Abstract
Background
To investigate the incidence of developing posterior vitreous detachment (PVD) in children after congenital cataract surgery.
Methods
This is a prospective study which recruited 131 children with congenital cataracts who underwent cataract surgery between June 1, 2015, and September 1, 2018. The patients were divided into two groups depending on their post-operation phakic status (with or without IOL implantation). Infants aged from 6 to 12 months from two groups were analyzed as subgroups, respectively. B-scan ultrasonography was performed before the procedure and at 1, 3, 6, 9, and 12-month follow-ups, respectively, after the operation.
Results
Of the 131 eyes included in the analyses, 74 were aphakic, and 57 were pseudophakic after surgery. The postoperative rate of PVD in all analyzed eyes was 6.9% (9 of 131 eyes). After 12 months, PVD was significantly more prevalent in the eyes that underwent cataract surgery with IOL implantation (10.5%, 6 of 57 eyes) compared to the eyes without IOL implantation (4.1%, 1 of 74 eyes, P < 0.05); however, the eyes in the aphakic group were significantly younger than the eyes in the pseudophakic group, while the mean axial length (AL) of the pseudophakic eyes (21.11 ± 2.07 mm) was significantly higher than that of the aphakic eyes (18.93 ± 1.86 mm) (P < 0.01). In patients between the ages of 6 and 12 months of age from the two groups, the AL of patients with IOL implantation continued to be significantly increased compared to the group without IOL implantation (20.44 ± 1.68 mm vs. 19.78 ± 1.52 mm, P < 0.01). At the follow-up appointments, two patients with PVD were observed among the 14 eyes that had undergone cataract surgery with IOL implantation, while one eye was observed to have developed PVD among the 15 eyes without IOL implantation.
Conclusions
PVD occurs with greater frequency after congenital cataract surgery, particularly in eyes that have undergone IOL implantation. We suggest that PVD should be carefully monitored in children after congenital cataract surgery to avoid subsequent ocular pathologies such as retinal detachment. Future studies are needed to determine other potential risk factors that have not been as thoroughly explored, as opposed to better-known factors such as older age, longer axial length, and IOL implantation.

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Retinal detachment (RD) after cataract extraction is a serious vision-threatening surgical complication. In adults, the risk of RD is 7.5 to 8.7 times higher after cataract surgery. Posterior vitreous detachment (PVD) is a known risk factor of RD [1, 2], and the risk of RD after cataract surgery is significantly higher in the patients that develop postoperative PVD (7.4%) compared with normal patients (0.30%). In children, the risk of RD after cataract surgery has been reported to be from 0.57 to 7% [3,4,5,6,7]; however, the incidence of PVD has not been determined after congenital cataract surgery.
PVD is defined as a separation of the posterior vitreous cortex from the surface of the retina. The use of B-scan ultrasonography is fundamental in diagnosing PVD [8, 9], which is known to follow vitreous gel liquefaction and weakening of vitreoretinal adhesion [10]. When using B-scan ultrasonography, a major sign of gel liquefaction is vitreous opacity. In some cases, such physiological changes may ultimately result in retinal tears, vitreous hemorrhages, or retinal detachment [11].
Unlike adult cataract surgery, anterior vitrectomy is routinely performed in congenital cataract surgery in order to prevent posterior capsule opacification in children. Some reports suggest that children with congenital cataracts are at a higher risk of developing retinal detachment than individuals with senile cataracts [12,13,14]. At this point in time, the development of PVD after congenital cataract treatment is not fully understood. Thus, the aim of this study is to investigate changes in the vitreous body after congenital cataract surgery and to observe its association with postoperative phakic status. To the best of our knowledge, no similar study has been reported on the topic.
Patients and methods
This prospective observational case series included infants and children with congenital cataract who underwent cataract extraction in the Eye Hospital of Wenzhou Medical University, Hangzhou, China. All the surgeries were performed under general anesthesia by the same surgeon (Z.Y.E) using the Accurus with the venturi vacuum system (Alcon Laboratories, Inc.); the cut rate was 2000 per minute, and the vacuum was 350 mm Hg. Two 1.0 mm paracentesis were created in the temporal and nasal clear cornea using a diamond knife; for those eyes planned IOL implantation, a 2.2-mm superior scleral tunnel incision was created. For patients older than 2 years, we performed lens aspiration after anterior continuous curvilinear capsulorhexis, followed by posterior continuouscurvilinear capsulorhexis and limited anterior vitrectomy with a 23-gauge vitrector and 23-guage irrigating cannula via two cornea paracentesis. While in patients younger than 2 years old, anterior and posterior vitrectorhexis was performed instead of manual capsulorhexis. The diameter of anterior capsule opening is about 5 mm, and the posterior capsule opening is about 3.5 mm. Then, a posterior chamber IOL was implanted into the capsular bag. Then, the main incision was closed with a 10–0 nylon sutures. The patients were divided into two groups depending on their post-operation phakic status (with or without IOL implantation); the selection was based on age, corneal diameter, and axial length, as well as the parents’ opinions. Infants 6 to 12 months of age from these two groups were then analyzed as subgroups, respectively.
Exclusion criteria included a history of ocular trauma, a history of intraocular surgery, preoperative glaucoma, a history of maternal rubella syndrome, chronic anterior uveitis, persistent fetal vasculature, ocular anomalies associated with an increased risk of glaucoma, and inability to complete examinations. Only the right eyes of patients were enrolled when diagnosed with binocular congenital cataract. All patients’ parents provided informed consent. The study followed the tenets of the Declaration of Helsinki.
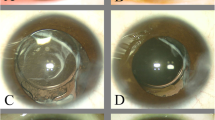
All of the patients underwent standard ophthalmic examinations by the same physician before surgery and in each subsequent follow-up, which included visual acuity and slit-lamp examination. Axial length (AL) and anterior chamber depth were measured via a contact A-scan (Axis nano, Quantel Medical, French) after intranasal anesthesia and topical anesthesia were administered. B-scan ultrasonography was performed by trained technicians using the Cinescan S device (Quantel Medical) with a 10 MHz probe. The procedure was performed by a standard contact method using high to maximum gain to detect and localize ultrasonographic PVD. Kinetic examination of the 4 standardized views was performed using directed movement of the patient’s globe. The B-scan images were evaluated by one experienced ophthalmologist and one trained technician independently. B-scans were performed before surgery and at 1, 3, 6, 9, and 12 months after the operation. Vitreous opacity was diagnosed by the presence of light spots or light masses with varying echo intensity in the vitreous body, which appear to float with the rotation of the eye. PVD was defined as a low reflective mobile echogenic membrane, or the presence of a ring in the peripapillary vitreous cortex partially, or completely detached from the retina. [15]
The data were analyzed using SPSS 23.0 (IBM co., America). A one-way ANOVA test or Mann-Whitney U test was employed to compare the means between the pseudophakic group and the aphakic group, depending on the normality of the analyzed variables. Pearson chi-square test was used to compare the constituent ratio between the two groups. All comparisons were considered statistically significant when P < 0.05.
Results
This study enrolled 131 eyes of 131 patients. The demographic characteristics of the included patients are presented in Table 1. Fifty-seven eyes underwent cataract removal with IOL implantation, while 74 eyes underwent extraction without IOL implantation. The median age was 36 months (ranging from 6 to 72 months) in the pseudophakic group, and the mean AL was 21.11 ± 2.07 mm. The median age was 4 months (ranging from 1.5 to 12 months) in the aphakic group, and the mean AL was 18.93 ± 1.86 mm.
Vitreous opacity was detected by B-scan in the pseudophakic group and was observed in 10 patients (17.5%) at 1 month, 19 patients (33.3%) at 3 months, 25 patients (43.9%) at 6 months, 33 patients (57.9%) at 9 months, and 36 patients (63.2%) at 1 year after surgery. At 1 month, 4 patients (7%) were diagnosed with PVD, while the incidence of PVD did not change until nine months. At 9 months, the incidence of PVD increases to 5 patients (8.8%), which further increased to 6 patients (10.5%) at 1 year (Fig. 1a).
In 74 patients that remained aphakic, one patient had PVD at 1 month (1.4%), a second at 6 months (2.7%), and a third at 1 year (4.1%). Examinations showed that 2 patients (2.7%) had vitreous opacity at the 1-month visit, 8 patients (10.8%) at the 3-month visit, 13 patients (17.6%) after 6 months, and 15 patients (20.2%) after 9 months. Overall, 26 patients (35.1%) develop vitreous opacity during the year-long follow-up period (Fig. 1b). The constituent ratios between the two groups were significantly different. (P < 0.01)
For age-matching subgroups, patients between the ages of 6 and 12 months (including 6 months and 12 months of age) in both groups are selected and analyzed (Fig. 2). Of these patients, 15 eyes underwent cataract extraction with IOL implantation and 14 eyes without IOL implantation. Among the patients with IOL implantation, eight were male and six were female. The median age was 9.5 months old (the interquartile range: 4 months), and the mean AL was 20.44 ± 1.68 mm. Subsequent B-scan follow through was normal in two patients and showed PVD in two patients (14.3%), who were observed at 1-month and 1-year postoperative examination, respectively. The incidence of vitreous opacity increased at each examination interval in postoperative follow-up visits. At 1 month, the incidence was 14.3% (2 cases), and at 3 months, the incidence was 42.9% (6 cases). The incidence continued to increase to 57.1% (8 cases) at 6 months, 71.4% (10 cases) at 9 months, and 71.4% (10 cases) at 12 months. In the group of patients without IOL implantation, 10 were male, and 5 were female. The median age was 7 months old (the interquartile range: 4 months), and the mean AL was 19.78 ± 1.52 mm. At the follow-up examination, one patient was diagnosed with PVD in the following 1-year interval. Nine cases that received treatment had a clear vitreous body. The incidences of vitreous opacity are 0% (0 cases), 6.7% (1 case), 20.0% (3 cases), 20.0% (3 cases), and 33.3% (5 cases) at 1, 3, 6, 9, and 12 months, respectively, after surgery.
There was no significant difference between the two groups in the age (P > 0.05), but a significant difference was found in the AL (P < 0.01). The constituent ratios between the two groups were significantly different (P < 0.01).
The postoperative PVD rate is 6.9% (9 of 131 eyes), with none resulting retinal tears or RD after the development of PVD that were also detected (Fig. 3).
Discussion
In this study, we investigated the occurrence of PVD in congenital cataract patients. Among the data, it was found that the postoperative rate of PVD was 6.9% (9 of 131 eyes). These data suggest a dynamic development process as the incidence of vitreous opacity and PVD increase gradually with time after the initial postoperative examination. To our knowledge, the present study is the first prospective case series investigating PVD after congenital cataract surgery.
In studies involving adults, retinal damage such as RD was related to the development of PVD. Bond-Taylor et al. reported that in adult patients with PVD, the incidence of retinal tears was 14.5%, and the incidence of vitreous and/or retinal hemorrhage was 22.7% [16]. Agarkar et.al observed that retinal breaks, associated with posterior vitreous detachment, were the most common cause of RD after cataract surgery, although there has not been any in-depth study on PVD [17].
The prevalence of PVD has been investigated in adults while taking age, different eye surgeries, and other risk factors into account. Several studies have shown that the prevalence of PVD in the population over 65 years old was 65% [10]. Previous studies investigating cataract surgery and other surgical interventions also suggest that the procedure accelerates the development of PVD. As Mirshahi et al. reported, partial and complete PVD had an incidence of 58.6% within 1 year after uneventful phacoemulsification using biomicroscope and ultrasound [18]. Hikichi et al. observed a PVD incidence of 30.0% within 3 years after phacoemulsification operation in 575 eyes of 419 patients [10, 19]. There is also evidence that liquefaction of vitreous is a physiological process which begins between 4 years of age and teenage years [10], where 20% of the total vitreous body underwent syneresis, and the rate increased to 50% for those over 70 years old [10, 20].
Within this study, it was documented that PVD occurred more frequently in eyes that have undergone cataract surgery with IOL implantation (10.5%, 6 of 57 eyes), compared to eyes without IOL implantation (4.1%, 3 of 74 eyes, P < 0.01). The rate of the vitreous opacity showed this same trend (63.2%, 36 of 57 eyes vs. 29%, 26 of 74 eyes, P < 0.01), while previous studies have suggested that vitreous opacity is usually considered as the preceding stage of PVD [10]. Our data indicates that choosing to implant or not implant an IOL during the congenital cataract surgery significantly affects the rate of PVD and vitreous opacity after surgery. Accordingly, we propose some hypotheses based on these differences of outcome. First and foremost, in pseudophakic eyes, postoperative continuous cortical hyperplasia may continuously spill from the unsealed capsule into the vitreous cavity, which may promote vitreous liquefaction, further leading to PVD. In aphakic eyes, the capsular bag of most patients can be healed into a sealed capsule, and no cortex is involved in the process of vitreous liquefaction [21]. In terms of the proportion of vitreous opacity, this is also illustrated. Certainly, further research is needed. Secondly, the focusing of light by the intraocular lens may result in an increase in the light-induced reactive oxygen species after surgery which can speed up the occurrence of vitreous liquefaction by changing collagen composition and destroying enzymatic collagen by influencing enzyme activity [10]. Thirdly, AL and age were the most important two factors in designing the operation strategy as the mean AL was remarkably longer and the mean age was significantly older in the patients with IOL implantation compared to those without IOL implantation. As AL continues to grow in children as they age, we made subgroups in order to analyze the patients aged 6–12 months, whose average age was similar in the aphakic and pseudophakic groups (8.90 ± 1.19 m vs 8.75 ± 2.30 m, P > 0.05). We also observed the same trend of B-scan results in the two age-matched subgroups. Within this study, the mean AL of the patients with IOL implantation was still longer than the other group who did not undergo IOL implantation (20.44 ± 1.68 mm vs. 19.78 ± 1.52 mm, P < 0.01). We speculated that older children with longer AL may have stronger tractional forces enhancing PVD. Similarly, older age at surgery may contribute to PVD considering the development of vitreous liquefaction. Consider that during late prenatal and early postnatal stages, the vitreous body is only made of the remnants of the hyaloid artery [22]. Hyaluronan (HA), a highly hydrophilic glycosaminoglycan (GAG), synthesis begins after birth, which is a type of age-related biochemical alteration resulting in vitreous liquefaction [22, 23]. It has been reported that liquid vitreous begins to appear, albeit in small quantities, during the first 5 years of life [10]. There are some physiological processes of PVD which are also important to consider here, namely gel liquefaction and vitreoretinal dehiscence, which cause the liquefied vitreous to enter into the subhyaloid space with subsequent dissection of remaining adhesions between the posterior vitreous cortex and the inner limiting membrane with eye movements [10, 24,25,26,27]. The anterior movements of the vitreous after removal of the lens and anterior vitreous can tract the posterior vitreous membrane [18, 25]. This mechanism suggests an effect of surgical mechanical forces on the vitreous structure and thus explains the increased incidence of PVD and vitreous opacity after operation; however, from this point of view, after anterior vitrectomy, the residual vitreous body moves forward as a whole, while the complex of capsule intraocular lens is used as a barrier to prevent the vitreous from moving forward. Contrarily, in aphakic eyes, the vitreous body is directly connected with the aqueous humor, which makes the forward shift more obvious. This is contradictory to the results and remains to be further studied.
In our study, PVDs were first spotted 1 month after surgery, which indicate that mechanical injury may play a role in the formation of PVD. Thus, we suggest that intraocular pressure fluctuations, which serve as an indicator of mechanical injury, should be carefully monitored throughout surgery.
This study has some limitations. PVD can be divided into complete PVD and partial PVD according to the adherence of retina to the vitreous base [8, 23, 28]. Since the b-mode ultrasound examination in children was performed under anesthesia, it was impossible to require children to carry out active cooperation like adults. In addition, irregular eye movements may occur in this state. So, even though B-scan was performed by our experienced doctors, they could not make sure in determining complete or partial PVD for every child at every examination. Nevertheless, the sample size of our study is small, and the follow-up period is only one year. A longer follow-up and a larger number of patients could facilitate the evaluation of potential risk factors and determine the relationship between the age and the incidence. But as the choice of operation between the two groups is largely based on the axial length, it is hard to have the same o axial length between the two groups. Regardless of these points, this is the first study to investigate the incidence rate of PVD after congenital cataract surgery.
In the present study, PVD was observed during follow-up of congenital cataract surgery, in a higher incidence in the group with IOL implantation—which can be related to surgical technique or to a difference of preoperative parameters as axial length. We suggest that PVD should be carefully monitored in children after congenital cataract surgery to avoid subsequent ocular pathologies such as retinal detachment. Future studies are needed to determine other potential risk factors that have not been as thoroughly explored, as opposed to better-known factors such as older age, longer axial length, and IOL implantation.
Data Availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request
References
Norregaard JC, Thoning H, Andersen TF, Bernthpetersen P, Javitt JC, Anderson GF (1996) Risk of retinal detachment following cataract extraction: results from the International Cataract Surgery Outcomes Study. Am J Ophthalmol 123:689–693
Boberg-Ans G, Henning V, Villumsen J, La CM (2009) Longterm incidence of rhegmatogenous retinal detachment and survival in a defined population undergoing standardized phacoemulsification surgery. Acta Ophthalmol 84:613–618
Haargaard B, Andersen EW, Oudin A, Poulsen G, Wohlfahrt J, Cour M et al (2014) Risk of retinal detachment after pediatric cataract surgery. https://doi.org/10.1167/iovs.14-13996
Chrousos GA, Parks MM, O’Neill JF (1984) Incidence of chronic glaucoma, retinal detachment and secondary membrane surgery in pediatric aphakic patients. Ophthalmology 91:1238–1241
Keech RV, Tongue AC, Scott WE (1989) Complications after surgery for congenital and infantile cataracts. Am J Ophthalmol 108:136–141
Hing S, Speedwell L, Taylor D (1990) Lens surgery in infancy and childhood. Br J Ophthalmol 74:73
Chak M, Wade A, Rahi JS (2006) Long-term visual acuity and its predictors after surgery for congenital cataract: findings of the British congenital cataract study. Investig Ophthalmol Vis Sci 47:4262–4269. https://doi.org/10.1167/iovs.05-1160
Abdolrahimzadeh S, Piraino DC, Scavella V, Abdolrahimzadeh B, Cruciani F, Gharbiya M et al (2016) Spectral domain optical coherence tomography and B-scan ultrasonography in the evaluation of retinal tears in acute, incomplete posterior vitreous detachment. BMC Ophthalmol 16:1–9. https://doi.org/10.1186/s12886-016-0242-0
Lorenzo-Carrero J, Perez-Flores I, Cid-Galano M, Fernandez-Fernandez M, Heras-Raposo F, Vazquez-Nuñez R et al (2009) B-Scan ultrasonography to screen for retinal tears in acute symptomatic age-related posterior vitreous detachment. Ophthalmology 116:94–99. https://doi.org/10.1016/j.ophtha.2008.08.040
Foulds WS (2014) Is your vitreous really necessary? Vitr Heal Dis xxi–xxviii. https://doi.org/10.1007/978-1-4939-1086-1
Richardson PSR, Benson MT, Kirkby GR (1999) The posterior vitreous detachment clinic: do new retinal breaks develop in the six weeks following an isolated symptomatic posterior vitreous detachment? Eye 13(Pt 2):237
Nuzzi R, Lavia C, Spinetta R (2017) Paediatric retinal detachment: a review. Int J Ophthalmol. https://doi.org/10.18240/ijo.2017.10.18
Kanski JJ, Elkington AR, Daniel R (1974) Retinal detachment after congenital cataract surgery. Br J Ophthalmol 58:92–95
Koç H, Koçak İ, Bozkurt S (2015) Retinal detachment after vitrectomy performed for dropped nucleus following cataract surgery: a retrospective case series. Int J Clin Exp Med 8:4591–4595
Gavrilov JC, Gaujoux T, Sellam M, Laroche L, Borderie V (2011) Occurrence of posterior vitreous detachment after femtosecond laser in situ keratomileusis: ultrasound evaluation. J Cataract Refract Surg 37:1300–1304. https://doi.org/10.1016/j.jcrs.2011.01.022
Bond-Taylor M, Jakobsson G, Zetterberg M (2017) Posterior vitreous detachment - prevalence of and risk factors for retinal tears. Clin Ophthalmol 11:1689–1695. https://doi.org/10.2147/OPTH.S143898
Agarkar S, Gokhale VV, Raman R, Bhende M, Swaminathan G, Jain M (2017) Incidence, risk factors, and outcomes of retinal detachment after pediatric cataract surgery. Ophthalmology 1–7. https://doi.org/10.1016/j.ophtha.2017.07.003
Mirshahi A, Hoehn F, Lorenz K, Hattenbach LO (2009) Incidence of posterior vitreous detachment after cataract surgery. J Cataract Refract Surg 35:987–991. https://doi.org/10.1016/j.jcrs.2009.02.016
Hikichi T (2012) Time course of development of posterior vitreous detachments after phacoemulsification surgery. Ophthalmology 119:2102–2107. https://doi.org/10.1016/j.ophtha.2012.03.050
Foos RY, Wheeler NC (1982) Vitreoretinal juncture. Synchysis senilis and posterior vitreous detachment. Ophthalmology 89:1502–1512
Jirásková N (2001) Operace katarakty u dĕtí [Cataract surgery in children]. Cesk Slov Oftalmol 57(2):127–31
Sebag J (2010) Vitreous anatomy, aging, and anomalous posterior vitreous detachment. Encycl Eye 13(2):307–315
Johnson MW (2010) Posterior vitreous detachment: evolution and complications of its early stages. Am J Ophthalmol 149:371–382.e1
Ivastinovic D, Schwab C, Borkenstein A, Lackner EM, Wedrich A, Velikay-Parel M (2012) Evolution of early changes at the vitreoretinal interface after cataract surgery determined by optical coherence tomography and ultrasonography. Am J Ophthalmol 153:705–709. https://doi.org/10.1016/j.ajo.2011.09.009
Hilford D, Hilford M, Mathew A, Polkinghorne PJ (2009) Posterior vitreous detachment following cataract surgery. Eye 23:1388–1392. https://doi.org/10.1038/eye.2008.273
Lorenzo Carrero J (2012) Incomplete posterior vitreous detachment: prevalence and clinical relevance. Am J Ophthalmol 153:497–503. https://doi.org/10.1016/j.ajo.2011.08.036
Kishi S (2016) Vitreous anatomy and the vitreomacular correlation. Jpn J Ophthalmol 60:239–273. https://doi.org/10.1007/s10384-016-0447-z
Goldman DR (2018) Stages of posterior vitreous detachment. In: Atlas of Retinal OCT: Optical Coherence Tomography. Elsevier, pp 159–161
Funding
This study was supported by research grants from the Zhejiang Provincial Natural Science Foundation of China (Grant No.LY18H120008), the National Natural Science Foundation of China (Grant No.81870680), the Zhejiang Provincial Key Research and Development Program (Grant No.2018C03012), and the Innovation Discipline of Zhejiang Province (lens disease in children) (Grant No.2016cxxk1]. The funding organization had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Contributions
PC designed the study and was a major contributor in writing the manuscript. ZF was a major contributor in writing the manuscript and analyzed and interpreted the data. JW analyzed and interpreted the patient data. YZ made substantial contributions to the design of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval and consent to participate
Informed consents to participate in the study were obtained from participants’ parent or legal guardian.
Consent for publication
For all manuscripts that include details, images, or videos relating to an individual person, written informed consent for the publication of these details was obtained from their parent or legal guardian.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 2347 kb)
Rights and permissions
About this article
Cite this article
Zhang, F., Chang, P., Zhao, Y. et al. Incidence of posterior vitreous detachment after congenital cataract surgery: an ultrasound evaluation. Graefes Arch Clin Exp Ophthalmol 259, 1045–1051 (2021). https://doi.org/10.1007/s00417-020-04997-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-020-04997-x