Abstract
Purpose
To prospectively evaluate the effect of benzalkonium chloride (BAK)-preserved latanoprost on ocular surface damage and identify the associated risk factors among treatment-naive glaucoma patients.
Methods
The basal Schirmer’s test results, corneal Oxford staining score, non-invasive keratograph tear-breakup time, oculus hyperemia index score (objective metrics), and ocular surface disease index (OSDI) questionnaire (subjective metric) were evaluated at baseline, 1 month, and 4 months after receiving latanoprost eye drops. Associated risk factors were assessed by multivariate linear regression.
Results
Seventy-four eyes (44 patients) were enrolled. Basal Schirmer’s test tear-flow and Oxford scores gradually deteriorated (β = −0.14, P = 0.001 and β = 0.1, P < 0.001, respectively). The percentage of unstable tear-film (breakup time < 10 s) increased significantly at 4 months (6.21% vs 9.11%, P = 0.042). Hyperemic scores increased significantly at 1 month and normalized at 4 months (P = 0.01 and P = 0.16, respectively); total OSDI scores tended to improve (β = −0.76, P = 0.06). Older age was associated with additional corneal Oxford staining (P = 0.005); female sex was associated with increased unstable tear-film scores (P = 0.01). Artificial tear use was associated with a smaller decrease in basal Schirmer’s test values (P = 0.01) and a smaller increase in unstable tear-film scores (P = 0.02).
Conclusions
Preserved latanoprost eye drops affected ocular surface changes in glaucoma patients through decreased basal tear secretion. Artificial tears represent an early intervention in vulnerable glaucoma patients with reduced tear secretion and impaired tear-film stability.
Similar content being viewed by others
Avoid common mistakes on your manuscript.

Introduction
Glaucoma is the leading cause of vision loss, currently affecting more than 70 million people worldwide; it is estimated to affect 111 million people by 2040 [1]. Topical eye drops have been the first line of therapy to control intraocular pressure and slow glaucoma progression in glaucoma patients for decades [2]. A serious issue with topical glaucoma medication is the risk for developing ocular surface disease (OSD) because 30–60% of patients with topical glaucoma eye drops reported having OSD on a questionnaire [3, 4].
The mechanism of OSD is complex and characterized by an inadequate quantity of tears, unstable tear film, and ocular surface breakdown. The symptoms of OSD include visual interference, irritation, burning, foreign body sensation, itching, and dryness [5]. Certain ocular conditions can aggravate the symptoms of OSD, including meibomian gland dysfunction, wearing contact lenses, keratopathy exposure, and lid malposition [6]. In previous literature, subjective and objective assessments were inconsistently utilized in different studies measuring OSD in glaucoma patients. [7].
The most widely used subjective measurement tool for assessing symptoms of OSD is the ocular surface disease index (OSDI), which is a valid and reliable instrument for measuring the severity of dry eye disease [8]. Previous studies found that glaucoma patients receiving topical therapy had higher OSDI scores than normal controls [9, 10]. Associated factors found with OSD in glaucoma patients included higher exposure to benzalkonium chloride (BAK), increased glaucoma severity, older age, number of medications, and long durations of treatment [9,10,11]. However, another study stated the higher scores of OSDI in glaucoma patients mainly stemmed from vision-related subscores of OSDI, instead of ocular discomfort-related subscores [12].
Objective measures assessing physiologic functions that influence ocular surface health have been developed over the past decades to evaluate OSD in glaucoma patients. The Schirmer’s test, commonly utilizing a limit of 5 mm wetting of the filter-paper strip under anesthesia to discriminate the sicca syndrome [13], has been shown to evaluate tear lacrimation in glaucoma patients; in addition, previous studies found a varying degree of decreased Schirmer’s test values compared to normal controls [4, 12]. The measurement of tear breakup time (TBUT) is a broadly used clinical technique, which can be performed after instillation of a fluorescein dye [14] or by keratography without the need for fluorescein [15]. Decreased TBUT has also been reported in glaucoma patients receiving topical medications [4, 16]. In glaucoma patients treated over long periods, elevated levels of IL-8 and IL-10 have been found in the conjunctival epithelium, and increased inflammatory cells were observed in the conjunctiva and trabecular meshwork using impression cytology [17].
The BAK preservative has demonstrated reduced tear production and nerve fiber density of the cornea, increased infiltration of inflammatory cells, and corneal staining in animal studies [18]. Although the high prevalence of OSD in glaucoma patients may result from the deleterious effect of preservatives in glaucoma medication [19, 20], preservative-free glaucoma medication is more expensive and may not be available in every country. While most previous studies compare glaucoma patients with topical therapy to normal control patients, a prospective study to investigate the impact of glaucoma eye drops on ocular surface disease is lacking. Moreover, the factors predictive of OSD risks in real-world clinical practice remain unknown.
In this study, we investigated the influence of a BAK-preserved latanoprost treatment on OSD in treatment-naive glaucoma patients. The serial changes in lacrimation function, tear film stability, conjunctival hyperemia, and corneal staining were documented and compared to the subjective symptoms of OSD. In addition, the important influencing predictors were identified.
Methods
This study protocol was approved by the Ethics Review Board of the National Taiwan University Hospital. Participants signed written informed consent forms and completed study procedures between June 2018 and June 2019.
Study patients
Consecutive patients aged 20 years or older were recruited prospectively from the Glaucoma Clinic of the National Taiwan University Hospital. Patients were eligible for enrollment if they were newly diagnosed with primary open-angle glaucoma or ocular hypertension in our clinic, and began using 0.005% latanoprost (containing 0.02% benzalkonium chloride as a preservative) (Xalatan, Pfizer, NY, USA), which has been one of the standard treatment methods for treating glaucoma patients at our institution.
Individuals who had a history of ocular trauma, contact lens wear, secondary glaucoma, clinically significant diseases affecting the ocular surface and meibomian gland, or required additional anti-glaucoma medication due to poor intraocular pressure control were excluded. All patients were instructed not to use any topical ophthalmic medications other than the given study medication during the period of study. Lubricant was prescribed to patients with complaints of dry eye and basal Schirmer’s test values ≤5 mm; the use of lubricants was analyzed as a possible influential factor for ocular surface disease.
Comprehensive ophthalmic and medical histories were obtained at the baseline visit. Documented risk factors associated with dry eye disease were recorded, including a history of corneal refractive surgery, rheumatoid disease, diabetes mellitus, and use of antidepressant medication. All participants underwent subjective and objective assessments at the beginning of BAK-latanoprost treatment and at 1-month and 4-month follow-up visits. The assessment consisted of administration of the ocular surface disease index (OSDI) questionnaire, keratography, slit lamp biomicroscopy, grading of the ocular surface, and a basal Schirmer’s test.
Ocular surface disease index questionnaire
The OSDI questionnaire was administered to all participants. The 12 items of the OSDI questionnaire were scored on a scale of 0 to 4, with scores of 0, 1,2,3, and 4 corresponding to the following answers: none of the time, some of the time, half of the time, most of the time, and all of the time, respectively. The total OSDI score was calculated based on the following formula: OSDI= [(sum of scores for all questions answered) × 100]/[(total number of questions answered) × 4]. The higher scores represented greater disability. Scores between 0 and 12 were categorized as normal; between 13 and 22, mild; between 23 and 32, moderate; and between 33 and 100, severe [8].
Assessment of ocular surface with keratography
An objective assessment with Keratograph 5 M (OCULUS Optikgerate GmbH, Wetzlar, Germany) was conducted before conventional examinations, with the intention of avoiding any influence of fluorescein on tear film stability. Noninvasive keratographic tear film break-up time (NIKBUT) was measured for each eye using infrared video, which generated the measurement of the first and average tear film break-up time (NIKf-BUT and NIKav-BUT), the location of first tear-break region, and the percentage of tear film break-up time of less than 10 s over the entire cornea (BUT10). The location of the first tear-break was further categorized into inferior and non-inferior types.
The tear meniscus height (TMH) was measured as the distance between the upper border of the tear meniscus and lower lid margin at the central point relative to the pupil center, perpendicular to the lid margin. Limbal and bulbar conjunctival hyperemia were assessed and scored automatically as the redness score (RS), according to the percentage area ratio between the blood vessels and the rest of the analyzed area in the limbar-nasal (LN), limbar-temporal (LT), bulbar-nasal (BN), and bulbar-temporal (BT) regions. In previous literature, the redness score demonstrated reliability and repeatability in ocular surface disease [21].
Grading of ocular surface
Ocular surface staining was performed by instilling one fluorescein drop and detecting superficial punctate keratopathy (SPK) with slit lamp examination. The grade of SPK was based on the area and density of exposed interpalpebral conjunctiva and cornea, and ranged from 0 to 5 according to the Oxford scale (0 = no staining; 1 = minimum; 2 = mild; 3 = moderate; 4 = marked; 5 = severe). [22]
Basal Schirmer’s test
The basal Schirmer’s test was performed to measure tearflow, with values ≤ 5 mm indicating impaired secretion [13]. Briefly, Schirmer’s test was performed with anesthesia by applying one drop of 0.5% proparacaine, and waiting for 5 min before applying a second drop. After another 5 min, the cotton swab was positioned between the lower fornix and lower lid margin to blot excess tears. The sterile filter-paper strip was placed at the junction between the middle and outer third of the lower eyelid for 5 min, avoiding contact between the cornea and paper strip. The test result was documented as the wet portion of the paper in millimeters (mm/5 min).
Statistical methods
The data have been reported as means ± standard deviation (SD). To evaluate the influence of BAK-latanoprost treatment on ocular surface disease, all continuous variables of subjective and objective assessments, including the OSDI score, basal Schirmer’s test, TMH, NIKf-BUT, NIKav-BUT, BUT10, R score-LT, R score-LN, R score-BT, R score-BN, and Oxford stain, were analyzed using a paired t-test to detect the differences between baseline versus 1-month data, and baseline versus 4-month data. A mixed liner model was used for trend analysis from baseline to the 4-month visit. Predictors of BAK-latanoprost that induced changes in ocular surface disease at 1 and 4 months were identified using multivariate linear regression models. The study outcomes included the results of the basal Schirmer’s test, BUT10, R score-BT, and Oxford stain.
To assess whether application of eye drops affect the location of the first tear-break region, a Chi-square test was used to compare the composition of inferior and non-inferior types between baseline and 1-month data, and baseline and 4-month data. Eyes with first tear-break up at simultaneous inferior and non-inferior locations were excluded from the analysis. P < 0.05 was considered to be statistically significant.
Results
The study enrolled 44 patients (74 eyes) receiving BAK-latanoprost treatment. Twenty-one patients (47.72%) were male, and the mean age at the baseline visit was 58.6 ± 11.88 years. Five patients (11.36%) had diabetes mellitus and six patients (13.64%) used antidepressant medications during the study period. Instillation of artificial tears was instructed in 16 eyes (21.62%); five eyes (6.76%) had history of LASIK surgery.
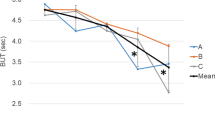
The subjective and objective measurements of ocular surface disease among 74 eyes at baseline, 1-month, and 4-month visits are listed in Table 1. The tearflow on the basal Schirmer’s test significantly decreased from 9.42 mm to 7.11 mm after 1 month (P = 0.007), and further deteriorated to 6.84 mm after 4 months (P = 0.003). The distribution of basal Schirmer’s test values among all eyes administered BAK-latanoprost during the study period is demonstrated in Fig. 1.
A mixed linear model showed an overall decreasing trend of basal Schirmer’s test values from baseline to 4 months after treatment (β = −0.14, P = 0.001). Regarding tear film stability, the NIKf-BUT and NIKav-BUT values did not change significantly at the 1-month visit (P = 0.916 and P = 0.357, respectively) or at the 4-month visit (P = 0.939 and P = 0.198, respectively). Nonetheless, BUT10 values increased from 6.21% to 6.44% at the 1-month visit (P = 0.813) and rose significantly to 9.11% at the 4-month visit (P = 0.042). The distribution of BUT10 among all eyes during the study period with BAK-latanoprost is demonstrated in Fig. 2. A mixed linear model showed a marginal increasing trend in BUT10 values (β = 1.22, P = 0.06).
Among 16 eyes receiving lubricants under instruction, the tearflow on the basal Schirmer’s test increased from 4.07 mm to 6.67 mm after 1 month (P = 0.090) and to 5.38 mm after 4 months (P = 0.106), although it did not reach statistical significance. The tear film stability with regard to NIKf-BUT, NIKav-BUT, and BUT10 also showed marginal improvement among the 16 eyes receiving lubricants. NIKf-BUT values increased from 6.94 s to 8.33 s after 1 month (P = 0.120) and to 6.74 s after 4 months (P = 0.874); NIKav-BUT values increased from 9.16 s to 11.02 s after 1 month (P = 0.063) and to 12.20 s after 4 months (P = 0.067). BUT10 decreased from 11.82% to 7.82% after 1 month (P = 0.275) and to 5.5% after 4 months (P = 0.214).
The hyperemic scores increased significantly in both, limbal and temporal regions at the 1-month visit, as the R score-LT (P = 0.001), R score-LN (P = 0.01), R score-BT (P = 0.01), and R score-BN (P = 0.02) all reached significance. Intriguingly, compared to the scores at 1-month, the R score-LT, R score-LN, R score-BT, and R score-BN all decreased at the 4-month visit. The Oxford stain values significantly increased from 0.07 to 0.2 after 1 month (P = 0.003) and further rose to 0.26 after 4 months (P = 0.001). A mixed linear model showed an overall increasing trend of Oxford stain grading from baseline to 4 months after treatment (β = 0.1, P < 0.001).
Unexpectedly, the subjective assessment of OSDI scores showed significant improvement from 6.85 to 4.23 at the 1-month visit (P < 0.001) and was 5.28 at the 4-month visit (P = 0.179). The mixed linear model showed an overall decreasing trend of OSDI scores (β = −0.76, P = 0.06).
The location of first tear film breakup had a tendency of shifting from a non-inferior to inferior location after medication use (Table 2); however, statistical significance was not observed at the 1-month and 4-month visits (P = 0.48 and P = 0.85, respectively).
Among 26 eyes with non-inferior first tear breakup at the baseline visit, 11 (42.31%) and 13 (50%) eyes demonstrated first tear breakup at an inferior location after instillation of eye drops at the 1-month and 4-month visits, respectively. Among 43 eyes with inferior first tear breakup at the baseline visit, inferior location remained the first tear breakup location in 36 (83.72%) and 26 eyes (63.41%) at 1-month and 4-month visits, respectively.
Predictors of ocular surface outcomes: Multivariate analysis
The predictors of ocular surface diseases induced by BAK-latanoprost treatment after 1-month and 4-months of treatment are listed in Tables 3 and 4.
In the multivariate regression models, older age (+0.15 mm wetting per year; 95% confidence interval [CI], 0.03 to 0.28; P = 0.02) and use of artificial tears (+4.92 mm wetting; 95% CI, 1.3 to 8.54; P = 0.01; Table 3) were associated significantly with smaller decrements in 1-month basal Schirmer test values. Similarly, older age (+0.2 mm wetting per year; 95% CI, 0.06 to 0.35; P = 0.01) and use of artificial tears (+4.64 mm wetting per year; 95% CI, 0.35 to 8.93; P = 0.03; Table 4) were significantly associated with smaller decrements in 4-month basal Schirmer’s test values.
Regarding tear film stability, the regression model identified male gender (−8.87%; 95% CI, −14.67 to −3.07; P = 0.003) and the use of artificial tears (−10.08%; 95% CI, −18.12 to –2.04; P = 0.02; Table 4) to be associated with smaller increments of BUT10 at the 4-month visit. The increment in BUT10 values at the 1-month visit was not significant on paired t-tests; therefore, none of the variables reached statistical significance in predicting BUT10 at 1-month (Table 3) on regression. Interestingly, older age (−0.01 per year; 95% CI, −0.02 to −0.001; P = 0.03) was associated with smaller increments in R score-BT values, while male gender (+0.34; 95% CI, 0.07 to 0.62; P = 0.01; Table 3) was found to be associated with greater increments of R score-BT values at 1-month.
Older age (+0.01 per year; 95% CI, 0.004 to 0.02; P = 0.005) and use of antidepressant medication (+0.58; 95% CI, 0.19 to 0.97; P = 0.004; Table 4) were associated significantly with increments in 4-month Oxford stain values.
Discussion
In this study, we reported longitudinal follow-up outcomes of ocular response to BAK-latanoprost treatment in glaucoma patients, using subjective and objective measurements. All of the patients were newly diagnosed and were treatment-naive. At baseline, the average basal Schirmer’s test value was 9.42 mm and the average of OSDI score was 6.85; this had been categorized into mild and moderately severe OSD in previous literature [3]. Objective measurements comprising the basal Schirmer’s test for tear lacrimation, BUT10 for tear film stability, and corneal Oxford staining all showed deterioration during the follow-up period. A lack of agreement was found between subjective OSDI scores and objective measurements in the current study. An improved OSDI score was observed among all eyes at the 1-month visit (P < 0.001). Improved OSDI scores could also be found among all 58 eyes not receiving artificial tears during the study period (5.91 ± 5.72 to 3.51 ± 4.03, P = 0.002). The OSDI score is not a robust metric for reflecting ocular surface disease alteration, as objective outcomes worsened in this study.
Similar to our findings, two studies showed discordance between symptoms and signs in glaucoma patients receiving topical therapy [4, 16]. Ghosh et al. found that signs, but not symptoms of OSD are significantly higher in individuals receiving topical glaucoma therapy than control patients [4]. Cvenkel et al. claimed that although clinical tests and impression cytology revealed ocular surface damage in patients using preserved antiglaucoma medications, the OSDI score failed to discriminate between the medication and control groups [16].
Our results suggest an overall trend of decreasing tear secretion (β = −0.14, P = 0.001) and increasing corneal staining after topical therapy (β = 0.1, P < 0.001). The difference between post-treatment and pre-treatment values could be observed at 1-month and 4 months intervals on paired t-tests. Many research studies have compared commercial 0.02% BAK-latanoprost to preservative-free latanoprost or tafluprost; they demonstrated that BAK-latanoprost significantly reduces the viability of human corneal epithelial cells ex vivo, significantly enhances cellular damage, and induces more inflammatory cell infiltration in vivo [23, 24]. A concentration of 0.01% of BAK significantly reduced corneal nerve fiber density and aqueous tear production, and increased fluorescein staining after one week of treatment in animal studies; the phenomenon was more significant with 0.1% BAK [18]. The above pathophysiology explains the clinical findings of latanoprost-treated patients in the current study.
In our study, the BAK-induced ocular surface damage aggravated from 1-month to 4 months after treatment. Interestingly, older age was associated with a lesser decrement in Schirmer test values (+0.2 mm wetting per year, P = 0.01) and an increment in corneal staining (+0.01 per year, P = 0.005) after adjusting for multiple variables. Older patients tended to have lower Schirmer test values (β= −0.38, P < 0.001) and greater corneal staining (β= 0.139, P = 0.041) at their baseline visits. The decrement of the Schirmer test in older patients may not be as pronounced as it is in patients who start with normal values. This finding agrees with those of previous studies [25], which found the number of sub-basal nerves of healthy volunteers older than 60 years to be reduced to a similar level as that of dry eye groups. This occurred despite the fact that the density of superficial epithelial cells of healthy volunteers aged older than 60 years remained normal as compared to the dry eye group. Decreased sub-basal nerve density correlates to reduced tear function in dry eye patients [26]. Our current study indicates that irrespective of lacrimation, epithelial cell damage is greater in the older population exposed to BAK treatment.
To investigate tear film stability, we utilized NIKf-BUT, NIKav-BUT and the percentage of corneal area with tear film break-up times of less than 10 s to illustrate the length of the tear film break-up time and the size of tear film instability. Neither NIKf-BUT nor NIKav-BUT could distinguish the decline in tear film stability in the present study. A previous study that performed keratography in glaucoma patients found a mean NIKf-BUT value of 9.71 in patients with multiple topical antiglaucoma therapy, although more than 10 antiglaucoma medications with or without preservatives were included in the study [10]. Another study using keratography found the mean value of NIKf-BUT in glaucoma patients with three topical medications to be 5.45, compared to 8.40 in control patients [27]. However, to the best of our knowledge, this is the first study to evaluate NIK-BUT values before and after single topical antiglaucoma therapy.
The critical value of 10 s for the NIBUT has long been the standard, since it provides a sensitivity of 82% and specificity of 86% for OSD [14]. In the current study, we used a cut-off value of 10 s for unstable tear films and calculated the segments of cornea with NIK-BUT of less than 10 s. The size of unstable tear films gradually increased from 6.21% to 6.44% at 1-month (P = 0.813) and to 9.11% at 4-months (P = 0.042). Female sex correlated with increased tear film instability after treatment (P = 0.003), while the use of artificial tears alleviated the condition (P = 0.02). Our study agrees with many others, that have found female sex to be associated with a less stable tear film, since relatively low levels of serum androgen reduce lacrimal and meibomian gland function and diminish the anti-inflammatory effects on the ocular surface [28]. In addition, wearing makeup could also be a risk factor for tear film instability [29].
The present study found hyperemia scores to be significantly increased in both limbal and temporal regions at the 1-month visit; these returned near-baseline values at the 4-month visit. This finding agrees with that of a previous study that investigated changes in hyperemia scores for latanoprost, bimatoprost, and travoprost [30] and found a significant increase in hyperemia scores after treatment; they reached their peak 15 days later, started to decrease at 1-month, and returned to near-baseline levels at 4 months after therapy was initiated. Evaluation of the redness score using keratography has been demonstrated as an objective and reliable method for evaluating bulbar hyperemia [21]. Comparing bulbar redness scores at 1-month and baseline, the current study identified younger age and male sex to predispose to hyperemic changes of latanoprost treatment. The reason for the difference in hyperemia among patients is not exactly known. As noted previously, one reason could be the chronic administration of a preservative; however, this reasoning is speculative. Localized vessel dilation, caused by the release of nitric oxide, is thought to be another important mechanism for conjunctival hyperemia [31].
Instead of excluding cases with artificial tears, the current study also evaluated the use of lubricants for latanoprost-induced OSD in real-world clinical settings. Among eyes receiving concomitant lubricants, the Schirmer’s test and the parameters of tear film stability (NIKf-BUT, NIKav-BUT, and BUT10) showed marginal improvement; however, they possibly failed to reach significance due to small case numbers. However, among all eyes receiving BAK-latanoprost treatment, the use of lubricants alleviated tear production reduction and tear film instability after adjusting for possible confounders. The effect of lubricants on tear film break-up time appears to be equivocal in previous literature, probably due to differences in patients and methods used to measure tear film stability. Markoulli et al. demonstrated that the first and average keratographic breakup time measurements at baseline and at 5, 15, and 60 min after instillation of lubricants were not different in patients with healthy tear films [32]. Lanzini et al. found no significant differences in tear breakup times or Schirmer’s test values after using lubricants for one month in dry eye patients [33]. In agreement with our findings, Calvão-Santos et al. found a significant improvement in tear breakup times and Schirmer test value following 30 days of lubricants in computer users and contact lens users with dry eyes [34]. It is worth noting that using lubricants may break the vicious cycle of dry eye induced by BAK.
One of the limitations of this study was that we could not thoroughly evaluate ocular surface damages induced by BAK-latanoprost without prescribing artificial tears in cases with symptomatic dry eye. Due to health insurance regulations, all cases receiving artificial tears should have Schirmer’s test values of ≤5 mm. The benefit of lubricant use in cases with mild severity could not be evaluated in the present study. Another weakness of the present study is that we did not include patients with preservative-free latanoprost as a control group since the eye drop is not available in our country. The results in the current study may be optimistic given that, in real-world settings, many patients are using more than one drop containing BAK.
It is fundamental to understand the potential risks of any therapy we recommend, and weigh the benefit–risk ratio for our patients. In this study, we confirmed that BAK-latanoprost induced ocular surface damages in several aspects, including reduced tear secretion, impaired tear film stability, and epithelial toxicity. We also identified several risk factors susceptible to ocular surface damage and lubricants as the important protective factor. We recommend caution when prescribing preservative-containing medications and the use of early intervention in vulnerable cases. Further large-scale prospective multi-center studies are needed to validate our findings.
Change history
05 May 2022
This article has been retracted. Please see the Retraction Notice for more detail: https://doi.org/10.1007/s00417-022-05690-x
References
Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY (2014) Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology 121:2081–2090. https://doi.org/10.1016/j.ophtha.2014.05.013
Lowry EA, Chansangpetch S, Lin SC (2019) Use of topical intraocular pressure-lowering medications in the US population: results from the NHANES study 1999 to 2014. J Glaucoma 28:772–776. https://doi.org/10.1097/IJG.0000000000001315
Leung EW, Medeiros FA, Weinreb RN (2008) Prevalence of ocular surface disease in glaucoma patients (2008). J Glaucoma 17:350–355. https://doi.org/10.1097/IJG.0b013e31815c5f4f
Ghosh S, O'Hare F, Lamoureux E, Vajpayee RB, Crowston JG (2012) Prevalence of signs and symptoms of ocular surface disease in individuals treated and not treated with glaucoma medication. Clin Exp Ophthalmol 40:675–681. https://doi.org/10.1111/j.1442-9071.2012.02781.x
Brewitt H, Sistani F (2001) Dry eye disease: the scale of the problem. Surv Ophthalmol 45:S199–S202. https://doi.org/10.1016/s0039-6257(00)00202-2
Methodologies to diagnose and monitor dry eye disease: report of the Diagnostic Methodology Subcommittee of the International Dry Eye WorkShop (2007) Ocul Surf 5:108–152. https://doi.org/10.1016/s1542-0124(12)70083-6
Pflugfelder SC, Baudouin C (2011) Challenges in the clinical measurement of ocular surface disease in glaucoma patients. Clin Ophthalmol 5:1575–1583. https://doi.org/10.2147/OPTH.S24410
Schiffman RM, Christianson MD, Jacobsen G, Hirsch JD, Reis BL (2000) Reliability and validity of the ocular surface disease index. Arch Ophthalmol 118:615–621. https://doi.org/10.1001/archopht.118.5.615
Skalicky SE, Goldberg I, McCluskey P (2012) Ocular surface disease and quality of life in patients with glaucoma. Am J Ophthalmol 153 e2:1–9. https://doi.org/10.1016/j.ajo.2011.05.033
Perez-Bartolome F, Martinez-de-la-Casa JM, Arriola-Villalobos P, Fernandez-Perez C, Polo V, Garcia-Feijoo J (2017) Ocular surface disease in patients under topical treatment for glaucoma. Eur J Ophthalmol 27:694–704. https://doi.org/10.5301/ejo.5000977
Fechtner RD, Godfrey DG, Budenz D, Stewart JA, Stewart WC, Jasek MC (2010) Prevalence of ocular surface complaints in patients with glaucoma using topical intraocular pressure-lowering medications. Cornea 29:618–621. https://doi.org/10.1097/ICO.0b013e3181c325b2
Mathews PM, Ramulu PY, Friedman DS, Utine CA, Akpek EK (2013) Evaluation of ocular surface disease in patients with glaucoma. Ophthalmology 120:2241–2248. https://doi.org/10.1016/j.ophtha.2013.03.045
van Bijsterveld OP (1969) Diagnostic tests in the sicca syndrome. Arch Ophthalmol 82:10–14. https://doi.org/10.1001/archopht.1969.00990020012003
Mengher LS, Pandher KS, Bron AJ (1986) Non-invasive tear film break-up time: sensitivity and specificity. Acta Ophthalmol 64:441–444. https://doi.org/10.1111/j.1755-3768.1986.tb06950.x
Jiang Y, Ye H, Xu J, Lu Y (2014) Noninvasive Keratograph assessment of tear film break-up time and location in patients with age-related cataracts and dry eye syndrome. J Int Med Res 42:494–502. https://doi.org/10.1177/0300060513504701
Cvenkel B, Štunf S, Srebotnik Kirbiš I, Strojan Fležar M (2015) Symptoms and signs of ocular surface disease related to topical medication in patients with glaucoma. Clin Ophthalmol 9:625–631. https://doi.org/10.2147/OPTH.S81247
Baudouin C, Hamard P, Liang H, Creuzot-Garcher C, Bensoussan L, Brignole F (2004) Conjunctival epithelial cell expression of interleukins and inflammatory markers in glaucoma patients treated over the long term. Ophthalmology 111:2186–2192. https://doi.org/10.1016/j.ophtha.2004.06.023
Sarkar J, Chaudhary S, Namavari A, Ozturk O, Chang JH, Yco L, Sonawane S, Khanolkar V, Hallak J, Jain S (2012) Corneal neurotoxicity due to topical benzalkonium chloride. Invest Ophthalmol Vis Sci 53:1792–1802. https://doi.org/10.1167/iovs.11-8775
Pisella PJ, Pouliquen P, Baudouin C (2002) Prevalence of ocular symptoms and signs with preserved and preservative free glaucoma medication. Br J Ophthalmol 86:418–423. https://doi.org/10.1136/bjo.86.4.418
Ramli N, Supramaniam G, Samsudin A, Juana A, Zahari M, Choo MM (2015) Ocular surface disease in Glaucoma: effect of polypharmacy and preservatives. Optom Vis Sci 92:e222–e226. https://doi.org/10.1097/OPX.0000000000000542
Wu S, Hong J, Tian L, Cui X, Sun X, Xu J (2015) Assessment of bulbar redness with a newly developed Keratograph. Optom Vis Sci 92:892–899. https://doi.org/10.1097/OPX.0000000000000643
Bron AJ, Evans VE, Smith JA (2003) Grading of corneal and conjunctival staining in the context of other dry eye tests. Cornea 22:640–650. https://doi.org/10.1097/00003226-200310000-00008
Pauly A, Roubeix C, Liang H, Brignole-Baudouin F, Baudouin C (2012) In vitro and in vivo comparative toxicological study of a new preservative-free latanoprost formulation. Invest Ophthalmol Vis Sci 53:8172–8180. https://doi.org/10.1167/iovs.12-10766
Liang H, Baudouin C, Pauly A, Brignole-Baudouin F (2008) Conjunctival and corneal reactions in rabbits following short- and repeated exposure to preservative-free tafluprost, commercially available latanoprost and 0.02% benzalkonium chloride. Br J Ophthalmol 92:1275–1582. https://doi.org/10.1136/bjo.2008.138768
Benitez del Castillo JM, Wasfy MA, Fernandez C, Garcia-Sanchez J (2004) An in vivo confocal masked study on corneal epithelium and subbasal nerves in patients with dry eye. Invest Ophthalmol Vis Sci 45:3030–3035. https://doi.org/10.1167/iovs.04-0251
Cruzat A, Qazi Y, Hamrah P (2017) In vivo confocal microscopy of corneal nerves in health and disease. Ocul Surf 15:15–47. https://doi.org/10.1016/j.jtos.2016.09.004
Portela RC, Fares NT, Machado LF, São Leão AF, de Freitas D, Paranhos A Jr, Prata TS, Gracitelli CPB (2008) Evaluation of ocular surface disease in patients with Glaucoma: clinical parameters, self-report assessment and Keratograph analysis. J Glaucoma 27:794–801. https://doi.org/10.1097/IJG.0000000000001007
Truong S, Cole N, Stapleton F, Golebiowski B (2014) Sex hormones and the dry eye. Clin Exp Optom 97:324–336. https://doi.org/10.1111/cxo.12147
Malik A, Claoue C (2012) Transport and interaction of cosmetic product material within the ocular surface: beauty and the beastly symptoms of toxic tears. Cont Lens Anterior Eye 35:247–259. https://doi.org/10.1016/j.clae.2012.07.005
Arcieri ES, Santana A, Rocha FN, Guapo GL, Costa VP (2005) Blood-aqueous barrier changes after the use of prostaglandin analogues in patients with pseudophakia and aphakia: a 6-month randomized trial. Arch Ophthalmol 123:186–192. https://doi.org/10.1001/archopht.123.2.186
Alm A (1998) Prostaglandin derivates as ocular hypotensive agents. Prog Retin Eye Res 17:291–312. https://doi.org/10.1016/s1350-9462(97)00003-7
Markoulli M, Sobbizadeh A, Tan J, Briggs N, Coroneo M (2018) The effect of optive and optive advanced artificial tears on the healthy tear film. Curr Eye Res 43:588–594. https://doi.org/10.1080/02713683.2018.1433860
Lanzini M, Curcio C, Colabelli-Gisoldi RA, Mastropasqua A, Calienno R, Agnifili L, Nubile M, Mastropasqua L (2015) In vivo and impression cytology study on the effect of compatible solutes eye drops on the ocular surface epithelial cell quality in dry eye patients. Mediat Inflamm 351424:2015. https://doi.org/10.1155/2015/351424
Calvao-Santos G, Borges C, Nunes S, Salgado-Borges J, Duarte L (2011) Efficacy of 3 different artificial tears for the treatment of dry eye in frequent computer users and/or contact lens users. Eur J Ophthalmol 21:538–544. https://doi.org/10.5301/EJO.2011.6324
Acknowledgements
The authors acknowledge statistical assistance provided by the Center of Statistical Consultation and Research in the Department of Medical Research, National Taiwan University Hospital.
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
All procedures used in this study were approved by the Ethics Review Board of the National Taiwan University Hospital and adhered to the tenets of the Declaration of Helsinki.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article has been retracted. Please see the retraction notice for more detail:https://doi.org/10.1007/s00417-022-05690-x
About this article
Cite this article
Su, CC., Lee, YC. & Lee, P.R.C. RETRACTED ARTICLE: Assessment of ocular surface disease in glaucoma patients with benzalkonium chloride-preserved latanoprost eye drops: a short-term longitudinal study. Graefes Arch Clin Exp Ophthalmol 259, 1243–1251 (2021). https://doi.org/10.1007/s00417-020-05067-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-020-05067-y