characterized by high sensitivity in the detection of type 1 MNV when structural OCT and OCTA data are combined [13].
Using OCTA, type 2 MNV is visualized below the neuroretina and above the RPE and may be displayed either as a glomerulus- or medusa-shaped complex [30]. OCTA longitudinal analysis of type 2 MNV undergoing anti-VEGF therapy demonstrated a significant reduction in lesion’s vessel density and size after treatment [31]. In addition, given that subretinal hyperreflective material or SHRM seen on structural OCT may be the expression of various tissue forms, including type 2 MNV, OCTA may be helpful to clarify the composition of SHRM [32].
Follow-up of neovascularization with OCTA
Since OCTA may provide quantitative and qualitative metrics to describe MNV lesions, previous important studies have investigated modifications in MNV during anti-VEGF treatment [29, 33]. These studies demonstrated that anti-VEGF therapy decreases the quantity and perfusion of the smaller neovessels, with an overall sparing of the larger vessels, hence generating a non-significant shrinking of the MNV size. The larger vessels may be resistant to the anti-VEGF therapy owing to the presence of pericytes protecting endothelial cells. As a consequence, anti-VEGF drugs may shift the balance between angiogenesis and arteriogenesis, with consequent “abnormalization” of the MNV [4].
OCTA was also employed to assess MNVs with a predominant fibrous component (i.e., “fibrocellular pattern”) [28]. In details, this study analyzed eyes with previously treated neovascular AMD in remission (no subretinal hemorrhage, no sign of fluid in or under the retina, and no treatment for at least 6 months). This study cohort was divided according to the presence of fibrosis on multicolor (MC) images, yielding two distinct phenotypic subgroups: (1) fibrocellular group and (2) fibrovascular group. In the latter group, OCTA images revealed a higher percentage of vessels within the neovascularization. Therefore, this study suggested that a fibrocellular scar is characterized by RPE atrophy and reduced perfusion. Finally, the latter results confirmed previous histological findings, as fibrotic MNV was demonstrated to have a reduced vascular component, although neovessels were still present within its volume.
OCTA studies also supported the hypothesis that type 1 neovessels may protect from macular atrophy, as it was proved that atrophy tends to develop eccentrically to the neovascular lesion. Dansingani and colleagues [34] analyzed 9 eyes from 8 patients who had received more than 50 anti-VEGF injections during a period of at least 4 years. OCTA analysis revealed that the presence of mature, tangled neovessels below the RPE seems to be associated with a decreased likelihood of developing macular atrophy despite the presence of choriocapillaris loss.
Type 3 MNV
Much of our understanding of type 3 lesions has arisen from histopathological studies [35, 36]. Histologically, these lesions appear as vascular complexes in the outer neurosensory retina, eventually abutting the inner aspect of Bruch’s membrane [35, 36]. These neovessels were delimited by the presence of an abundant eosinophilic extracellular matrix. More importantly, type 3 MNV is composed of different branches within the retina, this reflecting a complex organization of these vascular abnormalities [35]. Furthermore, the presence of intraretinal vessels co-localizes with loss of outer retina and RPE [36]. Finally, there was no evidence of a connection between the sub-RPE space and the CC [36].
Over the last years, various authors have further sought to investigate characteristics of type 3 MNV with imaging studies. Using structural OCT and OCTA, previous studies showed that type 3 MNV originates from the retinal deep vascular complex (DVC) and descends toward the RPE which is usually detached (because of the presence of an associated fibrovascular, drusenoid, or serous PED) leading to exudation [37]. OCTA was also employed to assess the microvascular morphology of type 3 MNV [38]. OCTA showed intraretinal vascular lesions characterized by a tuft-like capillary network. Notably, OCTA imaging also proved to be relevant for the identification of precursor lesions (nascent type 3 lesions) as intraretinal hyperreflective foci with flow. These lesions may predict the development of mature type 3 neovessels associated with significant exudation [39]. Importantly, exudation seemed to be associated with these lesions reaching the RPE or the sub-RPE space [39].
Type 3 MNVs were also investigated using a volume-rendered three-dimensional (3D) visualization of OCTA [40,41,42]. In details, Borrelli et al. [41] retrospectively enrolled 13 patients (15 eyes) with AMD and type 3 MNV. OCTA volume data were first processed with a volume projection removal algorithm, and subsequently, a 3D visualization of the analyzed type 3 MNVs was obtained. The latter analysis provided a volume rendering representation of type 3 MNV that was confirmed to correspond to retinal-retinal anastomosis originating from the DVC and connecting with the RPE/sub-RPE space [41]. Furthermore, 3D visualization was shown to facilitate recognition of a higher number of retinal-retinal anastomoses within each type 3 MNV, as more vessels emerging from the DVC could be distinguished with 3D visualization as compared with a 2D assessment (Fig. 3). This is perhaps not surprising as one might expect that a 3D analysis will not be as limited by overlapping anatomy and vessel foreshortening. Subsequently, Breazzano and colleagues [42] reported a single case of a patient with type 3 MNV and also demonstrated 3D OCTA visualization with a different analysis algorithm which also yielded a volumetric description of the type 3 lesion. The distinct vascular branches within type 3 MNV is in agreement with histopathological studies [35, 36] that provided the basis for the term “type 3 complex” to better describe these branching neovascular lesions within the retina.
Volume-rendered three-dimensional (3D) visualization of OCTA data of a type 3 MNV. The 3D volume rendering visualization of flow within the region with the type 3 MNV complex demonstrates the presence of several branches (highlighted with white asterisks) originating from the deep vascular complex and moving downward obliquely. These neighboring branches seem to converge into a glomerular-like lesion (white arrow). The 3D volume rendering visualization also shows the choroidal flow (white arrowhead)
Conclusion
This review highlights the new insights regarding neovascular AMD as revealed by OCTA imaging. Imaging findings seem to support previous histological data that a dysfunction of the unit comprised of photoreceptors, RPE, and CC is relevant in the pathogenesis of neovascular AMD. More importantly, OCTA represents a potential novel and powerful tool to evaluate and characterize MNV in vivo, with characteristics resembling those described ex vivo by histology.
In summary, new imaging technologies offer a remarkable chance to build a bridge between histology and clinical findings in neovascular AMD.
References
Spaide RF, Jaffe GJ, Sarraf D, et al (2019) Consensus nomenclature for reporting neovascular age-related macular degeneration data: consensus on neovascular age-related macular degeneration nomenclature study group. Ophthalmology. https://doi.org/10.1016/j.ophtha.2019.11.004
Borrelli E, Sadda SR, Uji A, Querques G (2019) Pearls and pitfalls of optical coherence tomography angiography imaging: a review. Ophthalmol Ther. https://doi.org/10.1007/s40123-019-0178-6
Borrelli E, Sarraf D, Freund KB, Sadda SR (2018) OCT angiography and evaluation of the choroid and choroidal vascular disorders. Prog Retin Eye Res. https://doi.org/10.1016/j.preteyeres.2018.07.002
Spaide RRF, Fujimoto JG, Waheed NK et al (2017) Optical coherence tomography angiography. Prog Retin Eye Res 64:1–55. https://doi.org/10.1016/j.preteyeres.2017.11.003
Borrelli E, Parravano M, Sacconi R et al (2020) Guidelines on optical coherence tomography angiography imaging: 2020 focused update. Ophthalmol Ther 9(4), 697–707
Seddon JM, McLeod DS, Bhutto IA, et al (2016) Histopathological insights into choroidal vascular loss in clinically documented cases of age-related macular degeneration. JAMA Ophthalmol. https://doi.org/10.1001/jamaophthalmol.2016.3519
McLeod DS, Grebe R, Bhutto I et al (2009) Relationship between RPE and choriocapillaris in age-related macular degeneration. Invest Ophthalmol Vis Sci 50:4982–4991. https://doi.org/10.1167/iovs.09-3639
Borrelli E, Abdelfattah N, Uji A et al (2017) Postreceptor neuronal loss in intermediate age-related macular degeneration. Am J Ophthalmol 181:1–11. https://doi.org/10.1016/j.ajo.2017.06.005
Borrelli E, Uji A, Sarraf D, Sadda SR (2017) Alterations in the choriocapillaris in intermediate age-related macular degeneration. Investig Opthalmology Vis Sci [in press]:4792–4798. https://doi.org/10.1167/iovs.17-22360
Borrelli E, Mastropasqua R, Senatore A, et al (2018) Impact of choriocapillaris flow on multifocal electroretinography in intermediate age-related macular degeneration eyes. Investig Opthalmology Vis Sci 59:AMD25. https://doi.org/10.1167/iovs.18-23943
Borrelli E, Shi Y, Uji A et al (2018) Topographical analysis of the choriocapillaris in intermediate age-related macular degeneration. Am J Ophthalmol 196:34–43. https://doi.org/10.1016/j.ajo.2018.08.014
Borrelli E, Sacconi R, Zuccaro B, et al (2020) Photoreceptor alteration in intermediate age-related macular degeneration. Sci Rep. https://doi.org/10.1038/s41598-020-78201-9
Inoue M, Jung JJ, Balaratnasingam C, et al (2016) A comparison between optical coherence tomography angiography and fluorescein angiography for the imaging of type 1 neovascularization. Investig Opthalmology Vis Sci 57:OCT314. https://doi.org/10.1167/iovs.15-18900
Jia Y, Bailey ST, Wilson DJ et al (2014) Quantitative optical coherence tomography angiography of choroidal neovascularization in age-related macular degeneration. Ophthalmology 121:1435–1444. https://doi.org/10.1016/j.ophtha.2014.01.034
Borrelli E, Souied EH, Freund KBB, et al (2018) Reduced choriocapillaris flow in eyes with type 3 neovascularization due to age-related macular degeneration. Retina. https://doi.org/10.1097/IAE.0000000000002198
Mai LE H, Souied EH, Querques G, et al (2021) Choriocapillaris flow impairment in type 3 macular neovascularization: a quantitative analysis using swept-source optical coherence tomography angiography. Retina. https://doi.org/10.1097/IAE.0000000000003119
Stefánsson E, Geirsdóttir Á, Sigurdsson H (2011) Metabolic physiology in age related macular degeneration. Prog Retin Eye Res 30:72–80
Querques G, Srour M, Massamba N et al (2013) Functional characterization and multimodal imaging of treatment-naive “quiescent” choroidal neovascularization. Invest Ophthalmol Vis Sci 54:6886–6892. https://doi.org/10.1167/iovs.13-11665
Roisman L, Zhang Q, Wang RK et al (2016) Optical coherence tomography angiography of asymptomatic neovascularization in intermediate age-related macular degeneration. Ophthalmology 123:1309–1319. https://doi.org/10.1016/j.ophtha.2016.01.044
Hanutsaha P, Guyer DR, Yannuzzi LA et al (1998) Indocyanine-green videoangiography of drusen as a possible predictive indicator of exudative maculopathy. Ophthalmology 105:1632–1636. https://doi.org/10.1016/S0161-6420(98)99030-3
de Oliveira Dias JR, Zhang Q, Garcia JMB et al (2017) Natural history of subclinical neovascularization in nonexudative age-related macular degeneration using swept-source OCT angiography. Ophthalmology 125(2):255–266
Yang J, Zhang Q, Motulsky EH, et al (2019) Two-year risk of exudation in eyes with nonexudative age-related macular degeneration and subclinical neovascularization detected with swept source optical coherence tomography angiography. Am J Ophthalmol. https://doi.org/10.1016/j.ajo.2019.06.017
Querques G, Sacconi R, Capuano V, et al (2021) Treatment-naïve quiescent macular neovascularization secondary to AMD: the 2019 Young Investigator Lecture of Macula Society. Eur J Ophthalmol. https://doi.org/10.1177/1120672120986370
Grossniklaus HE, Green WR (2004) Choroidal neovascularization. Am J Ophthalmol 137:496–503
Chen L, Messinger JD, Sloan KR, et al (2020) Non-exudative macular neovascularization supporting outer retina in age-related macular degeneration, a clinicopathologic correlation. Ophthalmology 0: https://doi.org/10.1016/j.ophtha.2020.01.040
Green WR, Enger C (1993) Age-related macular degeneration histopathologic studies: the 1992 Lorenz E. Zimmerman Lecture Ophthalmology 100:1519–1535. https://doi.org/10.1016/S0161-6420(93)31466-1
Killingsworth MC, Sarks JP, Sarks SH (1990) Macrophages related to Bruch’s membrane in age-related macular degeneration. Eye. https://doi.org/10.1038/eye.1990.86
Querques L, Parravano M, Borrelli E, et al (2020) Anatomical and functional changes in neovascular AMD in remission: comparison of fibrocellular and fibrovascular phenotypes. Br J Ophthalmol. https://doi.org/10.1136/bjophthalmol-2018-313685
Kuehlewein L, Bansal M, Lenis TL et al (2015) Optical coherence tomography angiography of type 1 neovascularization in age-related macular degeneration. Am J Ophthalmol 160:739-748.e2. https://doi.org/10.1016/j.ajo.2015.06.030
El Ameen A, Cohen SY, Semoun O et al (2015) Type 2 neovascularization secondary to age-related macular degeneration imaged by optical coherence tomography angiography. Retina 35:2212–2218. https://doi.org/10.1097/IAE.0000000000000773
Kuehlewein L, Sadda SR, Sarraf D (2015) OCT angiography and sequential quantitative analysis of type 2 neovascularization after ranibizumab therapy. Eye (Lond) 29:932–935. https://doi.org/10.1038/EYE.2015.80
Dansingani KK, Tan ACS, Gilani F et al (2016) Subretinal hyperreflective material imaged with optical coherence tomography angiography. Am J Ophthalmol 169:235–248. https://doi.org/10.1016/j.ajo.2016.06.031
Mastropasqua L, Toto L, Borrelli E, et al (2016) Optical coherence tomography angiography assessment of vascular effects occurring after aflibercept intravitreal injections in treatment-naive patients with wet AMD. Retina 1. https://doi.org/10.1097/IAE.0000000000001145
Dansingani KK, Freund KB (2015) Optical coherence tomography angiography reveals mature, tangled vascular networks in eyes with neovascular age-related macular degeneration showing resistance to geographic atrophy. Ophthalmic Surgery, Lasers Imaging Retin 46:907–912. https://doi.org/10.3928/23258160-20151008-02
Skalet AH, Miller AK, Klein ML et al (2017) Clinicopathologic correlation of retinal angiomatous proliferation treated with ranibizumab. Retina (Philadelphia, PA) 37(8):1620–1624
Li M, Dolz-Marco R, Messinger JD et al (2018) Clinicopathologic correlation of anti–vascular endothelial growth factor–treated type 3 neovascularization in age-related macular degeneration. Ophthalmology 125(2):276–287
Querques G, Querques L, Forte R et al (2013) Precursors of type 3 neovascularization: a multimodal imaging analysis. Retina 33:1241–1248. https://doi.org/10.1097/IAE.0b013e31827b639e
Capuano V, Souied EH, Miere A et al (2016) Choroidal maps in non-exudative age-related macular degeneration. Br J Ophthalmol 100:677–682. https://doi.org/10.1136/bjophthalmol-2015-307169
Sacconi R, Battista M, Borrelli E et al (2020) OCT-A characterisation of recurrent type 3 macular neovascularisation. Br J Ophthalmol 105(2):222–226
Spaide RF (2019) New proposal for the pathophysiology of type 3 neovascularization as based on multimodal imaging findings. Retina. https://doi.org/10.1097/IAE.0000000000002412
Borrelli E, Sacconi R, Klose G, et al (2019) Rotational three-dimensional OCTA: a notable new imaging tool to characterize type 3 macular neovascularization. Sci Rep. https://doi.org/10.1038/s41598-019-53307-x
Breazzano MP, Bacci T, Curcio CA, Freund KB (2020) Novel multimodal imaging and volume rendering of type 3 macular neovascularization. Retina. https://doi.org/10.1097/IAE.0000000000002892
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Borrelli, E., Bandello, F., Souied, E.H. et al. Neovascular age-related macular degeneration: advancement in retinal imaging builds a bridge between histopathology and clinical findings. Graefes Arch Clin Exp Ophthalmol 260, 2087–2093 (2022). https://doi.org/10.1007/s00417-022-05577-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-022-05577-x