Abstract
Purpose
To describe the types of strabismus operated on, the surgical procedures performed, and the 2-year reoperation rate in France.
Methods
Entire population 5-year cross-sectional analysis of a national medico-administrative database in France between January 2013 and December 2017 included all patients who underwent a first strabismus surgery, with a 2-year follow-up. Patient identification was based on the diagnostic codes of the 10th International Classification of Diseases and surgical procedures on the codes of the Common Classification of Medical Acts. A subgroup analysis comparing non-paralytic and paralytic strabismus was performed.
Results
Among the 56,654 patients included (women: 50.8%), 26,892 (47.5%) patients were under 10 years old. Overall, 52,711 (93%) were diagnosed with non-paralytic strabismus and 3,943 (7%) with paralytic strabismus. Among the non-paralytics, the most frequent diagnosis was esotropia (21,282, 37.6%), followed by exotropia (14,392, 25.4%) and vertical strabismus (2,017, 3.6%). Among the paralytics, fourth cranial nerve palsy (1,499, 2.6%) was more frequent than sixth cranial nerve palsy (691, 1.2%) and third cranial nerve palsy (431, 0.8%). The 2-year reoperation rate was 7.7% (4,362 patients), the lowest for non-paralytic (7.4%) and the highest for paralytic (11.4%).
Conclusion
This first French population-based study about strabismus will contribute to the evaluation of practices at a national level and permit comparisons between countries. Although the 2-year reoperation rate was found to be 1 out of 13 patients, it should be interpreted with caution. Long-term follow-up is still warranted due to considerable variability of the type and severity of strabismus as well as surgical practices.
Similar content being viewed by others
Avoid common mistakes on your manuscript.

Introduction
The prevalence of strabismus is highly variable in the literature, depending on the definition used and the geographical regions studied [1,2,3,4,5]. Patients with strabismus may require surgery to reduce ocular deviation, improve cosmetic appearance, and, at best, restore ocular alignment and fusion in case of normal retinal correspondence. Surgery is an important step in the treatment process, although some cases such as those with large deviations may require reoperation [6]. In an analysis of the US IRIS registry by Repka et al. [7], 4.8% of patients with a diagnosis of strabismus received their first surgical management, among which 6.7% received a reoperation within 1 year. In France, data concerning patients undergoing ocular surgery are collected through the medico-economic system called “Programme de Médicalisation des Systèmes d’Information” (PMSI). This database contains the diagnostic codes and surgical procedures performed for each patient, along with demographic information and hospital follow-up information. Previous studies have highlighted the usefulness of this database to perform large population-based epidemiological investigations in France (e.g., trends in glaucoma surgery [8], endophthalmitis following cataract surgery [9], or intravitreal injections [10]).
This study aimed to describe the types of strabismus operated on, the surgical procedures, and the 2-year reoperation rate in France.
Material and methods
Study design and participants
This French retrospective, multicenter, population-based study was conducted using data for the period from January 1st, 2011, to December 31st, 2020, from the national PMSI hospital discharge databases. According to the French law and regulation (MR005), 10-year data are available corresponding of the last decade (i.e., from 2011 to 2021). All patients who underwent strabismus surgery in France and French overseas departments (Guadeloupe, Martinique, Guyane, Mayotte, and La Réunion) between 2013 and 2017 were included in the cohort and represented the study population. The previous 2-year period 2011–2012 was necessary to accurately define the patient population of first strabismus surgery by excluding patients with a previous strabismus surgery in the past 24 months before the inclusion period. Patients who had therapeutic codes corresponding to a reoperation (BJMA008, BJMA009) were also excluded. Finally, only patients considered as having a first strabismus surgery were considered in the current study and followed over a 2-year period post-surgery.
The study was approved by the National Commission on Informatics and Liberty (n°2205437) and was in accordance with the ethical principles established in the Declaration of Helsinki. The institutional review board of the University Hospital of Tours approved this study.
Diagnostic and therapeutic codes
The French national administrative database PMSI collects administrative and medical (i.e., diagnoses and procedures) information on all hospital stays in France for epidemiological and financial purposes. Since 2005, the PMSI has been used for the implementation of activity-based pricing, the current remuneration system for French healthcare hospitals, both public and private. For each hospital stay, diagnostic codes based on the 10th edition of the International Classification of Diseases (ICD-10) and procedure codes from the Common Classification of Medical Acts [11] (CCAM: French common procedural terminology CPT) are collected.
As a patient can have a primary and several secondary ICD-10 diagnosis codes, prioritization was performed to retain only the diagnostic code corresponding to an etiological diagnosis rather than codes limited to an anatomical description (e.g., if the same patient was coded vertical strabismus and trochlear nerve palsy, only trochlear nerve palsy was retained) (Table 1).
For a given patient, several CPT codes can be found (e.g., displacement of a rectus muscle and displacement of an oblique muscle). Thus, the number of CCAM procedures was greater than the number of patients in the current study.
Data collection
For each patient, the following data were collected: demographics such as age (grouped by decade except for the first decade for which an interval of 2 years was chosen for greater accuracy, as patients under the age of 10 represented half of the cohort) and gender, hospital data such as public or private hospital, and length of stay (i.e., outpatient surgery, 1 night stay, or longer). The proportion of strabismus surgeries was calculated as the ratio of strabismus surgical procedures to all ophthalmological surgical therapeutic procedures. Non-surgical therapeutic procedures, procedures performed during consultation or in a dedicated room different from the operating room (e.g., removal of superficial foreign bodies, laser treatment performed during consultation, and intravitreal injection), and duplicates were excluded.
Reoperation rate within 24 months
The 2-year reoperation rate was defined by at least one supplementary strabismus surgery during the following 24 months (codes BJMA008 and BJMA009, corresponding to iterative surgeries, considered as exclusion criteria at inclusion were included in the calculation of the reoperation rate). Where applicable, the time to reoperation and the number of interventions were provided. The 2-year reoperation rate was compared between non-paralytic and paralytic strabismus groups.
Postoperative endophthalmitis
Acute postoperative endophthalmitis was identified using two ICD-10 specific codes (i.e., H440 for purulent endophthalmitis and H441 for other endophthalmitis) if it occurred during the 42 days following strabismus surgery [12].
Results
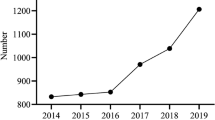
A total of 56,654 patients (50.8% women) were included in the study. Surgery was performed in a public versus a private hospital in 36.7% and 63.3%, respectively. Twenty-six thousand eight hundred and ninety-two (47.5%) were under the age of 10 years old. All age groups were concerned by strabismus surgery. The demographic distribution of patients operated on for strabismus is shown in Fig. 1. A total of 40,080 (70.7%) patients were treated as outpatients, 10,910 (19.3%) required a 1 night stay, and 5,664 (10%) required more than 1 night stay. The mean length of stay was 0.48 day in public hospitals and 0.41 day in private hospitals.
Strabismus types
The different types of strabismus are described in Table 1. Non-paralytic and paralytic strabismus corresponded respectively to 93% (52,711) and 7% (3,943) of all strabismus.
Therapeutic procedures
The 72,342 therapeutic procedures corresponding to a first surgery are described in Supplemental Table 1. The two most common procedures were unilateral (BJMA005) and bilateral (BJMA003) strengthening, weakening, or displacement of the insertion of two extraocular muscles corresponding respectively to 24.7% and 23.1%.
For non-paralytic esotropia and exotropia, surgery was most often performed on two extraocular muscles (respectively 61.2% and 62.9% (BJDA001 + BJMA003 + BJMA005)). Non-paralytic vertical strabismus was managed with a single-rectus muscle (BJMA002) surgery in 25.9% of cases and a single-oblique muscle surgery in 22.6% (BJMA004).
For paralytic strabismus, surgeries were mainly performed on one eye, irrespective of the type of strabismus. In cases of third cranial nerve palsy, procedures were highly variable although two-muscle surgery (BJMA005) was performed in 30.2% of cases. In case of fourth cranial nerve palsy, a strengthening, weakening, or displacement of the insertion of a single-oblique muscle (BJMA004) or an extraocular muscles transposition (BJEA001) was performed respectively in 41% and 29.7% of cases. In cases of sixth cranial nerve palsy, surgery was most often performed on one or two extraocular muscles, 21.6% on one muscle (BJMA002) and 25.7% on two muscles (BJMA005).
Strabismus surgery with adjustable sutures accounted for 3.5% of cases, while retroequatorial Cüppers myopexy for 12.3% and botulinum toxin injection for 1.4%.
Reoperation rate within 24 months
The 2-year reoperation rate was 7.7% (4,362) over the study period. In total, 6,996 (12.3%) required at least one reoperation from January 2013 to December 2020 (i.e., a maximum of 84 months for the first patient included in the study and a minimum of 36 months for the last patient included in the study). The median time between the first surgery and the first reoperation was 513 days (i.e., 1.4 years; Q1 = 257, Q3 = 1,022). Among the 6,996 patients who underwent at least one reoperation, 6,132 (87.7%) had a single reoperation, 706 (10.1%) 2 reoperations, 117 (1.7%) 3 reoperations, and 41 (0.6%) at least 4 reoperations.
The 2-year reoperation rate was higher in the paralytic group compared with the non-paralytic group (11.4% versus 7.4%).
In the non-paralytic strabismus group, 284 (14.1%) patients with vertical strabismus, 1,140 (7.9%) patients with exotropia, and 1,247 (5.9%) patients with esotropia had at least one reoperation within 24 months.
In the paralytic strabismus group, 74 (17.2%) patients with third cranial nerve palsy, 115 (16.6%) with sixth cranial nerve palsy, and 140 (9.3%) with fourth cranial nerve palsy had at least one reoperation within 24 months.
Postoperative endophthalmitis
Endophthalmitis was reported in only 3 cases during the 42 postoperative days among the 56,654 patients.
Discussion
This national cross-sectional study of more than 56,000 patients provides a contemporary view of strabismus management occurring over the 5-year period for patients hospitalized for surgery with a 24-month follow-up. We observed that strabismus surgery accounts for 2% of all eye surgery procedures and mainly concerns children (1 out of 2 aged below 10 years). In more than 9 out of 10 patients, indication was non-paralytic strabismus, including 37.6% of convergent deviations, 25.4% of divergent deviations, and 3.6% of vertical deviations. The 2-year reoperation rate was 7.7%, but was highly variable between groups. Paralytic strabismus displayed a higher rate of reoperation when compared to non-paralytic strabismus (11.4% versus 7.4%). Within the non-paralytic group, the reoperation rate was higher for vertical deviations followed by divergent and convergent deviations. Moreover, the large dataset allowed an assessment of the risk of endophthalmitis, and highlighted the rarity of the occurrence.
The use of medico-administrative databases has already proven its usefulness and relevance in several ophthalmological conditions. Daien et al. [13] evaluated epidemiological factors and safety of ophthalmological procedures in France (thanks to the EPISAFE program (Epidemiology and Safety in Ophthalmology)). Other French studies have investigated the rate of postoperative endophthalmitis following vitreoretinal and combined surgery [9, 14]. Several population-based studies have been performed worldwide on various databases: the IRIS registry in the USA [15], the UK Ophthalmology Database [16], and the Swedish National Cataract Register [17]. Despite this, strabismus has been poorly studied using this “big data” approach. To date, the study performed by Repka et al. [7] on the IRIS registry is one of the largest of its kind on strabismus and the only population-based study that can be compared with the current findings.
In France, strabismus surgery is performed for one-third in public hospitals and for two-thirds in private hospitals. These hospitals are not distributed uniformly on the French territory and access to care is unequal for all French citizens. Most strabismus surgeries are performed on an outpatient basis. Nevertheless, this represents only two-thirds (70.7%) of patients. The trend towards outpatient care will increase in the coming years.
In our study, 93% of patients operated on had non-paralytic strabismus (of whom 37.6% had esotropia and 25.4% exotropia) and 7% had paralytic strabismus. In comparison, Repka et al. reported 30.6% of esotropia, 21.8% of exotropia, and 3.4% of paralytic strabismus [7]. Our findings are similar to those from the IRIS registry, suggesting that the proportions of each strabismus category requiring surgery may be comparable between countries.
One out of 13 patients was re-operated on during the following 24 months after initial strabismus surgery. The reoperation rate was highly variable and correlated with the type of strabismus (i.e., higher for paralytics) as well as the type of deviation (i.e., highest for non-paralytic vertical deviations while lowest for non-paralytic convergent deviations). The 2-year reoperation rate found in our study is comparable with the 1-year reoperation rate found by Repka et al. (6.7%) [7]. In their study, no subgroup analysis based on the type of strabismus was performed, but the 1-year reoperation rate positively correlated with age. This correlation could be related to the higher incidence of paralytic strabismus in older patients and could therefore represent a confusion bias. A retrospective single-center study performed in Canada over a 21-year period on 6177 patients found a reoperation rate of 15.7% [6]. The longer the follow-up period, the higher the reoperation rate. This assumption is supported by an increase in the reoperation rate from 7.7 over a 2-year period to 12.3% with a maximum follow-up period of 7 years in our study. In both Benson et al.’s study and the current study, most patients required only one reoperation (respectively 77.7% and 87.7%), while fewer patients underwent 2 reoperations (respectively 17.1% and 10.1%). The mean time for reoperation was comparable between Benson et al. and our study (respectively 2.3 and 1.9 years). Together, this suggests that when necessary, reoperation is mainly performed within 2 years following initial intervention. Reoperation cannot be solely considered as a failure of initial surgery. The reoperation rate should be interpreted with caution as reoperation can be a necessary step to correct complex cases or due to failure or recurrence. On the contrary, reoperation may not be performed in some patients even despite failure or recurrence. The surgical indication for strabismus must take into account the extent of deviation, the symptoms, the impact on vision-related quality of life, and the aesthetic discomfort experienced by the patient.
Strabismus surgery is presented as a safe procedure in terms of infectious complications. Despite this, endophthalmitis can occur even in the absence of scleral perforation while performing muscle recession or resection [18]. Considering the rarity of such complications, large-scale studies are needed. Our population-based findings confirm that endophthalmitis is an uncommon complication following strabismus surgery. Since endophthalmitis is a vision-threatening condition, it would seem unlikely that patients with such a complication were missed because not treated. Moreover, the corresponding diagnostic code is systematically implemented when a patient is hospitalized.
Studies based on medical administrative databases are classified at an intermediate level according to the Oxford Evidence Based Medicine Recommendations [19]. These studies, however, are complementary to randomized controlled trials, which have a higher level of scientific evidence, the latter being carried out under ideal follow-up conditions for a smaller number of selected patients. Population-based investigations under real conditions of practice avoid center effects and allow the study of rare events. These data can then be used to evaluate the epidemiology of diseases on a country-wide scale and to adapt medical care accordingly based on the completeness, routine implementation, and follow-up of the cases.
Furthermore, as the PMSI contributes to the financing of French public and private healthcare establishments, its database is all the more exhaustive, as complete filing for each patient by physicians is an essential prerequisite for the reimbursement of healthcare structures by the health agencies. By comparison, the IRIS registry is implemented with data reported by volunteer ophthalmologists who represent only 42% of the ophthalmologists in the USA. This allows for an analysis of current clinical practices, but does not permit an epidemiological assessment at the national level.
Several limitations to this study must be acknowledged. First, the use of administrative hospital databases introduced an inherent bias to importantly consider. The strengths and limitations of using healthcare databases for epidemiological purposes have already been extensively discussed [20,21,22,23,24]. Hence, while the PMSI is designed for billing purposes, it occurs now to be a powerful tool for epidemiological surveillance. One must keep in mind, however, that observed changes in disease patterns could be biased by variations in coding practices due to financial incentives for obtaining higher reimbursement rates [25]. In our study, 24% of patients were operated on for unspecified non-paralytic strabismus (H508, H509), thus limiting the interpretation of the data obtained. Second, some concerning issues are not recorded in the hospital discharge database; for instance, there are no clinical data (e.g., amplitude of the deviation or the therapeutic codes do not specify which muscles were operated on and whether it was a recession, plication, or resection). Third, since this study was performed in only one country, the extrapolation of our findings to other countries may be limited. Fourth, surgical practices can be highly variable owing to a wide range of strabismus types, severity, and aetiologies as well as differences between surgeons’ personal experience.
To date, this is the first population-based study in France for patients with strabismus requiring surgery. These findings will serve as a reference for comparisons between countries. A national medico-administrative database contributes to the evaluation of clinical practices and provides patients and surgeons with reliable epidemiological data on their disease and the 2-year reoperation rate (1 out of 13). Still, patients should undergo life-long follow-up since surgery does not represent a cure as strabismus are most often not related to a muscular problem but rather to an impairment of the eye movement control system.
Abbreviations
- CCAM:
-
Common Classification of Medical Acts
- ICD-10:
-
10Th edition of the International Classification of Diseases
- PMSI:
-
Programme de Médicalisation des Systèmes d’Information
References
Multi-ethnic Pediatric Eye Disease Study Group (2008) Prevalence of amblyopia and strabismus in African American and Hispanic children ages 6 to 72 months the multi-ethnic pediatric eye disease study. Ophthalmology 115:1229-1236.e1. https://doi.org/10.1016/j.ophtha.2007.08.001
McKean-Cowdin R, Cotter SA, Tarczy-Hornoch K et al (2013) Prevalence of amblyopia or strabismus in asian and non-Hispanic white preschool children: multi-ethnic pediatric eye disease study. Ophthalmology 120:2117–2124. https://doi.org/10.1016/j.ophtha.2013.03.001
Martinez-Thompson JM, Diehl NN, Holmes JM, Mohney BG (2014) Incidence, types, and lifetime risk of adult-onset strabismus. Ophthalmology 121:877–882. https://doi.org/10.1016/j.ophtha.2013.10.030
Bruce A, Santorelli G (2016) Prevalence and risk factors of strabismus in a UK multi-ethnic birth cohort. Strabismus 24:153–160. https://doi.org/10.1080/09273972.2016.1242639
Hashemi H, Fotouhi A, Yekta A et al (2018) Global and regional estimates of prevalence of refractive errors: systematic review and meta-analysis. J Curr Ophthalmol 30:3–22. https://doi.org/10.1016/j.joco.2017.08.009
Benson MD, Wozniak J, MacDonald IM (2019) An analysis of strabismus reoperations in Northern Alberta, Canada from 1995 to 2015. Can J Ophthalmol 54:94–97. https://doi.org/10.1016/j.jcjo.2018.04.007
Repka MX, Lum F, Burugapalli B (2018) Strabismus, strabismus surgery, and reoperation rate in the United States. Ophthalmology 125:1646–1653. https://doi.org/10.1016/j.ophtha.2018.04.024
Bron AM, Mariet A-S, Benzenine E et al (2017) Trends in operating room-based glaucoma procedures in France from 2005 to 2014: a nationwide study. Br J Ophthalmol 101:1500–1504. https://doi.org/10.1136/bjophthalmol-2016-309946
Creuzot-Garcher C, Benzenine E, Mariet A-S et al (2016) Incidence of acute postoperative endophthalmitis after cataract surgery: a nationwide study in France from 2005 to 2014. Ophthalmology 123:1414–1420. https://doi.org/10.1016/j.ophtha.2016.02.019
Baudin F, Benzenine E, Mariet A-S et al (2018) Association of acute endophthalmitis with intravitreal injections of corticosteroids or anti-vascular growth factor agents in a nationwide study in France. JAMA Ophthalmol 136:1352–1358. https://doi.org/10.1001/jamaophthalmol.2018.3939
Bousquet C, Trombert B, Souvignet J et al (2010) Evaluation of the CCAM hierarchy and semi structured code for retrieving relevant procedures in a hospital case mix database. AMIA Annu Symp Proc 2010:61–65
(1995) Results of the endophthalmitis vitrectomy study. A randomized trial of immediate vitrectomy and of intravenous antibiotics for the treatment of postoperative bacterial endophthalmitis. Endophthalmitis Vitrectomy Study Group. Arch Ophthalmol 113:1479–1496
Daien V, Korobelnik J-F, Delcourt C et al (2017) French medical-administrative database for epidemiology and safety in ophthalmology (EPISAFE): the EPISAFE collaboration program in cataract surgery. Ophthalmic Res 58:67–73. https://doi.org/10.1159/000456721
Ben Ghezala I, Mariet A, Benzenine E, et al (2020) Incidence of acute postoperative endophthalmitis following macular surgery in France between 2006 and 2016. Acta Ophthalmol 98: https://doi.org/10.1111/aos.14279
Coleman AL (2015) How big data informs us about cataract surgery: the LXXII Edward Jackson memorial lecture. Am J Ophthalmol 160:1091-1103.e3. https://doi.org/10.1016/j.ajo.2015.09.028
Day AC, Donachie PHJ, Sparrow JM et al (2015) The Royal College of Ophthalmologists’ National Ophthalmology Database study of cataract surgery: report 1, visual outcomes and complications. Eye (Lond) 29:552–560. https://doi.org/10.1038/eye.2015.3
Zetterberg M, Montan P, Kugelberg M et al (2020) Cataract surgery volumes and complications per surgeon and clinical unit: data from the Swedish National Cataract Register 2007 to 2016. Ophthalmology 127:305–314. https://doi.org/10.1016/j.ophtha.2019.10.007
Zloto O, Mezer E, Ospina L et al (2017) Endophthalmitis following strabismus surgery: IPOSC Global Study. Curr Eye Res 42:1719–1724. https://doi.org/10.1080/02713683.2017.1351569
OCEBM Levels of Evidence Working Group (2011) “ The Oxford 2011 levels of evidence.” Oxford Centre for Evidence-Based Medicine. http://www.cebmnet/indexaspx?o=5653
Jouan Y, Grammatico-Guillon L, Espitalier F et al (2015) Long-term outcome of severe herpes simplex encephalitis: a population-based observational study. Crit Care 19:345. https://doi.org/10.1186/s13054-015-1046-y
Sunder S, Grammatico-Guillon L, Baron S et al (2015) Clinical and economic outcomes of infective endocarditis. Infect Dis (Lond) 47:80–87. https://doi.org/10.3109/00365548.2014.968608
Grammatico-Guillon L, Baron S, Gettner S et al (2012) Bone and joint infections in hospitalized patients in France, 2008: clinical and economic outcomes. J Hosp Infect 82:40–48
Grammatico-Guillon L, Baron S, Gaborit C et al (2014) Quality assessment of hospital discharge database for routine surveillance of hip and knee arthroplasty-related infections. Infect Control Hosp Epidemiol 35:646–651
Grammatico-Guillon L, Baron S, Rosset P et al (2015) Surgical site infection after primary hip and knee arthroplasty: a cohort study using a hospital database. Infect Control Hosp Epidemiol 36:1198–1207
Rhee C, Gohil S, Klompas M (2014) Regulatory mandates for sepsis care—reasons for caution. N Engl J Med 370:1673–1676. https://doi.org/10.1056/NEJMp1400276
Acknowledgements
The English in this manuscript has been checked by A.D.T. International - L'Agence de Traduction.
Author information
Authors and Affiliations
Contributions
QC, JC, SA, PJP, LGG, and RKK were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be published. RKK had full access to all of the data in the study and takes responsibility for the integrity and the accuracy of the data.
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The local Ethics Committee of the University Hospital of Tours approved this study. No nominative, sensitive, or personal data on patients were collected. Our study involves the reuse of already recorded and anonymized data. The study falls within the scope of the French reference methodology MR-005 according to 2016–41 law dated January 26th, 2016, on the modernization of the French health system, which requires neither information nor non-opposition of the included individuals. Access to linked anonymous file in the PMSI databases was approved by the French National Commission for Data Protection and Liberties (CNIL MR-005 number 3014040220).
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Colas, Q., Capsec, J., Arsène, S. et al. Strabismus outcomes after surgery: the nationwide SOS France study. Graefes Arch Clin Exp Ophthalmol 260, 2037–2043 (2022). https://doi.org/10.1007/s00417-021-05541-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-021-05541-1