Abstract
Purpose
To study the association of myopia progression with the morphological changes of optic disc and β-peripapillary atrophy (β-PPA) in 8–11 years old primary school students.
Methods
This study was a prospective, school-based investigation. This study included 610 children (1008 eyes) who were continuously observed and had data available from 2016 to 2017 in the Sanhe Cohort Study of the Risk Factors for Myopia (SCSRFM). The children underwent a comprehensive eye examination including measurement of visual acuity, autorefractometry, and posterior segment of the eye. β-PPA regions and optic disc ovality index were identified and measured on the fundus photographs.
Results
The prevalence of myopia was 72.62% (732/1008) in 2016. In myopic children, the prevalence of the vertical β-PPA, the horizontal β-PPA, and the oval optic disc were 75.68% (554/732), 75.96% (556/732) and, 11.61% (85/732) respectively. From 2016 to 2017, with the progression of vertical β-PPA, horizontal β-PPA, area of β-PPA, and optic disc ovality index, the myopic diopter and the axial length (AL) were increased. The progression of horizontal β-PPA was significantly correlated with the progression of myopic diopter and AL (all p < 0.05). The analysis on the distribution of progression rate of parameters in different groups found that the progression rate of horizontal β-PPA, area of β-PPA, and optic disc ovality index increased with the increase of the progression of diopter and AL. The progression of horizontal β-PPA, area of β-PPA, optic disc ovality index, and diopter in girls were greater than that in boys, and the progression of optic disc ovality index and diopter had a statistical significance (all p < 0.05).
Conclusions
The 1-year follow-up study of the third-grade primary school students showed that with the progression of myopia and the growth of AL, β-PPA and optic disc ovality index also changed. There was a positive correlation between the change of β-PPA and optic disc ovality index and the progression of myopia diopter and AL.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.

Introduction
As a complex disease with both genetic and environmental factors [1, 2], myopia is increasing in its prevalence globally, with a prediction that myopic population will account for 49.8% (4758 million) of the global population, with highly myopic population accounting for 9.8% (938 million) by 2050 [3]. Peripapillary atrophy (PPA) is frequently detected in highly myopic eyes and is considered to be a sign of pathological myopia among adults [4]. According to the histological changes of peripapillary region of highly myopic eyes, PPA had been considered to be composed of an alpha zone and a beta zone [5]. PPA alterations have been reported to be associated with older age and higher myopia [6].
Although many previous studies have focused on PPA and AL in high myopia, only few investigations have reported the prevalence, size, and associations of the β-PPA in eyes of children [7,8,9,10]. Myopia severity is reported to be associated with increased β-PPA and optic disc ovality. Multiple regression showed that increased β-PPA to optic disc area ratio is associated with increased axial length (AL), increased myopia severity, and increasing age [7]. The optic disc ovality index and the longitudinal variation of optic disc tilt axis can be evaluated with continuous fundus photographs. The relationship between the longitudinal changes of optic disc tilt and other factors provides important clues for the pathogenesis of myopia optic disc tilt [11]. Children around the age of 10 years are at the rapid growth and development period, and with the increased education load, the incidence of myopia would also gradually increase. The rapid progression of myopia in childhood will lead to high myopia and even pathological myopia, and pathological myopia will cause fundus changes. Therefore, it is very important to observe the changes of fundus during the children’s growth and development period and myopia progression, so as to monitor the progression of myopia and closely follow up on whether it will develop into pathological myopia. However, there is no follow-up study reporting on the relationship between the progression of myopia and the morphological changes of optic disc in the same person. Therefore, this 1-year follow-up study aims to observe the relationship between the progression of myopia and the morphological changes of β-PPA as well as the optic disc ovality index in school-age children.
Methods
Participants
This study was a prospective, school-based investigation. Using random cluster sampling, children from six primary schools of Sanhe city in Hebei province of Northern China were invited to participate in the Sanhe Cohort Study of the Risk Factors for Myopia (SCSRFM). At baseline, children with eye diseases or undergoing myopia control interventions, such as low concentration atropine and orthokeratology, were excluded. The study was approved by the Institutional Review Board of Beijing Tongren Hospital (QN20150228), Capital Medical University, and the protocol adhered to the Declaration of Helsinki.
The study included 1008 eyes of 610 children, 512 (50.79%) right eyes and 496 (49.21%) left eyes, who were continuously observed and had data available once a year from 2016 to 2017. There were 275 males (45.08%) and 335 females (54.92%), with an average age of 10.18 ± 0.47 (8–11) years old in 2016. Data on diopter, AL, and fundus images of all participants were obtained twice in 2016 and in 2017. Myopia was defined as a spherical equivalent (SE) refractive error less than − 0.5 diopters (D) [12].
Ocular examination
The children underwent a comprehensive eye examination including measurement of visual acuity and autorefractometry, and posterior segment of the eye. A Lenstar LS900 (Haag-Streit, Koeniz, Switzerland) was used to measure AL. Refractive error was confirmed with subjective refraction, and objective refraction was performed without cycloplegia using an automatic optometer RK-3000 (Topcon, Tokyo, Japan) to provide reference value. Fundus images were collected with non-mydriatic digital fundus photography (CR-DGI camera; Canon Inc., Tokyo, Japan). All examinations were carried out by trained ophthalmologists and optometrists.
Measurement of optic disc shape and external optic disc atrophy
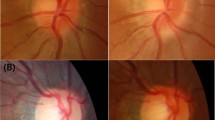
β-PPAs were identified and measured on the fundus photographs. The characteristics of β-PPA included good visibility of the large choroidal vessels and the sclera, thinning of the chorioretinal tissues, and circular boundary to the surrounding α area and to the peripapillary ring centrally [13]. All photographs were reviewed by 2 experienced ophthalmologists. The optic disc morphology and β-PPA were determined with image processing software (Beijing Institute of Technology, China), including the position of the optic disc and β-PPA. In addition, the following parameters were obtained, including the vertical width of β-PPA, horizontal width of β-PPA, the area of β-PPA, and optic disc ovality index (Fig. 1) [14]. The ovality index of the optic disc was measured as the maximal-to-minimal optic disc diameter ratio. The oval optic disc was defined as the optic disc ovality index exceeding 1.3 [12]. The values of the parameters obtained were pixel values. As the resolution of the fundus image was 3888 * 2592, the actual size of the fundus image was 22.2 mm * 14.8 mm, and the magnification of the fundus image was 1.4, the actual size of parameters in the fundus image could be calculated with the formula (um = (22.2*1000)/(3888*1.4)).
The parameters were obtained from the fundus, including outer vert diam (a), inner vert diam (b), outer horizontal diam (c), inner horizontal diam (d), and the areas of white circle and green circle, so as to calculate the vertical width of β-PPA (a–b), horizontal width of β-PPA (c–d), the area of β-PPA (white circle–green circle), and optic disc ovality index (b/d)
Statistical analysis
For the data with normal distribution, the mean ± standard deviation was used to describe the parameters, and Pearson’s correlation coefficients were used to explore the correlation between the parameters. For the data with non-normal distribution, the median and interquartile range were used to describe the parameters, and Spearman’s correlation was used to explore the correlation between the parameters. The rank sum test was performed to compare the differences between boys and girls parameters, and the mixed effect model was adopted to explore the influencing factors of diopter and AL progression. The prevalence of progression was defined as the number of progression (2017–2016)/the number of defined in 2016. In order to reduce the individual difference, the progression rate of parameters (progression rate = the value of progression (2017–2016)/the value in 2016) was further analyzed. The P < 0.05 was considered to be statistically significant. All analyses were performed using SPSS software version 20.0 (SPSS, Inc., IBM, NY, USA).
Results
The baseline description of parameters in myopic children in 2016
In this study, the prevalence of myopia was 72.62% (732/1008), 74.60% (382/512) in right eyes, and 70.56% (350/496) in left eyes. The average age of myopic children was 10.20 ± 0.48 years old, and the median diopter was − 1.62D. The median values of the vertical β-PPA, the horizontal β-PPA, the area of β-PPA, and the oval optic disc index were 40.84 μm, 161.16 μm, 347,871.86μm2, and 1.16. In myopic children, the prevalence of the vertical β-PPA, the horizontal β-PPA, and the oval optic disc were 75.68% (554/732), 75.96% (556/732), and 11.61% (85/732) respectively. There was no significant difference between the left eye and the right eye, and the detailed data are shown in Table 1.
Correlation analysis of parameters with AL and diopter in 2016
Univariate correlation analysis was made between the parameters and AL and diopter. With the increase of AL and myopic diopter, the vertical β-PPA and the horizontal β-PPA widened and the area of β-PPA increased. AL and the myopic diopter were significantly correlated with the vertical β-PPA, the horizontal β-PPA, and the area of β-PPA (all p < 0.05). However, the optic disc ovality index and the age did not have the statistically significant correlation with the myopic diopter and AL (all p > 0.05) (Table 2).
Description of parameters progression from 2016 to 2017
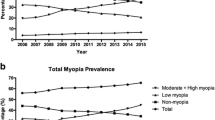
From 2016 to 2017, the median progression of diopter and axial length was − 0.63D and 0.39 mm, respectively. The median values of the progression of the vertical β-PPA, the horizontal β-PPA, the area of β-PPA, and the optic disc ovality index were 28.06 μm, 80.49 μm, 155,314.97μm2, and 0.03. The vertical β-PPA, the horizontal β-PPA, the area of β-PPA, and the optic disc ovality index increased in most children, the prevalence of progression of which were 66.80% (489/732), 83.33% (610/732), and 74.59% (546/732) respectively (Fig. 2). There was no significant difference between the left eye and the right eye, and the detailed data are shown in Table 3.
Correlation analysis on parameters progressions from 2016 to 2017
In order to further clarify the correlation between the progression of parameters and the progression of AL and myopic diopter, univariate regression analysis was conducted. The results showed that horizontal β-PPA increased with the progression of myopia and the increase of AL. The progression of horizontal β-PPA was significantly correlated with the progression of myopic diopter and AL (p = 0.017 and p = 0.019) (Table 4).
The analysis on the progression rate of parameters
In order to reduce the individual difference, this study further analyzed the progression rate of each parameter. The analysis on the distribution of progression rate of parameters in different groups found that the progression rate of horizontal β-PPA, area of β-PPA, and optic disc ovality index were higher in the groups of myopic diopter < − 1D, and the difference was significant (all p < 0.05) (Table 5), while the progression rate of horizontal β-PPA, area of β-PPA, and optic disc ovality index were higher in the Q4 group, and the difference was significant (all p < 0.05) (Table 6). Therefore, the results indicated that the faster the increase of myopia diopter and AL was, the greater the progression of β-PPA and the change of optic disc ovality would be.
The gender difference of the parameters
In different genders, the prevalence of myopia was 67.19% (301/448) in boys, and 76.96% (431/560) in girls. In the myopic children, the prevalence of the vertical β-PPA, the horizontal β-PPA, and the oval optic disc were 76.41% (230/301), 76.74% (231/301), and 9.97% (30/301) in boys, while were 75.17% (324/431), 75.41% (325/431), and 12.76% (55/431) in girls respectively. The prevalence of myopia and the oval optic disc were higher in girls than in boys in 2016. From 2016 to 2017, the progression of horizontal β-PPA, area of β-PPA, optic disc ovality index, and diopter in boys were less than that in girls, and the progression of optic disc ovality index and diopter had a statistical significance (all p < 0.05). The detailed data are shown in Table 7.
Discussion
This study mainly investigated the association of β-PPA and optic disc ovality index changes with the progression of diopter and AL. In children aged 8–11 years, with the progression of AL and diopter, all the indexes of the β-PPA and optic disc ovality index increased. At the same time, the indexes of β-PPA were significantly correlated with AL and diopter; thus, the follow-up of β-PPA is of predictive value with regard to the development of myopia, and the increase of β-PPA can indicate that the myopia is still progressing, especially for children aged 8–11 years. The current study revealed that the progressions of the AL and diopter were correlated with the increase of the horizontal β-PPA. Further analysis showed that the changes of β-PPA and optic disc ovality index were greater in the groups with < − 1D progression, and the changes of β-PPA and optic disc ovality index were greater when the progression of AL was longer than 0.47 mm. As the change of optic disc could reflect the growth of myopia, it is of great significance for follow-up of the progression of myopia, especially, given the fundus images were easy to obtain. With the progression of myopia, the increase of AL, the corresponding change of optic disc morphology and β-PPA could be used as an important indicator for the monitoring of myopia progression, which also provided a new approach for the study of mechanism of myopia and myopia control.
In the current study, the incidence of myopia was analyzed to gain a better understanding of the refractive status of 8–11 years old children with myopia. In recent years, the prevalence of myopia in children has been increasing, and the age of myopic children has gradually become younger. The prevalence of myopia in 12-year-old children in Hong Kong had reached 61.5% [15], while in other areas of East Asia where myopia prevalence is still high. The prevalence of myopia among young students was 26.4–76.5% [16]. In the current study, the incidence of myopia reached 72.62%, which was higher than other studies. The main reason may be that the refractive error was assessed without cycloplegia, as the prevalence of myopia in the current study was similar to that in other studies that also did not use cycloplegia [17].
Many studies have shown that there is a significant correlation between PPA and myopia, especially in high myopia. Jonas et al. [5] examined the parapapillary region in highly myopic eyes histomorphometrically and found that the length of the scleral flange, the sclera between the optic nerve edge and optic nerve dura mater, increased as the AL increased. In highly myopic eyes, the parapapillary region consisted of an elongated parapapillary scleral flange, and the parapapillary retina was composed of only the retinal nerve fiber layer or its remnants, without any other retinal layers. The underlying Bruch’s membrane and choroid were also absent. These histologic features could be observed in eyes with high myopia. Li et al. also found, in highly myopic Chinese populations, β-PPA, optic disc tilting, and rotation are very common. Older age, female gender, and greater myopic spherical equivalent are risk factors of greater degree of optic disc tilting [18]. For school-age children, generally low myopia is more common, and some studies have shown that myopia in school-age children is also related to the β-PPA. Guo [13] found that larger β-PPA area was associated with longer indoors studying time after adjustment for AL, refractive error, and region of habitation. As a corollary, longer indoors studying time was significantly associated with a larger area of β-PPA after adjusting for a higher AL/corneal curvature (CC) ratio and urban region of habitation. In the follow-up examination, an increase in the AL/CC ratio and in AL was significantly associated with longer indoors studying time and larger β-PPA area. In the current study, with the increase of AL and myopia diopter, the horizontal β-PPA also progressed. Further analysis showed that the proportion of children with increase of the horizontal width and area of the β-PPA was higher in the groups with < − 1D progression, while for the group with the longest AL progression, the proportion of children with increase of the horizontal width and area of the β-PPA was the highest. In the current study, the morphological changes and progression of β-PPA were analyzed, presenting the β-PPA in myopia students about 10 years old, and revealing that the β-PPA will gradually widen with diopter and AL, mainly in the horizontal direction. The progression of diopter and AL was statistically different from that of the horizontal PPA. Especially, the longer the AL was and the higher of myopia was, the wider the β-PPA would be. Through the follow-up on the changes of β-PPA, the researchers could evaluate the myopia progression and prevention efficacy to a certain extent. However, the β-PPA also occurred in normal axial growth and not all myopic child had β-PPA; thus, the presence of myopia could not be determined by the β-PPA alone, and the children’s refractive state should also be taken into consideration. Meanwhile, the relationship between the appearance of β-PPA and the development of eyeball and the progression of myopia needs to be analyzed through long-term follow-up and observation.
The current study showed that the change of optic disc ovality index was also significantly correlated with the progression of myopia. Sun et al. analyzed 220 myopic eyes and found that the upper optic disc rotation was more likely to occur than the lower optic disc rotation, and it was correlated with intraocular pressure, AL, and area of the β-PPA [12]. The papillary and peripapillary regions of highly myopic eyes are distorted by the mechanical stretching of the globe in high myopia. The stretching results in the formation of various kinds of deformities of the optic discs including tilted optic discs, acquired large cups, and small discs [19]. In previous studies [10], the maximum width of the PPA and the vertical diameter of the optic disc were used to show the relationship between optic disc tilt and myopia progression (ONH/PPA, the maximum PPA width to vertical disc diameter). The univariate analysis revealed that ONH/PPA change was significantly associated with age between 7 and 9 years, initial spherical equivalents (SEs) and change of SEs during follow-up, and association of age between 7 and 9 years with the change of SEs remained statistically significant in the multivariate analysis. The results showed that for school-age children, with the progression of myopia, the degree of optic disc tilt increased. Based on the optic disc shape assessed by its ovality factor (measured as the maximal-to minimal optic disc diameter ratio), Guo et al. [14] revealed that the prevalence of oval optic discs (defined as a maximal-to-minimal disc diameter ratio of ≥ 1.33) was 6.6%. A greater optic disc ovality was significantly associated with older age, female sex, larger β-PPA, and shorter time spent indoors studying, and was associated with greater increase in myopic refractive error with marginal significance. In univariate analysis, the presence of oval optic discs was additionally associated with higher AL/CC ratio and greater myopic refractive error. In this study, the prevalence was 11.61%, which was higher than that in other studies. The main reason was that the children in this study were older, and the optic disc ovality was defined as greater than 1.3 according to the literature [12]. Therefore, the results of this study, to a certain extent, reflect the prevalence of optic disc ovality in 10-year-old myopic children. In the population-based cross-sectional study of the adolescent children from Singapore Cohort Study of Risk Factors for Myopia (SCORM) [8], Samarawickrama et al. identified 454 (37.0% sample prevalence) cases of tilted optic disc. The adolescents with tilted optic discs tended to have a longer AL and a greater myopic SER. After adjusting for age, gender, ethnicity, AL, and cylindrical error, tilted optic discs were significantly associated with myopic refractive error. Adolescents of Chinese ethnicity had the highest proportion of tilted optic discs. At the same time, Hwang et al. suggested that the degree of optic disc tilt and the longitudinal variation of optic disc tilt axis could be evaluated by continuous fundus photographs. They believe that the relationship between the longitudinal changes of optic disc tilt and other factors can provide important clues for the pathogenesis of myopia optic disc tilt [11]. However, there is no further evidence on the relationship between the change of optic disc tilt and the progression of myopia during follow-up. In this study, the changes of optic disc ovality index in children with different diopter and AL progressions were analyzed through 1-year follow-up, showing that the progression of myopia and AL was positively correlated with the increase of optic disc ovality index, with statistical significance. The results of this study also showed that there is a correlation between optic disc ovality and diopter. With the increase of myopia diopter, the optic disc ovality index also increased, which was consistent with other studies. In addition, this study also revealed that for children with longer AL and increased diopter, the increase of optic disc ovality would be greater.
The reason for the change of fundus optic disc is not very clear at present. Some studies have shown it might be related to the thickness of the choroid. In Chen’s study, 821 young myopic patients were tested for the optic disc tilt, PPA, and the thickness of the choroid and found that the prevalence of the optic disc tilt and PPA increased as AL increased, while with the increase of the area of PPA, the choroidal thickness of macular and peripapillary decreased. In addition, with the increase of the rate of optic disc tilt, the choroidal thickness of macular increased, and the peripapillary choroidal thickness decreased [20]. The area of β-PPA was also correlated with the density of peripapillary capillaries. Sung et al. examined 80 myopic subjects with β-PPA whose mean AL and SE refractive error were 26.47 ± 1.17 mm and − 6.28 ± 2.71 diopters. The group with the presence of Bruch membrane (BM) had a more inferiorly rotated optic disc, larger β-PPA, and lower superficial and deep parapapillary vessel density. Multivariate linear regression analysis showed that the average PPA + BM width on horizontal scans was significantly associated with superficial and deep parapapillary vessel density (P = 0.034 and P = 0.003, respectively). So PPA was closely correlated with parapapillary vessel density [21]. Therefore, for children with myopia, the morphological changes of optic disc and β-PPA were of great significance for the study of the pathogenesis of myopia. Meanwhile, this study showed that the morphological changes of optic disc and β-PPA in the follow-up of myopia were also an important indicator for the evaluation of myopia progression and had great potential in the prevention and control of myopia.
There are some differences in myopia progression between genders. Czepita et al. studied the role of gender in the progression of myopia among Polish schoolchildren, with 4875 children from elementary schools and high schools examined (2470 boys, aged 6–16 years, mean age 11.0, SD = 2.6 and 2405 girls, aged 6–16 years, mean age 11.1, SD = 2.6). It was found that the SE among Polish boys was similar to that among Polish girls before the age of 9 years. However, in older children, lower SE values and higher prevalence of myopia were found among girls, both at 9–13 years range and at 13–16 years range [22]. Rudnicka et al. also reported that sex difference in the age-specific prevalence of myopia exists in whites and East Asians, which emerges at about 9 years of age and becomes more marked through adolescence showing double the odds of myopia in girls compared with boys [23]. In the Handan Offspring Myopia Study, the prevalence of myopia (spherical equivalent refraction < − 0.5 diopter) were 23.5% in males and 30.8% in females [24]. In the current study, the primary school students were mostly 10 years old, and the prevalence of myopia was 67.19% in boys, and 76.96% in girls. The study also found that the progression of horizontal β-PPA, area of β-PPA, optic disc ovality index, and diopter in girls were slightly faster than that in boys. To some extent, the changes of fundus in girls might be faster than that in boys during the development of myopia.
The current study also has some limitations. Firstly, the follow-up interval was only 1 year, and some subtle changes would not be identified in such a short time period, so this study fails to observe the long-term changes. Therefore, the follow-up interval should be increased in the future research. Second, as the parents of the students did not agree to use cycloplegia, the refractive error was assessed without cycloplegia. However, for children who were suspected of spasm of accommodation, the fogging lenses were performed to negate the effect of accommodation, which could improve the accuracy to a certain extent, and also could reflect the refractive state of the children [25, 26].
The 1-year follow-up study of the third-grade primary school students showed that the myopia progressed significantly. It was also found that with the progression of myopia and the growth of AL, the β-PPA and the optic disc ovality index also changed. There was a positive correlation between the change of the β-PPA and optic disc ovality index and the progression of myopia diopter and AL.
References
Cai XB, Shen SR, Chen DF, Zhang Q, Jin ZB (2019) An overview of myopia genetics. Exp Eye Res 188:107778. https://doi.org/10.1016/j.exer.2019.107778
Jin ZB, Wu J, Huang XF, Feng CY, Cai XB, Mao JY, Xiang L, Wu KC, Xiao X, Kloss BA, Li Z, Liu Z, Huang S, Shen M, Cheng FF, Cheng XW, Zheng ZL, Chen X, Zhuang W, Zhang Q, Young TL, Xie T, Lu F, Qu J (2017) Trio-based exome sequencing arrests de novo mutations in early-onset high myopia. Proc Natl Acad Sci U S A 114:4219–4224. https://doi.org/10.1073/pnas.1615970114
Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, Wong TY, Naduvilath TJ, Resnikoff S (2016) Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology 123:1036–1042. https://doi.org/10.1016/j.ophtha.2016.01.006
Cai XB, Zheng YH, Chen DF, Zhou FY, Xia LQ, Wen XR, Yuan YM, Han F, Piao SY, Zhuang W, Lu F, Qu J, Yu AY, Jin ZB (2019) Expanding the phenotypic and genotypic landscape of nonsyndromic high myopia: a cross-sectional study in 731 Chinese patients. Invest Ophthalmol Vis Sci 60:4052–4062. https://doi.org/10.1167/iovs.19-27921
Jonas JB, Jonas SB, Jonas RA, Holbach L, Panda-Jonas S (2011) Histology of the parapapillary region in high myopia. Am J Ophthalmol 152:1021–1029. https://doi.org/10.1016/j.ajo.2011.05.006
Liu W, Gong L, Li Y, Zhu X, Stewart JM, Wang C (2017) Peripapillary atrophy in high myopia. Curr Eye Res 42:1308–1312. https://doi.org/10.1080/02713683.2017.1307992
Tong L, Saw SM, Chua WH, Luu C, Cheng B, Yeo I, Wong E, Tan D, Koh A (2004) Optic disk and retinal characteristics in myopic children. Am J Ophthalmol 138:160–162. https://doi.org/10.1016/j.ajo.2004.02.026
Samarawickrama C, Mitchell P, Tong L, Gazzard G, Lim L, Wong TY, Saw SM (2011) Myopia-related optic disc and retinal changes in adolescent children from Singapore. Ophthalmology 118:2050–2057. https://doi.org/10.1016/j.ophtha.2011.02.040
Samarawickrama C, Pai A, Tariq Y, Healey PR, Wong TY, Mitchell P (2012) Characteristics and appearance of the normal optic nerve head in 6-year-old children. Br J Ophthalmol 96:68–72. https://doi.org/10.1136/bjo.2010.197426
Kim TW, Kim M, Weinreb RN, Woo SJ, Park KH, Hwang JM (2012) Optic disc change with incipient myopia of childhood. Ophthalmology 119:21–26. https://doi.org/10.1016/j.ophtha.2011.07.051
Hwang YH, Kim YY (2012) Myopic optic disc changes in adolescents. Ophthalmology 119:885–886. https://doi.org/10.1016/j.ophtha.2011.12.004
Sung MS, Kang YS, Heo H, Park SW (2016) Characteristics of optic disc rotation in myopic eyes. Ophthalmology 123:400–407. https://doi.org/10.1016/j.ophtha.2015.10.018
Guo Y, Liu LJ, Xu L, Lv YY, Tang P, Feng Y, Zhou JQ, Meng M, Jonas JB (2014) Parapapillary beta zone in primary school children in Beijing: associations with outdoor activity. Invest Ophthalmol Vis Sci 55:918–925. https://doi.org/10.1167/iovs.13-13502
Guo Y, Liu LJ, Xu L, Lv YY, Tang P, Feng Y, Zhou JQ, Meng M, Jonas JB (2015) Optic disc ovality in primary school children in Beijing. Invest Ophthalmol Vis Sci 56:4547–4553. https://doi.org/10.1167/iovs.15-16590
Mak CY, Yam JC, Chen LJ, Lee SM, Young AL (2018) Epidemiology of myopia and prevention of myopia progression in children in East Asia: a review. Hong Kong Med J 24:602–609. https://doi.org/10.12809/hkmj187513
Xiang ZY, Zou HD (2020) Recent epidemiology study data of myopia. J Ophthalmol 2020:4395278. https://doi.org/10.1155/2020/4395278
Grzybowski A, Kanclerz P, Tsubota K, Lanca C, Saw SM (2020) A review on the epidemiology of myopia in school children worldwide. BMC Ophthalmol 20:27. https://doi.org/10.1186/s12886-019-1220-0
Li Z, Guo X, Xiao O, Lee PY, Liu R, Wang D, Sankaridurg P, He M (2018) Optic disc features in highly myopic eyes: the ZOC-BHVI High Myopia Cohort Study. Optom Vis Sci 95:318–322. https://doi.org/10.1097/OPX.0000000000001200
Ohno-Matsui K, Lai TY, Lai CC, Cheung CM (2016) Updates of pathologic myopia. Prog Retin Eye Res 52:156–187. https://doi.org/10.1016/j.preteyeres.2015.12.001
Chen Q, He J, Yin Y, Zhou H, Jiang H, Zhu J, Ohno-Matsui K, Zou H, Fan Y, Xu X (2019) Impact of the morphologic characteristics of optic disc on choroidal thickness in young myopic patients. Invest Ophthalmol Vis Sci 60:2958–2967. https://doi.org/10.1167/iovs.18-26393
Sung MS, Heo H, Park SW (2018) Microstructure of parapapillary atrophy is associated with parapapillary microvasculature in myopic eyes. Am J Ophthalmol 192:157–168. https://doi.org/10.1016/j.ajo.2018.05.022
Czepita M, Czepita D, Safranow K (2019) Role of gender in the prevalence of myopia among Polish schoolchildren. J Ophthalmol 2019:9748576. https://doi.org/10.1155/2019/9748576
Rudnicka AR, Kapetanakis VV, Wathern AK, Logan NS, Gilmartin B, Whincup PH, Cook DG, Owen CG (2016) Global variations and time trends in the prevalence of childhood myopia, a systematic review and quantitative meta-analysis: implications for aetiology and early prevention. Br J Ophthalmol 100:882–890. https://doi.org/10.1136/bjophthalmol-2015-307724
Gao TY, Zhang P, Li L, Lin Z, Jhanji V, Peng Y, Li ZW, Sun LP, Han W, Wang NL, Liang YB (2014) Rationale, design, and demographic characteristics of the Handan Offspring Myopia Study. Ophthalmic Epidemiol 21:124–132. https://doi.org/10.3109/09286586.2014.887734
Queiros A, Gonzalez-Meijome J, Jorge J (2008) Influence of fogging lenses and cycloplegia on open-field automatic refraction. Ophthalmic Physiol Opt 28:387–392. https://doi.org/10.1111/j.1475-1313.2008.00579.x
Suryakumar R, Bobier WR (2003) The manifestation of noncycloplegic refractive state in pre-school children is dependent on autorefractor design. Optom Vis Sci 80:578–586. https://doi.org/10.1097/00006324-200308000-00012
Funding
The Beijing Hospitals Authority provided financial support in the form of Beijing Hospitals Authority Clinical medicine Development of special funding support (XMLX202133) funding; the work committee for women and children of China State department provided financial support in the form of Fund of work committee for women and children of China State department (2014108) funding; and the Beijing Institute of Ophthalmology provided financial support in the form of Beijing Institute of Ophthalmology Key Research Program Funding Projects (2019009) funding.
The sponsors had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Contributions
Conception and design (XHW, JSZ, JL, JDW); acquisition of data (JSZ, JL, JDW, YX, SMH, XLS, SYC, ZYL); analysis and interpretation of data (JSZ, KC); drafting the article or revising it (SJZ, MY); final approval of the version (ZBJ, NLW, XHW).
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional Review Board of Beijing Tongren Hospital (QN20150228), Capital Medical University and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhang, JS., Li, J., Wang, JD. et al. The association of myopia progression with the morphological changes of optic disc and β-peripapillary atrophy in primary school students. Graefes Arch Clin Exp Ophthalmol 260, 677–687 (2022). https://doi.org/10.1007/s00417-021-05331-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-021-05331-9