Abstract
Purpose
Transforming growth factor beta 1 (TGF-β1) is an important cytokine released after ocular surface injury to promote wound healing. However, its persistence at the injury site triggers a fibrotic response that leads to corneal scarring and opacity. Thiazolidinediones (TZDs) are synthetic peroxisome proliferator-activated receptor gamma (PPAR-γ) ligands used to regulate glucose and lipid metabolism in the management of type 2 diabetes. Studies have also showed TZDs have antifibrotic effect. In this study, we investigated the antifibrotic effect of the TZD lobeglitazone on TGF-β1-induced fibrosis in corneal fibroblasts.
Methods
Human primary corneal fibroblasts were cultivated and treated with TGF-β1 (5 ng/mL) to induce fibrosis, with or without pre-treatments with different concentrations of lobeglitazone. Myofibroblast differentiation and extracellular matrix (ECM) protein expression was evaluated by western blotting, immunofluorescence, real-time PCR, and collagen gel contraction assay. The effect of lobeglitazone on TGF-β1-induced reactive oxygen species (ROS) generation was evaluated by DCFDA–cellular ROS detection assay kit. Signaling proteins were evaluated by western blotting to determine the mechanism underlying the antifibrotic effect.
Results
Our results showed lobeglitazone attenuated TGF-β1-induced ECM synthesis and myofibroblast differentiation of corneal fibroblasts. This antifibrotic effect appeared to be independent of PPAR signaling and rather due to the inhibition of the TGF-β1-induced Smad signaling. Lobeglitazone also blocked TGF-β1-induced ROS generation and nicotinamide adenine dinucleotide phosphate oxidase (Nox) 4 transcription.
Conclusion
These findings indicate that lobeglitazone may be a promising therapeutic agent for corneal scarring.
Key messages

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Corneal fibrosis results in corneal scarring and opacity and has rendered millions of people worldwide either visually impaired or completely blind. Corneal scarring remains a major concern in clinical ophthalmology, with post-surgical scarring posing an enormous challenge to clinicians [1]. It is caused by abnormal corneal wound healing characterized by the prevalence of myofibroblasts, which synthesize large amounts of aberrant extracellular matrix (ECM) proteins but small amounts of water-soluble corneal crystalline enzymes, culminating in corneal opacification [2,3,4].
The pleiotropic cytokine, transforming growth factor beta 1 (TGF-β1), plays a crucial role in corneal stromal wound healing by promoting the transdifferentiation of quiescent keratocytes into active myofibroblasts [5,6,7]. These myofibroblasts deposit and cross-link large amounts of aberrant ECM proteins at the site of injury to remodel the injured tissue. They also express alpha-smooth muscle actin (α-SMA) proteins, which exert contractile force on the ECM to facilitate wound closure [8,9,10]. The myofibroblasts undergo apoptosis after the resolution of the wound [11], and the ECM proteins are broken down by the repopulated keratocytes to restore corneal integrity [12]. However, persistent TGF-β1 secretion retains the myofibroblasts at the injury site, causing continuous and prolonged synthesis of the aberrant ECM proteins, ultimately resulting in the formation of fibrotic cornea tissues with distorted architecture and thus a non-functional cornea [8]. Therapeutic agents and methods aimed at modulating TGF-β1 synthesis, and its effects at the site of injury offer a promising strategy to prevent corneal scarring.
Thiazolidinediones (TZDs), also known as glitazones, are synthetic peroxisome proliferator-activated receptor gamma (PPAR-γ) ligands used to regulate glucose and lipid metabolism in the management of type 2 diabetes [13, 14]. Several findings indicate that these synthetic PPAR-γ ligands also have anti-inflammatory and antifibrotic effects in various organs and tissues through mechanisms that are dependent or independent of their receptors [15,16,17,18,19,20,21,22]. Some of these PPAR-γ independent antifibrotic effects have been observed to result from the suppression of TGF-β1 production or the inhibition of its downstream signaling pathways [16,17,18]. PPAR-γ gene over-expression has also been seen to promote wound healing after cornea alkali injury in mice [23], supporting the antifibrotic effect of PPAR-γ signal activation.
In this study, we investigated the effect of a fairly new synthetic TZD, lobeglitazone, on TGF-β1-induced corneal fibrosis. Lobeglitazone was approved by the Ministry of Food and Drug Safety (South Korea) in 2013, and is a dual activator of PPAR-α and PPAR-γ receptors. Lobeglitazone is structurally similar to rosiglitazone but has a pyrimidine moiety in place of the pyridine moiety in rosiglitazone and a p-methoxyphenol functional group at the 4-position of its pyrimidine moiety [24, 25]. These structural modifications cause lobeglitazone to have a higher affinity for PPAR-γ receptors, thus making it more potent, at a significantly lower dosage, for the management of type 2 diabetes with less side effects compared to rosiglitazone [24,25,26]. Findings from our laboratory and other research laboratories indicate that rosiglitazone, similar to other TZDs, suppresses TGF-β1-induced fibrogenesis [17, 27]. Since studies have shown that slight changes in receptor-ligand interactions can result in significant differences in the pharmacological actions of TZDs [13, 28], we sought to investigate the antifibrotic effects of lobeglitazone on corneal fibroblasts and the molecular mechanism underlying any such antifibrotic effects.
Materials and methods
Isolation and culture of primary human corneal fibroblasts
Primary human corneal fibroblasts were obtained from the corneal limbus or central button as described previously [29, 30]. Briefly, the stromal layer was isolated by Dispase II (Sigma-Aldrich) digestion of the epithelial and endothelial layers followed by scraping under a microscope. The stromal layer was then digested with 2 mg/mL collagenase and 0.5 mg/mL hyaluronidase (Sigma-Aldrich, St. Louis, MO, USA) at 37 °C over night. After digestion, the cells were collected through centrifugation at 1500×g for 5 min and cultured at 37 °C in a humidified atmosphere of 5% CO2 in Dulbecco’s modified Eagle’s medium (DMEM; Welgene, Gyeongsan, Korea) containing 10% fetal bovine serum and 1% antibiotics/antimycotics (streptomycin, penicillin, and amphotericin B; Gibco Life Technologies, Thermo Fisher Scientific, Waltham, MA, USA). Cells from passages 2–10 were stored at −80 °C for subsequent use.
Western blotting
For protein analysis, the cells were serum starved in DMEM culture media with 1% antibiotics/antimycotics for 24 h, after which they were pre-treated for 3–4 h with 5-μM and 10 μM lobeglitazone (Chong Keun Dang Pharmaceutical Corp., Seoul, Korea) in dimethyl sulfoxide (Sigma-Aldrich), followed by treatment with 5 ng/mL TGF-β1 (PeproTech, Seoul, Korea) to induce fibrosis. The cells were incubated for 48 h for ECM protein expression analysis and for 6 h for signaling protein expression analysis. To determine if the antifibrotic effect is PPAR-α- and/or PPAR-γ-dependent, the cells were pre-treated with 1 μM of the respective ligand’s synthetic inhibitor GW6741 and GW9662 for 3–4 h (Tocris Bioscience, Bristol, UK) before treatment with 10 μM lobeglitazone. For a negative control set, the pre-treated cells were not subjected to lobeglitazone treatment. A 5 μM Smad3 specific inhibitor SIS3-HCl (Selleckchem) pre-treatment was done to compare the effect of Smad signal inhibition and lobeglitazone treatment on the TGF-β1-induced fibrotic process. Total protein was extracted using radioimmunoprecipitation assay buffer (Thermo Fisher Scientific) mixed with protease and phosphatase inhibitors (Sigma-Aldrich). Protein quantification was performed using the Bradford assay reagent (Thermo Fisher Scientific). Equal amounts of proteins were resolved using 10% sodium dodecyl sulfate polyacrylamide gel electrophoresis and transferred onto polyvinylidene fluoride membranes (Millipore, Milan, Italy) and blocked with 5% skimmed milk solution. The membranes were incubated with primary antibody at 4 °C overnight, washed (3 × 5 min) with 1X TBST (Tris-buffered saline with 0.1% Tween® 20 detergent), incubated with horseradish peroxidase-conjugated secondary antibody for 2 h at room temperature followed by another washing with 1X TBST (3 × 5 min). The blots were detected using Pierce™ enhanced chemiluminescence western blotting substrate (Thermo Fisher Scientific). The images were captured using Image Lab™ Software version 6.0 (Bio-Rad Laboratories, Hercules, CA, USA). The relative expression levels of the target proteins were evaluated with densitometry using the ImageJ software Java 1.8.0_66 (64-bits) (http://imagej.nih.gov/ij/index.html). Antibody information is provided in Supplemental Table 1.
RNA isolation and real-time quantitative polymerase chain reaction (RT-qPCR)
For real-time quantitative analysis, the cells were seeded and treated with 5 μM or 10 μM lobeglitazone and 5 ng/mL TGF-β1, as described above. After incubation for 24 h, the cells were harvested. The total RNA was extracted using an RNA extraction kit (Qiagen, Hilden, Germany) according to the manufacturer’s protocol. The quality and quantity of the RNA extracts were assessed using a NanoDrop One spectrophotometer (Thermo Fisher Scientific). The RNA was reverse transcribed into cDNA using a LaboPassTM cDNA synthesis kit (Cosmo Genetech, Seoul, Korea) according to the manufacturer’s protocol. RT-qPCR was performed using the primer pairs of target genes in a 10 μL reaction mixture with SYBR green PCR mix (Applied Biosystems, Life Technologies, Foster City, CA, USA). The primer pair sequences used are listed in Supplemental Table 2.
Collagen gel matrix contraction assay
The cells were suspended in serum-free DMEM at a concentration of 1.5 × 105 cells/mL. Next, 400 μL of the cell suspension was mixed with 200 μL of type I collagen (Gibco Life Technologies) and neutralized with 5 μL of 1 M NaOH. Then, 600 μL of the cell and gel mixture was pipetted into each well of a 24-well plate and incubated at 37 °C for 30 min to polymerize. A 200 μL pipette tip was gently run along the edges of the gels to dissociate them from the wells. Cells belonging to four treatment regimens—vehicle-treated control cells, 5 ng/mL TGF-β1-treated cells, 5 ng/mL TGF-β1 plus 10 μM lobeglitazone-treated cells, and 5 ng/mL TGF-β1 plus 10 μM lobeglitazone plus 1 μM PPAR-γ synthetic inhibitor GW9662-treated cells in DMEM—were cultured at 37 °C and 5% CO2. Each treatment regimen was performed in triplicate. The gel images were recorded at 0 h, 24 h, 48 h, and 72 h using a digital camera (Sony Cyber-Shot DSC-RX100 V 20.1) at a fixed distance above the gels. The degree of contraction of the gel surface area was measured and quantified using the ImageJ software.
Immunoflourescence
Fibroblasts of passage 2 were cultured on glass chamber slides and pre-treated with 10 μM lobeglitazonein serum-free media for 3–4 h, followed by 5 ng/mL TGF-β1 treatment. After incubation for 72 h, the cells were fixed with 4% paraformaldehyde (PFA), followed by cell permeation with 0.3 % Triton X-100 in PBS (PBS-T), protein blocking with 5% BSA, and overnight incubation with antibodies to a-SMA and fibronectin at 4 °C. After washing, the cells were incubated with Alexa Fluor-conjugated secondary antibodies (Thermo Fisher Scientific, Rockford, IL, USA) for 2 h at room temperature in the dark. The nuclei were counterstained with 4′,6-diamidino-2-phenylindole (DAPI) in mounting media, and the immunofluorescence images were captured using a fluorescence microscope (Olympus BX51 Fluorescence Microscope; Tokyo, Japan). PBS and secondary antibodies without the primary antibody treatments were used as internal control. Fluorescence quantification analyses were done using ImageJ software. All treatments were done in triplicates.
Cell viability test
Cell viability was determined by the Cell Counting Kit-8 (CCK-8 ; Dojindo Laboratories, Kumamoto, Japan) assay and also by counting the number of viable cells using a hemocytometer.
For the CCK-8 assay, the cells were seeded into a 96-well plate at a density of 5000 cells/well and incubated for 24 h in DMEM. The cells were then treated with lobeglitazone at different concentrations (0 μM, 5 μM, 10 μM, 20 μM, and 40 μM) for the first set, and with 5 ng/mL TGF-β1, 5 ng/mL TGF-β1 plus 10 μM lobeglitazone, and vehicle-treated control for the second set, and incubated for 48 h. The assay kit was used to determine cell viability according to the manufacturer’s protocol. The optical absorbance was read at 450 nm on a microplate reader (Beckman Coulter DTX 880 Multimode Detector) after incubation for 2 h. The experiment were performed in triplicate for each treatment set.
For the viable cell counting using a hemecytometer, the cells were treated and incubated as indicated above in a 60 mm culture plate. After the 48 h incubation, the adhered cells were detached with trypsin/EDTA, centrifuged, and resuspended in phosphate-buffered saline (PBS; Welgene, Gyeongsan, Korea). Equal volumes of trypan blue and the cell suspension were mixed and 10 μM of the mixture was filled into the hemocytometer chamber. The viable cells (unstained) and non-viable cells (stained blue) were countered under an EVOSTM XL core microscope (Thermo Fisher Scientific, Bothell, WA, USA). The percentages of viable cells were then calculated for each treatment regimen. The experiment was performed in triplicate for each treatment set.
Reactive oxygen species (ROS) assay
The effect of lobeglitazone on TGF-β1-induced ROS generation was determined using the DCFDA–cellular ROS detection assay kit. The cells were seeded into a dark, clear bottom 96-well microplate and allowed to adhere overnight. They were then treated with 5 ng/mL TGF-β1, with or without 10 μM lobeglitazone pre-teatment, and incubated for 3 h, 6 h, and 12 h. The cells were then washed with 1X buffer. Approximately 100 μL/well of diluted DCFDA solution was added to the cells and incubated at 37 °C in the dark for 45 min. After incubation, the DCFDA solution was removed, and 100 μL/well of 1X buffer was added to the cells. The fluorescence was immediately measured using the DTX-800 multimode microplate reader at an excitation wavelength of 485 nm and an emission wavelength of 535 nm.Vehicle-treated cells were used as controls. All treatments were done in triplicates.
Statistical analysis
The data were analyzed using GraphPad Prism 5.0 software (GraphPad Software, San Diego, CA, USA). Statistical comparisons were performed using a Student’s t test and one-way analysis of variance and Tukey’s multiple comparisons test. Significance was defined as P value < 0.05 in all cases.
Results
Lobeglitazone suppresses TGF-β1-induced transdifferentiation of cornea fibroblasts
The antifibrotic effect of lobeglitazone in cornea fibroblasts was assessed by investigating its effect on TGF-β1-induced myofibroblast transdifferentiation and ECM protein synthesis. The cells were pre-treated for 3–4 h with 5 μM and 10 μM lobeglitazone and then with 5 ng/mL TGF-β1 and incubated for 48 h. The protein blotting results showed that 10 μM lobeglitazone effectively inhibited the synthesis of the myofibroblast differentiation marker α-SMA (P value < 0.001) and the ECM protein fibronectin (P value < 0.001) (Fig. 1A). Real-time PCR results also showed a significant inhibition of the transcription of α-SMA (P value < 0.001), fibronectin (P value < 0.001), and other ECM mRNAs collagen 1 (P value < 0.001) and extra domain A (EDA)-fibronectin (P value < 0.001) (Fig. 1B).
Effect of lobeglitazone on TGF-β1-induced myofibroblast differentiation. A Representative western blot and quantitative analysis showing the antifibrotic effect of lobeglitazone on TGF-β1-induced expression of α-SMA and fibronectin; (B) Quantitative analysis of real-time PCR results showing the antifibrotic effect of lobeglitazone on TGF-β1-induced transcription of α-SMA, fibronectin, collagen 1, and EDA-fibronectin mRNA (###P value <0.001 compared to vehicle-treated control cells; ***P value <0.001 and **P value <0.01, compared to TGF-β1 only treated cells)
A comparison of the antifibrotic effect of lobeglitazone and the structurally similar TZD rosiglitazone indicated a lower effective antifibrotic dose for lobeglitazone than for rosiglitazone. As shown in (Fig. 2), 10 μM lobeglitazone-treated cells showed a much stronger inhibition of the synthesis of α-SMA (P value < 0.001) and fibronectin (P value = 0.004) compared to the cells treated with only TGF-β1, whereas the 10 μM rosiglitazone-treated cells showed no significant inhibition of α-SMA and fibronectin protein synthesis compared to the cells treated with only TGF-β1.
Comparison of the effective antifibrotic dose of lobeglitazone and rosiglitazone. Representative western blot images and quantitative analysis comparing the effective antifibrotic dose of 10 μM lobeglitazone on TGF-β1-induced expression of α-SMA and fibronectin to that of 10 μM rosiglitazone showed no significant antifibrotic effects with the rosiglitazone treatment (###P value <0.001, compared to vehicle-treated control cells; ***P value <0.001, compared to TGF-β1 only treated cells)
To ascertain that the reduced protein synthesis did not result from decreased cell viability, we evaluated the cytotoxic effect of lobeglitazone at its effective antifibrotic dose. Using both the CCK-8 assay and the hemocytometer to count viable cells, our results showed no cytotoxicity effect of lobeglitazone at the effective antifibrotic dose of 10 μM, as there was no significant difference in viability between the vehicle-treated controls and 10 μM lobeglitazone-treated cells (Fig. 3). Cell viability was however seen to reduce significantly 24 h after treatment with 40 μM lobeglitazone.
Effect of lobeglitazone treatment on cell viability. A Analysis of the effect of lobeglitazone on cell viability, showing no loss of cell viability at the effective antifibrotic dose of 10 μM after 48 h of treatment. B Dose kinetics of lobeglitazone treatment shows significant decrease in cell viability 24 h after 40 μM (#P value <0.05 and ##P value <0.01 compared to vehicle-treated control cells)
Antifibrotic effect of lobeglitazone is independent of PPAR signaling
We then evaluated the role of PPAR signaling in the antifibrotic effect of lobeglitazone on the cornea fibroblasts. First, we ascertained the activation of PPAR signaling by lobeglitazone and the inhibition of the signaling pathway by the PPAR-γ synthetic inhibitor GW9662 by assessing the transcription of perilipin 2 (Plin2), which is a lipid droplet-associated protein expressed widely in the body and known to be transcriptionally activated by PPAR signaling [31]. Our real-time PCR results showed that both concentrations of lobeglitazone significantly stimulated PPAR signaling compared with the 5 ng/mL TGF-β1-only treatment, indicated as an increase in Plin2 mRNA transcription (P value = 0.002 for 5 μM; P value < 0.001 for 10 μM). Thus, Plin2 served as a positive control to confirm lobeglitazone-induced receptor activation. The PPAR inhibitor treatment significantly inhibited PPAR signaling in the cells (P value < 0.001; Fig. 4A), resulting in decreased Plin2 mRNA transcription. After this confirmatory experiment, the cells were pre-treated with 1 μM each of the PPAR-α synthetic inhibitor GW6741 and the PPAR-γ synthetic inhibitor GW9662 for 3–4 h with or without 10 μM lobeglitazone treatment and then with 5 ng/mL TGF-β1; these cells were then incubated for 48 h. Our results showed that the observed antifibrotic effect was independent of both PPAR-α and -γ signaling as treatment with the ligand alongside the inhibitors did not attenuate the observed antifibrotic effect (Fig. 4B).
Role of PPAR signaling in the antifibrotic action of lobeglitazone. A Quantitative analysis of Plin2 mRNA transcription after treatment with PPAR agonist lobeglitazone and PPAR antagonist GW9662, showing signal activation and inhibition respectively. B Representative western blot and quantitative analysis indicating that 10 μM lobeglitazone treatment inhibited the TGF-β1-induced α-SMA and fibronectin expression with or without 1 μM PPAR-α inhibitor GW6741 or 1 μM PPAR-γ inhibitor GW9662 co-treatment. C Representative immunofluorescent images and their quantitative analysis demonstrating that 10 μM lobeglitazone inhibited the TGF-β1-induced α-SMA (green) and fibronectin (red) expression with or without inhibitor GW9662 co-treatment. The nuclei were counterstained with DABI (blue). D Representative collagen gel images and the quantitative analysis showing significant inhibition of the TGF-β1-induced gel contraction by 10 μM lobeglitazone with or without inhibitor co-treatment (###P value <0.001, ##P value <0.01, and #P value <0.05, compared to vehicle-treated control cells; ***P value <0.001 and **P value <0.01, compared to TGF-β1 only treated cells)
Immunofluorescence, as well as gel contraction experiments, both confirmed the antifibrotic effect of lobeglitazone and its independence of PPAR signaling in corneal fibroblasts. The immunofluorescence results showed an approximately threefold increase in the expression of cytosolic α-SMA and fibronectin in the cells treated with 5 ng/mL TGF-β1 for 72 h compared with the vehicle-treated controls. Treatment with 10 μM lobeglitazone alone significantly inhibited the TGF-β1-induced synthesis of these proteins, whereas co-treatment of 10 μM lobeglitazone with 1 μM GW9662 did not reverse this antifibrotic effect (Fig. 4C). The morphological shift of the fibroblasts treated with only 5 ng/mL TGF-β1from the dendritic shape/morphology of the vehicle-treated control set to larger, flattened, and spread-out morphology indicates myofibroblast differentiation of the fibroblasts. The 10 μM lobeglitazone with 5 ng/mL TGF-β1-treated set and 5 ng/mL TGF-β1 plus 10 μM lobeglitazone with 1 μM GW9662 co-treatment set also retained the dendritic morphology of the fibroblasts, confirming the inhibition of myofibroblast differentiation. The collagen gel matrix contraction experiments also showed significant collagen contraction, which is a characteristic of activated fibroblasts (myofibroblast), with 5 ng/mL TGF-β1 treatment by the third day compared to that with vehicle treatment. The 10 μM lobeglitazone with 5 ng/mL TGF-β1-treated set and the 5 ng/mL TGF-β1 plus 10 μM lobeglitazone with 1 μM GW9662 co-treatment set did not show significant gel contractions compared with the vehicle-treated control set, thus indicating inhibition of TGF-β1-induced myofibroblast differentiation by lobeglitazone (Fig. 4D).
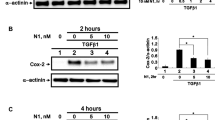
Antifibrotic effect of lobeglitazone occurs via Smad signaling
To determine the mechanisms by which lobeglitazone mediates its antifibrotic effect, we investigated the canonical Smad signaling pathway as well as the non-canonical mitogen-activated protein kinase (MAPK) pathways downstream of TGF-β1 signaling. The cells were serum starved for 24 h and pre-treated with 5 μM and 10 μM lobeglitazone for 3–4 h, followed by 5 ng/mL TGF-β1 treatment. The cells were then incubated for 6 h, after which the protein was extracted for western blotting to analyze the expression of signaling proteins. The results showed an almost complete shutdown of Smad signaling after 24 h of serum starvation compared to reduced but persistent MAPK signaling (Fig. 5A). TGF-β1 treatment significantly increased the canonical Smad signaling compared to the vehicle, whereas lobeglitazone treatment reduced the TGF-β1-induced Smad signaling significantly (P value < 0.001). Nonetheless, lobeglitazone treatment had no significant effects on MAPK signaling. To confirm the role of Smad signaling in TGF-β1-induced fibrogenesis in cornea fibroblasts and to compare the effect of blocking that signaling pathway with the results obtained from lobeglitazone treatment, we treated the cells with 5 μM of the specific Smad3 inhibitor SIS3-HCl and compared the expression levels of α-SMA and fibronectin proteins with their expression in cells treated with 10 μM lobeglitazone. As shown in our results, 5 μM of the SIS3-HCl treatment significantly blocked the expression of α-SMA (P value < 0.001) and fibronectin proteins (P value < 0.001), as seen with lobeglitazone treatment, thus confirming the role of Smad signaling in TGF-β1-induced fibrogenesis in corneal fibroblasts (Fig. 5B).
Effect of lobeglitazone on Smad and MAPK signaling pathways downstream of TGF-β1 signaling. A Representative western blot images and quantitative analyses of MAPK and Smad signaling pathways downstream of TGF-β1 signaling, demonstrating an inhibition of Smad signaling by lobeglitazone while having no such effect on MAPK signaling. B Treatment with 5 μM of the Smad3 inhibitor SIS3 showed decreased expression levels of α-SMA and fibronectin proteins, similar to that seen with 10 μM lobeglitazone treatment (###P value <0.001, ##P value <0.01, and #P value <0.05, compared to vehicle-treated control cells; ***P value <0.001, compared to only TGF-β1-treated cells)
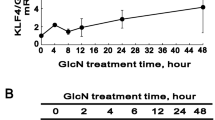
Lobeglitazone suppresses TGF-β1-induced nicotinamide adenine dinucleotide phosphate oxidase 4 transcription and ROS production
The profibrotic responses mediated by TGF-β1-induced Smad signaling have been linked to nicotinamide adenine dinucleotide phosphate oxidase (Nox) 4-dependent redox signaling [32]. Therefore, we also evaluated the effect of lobeglitazone on Nox4 mRNA transcription via real-time PCR and then on the subsequent generation of ROS by DCFDA–cellular ROS detection assay. Our results showed a significant increase in Nox4 mRNA transcription with 5 ng/mL TGF-β1 treatment compared with the vehicle treated control group (P value < 0.001). However, lobeglitazone treatment significantly inhibited the TGF-β1-induced mRNA transcription (P value < 0.001), further confirming the role of Smad signaling in the antifibrotic effect of lobeglitazone (Fig. 6A). As expected, the ROS assay also showed significant increase in ROS generation with TGF-β1 treatment, detected at 3 h and 6 h of incubation; this increase was effectively blocked by 10 μM lobeglitazone treatment at both time points (Fig. 6B). The ROS level was observed to peak at 6 h of incubation time but reduced at 12 h of incubation time, demonstrating its role in the early stages of the fibrotic response. Confirmatory experiments with 5 μM SIS3-HCl treatment also showed a reduction in Nox4 mRNA transcription similar to that observed with 10 μM lobeglitazone treatment (Fig. 6C).
Effect of lobeglitazone on TGF-β1-induced Nox 4 transcription and ROS production. A Quantitative analysis of Nox4 mRNA transcription, indicating that lobeglitazone treatment modulated TGF-β1-induced transcription. B Quantitative analysis of ROS generation after 5 ng/mL TGF-β1 treatment shows a significant increase at 3 h of incubation, peaked at 6 h, and then reduced at 12 h. Treatment with 10 μM lobeglitazone significantly blocked TGF-β1-induced ROS generation. C Quantitative analysis of Nox4 mRNA transcription with 5 μM SIS3-HCl (Smad3 inhibitor) treatment showed decreased transcription as seen with 10 μM lobeglitazone treatment (###P value <0.001, ##P value <0.01, and #P value <0.05, compared to vehicle-treated control cells; ***P value <0.001, **P value <0.01, and *P value <0.05, compared to TGF-β1 only treated cells)
Discussion
PPAR-γ is a transcription factor that has long been known to play a critical role in lipid metabolism and glucose homeostasis. After ligand binding, it heterodimerizes with the retinoid X receptor and translocates to the nucleus, where it binds to specific regions on the DNA of target genes called PPAR-γ response elements to regulate the transcription of multiple genes involved in adipocyte differentiation, lipid metabolism, and glucose homeostasis [33, 34]. Studies have also identified PPAR-γ activation as an important antifibrotic mechanism in cells, indicating a link between metabolism and fibrogenesis [35]. In this regard, both the synthetic and natural ligands of PPAR-γ have been shown to be effective in attenuating the TGF-β1-induced fibrosis in various organs and tissues through mechanisms that seem to be cell specific [14,15,16,17,18,19,20,21,22, 27]. In this study, we investigated the antifibrotic effect of lobeglitazone, the synthetic dual PPAR-α, and PPAR-γ ligand, on TGF-β1-induced fibrosis in corneal fibroblasts. Our results showed that lobeglitazone is an effective antifibrotic agent in corneal fibroblasts at a low dose of 10 μM (Figs. 1 and 3). It attenuated the TGF-β1-induced myofibroblast differentiation of corneal fibroblasts and the resulting synthesis of aberrant ECM proteins, thus supporting the reported antifibrotic effect of TZDs in several tissues and organs.
A comparison of its antifibrotic effect with that of rosiglitazone, a structurally similar PPAR-γ ligand, at the same concentration of 10 μM, showed a remarkable difference in the antifibrotic effect of these two TZDs. Lobeglitazone showed a significant inhibition of myofibroblast differentiation and ECM protein synthesis compared to rosiglitazone, which did not show any significant antifibrotic effect at this concentration (Fig. 2). Huxlin et al. (2013) [36] reported 25 μM to be the least effective antifibrotic dose of rosiglitazone in cornea fibroblasts. Lobeglitazone contains a pyrimidine moiety in the place of the pyridine moiety of rosiglitazone, with a p-methoxyphenol functional group at the 4-position of its pyrimidine moiety [24, 25]. Structural modifications resulting in more potent antifibrotic effects have also been reported for electrophilic TZDs compared to those for non-electrophilic TZDs in corneal fibroblasts [37] and human lung fibroblasts [38, 39], and was attributed to the possible modification of cellular proteins by their electrophilic centers. Thus, our results, in conjunction with those of other studies, confirm the effect of the structure of TZDs on their antifibrotic effects.
Next, we investigated the possible molecular mechanisms underlying the observed antifibrotic effects of lobeglitazone. PPAR-γ ligands have been shown to modulate multiple cellular functions via both PPAR-γ-dependent and PPAR-γ-independent mechanisms. We first determined if the antifibrotic effects of lobeglitazone were dependent on its PPAR-α and PPAR-γ signaling pathways. Our results showed that the antifibrotic effect was independent of both its PPAR-α and PPAR-γ receptors, as treatment with the PPAR-γ receptor antagonist GW9662 and PPAR-α receptor antagonist GW6741 did not reverse the observed antifibrotic effects (Fig. 4). This finding is consistent with the previous findings for other TZDs in corneal fibroblasts [17, 27, 36] as well as other tissues and organs [16, 19]. Ferguson et al. (2009) [38] hypothesized that the PPAR-γ-independent antifibrotic effect is much stronger than the PPAR-γ-dependent effect. Thus, compounds that exert their antifibrotic effects independent of PPAR-γ signaling inhibit TGF-β-induced myofibroblast differentiation more potently at lower doses, and are more likely to have greater therapeutic potential as antifibrotic agents than those having PPAR-γ-dependent effects.
We then investigated the signaling pathways downstream of TGF-β1 signaling. TGF-β1transduces signals through the canonical Smad signaling pathway as well as through non-canonical/non-Smad signaling pathways, such as the MAPK signaling pathways. Our results showed that lobeglitazone modulated the canonical Smad signaling pathway to elicit its antifibrotic response in corneal fibroblasts, whereas no such effect was observed with MAPK signaling (Fig. 5). TGF-β1 activates TGF-β receptor I kinase, causing the phosphorylation of the receptor-regulated Smad (R-Smad) proteins Smad2 and Smad3. These activated R-Smad proteins then complex with a common mediator Smad4 and translocate to the nucleus to regulate the transcription of target genes [40]. A study in unilateral ureteral obstruction-induced renal fibrosis in mice also indicated that the antifibrotic effect of lobeglitazone occurred via TGF-β1/Smad signal modulation [41], thus supporting our findings.
The profibrotic responses mediated by TGF-β1-induced Smad signaling have been linked to Nox-dependent redox signaling through different mechanisms [32]. In particular, Nox4, which is constitutively expressed in many cell types including fibroblasts, has been found to be the most important downstream effector mediating this TGF-β1-induced fibrosis [32, 42,43,44]. Its role in TGF-β1-induced fibrotic response in ocular wound healing has also been established [45,46,47]. The resultant ROS generated in turn activates latent TGF-β1 and induces TGF-β1 gene expression, leading to an increase in TGF-β1 activity [32]. ROS is also known to mediate many of the profibrogenic effects of TGF-β1, such as the promotion of myofibroblast differentiation and epithelial–mesenchymal transition, and the suppression of ECM degradation [32, 42]. We therefore evaluated the effect of lobeglitazone on Nox4 expression. Our results showed a marked inhibition of Nox4 transcription with lobeglitazone treatment, confirming the role of lobeglitazone in inhibiting Smad signaling as well as the pivotal role of Nox4 in the profibrotic responses mediated by TGF-β1/Smad signaling. As expected, TGF-β1-induced ROS generation also decreased significantly with lobeglitazone treatment. Smad inhibitor treatment validated our results by showing decreased Nox4 transcription (Fig. 6). The mechanism underlying lobeglitazone’s inhibition of Smad phosphorylation however remains unclear. As reviewed by Gong and Yang [48], studies have shown that the TGF-β1/Smad-induced fibrotic responses are downregulated by ROS scavenging. In line with this, it has also been reported that antioxidants—reduced glutathione, N-acetyl cysteine, and L-cysteine—are capable of blocking TGF-β-stimulated Smad2 phosphorylation [49]. The TZD troglitazone, with structural similarities to α-tocopherol—a known antioxidant—showed ROS scavenging abilities in an in vivo studies. However, in the same study, another TZD pioglitazone with structural similarities to both lobeglitazone and rosiglitazone did not exhibit any such ROS scavenging effect [50]. This again showing the different mechanisms of action of these TZDs as being directly related to their structures, and thus also suggesting that lobeglitazone may not have an ROS scavenging effect. A study in non-alcoholic fatty liver disease (NAFLD) showed that lobeglitazone ameliorated oxidative stress-mediated liver injury by inhibiting ROS generation [51] supporting our findings. Further studies are thus needed to elucidate the exact mechanism of Smad signal inhibition.
Lobeglitazone has a more favorable safety profile in humans than other TZDs in the management of diabetes. Research findings indicate that the structural modifications in lobeglitazone aid in exerting a more potent antidiabetic effect at a significantly lower dosage due to its stronger binding affinity for the PPAR-γ receptor than other TZDs [24, 25, 52]. This low effective dose of lobeglitazone results in a significant decrease in the adverse effects caused by chemical toxicity and off-target effects associated with high drug dose [27, 53,54,55]. Notably, our results showed a potent low effective antifibrotic dose compared with rosiglitazone. Since its antifibrotic effect is independent of PPAR-γ receptor signaling, we hypothesize this potent low effective antifibrotic dose may be due to its modulation of TGF-β1/Smad signaling—the canonical pathway of the profibrotic effects of TGF-β1 [40, 56]. Furthermore, our lab and others have shown that rosiglitazone elicits its antifibrotic response in corneal fibroblasts by inhibiting the TGF-β1-induced non-canonical p38 MAPK signaling pathway [17, 27], thus highlighting the different mechanisms of action of these two TZDs.
In summary, our results demonstrated that lobeglitazone exerts extremely potent antifibrotic effects in corneal fibroblasts through the inhibition of TGF-β1/Smad signaling. Thus, lobeglitazone appears to be a promising therapeutic agent for corneal scarring.
Data availability
Yes
Code availability
Not applicable
References
Wilson SE (2019) Coordinated modulation of corneal Scarring by the epithelial basement membrane and Descemet’s basement membrane. J Refract Surg 35(8):506–516
Fini ME (1999) Keratocyte and fibroblast phenotypes in the repairing cornea. Prog. Retin. Eye Res 18:529–551
Friedlander M (2007) Fibrosis and diseases of the eye. J Clin Invest 117:576–586
Torricelli AA, Santhanam A, Wu J, Singh V, Wilson SE (2016) The corneal fibrosis response to epithelial-stromal injury. Exp. Eye Res 142:110–118
Saika S (2006) TGF-β pathobiology in the eye. Lab Investig 86:106–115
Tandon A, Tovey JC, Sharma A, Gupta R, Mohan RR (2010) Role of transforming growth factor Beta in corneal function, biology and pathology. Curr Mol Med 10:565–578
Wilson SE (2020) Corneal myofibroblasts and fibrosis. Exp Eye Res 201:108272
Louise M, Carrington JA, Anderson I, Kamma C, Boulton M (2006) Differential regulation of key stages in early corneal wound healing by TGF-β isoforms and their inhibitors. Invest Ophthalmol Vis Sci 47:1886–1894
Shu DY, Lovicu FJ (2017) Myofibroblast transdifferentiation: the dark force in ocular wound healing and fibrosis. Prog Retin Eye Res 60:44–65
Wilson SE (2012) Corneal myofibroblast biology and pathobiology: generation, persistence, and transparency. Exp Eye Res 99:78–88
Kaur H, Chaurasia SS, Agrawal V, Suto C, Wilson SE (2009) Corneal myofibroblast viability: opposing effects of IL-1 and TGF beta1. Exp Eye Res 89:152–158
Torricelli AA, Singh V, Santhiago MR, Wilson SE (2013) The corneal epithelial basement membrane: structure, function, and disease. Invest Ophthalmol Vis Sci 54:6390–6400
Choi JH, Banks AS, Estall JL, Kajimura S, Boström P, Laznik D, Ruas JL, Chalmers MJ, Kamenecka TM, Blüher M, Griffin PR, Spiegelman BM (2010) Anti-diabetic drugs inhibit obesity-linked phosphorylation of PPAR-γ 3 by Cdk5. Nature. 466:451–456
Thangavel N, Al Bratty M, Javed SA, Ahsan W, Alhazmi HA (2017) Targeting peroxisome proliferator-activated receptors using thiazolidinediones: strategy for design of novel antidiabetic drugs. Int J Med Chem 2017:1069718
Burgess HA, Daugherty LE, Thatcher TH, Lakatos HF, Ray DM, Redonnet M, Phipps RP, Sime PJ (2005) PPAR gamma agonists inhibit TGF-beta induced pulmonary myofibroblast differentiation and collagen production: implications for therapy of lung fibrosis. Am J Phys Lung Cell Mol Phys 288:L1146–L1153
Ghosh AK, Bhattacharyya S, Lakos G, Chen SJ, Mori Y, Varga J (2004) Disruption of transforming growth factor beta signaling and profibrotic responses in normal skin fibroblasts by peroxisome proliferator-activated receptor gamma. Arthritis Rheum 50:1305–1318
Jeon K-I, Kulkarni A, Woeller CF, Phipps RP, Sime PJ, Hindman HB, Huxlin KR (2014) Inhibitory effects of PPARγ ligands on TGF-β1-induced corneal myofibroblast transformation. Am J Pathol 184:1429–1445
Kawai T, Masaki T, Doi S, Arakawa T, Yokoyama Y, Doi T, Kohno N, Yorioka N (2009) PPAR-gamma agonist attenuates renal interstitial fibrosis and inflammation through reduction of TGF-beta. Lab Investig 89:47–58
Liu Y, Dai B, Xu C, Fu L, Hua Z, Mei C (2011) Rosiglitazone inhibits transforming growth factor-beta 1 mediated fibrogenesis in ADPKD cyst-lining epithelial cells. PLoS One 6:e28915
Milam JE, Keshamouni VG, Phan SH, Hu B, Gangireddy SR, Hogaboam CM, Standiford TJ, Thannickal VJ, Reddy RC (2008) PPAR-γ agonists inhibit profibrotic phenotypes in human lung fibroblasts and bleomycin-induced pulmonary fibrosis. Am J Phys Lung Cell Mol Phys 294:L891–L901
Zheng F, Fornoni A, Elliot SJ, Guan Y, Breyer MD, Striker LJ, Striker GE (2002) Upregulation of type I collagen by TGF-beta in mesangial cells is blocked by PPAR gamma activation. Am. J. Physiol. Renal Physiol 282:F639–F648
Shi-wen X, Eastwood M, Stratton RJ, Denton CP, Leask A, Abraham DJ (2010) Rosiglitazone alleviates the persistent fibrotic phenotype of lesional skin scleroderma fibroblasts. Rheumatology 49:259–263
Saika S, Yamanaka O, Okada Y, Miyamoto T, Kitano A, Flanders KC, Ohnishi Y, Nakajima Y, Kao WWY, Ikeda K (2007) Effect of overexpression of PPAR gamma on the healing process of corneal alkali burn in mice. Am J Phys Cell Phys 293(1):C75–C86
Jang JY, Bae H, Lee YJ, Choi YI, Kim H-J, Park SB, Suh SW, Kim SW, Han BW (2018) Structural basis for the enhanced anti-diabetic efficacy of lobeglitazone on PPAR-γ. Sci Rep 8:31
Kroker AJ, Bruning JB (2015) Review of the structural and dynamic mechanisms of PPAR-γ partial agonism. PPAR Res 2015:816856
Lee MA, Tan L, Yang H, Im Y-G, Im YJ (2017) Structures of PPARγ complexed with lobeglitazone and pioglitazone reveal key determinants for the recognition of antidiabetic drugs. Sci Rep 7:16837
Nuwormegbe SA, Sohn JH, Kim SW (2017) A PPAR-gamma agonist rosiglitazone suppresses fibrotic response in human pterygium fibroblasts by modulating the p38 MAPK pathway. Invest Ophthalmol Vis Sci 58:5217–5226
Bruning JB, Chalmers MJ, Prasad S, Busby SA, Kamenecka TM, He Y, Nettles KW, Griffin PR (2007) Partial agonists activate PPARγ using a helix 12 independent mechanism. Structure 15:1258–1271
Jester JV, Huang J, Fisher S, Spiekerman J, Chang JH, Wright WE, Shay JW (2003) Myofibroblast differentiation of normal human keratocytes and hTERT, extended-life human corneal fibroblasts. Invest Ophthalmol Vis Sci 44:1850–1858
Nuwormegbe SA, Kim SW (2020) AMPK activation by 5-amino-4-imidazole carboxamide riboside-1-β-D-ribofuranoside attenuates alkali injury-induced corneal fibrosis. Invest Ophthalmol Vis Sci 61:43
Bickel PE, Tansey JT, Welte MA (2009) PAT proteins, an ancient family of lipid droplet proteins that regulate cellular lipid stores. Biochim Biophys Acta 1791:419–440
Liu RM, Desai LP (2015) Reciprocal regulation of TGF-β and reactive oxygen species: a perverse cycle for fibrosis. Redox Biol 6:565–577
Ahmadian M, Suh JM, Hah N, Liddle C, Atkins AR, Downes M, Evans RM (2013) PPARγ signaling and metabolism: the good, the bad and the future. Nat Med 19:557–566
Mangelsdorf DJ, Thummel C, Beato M, Herrlich P, Schütz G, Umesono K, Blumberg B, Kastner P, Mark M, Chambon P, Evans RM (1995) The nuclear receptor superfamily: the second decade. Cell 83:835–839
Wei J, Bhattacharyya S, Jain M, Varga J (2012) Regulation of matrix remodeling by peroxisome proliferator-activated receptor-gamma: a novel link between metabolism and fibrogenesis. Open Rheumatol J 6:103–115
Huxlin KR, Hindman HB, Jeon K-I, Bühren J, MacRae S, DeMagistris M, Ciufo D, Sime PJ, Phipps RP (2013) Topical rosiglitazone is an effective anti-scarring agent in the cornea. PLoS One 8:e70785
Kuriyan AE, Lehmann GM, Kulkarni AA, Woeller CF, Feldon SE, Hindman HB, Sime PJ, Huxlind KR, Phipps RP (2012) Electrophilic PPAR gamma ligands inhibit corneal fibroblast to myofibroblast differentiation in vitro: a potentially novel therapy for corneal scarring. Exp. Eye Res 94:136–145
Ferguson HE, Kulkarni A, Lehmann GM, Garcia-Bates TM, Thatcher TH, Huxlin KR, Phipps RP, Sime PJ (2009) Electrophilic peroxisome proliferator-activated receptor-gamma ligands have potent antifibrotic effects in human lung fibroblasts. Am J Respir Cell Mol Biol 41:722–730
Hogan CM, Thatcher TH, Sapinoro RE, Gurell MN, Ferguson HE, Pollock SJ, Jones C, Phipps RP, Sime PJ, Drew P (2011) Electrophilic PPAR ligands attenuate IL-1 and silica-induced inflammatory mediator production in human lung fibroblasts via a PPAR-γ independent mechanism. PPAR Res 2011:318134
Hu H-H, Chen D-Q, Wang Y-N, Feng Y-L, Cao G, Vaziri ND, Zhao Y-Y (2018) New insights into TGF-β/Smad signaling in tissue fibrosis. Chem Biol Interact 292:76–83
Bae K-H, Seo JB, Seo H-Y, Kang SH, Jeon H-J, Lee JM, Lee S, Kim J-G, Lee I-K, Jung G-S, Park KG (2017) Lobeglitazone, a novel peroxisome proliferator-activated receptor γ agonist, attenuates renal fibrosis caused by unilateral ureteral obstruction in mice. Endocrinol Metab 32:115–123
Jiang F, Liu G-S, Dusting GJ, Chan EC (2014) NADPH oxidase-dependent redox signaling in TGF-β-mediated fibrotic responses. Redox Biol 2:267–272
Yeh YH, Kuo CT, Chang GJ, Qi XY, Nattel S, Chen WJ (2013) Nicotinamide adenine dinucleotide phosphate oxidase 4 mediates the differential responsiveness of atrial versus ventricular fibroblasts to transforming growth factor-beta. Circ Arrhythm Electrophysiol 6:790–798
Bondi CD, Manickam N, Lee DY, Block K, Gorin Y, Abboud HE, Barnes JL (2010) NAD(P)H oxidase mediates TGF-β1–induced activation of kidney myofibroblasts. J Am Soc Nephrol 21:93–102
Brown KD, Shah MH, Liu GS, Chan EC, Crowston JG, Peshavariya HM (2017) Transforming growth factor β1-induced NADPH oxidase-4 expression and fibrotic response in conjunctival fibroblasts. Invest Ophthalmol Vis Sci 58:3011–3017
Hakami NY, Dusting GJ, Chan EC, Shah MH, Peshavariya HM (2020) Wound healing after alkali burn injury of the cornea involves Nox4-type NADPH oxidase. Invest Ophthalmol Vis Sci 61:20
Shah MH, Chan EC, Van Bergen NJ, Pandav SS, Ng S, Crowston JG, Peshavariya HM (2020) Nox4 facilitates TGF beta 1-induced fibrotic response in human tenon’s fibroblasts and promotes wound collagen accumulation in murine model of glaucoma filtration surgery. Antioxidants. 9:1126
Gong Y, Yang Y (2020) Activation of Nrf2/AREs-mediated antioxidant signalling, and suppression of profibrotic TGF-β1/Smad3 pathway: a promising therapeutic strategy for hepatic fibrosis—a review. Life Sci 256:117909
Li WQ, Qureshi HY, Liacini A, Dehnade F, Zafarullah M (2004) Transforming growth factor Beta 1 induction of tissue inhibitor of metalloproteinases 3 in articular chondrocytes is mediated by reactive oxygen species. Free Radic Biol Med 37(2):196–207
Inoue I, Katayama S, Takahashi K, Negishi K, Miyazaki T, Sonoda M et al (1997) Troglitazone has a scavenging effect on reactive oxygen species. Biochem Biophys Res Commun 235:113–116
Lee YS, Park JS, Lee DH, Lee DK, Kwon SW, Lee BW, Bae SH (2018) The antidiabetic drug lobeglitazone protects mice from lipogenesis-induced liver injury via mechanistic target of rapamycin complex 1 inhibition. Front Endocrinol 9:539
Lee HW, Kim BY, Ahn JB, Kang SK, Lee JH, Shin JS, Ahn SK, Lee SJ, Yoon SS (2005) Molecular design, synthesis, and hypoglycemic and hypolipidemic activities of novel pyrimidine derivatives having thiazolidinedione. Eur J Med Chem 40:862–874
Kim SG, Kim DM, Woo J-T, Jang HC, Chung CH, Ko KS, Park JH, Park YS, Kim SJ, Choi DS (2014) Efficacy and safety of lobeglitazone monotherapy in patients with type 2 diabetes mellitus over 24-weeks: a multicenter, randomized, double-blind, parallel-group, placebo controlled trial. PLoS One 9:92843
Lee HS, Chang M, Lee J-E, Kim W, Hwang I-C, Kim D-H, Park H-K, Choi H-J, Jo W, Cha SW, Son WC (2014) Carcinogenicity study of CKD-501, a novel dual peroxisome proliferator-activated receptors alpha and gamma agonist, following oral administration to Sprague Dawley rats for 94-101 weeks. Regul Toxicol Pharmacol 69:207–216
Moon KS, Lee J-E, Lee HS, Hwang I-C, Kim D-H, Park H-K, Choi H-J, Jo W, Son W-C, Yun H-I (2014) CKD-501, a novel selective PPARgamma agonist, shows no carcinogenic potential in ICR mice following oral administration for 104 weeks. J Appl Toxicol 34:1271–1284
Walton KL, Johnson KE, Harrison CA (2017) Targeting TGF-β mediated SMAD signaling for the prevention of fibrosis. Front Pharmacol 8:461
Funding
This work was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science, and Technology (2017R1D1A3B03036549 and 2020R1I1A3073515).
Author information
Authors and Affiliations
Contributions
Conceptualization, Sun Woong Kim; Funding acquisition, Sun Woong Kim; Supervision, Sun Woong Kim; Investigation, Selikem Nuwormegbe; Methodology, Selikem Nuwormegbe and Sun Woong Kim; Formal analysis, Selikem Nuwormegbe and Na-Young Park; Writing original draft, Selikem Nuwormegbe; Writing—review and editing, Na-Young Park and Sun Woong Kim
Corresponding author
Ethics declarations
Ethics approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplemental information
ESM 1
(DOC 227 kb)
Rights and permissions
About this article
Cite this article
Nuwormegbe, S., Park, NY. & Kim, S.W. Lobeglitazone attenuates fibrosis in corneal fibroblasts by interrupting TGF-beta-mediated Smad signaling. Graefes Arch Clin Exp Ophthalmol 260, 149–162 (2022). https://doi.org/10.1007/s00417-021-05370-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-021-05370-2