Abstract
Purpose
This study aims to determine the 5-year visual field progression and identify the prognostic factors for progression in Malay patients with primary glaucoma.
Methods
A retrospective cohort record review study was conducted among 222 patients (222 eyes) with primary glaucoma who were selected from a glaucoma research database of a tertiary center in Malaysia. The patients were Malays and diagnosed with primary open-angle glaucoma (POAG) or primary angle-closure glaucoma (PACG). Patients who were followed up regularly for at least 6 months between 1 January 2009 and 31 December 2014 and completed another 1-year follow-up after recruitment (between 1 January 2015 and 31 December 2015) were selected. Multiple prognostic factors that influence visual field progression were identified. Progression of visual field loss was based on the Advanced Glaucoma Intervention Study and Hodapp–Parrish–Anderson scores. Kaplan–Meier survival and Cox proportional hazard regression analyses were performed.
Results
Sixty-three patients (28.4%) developed visual field progression after a mean (SD) follow-up of 6.9 (3.3) years. Those with POAG progressed faster (mean time, 10.6 years; 95% confidence interval [CI], 9.3, 11.9) than those with PACG (17.3 years; 95% CI, 14.8, 19.9) but not statistically significant. Disc hemorrhage and history of eye pain increased the risk of progression by 2.8-folds (95% CI, 1.6, 4.8) and 2.5-folds (1.4, 4.4), respectively.
Conclusion
The 5-year survival of the Malay primary glaucoma patients with visual field progression was similar with that of other Asian populations. However, aggressive management is required for those with disc hemorrhages and eye pain related to increased intraocular pressure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.

Introduction
The improvement of health care over the past decades has increased the life span of Asians, which might have contributed to the higher incidence of age-related diseases such as glaucoma. Asians account for 59.76% of the total world population [1]. Glaucoma is known as the most common cause of blindness in Asia [2, 3]. Previous studies estimated that the higher prevalence of blindness due to glaucoma in Asia is owing to the higher incidence of primary angle-closure glaucoma (PACG) [4, 5].
Asia consists of a heterogenous population, making it a melting pot [6]. Accordingly, the prevalence of glaucoma varies among Asian populations. Malays are the people who reside in the Malay Archipelago, which includes Malaysia, Indonesia, Singapore, Thailand, Brunei, and the Philippines. They compose 4.2% of the world population [7]. Although approximately 300 million people of Malay ethnicity live in Asia [8], information on the burden, causes, risk factors, and epidemiology of blinding eye diseases in this ethnic group is lacking. Most knowledge about eye diseases has been derived from Chinese, Japanese, and Indian populations [6, 9,10,11], but little knowledge is known in the Malay population. Thus, so far, the Singapore Malay Eye Study provides the only available epidemiological data on ocular diseases in Malays [12]. The prevalence of glaucoma was reported to be 4.6, with prevalence rates of 3.2 and 0.2 for primary open-angle glaucoma (POAG) and PACG, respectively [12]. Thus, understanding glaucoma in this subethnic group of Asians is of profound importance.
On the basis of the National Eye Survey II conducted in Malaysia to determine the causes of blindness and visual impairment in persons aged ≥ 50 years, glaucoma is responsible for 6.6% of all cases of blindness [13]. While most other causes of blindness in this survey are reversible blindness, 58% were due to cataract, 5% were due to cataract surgery-related complications, and 3.5% were due to corneal opacity [13]. As the aging population is increasing exponentially, understanding the characteristic of the progression rate and factors affecting visual field progression in Malay patients with glaucoma is crucial. According to Department of Statistics Malaysia, Malays account for 69.8% of the population in Malaysia [14]. To prepare Malaysia to be an aging country, these data are crucial for rehabilitation and prevention of blindness among older adults. The main objective of this study was to determine the 5-year survival rate and factors affecting visual field progression in Malay patients with POAG and PACG.
Materials and methods
A retrospective cohort record review was conducted in patients with POAG and PACG who were treated and followed up at Hospital Universiti Sains Malaysia (HUSM), a tertiary center in Kelantan, in the east coast of Malaysia. Kelantan is one of the states whose populations are mostly Malays [15]. This study received ethical approval from the research and ethics committee of the School of Medical Sciences, Universiti Sains Malaysia (reference code, USM/JePEM/16090340).
Potential patients were identified from the Malay Glaucoma Eye Study (MaGES) database created in 2014. This database was established to study the modifiable risk factors of POAG and PACG in Malay patients. POAG is characterized as a chronic, slowly progressive visual field loss and optic nerve cupping, often associated with an elevated intraocular pressure (IOP) and visually open anterior chamber angles on gonioscopy, without any underlying secondary ocular disease [16]. PACG is defined as an eye condition that presents with 180º or more occludable drainage angle and features that indicate trabecular obstruction by the peripheral iris, such as an increased IOP of > 21 mmHg, peripheral anterior synechiae, iris whirling, “glaucomflecken” lens opacities, or excessive pigment deposition on the trabecular surface with evidence of glaucomatous optic neuropathy [17]. In our database, the Malay patients were Muslims who descended from at least three generations, without interracial marriages, spoke Malay as their first language, and practiced Malay customs. They had already undergone screening for eligibility, which included the use of a pedigree chart to exclude any potential interracial marriages in three generations of their lineage, before entry into the database.
The MaGES database is comprised of 750 Malay patients who were recruited from four tertiary centers in Malaysia, namely, HUSM, Hospital Sultanah Bahiyah, Hospital Sultanah Nur Zahirah, and Hospital Kuala Lumpur. Of the 750 patients, only 265 were from HUSM. MaGES database only included Malay patients who fulfilled the diagnosis of POAG and PACG with good follow-up record and achieved target pressure for the last one year. The recruited patients must provide two reliable and reproducible visual fields within 3 months of the recruitment period. Patients with underlying retinal, media opacities, neuro-ophthalmology, or other systemic neurological disease that interferes with visual field interpretation were excluded. Myopic patients with refractive error of ≥ 4 diopters were also excluded. Those with dementia, chronic or persistent disorder of the mental processes, brain disease or injury, memory disorder, and psychotic instability were also excluded.
The medical records of the selected patients were traced. All the recruited patients must have at least six reliable and reproducible visual fields using the Humphrey visual field (HVF) based on the Swedish Interactive Threshold Algorithm standard 24–2 analysis. The reliability of the HVF is based on the reliability index of the visual field. A reliable visual field includes a fixation loss of < 20%, false-negative result of < 33%, and false-positive result of < 33% [18]. Of the 265 patients identified from the database, 28 were diagnosed after December 31, 2015, six failed to complete 5 years of follow-up or a minimum of 18 eye clinic visits, and seven failed to produce six reliable and reproducible HVFs. A total of 222 patients (222 eyes) who had primary glaucoma (POAG and PACG) and who were diagnosed and followed up for a minimum period of 5 years (minimum of 18 eye clinic visits) between January 1, 2009, and December 31, 2014, were included. They were also required to be followed up for another year between January 1, 2015, and December 31, 2015.
Scoring of the HVF was performed by two glaucoma consultants (LS and AY) using the Hodapp–Parrish–Anderson (HPA) scoring system [19] and Advanced Glaucoma Intervention Study (AGIS) criteria [20]. They were blinded from each other’s scoring. Visual field progression is defined when the HPA score indicates changes in severity [21] and the worsening of 4 unit based on AGIS score [22, 23]. Time of progression refers to the duration between the time of the initial diagnosis and the time when the first VF progression was detected (in years). Only the right eye was selected for HVF scoring if both eyes were eligible for recruitment. Based on the definition of progression, the patients were divided into two groups: a progression group and a non-progression group.
The medical records of the selected patients were traced. Data were collected by three investigators (WEA, HAS, and DTSJ) and divided into ocular and systemic parameters. Ocular parameters included the presence of ocular pain, red eye, and symptoms of acute angle-closure (AAC); visual acuity and IOP at diagnosis; laterality; vertical cup-to-disc ratio (VCDR); disc hemorrhage; central corneal thickness; and treatment given. The IOPs at diagnosis (baseline); 12, 24, and 36 months after diagnosis; and the time of recruitment were also recorded. The presence of other systemic comorbidities such as hypertension, diabetes mellitus, and hyperlipidemia were noted. These parameters were used as potential prognostic factors in the analysis. Any patients with missing data of > 30% were excluded. None of our patients were excluded owing to this reason.
All data were entered into the Statistical Program for Social Science (SPSS) version 22.0 software. They were checked and cleaned to ensure accurate documentation and to eliminate any missing or erroneous values (NMY and NSB). The SPSS and Statistical Data Analysis (STATA) version 22.0 software were used for the statistical analysis. For all the numerical variables, the normality distribution was assessed. A Kaplan–Meier survival probability curve was plotted to estimate the progression of glaucoma on the basis of the visual field progression [24]. Multivariable analysis using the Cox proportional hazard regression model was used to identify the prognostic factor for the progression of glaucoma. All covariates with p values < 0.25 in the univariable analysis or that were clinically important were included in the multivariable analysis. The parsimonious model refers to the simplest model with the fewest possible number of significant variables.
Results
In this study, 110 patients with POAG and 112 patients with PACG were recruited. The study included 113 (50.9%) female and 109 (49.1%) male patients who were followed up for a mean (SD) duration of 6.5 (3.6) years. Patients with visual field progression were significantly older at the time of recruitment and followed up for a shorter duration (Table 1). Most patients had a bilateral disease. A significantly higher percentage of those with a history suggestive of acute IOP elevation developed visual field progression (Table 2). Disc hemorrhage was found in 35 eyes, of which 54.3% developed visual field progression (Table 2).
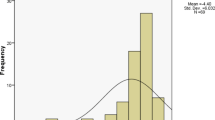
Based on two event analyses of HVF, 63 eyes (28.4%) were confirmed to have visual field progression. The Kaplan–Meier analysis estimated that the cumulative probability of non-progression was 79.8% at 5 years of follow-up (Fig. 1). The estimated median time of progression was 12.0 (95% confidence interval [CI], 8.5, 15.5) years, which indicated 50% of the study population were expected to progress at this timeline. No significant difference in cumulative probability of non-progression was found between the patients with POAG (67.4%) and those with PACG (70.2%) (Fig. 2, Table 3). In general, PACG progressed slower than POAG but not significantly (Tables 2 and 3). However, the female patients had a lower cumulative probability of non-progression (67.5%) than the male patients (70.1%) at 5 years, but the difference was not statistically significant (Tables 1 and 3).
The Malay patients with a history of ocular pain and red eyes had a significantly higher probability of progression based on the Kaplan–Meier survival analysis (Tables 2 and 3). The probability of progression was also higher in the patients with disc hemorrhage (Tables 2 and 3). These predictors were significant in the simple Cox regression analysis, but only disc hemorrhage and ocular pain remained significant in the multiple Cox regression analysis (Table 4). The presence of disc hemorrhage increased the risk of visual field progression by 2.8-folds (95% CI, 1.61–4.76). The patients with a history of ocular pain had a 2.5-folds (95% CI, 1.37–4.44) increased risk of visual progression.
Discussion
The progression of glaucoma is subtle and often asymptomatic, which leads to late detection [4]. The absence of a standardized definition of progression further complicates the issue. Visual field changes are the features most commonly adopted in the definition of glaucoma progression [25]. Currently, with the popularity of optical coherent tomography (OCT), progression can now be detected on the basis of structural changes [26].
Visual field progression can be defined using an event- or trend-based analysis. In the present study, progression was defined based on the agreement of the results of two event-based analysis, namely, the AGIS score and HPA classification. A total of 63 patients (28.4%) with primary glaucoma were found to show visual field progression after 6 years of follow-up. The Kaplan–Meier analysis revealed that the cumulative probability of survival of the patients with no progression was 79.8% at 5 years, which was interpreted as an estimation of visual field progression of 20.2% at 5 years of follow-up in the patients with POAG and PACG. So far, no similar study has combined these two most common types of primary glaucoma.
Survival analysis for visual field progression in patients with POAG is often performed as the outcome of treatment or surgical intervention in many large prospective randomized controlled trials such the AGIS, Early Manifest Glaucoma Treatment Study (EMGTS), and Collaborative Initial Glaucoma Treatment Study [20, 27, 28]. Chen et al. found that 14.6% of patients with OAG became blind after 15 years of follow-up on the basis of their Kaplan–Meier survival analysis results [2]. Hattenhauer et al. found that 27% of patients with POAG became blind after 20 years of follow-up [29]. By using a special software analysis, many studies defined progression based on the rate of progression [30,31,32]. Thus, direct comparison between studies is difficult because they used different definitions of progression.
Visual field defect in PACG eyes is more diffuse [33]. Both POAG and PACG eyes showed more pronounced damage in superior hemifield but with higher tendency in POAG eyes [33, 34]. Based on mean deviation, the rate of visual field progression is faster in Asian patients with POAG [34,35,36]. The rate of progression predicts visual field defect per year and differs from estimation of cumulative probability of progression in survival analysis. However, if one presumed that the rate of progression is constant, the summation over the years may represent the cumulative probability of progression. Perhaps the cumulative effect of the rate of progression causes shorter median time to progress in Malay patients with POAG. Baseline visual field defect determines the subsequent progression. POAG eyes showed faster rate of progression compared to PACG eyes with similar baseline visual field defect [35]. However, baseline visual field of both type of glaucoma was not matched in the present study.
In Asian patients, PACG is believed to progress faster than in Caucasian patients [37, 384]. PACG is believed to be more aggressive in Malays than in Chinese [39, 40]. However, no significant difference in the percentage of progression was found between POAG (31.8%) and PACG (25.0%) in the present study. In fact, patients with PACG showed a higher cumulative probability of non-progression at 5 years of follow-up, with a longer estimated mean time of progression than POAG but with no statistically significant difference. Quek et al. reported that 32.5% of Chinese patients with PACG developed visual field progression after 10 years of follow-up [41]. On the basis of an indirect comparison, our study showed a slightly higher cumulative probability of non-progression at 5 and 10 years than their study. However, this analysis was not described in detail in their study. Apart from this discrepancy, the differences in follow-up duration and definition of progression make direct comparison impossible. Different methods of assessment cause a discrepancy in the detection of visual field progression [23]. Our study adopted a stricter definition of progression, which might have contributed to the lower percentage of visual field progression.
In general, PACG is more common in women, and men are more predisposed to POAG [42, 43]. However, no evidence has been found to support the role of sex in the progression and severity of glaucoma. Female patients were more likely to develop visual progression in the present study. Though not statistically significant, they had a lower cumulative probability of non-progression (67.5% at 5 years) but longer estimated time (15.1 years) of progression than men. Women have longer life spans, which increase the likelihood of progression at a later age [44,45,46].
In this study, disc hemorrhage was a strong predictor of progression in Malay patients with primary glaucoma. The cumulative probability of non-progression was 40.5% at 5 years in the patients who presented with disc hemorrhage. Drance et al. found that the presence of disc hemorrhage reduced the survival time to 1187 days compared with the 2159 days in those without disc hemorrhage [47]. Disc hemorrhage was also found to increase the risk of progression by 2% in the EMGTS [44]. It is known to cause a localized progression of visual field defect [45, 46]. In the present study, disc hemorrhage increased the risk of progression by 2.8-folds (95%CI 1.61, 4.76), which is almost similar to the finding reported by Drance et al. [47]. Disc hemorrhage was strongly associated with glaucoma progression in many prospective cohort studies [48, 51,52,53].
POAG is almost asymptomatic; however, many cases of sudden elevation of IOP have been reported [54]. Elevation of IOP may present with painful red eye [55]. PACG is more symptomatic especially in patients with a history of AAC [56]. However, not all patients with AAC will develop PACG if proper prompt treatment is given [57]. On the other hand, many cases of asymptomatic PACG that behave similarly to POAG have been reported especially in Asians [38, 39, 58]. Such cases were also observed in this study, with only a third of the patients with PACG presenting with a history of AAC. Fluctuation of IOP is known to cause further glaucomatous damage [59, 60]. In this study, a significant difference in 5-year progression of visual field was found between the patients with and those without eye pain.
The risk of progression was 2.5-folds (95% CI, 1.37–4.44) higher in the presence of eye pain but with no statistical significance. The presence of red eye increased the risk of progression of PACG by 2.7-folds (95% CI, 1.07–6.93) in a retrospective study involving all spectrums of primary angle-closure [39]. Including patients with POAG probably reduced the significant role of red eye in the present study. On the other hand, the incidence of eye pain and red eye may overlap with symptoms of AAC in patients with PACG. The retrospective nature of this study might likely be responsible for this bias.
In addition, owing to the nature of this study, several confounding factors could not be included because of missing data. This includes IOP fluctuation during follow-up. As structural changes preceded the visual field changes, the changes may be inaccurate because of the discrepancy during clinical observation. Our retrospective review was conducted during the time when diagnostic imaging was not available for the optic nerve head. A prospective cohort study will provide a better understanding of progression in Malay patients. PACG has different presentations from POAG; thus, a separate analysis of the prognostic factors for progression in patients with PACG is important.
In conclusion, the prevalence rate of visual field progression in Malay patients with primary glaucoma was 28.4%, and the median time for progression was 12.0 years (95% CI, 8.5–15.5). The visual field progression in Malay patients was almost similar with that in other Asian populations. The risk of progression was higher in the eyes with disc hemorrhage and history of eye pain, which warrant early detection and aggressive management.
Data availability
The data sets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
References
Worldometer (2021) Asia population (live). https://www.worldometers.info/world-population/asia-population/ Accessed 7 Aug 2021
Chen PP (2003) Blindness in patients with treated open-angle glaucoma. Ophthalmology 110:726–733. https://doi.org/10.1016/S0161-6420(02)01974-7
Resnikoff S, Pascolini D, Etya’ale D, Kocur I, Pararajasegaram R, Pokharel GP, Mariotti SP (2004) Global data on visual impairment in the year 2002. Bull World Health Organ 82:844–851. https://doi.org/10.1590/S0042-96862004001100009
Quigley HA, Broman AT (2006) The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol 90:262–267. https://doi.org/10.1136/bjo.2005.081224
Rao A (2012) Blindness and long-term progression of visual field defects in Chinese patients with primary angle-closure glaucoma. Am J Ophthalmol 153: 382; author reply 382–383. https://doi.org/10.1016/j.ajo.2011.11.013
Stein JD, Kim DS, Niziol LM, Talwar N, Nan B, Musch DC, Richards JE (2011) Differences in rates of glaucoma among Asian Americans and other racial groups, and among various Asian ethnic groups. Ophthalmology 118:1031–1037. https://doi.org/10.1016/j.ophtha.2010.10.024
US Census Bureau (2021) Malaysia. https://www.census.gov/popclock/world/my Accessed 1 July 2021
Wikipedia (2021) Malays (ethnic group). https://en.wikipedia.org/wiki/Malays_(ethnic_group) Accessed 23 September 2021
Hung KH, Cheng CY, Liu CJ (2015) Risk factors for predicting visual field progression in Chinese patients with primary open-angle glaucoma: a retrospective study. J Chin Med Assoc 78:418–423. https://doi.org/10.1016/j.jcma.2015.02.004
Sakata R, Yoshitomi T, Iwase A, Matsumoto C, Higashide T, Shirakashi M, Aihara M, Sugiyama K, Araie M, Lower Normal Pressure Glaucoma Study Members in Japan Glaucoma S (2019) Factors associated with progression of Japanese open-angle glaucoma with lower normal intraocular pressure. Ophthalmology 126: 1107-1116. https://doi.org/10.1016/j.ophtha.2018.12.029
Gothwal VK, Reddy SP, Bharani S, Bagga DK, Sumalini R, Garudadri CS, Rao HL, Senthil S, Pathak-Ray V, Mandal AK (2012) Impact of glaucoma on visual functioning in Indians. Invest Ophthalmol Vis Sci 53:6081–6092. https://doi.org/10.1167/iovs.12-9885
Rosman M, Zheng Y, Lamoureux E, Saw SM, Aung T, Tay WT, Wang JJ, Mitchell P, Tai ES, Wong TY (2012) Review of key findings from the Singapore Malay Eye Study (SiMES-1). Singapore Med J 53:82–87
Chew FLM, Salowi MA, Mustari Z, Husni MA, Hussein E, Adnan TH, Ngah NF, Limburg H, Goh PP (2018) Estimates of visual impairment and its causes from the National Eye Survey in Malaysia (NESII). PLoS ONE 13:e0198799. https://doi.org/10.1371/journal.pone.0198799
Department of Statistics Malaysia Official Portal (2021) Current population estimates, Malaysia, 2021.https://www.dosm.gov.my/v1/index.php?r=column/cthemeByCat&cat=155&bul_id=ZjJOSnpJR21sQWVUcUp6ODRudm5JZz09&menu_id=L0pheU43NWJwRWVSZklWdzQ4TlhUUT09. Accessed 15 July 2021
Population C (2010) Kelantan. https://www.citypopulation.de/en/malaysia/admin/03__kelantan/. Accessed 6 July 2021
(2017) European Glaucoma Society Terminology and Guidelines for Glaucoma, 4th Edition - Chapter 2: Classification and terminology supported by the EGS Foundation: Part 1: Foreword; Introduction; Glossary; Chapter 2 Classification and Terminology. Br J Ophthalmol 101: 73–127. https://doi.org/10.1136/bjophthalmol-2016-EGSguideline.002
Foster PJ, Buhrmann R, Quigley HA, Johnson GJ (2002) The definition and classification of glaucoma in prevalence surveys. Br J Ophthalmol 86:238–242. https://doi.org/10.1136/bjo.86.2.238
Birt CM, Shin DH, Samudrala V, Hughes BA, Kim C, Lee D (1997) Analysis of reliability indices from Humphrey visual field tests in an urban glaucoma population. Ophthalmology 104:1126–1130. https://doi.org/10.1016/s0161-6420(97)30173-0
Banes MJ, Culham LE, Bunce C, Xing W, Viswanathan A, Garway-Heath D (2006) Agreement between optometrists and ophthalmologists on clinical management decisions for patients with glaucoma. Br J Ophthalmol 90:579–585. https://doi.org/10.1136/bjo.2005.082388
AGIS (2000) The Advanced Glaucoma Intervention Study (AGIS): 7. The relationship between control of intraocular pressure and visual field deterioration. The AGIS Investigators Am J Ophthalmol 130:429–440. https://doi.org/10.1016/s0002-9394(00)00538-9
Zhang X, Dastiridou A, Francis BA, Tan O, Varma R, Greenfield DS, Schuman JS, Huang D, Advanced Imaging for Glaucoma Study G (2017) Comparison of glaucoma progression detection by optical coherence tomography and visual field. Am J Ophthalmol 184: 63-74. https://doi.org/10.1016/j.ajo.2017.09.020
McCarty CA, Nanjan MB, Taylor HR (2001) Vision impairment predicts 5 year mortality. Br J Ophthalmol 85:322–326. https://doi.org/10.1136/bjo.85.3.322
Zahari M, Mukesh BN, Rait JL, Taylor HR, McCarty CA (2006) Progression of visual field loss in open angle glaucoma in the Melbourne Visual Impairment Project. Clin Exp Ophthalmol 34:20–26. https://doi.org/10.1111/j.1442-9071.2006.01142.x
Stel VS, Dekker FW, Tripepi G, Zoccali C, Jager KJ (2011) Survival analysis I: the Kaplan-Meier method. Nephron Clin Pract 119:c83-88. https://doi.org/10.1159/000324758
Gardiner SK, Crabb DP (2002) Frequency of testing for detecting visual field progression. Br J Ophthalmol 86:560–564. https://doi.org/10.1136/bjo.86.5.560
Dong ZM, Wollstein G, Schuman JS (2016) Clinical utility of optical coherence tomography in glaucoma. Invest Ophthalmol Vis Sci 57: OCT556–567. https://doi.org/10.1167/iovs.16-19933
Feiner L, Piltz-Seymour JR, Treatment CIG, S, (2003) Collaborative Initial Glaucoma Treatment Study: a summary of results to date. Curr Opin Ophthalmol 14:106–111
Leske MC, Heijl A, Hyman L, Bengtsson B (1999) Early Manifest Glaucoma Trial: design and baseline data. Ophthalmology 106:2144–2153. https://doi.org/10.1016/s0161-6420(99)90497-9
Hattenhauer MG, Johnson DH, Ing HH, Herman DC, Hodge DO, Yawn BP, Butterfield LC, Gray DT (1998) The probability of blindness from open-angle glaucoma. Ophthalmology 105:2099–2104. https://doi.org/10.1016/S0161-6420(98)91133-2
Kwon YH, Kim CS, Zimmerman MB, Alward WL, Hayreh SS (2001) Rate of visual field loss and long-term visual outcome in primary open-angle glaucoma. Am J Ophthalmol 132:47–56. https://doi.org/10.1016/s0002-9394(01)00912-6
Pereira ML, Kim CS, Zimmerman MB, Alward WL, Hayreh SS, Kwon YH (2002) Rate and pattern of visual field decline in primary open-angle glaucoma. Ophthalmology 109:2232–2240. https://doi.org/10.1016/s0161-6420(02)01248-4
Musch DC, Gillespie BW, Lichter PR, Niziol LM, Janz NK, Investigators CS (2009) Visual field progression in the Collaborative Initial Glaucoma Treatment Study the impact of treatment and other baseline factors. Ophthalmology 116:200–207. https://doi.org/10.1016/j.ophtha.2008.08.051
Boland MV, Zhang L, Broman AT, Jampel HD, Quigley HA (2008) Comparison of optic nerve head topography and visual field in eyes with open-angle and angle-closure glaucoma. Ophthalmology 115(239–245):e232. https://doi.org/10.1016/j.ophtha.2007.03.086
Yousefi S, Sakai H, Murata H, Fujino Y, Garway-Heath D, Weinreb R, Asaoka R (2018) Asymmetric patterns of visual field defect in primary open-angle and primary angle-closure glaucoma. Invest Ophthalmol Vis Sci 59:1279–1287. https://doi.org/10.1167/iovs.17-22980
BallaeGaneshrao S, Senthil S, Choudhari N, Sri Durgam S, Garudadri CS (2019) Comparison of visual field progression rates among the high tension glaucoma, primary angle closure glaucoma, and normal tension glaucoma. Invest Ophthalmol Vis Sci 60:889–900. https://doi.org/10.1167/iovs.18-25421
Lee YH, Kim CS, Hong SP (2004) Rate of visual field progression in primary open-angle glaucoma and primary angle-closure glaucoma. Korean J Ophthalmol 18:106–115. https://doi.org/10.3341/kjo.2004.18.2.106
Aung T, Ang LP, Chan SP, Chew PT (2001) Acute primary angle-closure: long-term intraocular pressure outcome in Asian eyes. Am J Ophthalmol 131:7–12. https://doi.org/10.1016/s0002-9394(00)00621-8
Aung T, Friedman DS, Chew PT, Ang LP, Gazzard G, Lai YF, Yip L, Lai H, Quigley H, Seah SK (2004) Long-term outcomes in Asians after acute primary angle closure. Ophthalmology 111:1464–1469. https://doi.org/10.1016/j.ophtha.2003.12.061
Liza-Sharmini AT, Sharina YN, Dolaboladi AJ, Zaid NA, Azhany Y, Zunaina E (2014) Clinical presentation, severity and progression of primary angle closure in Malays. Med J Malaysia 69:21–26
Sharmini AT, Yin NY, Lee SS, Jackson AL, Stewart WC (2009) Mean target intraocular pressure and progression rates in chronic angle-closure glaucoma. J Ocul Pharmacol Ther 25:71–75. https://doi.org/10.1089/jop.2008.0061
Quek DTL, Koh VT, Tan GS, Perera SA, Wong TT, Aung T (2011) Blindness and long-term progression of visual field defects in Chinese patients with primary angle-closure glaucoma. Am J Ophthalmol 152:463–469. https://doi.org/10.1016/j.ajo.2011.02.023
Congdon N, Wang F, Tielsch JM (1992) Issues in the epidemiology and population-based screening of primary angle-closure glaucoma. Surv Ophthalmol 36:411–423. https://doi.org/10.1016/s0039-6257(05)80022-0
Anton A, Andrada MT, Mujica V, Calle MA, Portela J, Mayo A (2004) Prevalence of primary open-angle glaucoma in a Spanish population: the Segovia study. J Glaucoma 13:371–376. https://doi.org/10.1097/01.ijg.0000133385.74502.29
De Moraes CG, Liebmann JM, Levin LA (2017) Detection and measurement of clinically meaningful visual field progression in clinical trials for glaucoma. Prog Retin Eye Res 56:107–147. https://doi.org/10.1016/j.preteyeres.2016.10.001
De Moraes CG, Liebmann JM, Greenfield DS, Gardiner SK, Ritch R, Krupin T, Low-pressure Glaucoma Treatment Study G (2012) Risk factors for visual field progression in the low-pressure glaucoma treatment study. Am J Ophthalmol 154: 702-711. https://doi.org/10.1016/j.ajo.2012.04.015
Spry PG, Sparrow JM, Diamond JP, Harris HS (2005) Risk factors for progressive visual field loss in primary open angle glaucoma. Eye (Lond) 19:643–651. https://doi.org/10.1038/sj.eye.6701605
Drance S, Anderson DR, Schulzer M, Collaborative Normal-Tension Glaucoma Study G (2001) Risk factors for progression of visual field abnormalities in normal-tension glaucoma. Am J Ophthalmol 131: 699-708. https://doi.org/10.1016/s0002-9394(01)00964-3
Leske MC, Heijl A, Hussein M, Bengtsson B, Hyman L, Komaroff E (2003) Factors for glaucoma progression and the effect of treatment: the early manifest glaucoma trial. Arch Ophthalmol 121:48–56. https://doi.org/10.1001/archopht.121.1.48
Law SK, Choe R, Caprioli J (2001) Optic disk characteristics before the occurrence of disk hemorrhage in glaucoma patients. Am J Ophthalmol 132:411–413. https://doi.org/10.1016/s0002-9394(01)01009-1
Kim KE, Jeoung JW, Kim DM, Ahn SJ, Park KH, Kim SH (2015) Long-term follow-up in preperimetric open-angle glaucoma: progression rates and associated factors. Am J Ophthalmol 159(160–168):e161-162. https://doi.org/10.1016/j.ajo.2014.10.010
Kass MA, Heuer DK, Higginbotham EJ, Johnson CA, Keltner JL, Miller JP, Parrish RK, 2nd, Wilson MR, Gordon MO (2002) The ocular hypertension treatment study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol 120: 701–713; discussion 829–730. https://doi.org/10.1001/archopht.120.6.701
Quigley HA (2005) European glaucoma prevention study. Ophthalmology 112: 1642–1643; author reply 1643–1645. https://doi.org/10.1016/j.ophtha.2005.05.024
Seol BR, Jeoung JW, Park KH (2019) Ocular and systemic risk factors associated with recurrent disc hemorrhage in primary open-angle glaucoma. PLoS ONE 14:e0222166. https://doi.org/10.1371/journal.pone.0222166
Siam GA, de Barros DS, Gheith ME, Da Silva RS, Lankaranian D, Tittler EH, Myers JS, Spaeth GL (2007) The amount of intraocular pressure rise during pharmacological pupillary dilatation is an indicator of the likelihood of future progression of glaucoma. Br J Ophthalmol 91:1170–1172. https://doi.org/10.1136/bjo.2007.116855
Leibowitz HM (2000) The red eye. N Engl J Med 343:345–351. https://doi.org/10.1056/NEJM200008033430507
Walland MJ (2008) On the lookout: how to save the sight of Australians who have glaucoma. Med J Aust 188:269–270. https://doi.org/10.5694/j.1326-5377.2008.tb01616.x
Chew SS, Vasudevan S, Patel HY, Gurria LU, Kerr NM, Gamble G, Crowston JG, Danesh-Meyer HV (2011) Acute primary angle closure attack does not cause an increased cup-to-disc ratio. Ophthalmology 118:254–259. https://doi.org/10.1016/j.ophtha.2010.06.026
Gemenetzi M, Yang Y, Lotery AJ (2012) Current concepts on primary open-angle glaucoma genetics: a contribution to disease pathophysiology and future treatment. Eye (Lond) 26:355–369. https://doi.org/10.1038/eye.2011.309
Parikh RS, Parikh SR, Navin S, Arun E, Thomas R (2008) Practical approach to medical management of glaucoma. Indian J Ophthalmol 56:223–230. https://doi.org/10.4103/0301-4738.40362
Matlach J, Bender S, Konig J, Binder H, Pfeiffer N, Hoffmann EM (2019) Investigation of intraocular pressure fluctuation as a risk factor of glaucoma progression. Clin Ophthalmol 13:9–16. https://doi.org/10.2147/OPTH.S186526
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This study received ethical approval from the Research and Ethical Committee, School of Medical Sciences, Universiti Sains Malaysia (Reference code: USM/JePEM/16090340), and was conducted in accordance to Declaration of Helsinki for human research.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Patients signed informed consent regarding publishing their data.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Part of this study was presented as e-poster in the 34th Asia Pacific Academy of Ophthalmology Congress Bangkok Thailand 6–9 March 2019. the abstract is available in the program book page 144.
Progression of Primary Glaucoma in Malays: Survival Analysis Outcome.
Diana-Toh SJ, Wan Ezatul Arisha WM, Najib MY, Norsa’adah B, Liza-Sharmini AT.
Rights and permissions
About this article
Cite this article
Wan-Ezatul-Arisha, W.M., Diana-Toh, S.J., Huwaina, A.S. et al. Visual field progression in Malay patients with primary glaucoma: survival analysis and prognostic factors. Graefes Arch Clin Exp Ophthalmol 260, 2003–2012 (2022). https://doi.org/10.1007/s00417-021-05466-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-021-05466-9