Abstract
Purpose
To evaluate the correlations between anatomical and functional changes in idiopathic macular hole (IMH) surgery in long-term follow-up.
Methods
This is a prospective, interventional single centre case series. The final sample is formed by 14 eyes of 14 patients who had undergone IMH surgery in our institution between 2005 and 2009 and were still followed up in 2019. Reported data were pre- and post-operative best-corrected visual acuity (BCVA), retinal sensitivity and fixation stability values on MP-1 and structural macular features on spectral domain optical coherence tomography. Optical coherence tomography angiography (OCTA) was utilized to assess microvascular characteristics at the final visit. Only patients with a successful MH closure were enrolled, excluding eyes affected by other relevant pathologies.
Results
Mean BCVA improvement was significant after surgery (t test, p value < 0.001) and presented a slight, not statistically significant raise, between the post-operative and long-term follow-up. Differently, mean retinal sensibility (dB) showed a highly statistically significant difference between pre-operative and post-operative (t test, p value = .002) and post-operative and last follow-up (p value < 0.001). In the long-term follow-up, subjects having integrity of the inner segment/outer segment (IS/OS) layer showed no statistically significant difference in BCVA compared with subjects with IS/OS discontinuity (t test, p value = 0.72). OCTA parameters of the operated eye showed no statistical significance compared with the fellow eye.
Conclusions
In successfully closed MHs, retinal sensibility measured by microperimetry significatively increases after a long follow-up period even when BCVA remains stable or raises slightly. Vessel density organization tends to be quantitatively similar to fellow eye several years after surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Idiopathic macular hole (IMH) is a relevant vitreomacular interface disorder causing metamorphopsia and poor central vision [1]. IV-stage MH, according to Gass [2], appears as a full-thickness round defect with diameter > 400 μm with a complete posterior vitreous detachment [3]. International Vitreomacular Traction Study (IVTS) Classification divides MHs by dimensions in three types: small ≤ 250 μm, medium between 250 and 400 μm and large ≥ 400 μm [4]. MH is a vitreomacular interface (VMI) disorder involving posterior vitreous cortex, inner limiting membrane (ILM) and the interposing extracellular matrix [5]. Anatomical variants such as high myopia/hypermetropia, trauma and previous retinal surgery have been described as proven causes of the increased risk for VMI disorders [6], although IMH are the most frequent [7]. The aim of the surgery is to release traction forces on the retina consenting anatomic restoration and BCVA improvement [8]. Via pars plana vitrectomy (VPP) has been introduced as a therapy to treat full-thickness MH that normally, if untreated, has arduous visual recovery since spontaneous closure [9]. The ILM retinal peeling was introduced by Eckardt in 1997 [10]. The use of this technique has improved MH healing rate and visual outcomes compared with the surgery with only vitrectomy and gas tamponade [11].
Microperimetry is a rapid, safe and non-invasive psycho-physical method that allows to determine retinal sensitivity [12]; it permits to detect an exact correlation between macular diseases and corresponding functional alterations [13]. Microperimetry has been defined as more sensitive than visual acuity, contrast sensitivity and colour vision in determining macular function after MH surgery [14, 15].
OCT angiography (OCTA) is a new imaging technique that uses motion contrast to visualize the retinal microcirculation quickly and non-invasively [16]. OCTA advent could permit a better comprehension of MH pathogenesis and healing process [17].
The purpose of this study is to evaluate retinal anatomical and functional changes in patients who underwent successful surgery for MH with a follow-up of at least 9 years.
Patients and methods
This prospective, interventional single centre case series was conducted at the Eye Clinic, Polytechnic University of Marche, Ancona, Italy. Nineteen eyes from 19 patients with large IV-stage FTMH (full-thickness macular hole) [2, 4] were initially included. Study consent was obtained from all the participants. The procedures of this study were in accordance with the Declaration of Helsinki. Written consent was obtained from all individual participants included in this paper, and it was approved by the local Institutional Review Board (IRB). All the patients underwent via pars plana 25-G vitrectomy with ILM peeling and gas tamponade. No vital dye was utilized for staining the ILM and octafluoropropane (C3F8) was employed as gas tamponade. The cataract phacoemulsification was carried out in all enrolled patients. Data were collected from 2005 to 2019 and all the patients had a minimum follow-up period of 9 years. Exclusion criteria were the following: (1) the presence of a refractive error of more than 5 diopters in the affected eye; (2) history of amblyopia, age-related macular degeneration, diabetic retinopathy or retinal vascular occlusion; (3) history of intraocular surgery other than uncomplicated cataract surgery. During the long follow-up period, the original patient cohort dimension has decreased: one eye suffered from retinal detachment few years after macular surgery and four patients were lost to follow-up over the years. Ultimately, fourteen eyes (78.9%) were enrolled and all of those presented a successful surgery (closure of the hole).
All the patients underwent a complete slit lamp ophthalmic evaluation, LogMAR BCVA assessment and Goldmann applanation tonometry. Pre-operative (1 week before surgery), post-operative (6 months after surgery) and long-term (9–14 years, mean 12 years) clinical evaluations were performed to every patient.
All the OCT images were collected using the Heidelberg Spectralis system (Heidelberg Engineering, Heidelberg, Germany) and analysed with Heidelberg Eye Explorer software. A certified examiner (AR) performed all the OCT scans. A radial 20 degree, 6 line scans were averaged to measure the basal diameter of the hole. Continuity of inner segment/outer segment (IS/OS) layers was evaluated using grayscale OCT images acquired in all the 6 scansions. IS/OS layers were defined continuous or disrupted.
The MP-1 microperimeter (Nidek Technologies, Tokyo, Japan) was used. Pupils were dilated using 1% tropicamide and a reference frame was obtained using the integrated infrared camera. Patients underwent a brief period of training and had 5-min adaptation before starting the examination. They were asked to fix the red cross of 2 degrees at the centre of the visual field. Eye movements were tracked during the acquisition. A double-staircase 4-2 strategy was used during the test with a white background illumination of 4 apostilbs (asb) and a light stimulus set at 10 dB with a 200-ms stimulus duration. Then, a grid of 45 stimuli with a Goldmann III stimulus size was projected at the centre of the 8 degrees of the visual field with 1 s distance between stimuli. Parameters collected included retinal mean sensitivity and retinal medium defect. Fixation stability was calculated as the percentage of fixation points within the 2- and 4-degree diameter circle. We considered and calculated scotomatous defects as relative or absolute. Relative scotoma was considered a specific retinal location where sensitivity values fell below the normal population 95% confidence interval. While, if the brightest possible stimulus was not responded to, the locus was designated as absolute scotoma [18]. An accurate calibration was conducted before the examinations and all the tests were performed by the same experienced ophthalmologist (AF).
AngioVue system (Optovue RTVue XR Avanti; Optovue, Inc., Fremont, CA, USA) was used to acquire OCTA images at the last follow-up. Scans collected in the macula were 4.5 × 4.5 mm. Parameters collected, analysed automatically by the AngioVue OCTA software, included the following: whole image vessel density (VD), foveal VD and volumetric posterior pole analysis (foveal, parafoveal and perifoveal volume). All the eyes with FTMH were compared with the fellow eye, none of which developed any retinal pathology. We excluded from the analysis low-quality images due to blinking artefacts or eye motion.
Statistical Package for Social Sciences (version 17.0, SPSS Inc.) was used for statistical analysis. Normal distribution of data was checked before performing mean and standard deviation tests. Two-tailed t test was used for continuous variables. Non-parametric Wilcoxon test was used for not normally distributed data (BCVA, IS/OS layer interruption); p values < 0.05 were considered significant. Data obtained are summarized in Tables 1 and 2.
Results
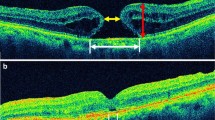
A total of 14 patients were included in the analysis. Mean patients age was 51 ± 8.49 years (median age 70); 6 (43%) were males and 8 (57%) were females. Mean follow-up period was 12.27 ± 2.65 years (95% CI 9.49 to 13.5). MH mean diameter was 424.64 ± 71.07 μm (95% CI 71.07 to 424.64) and 6 (43%) FTMH out of 14 presented a continuity of IS/OS layer (Fig. 1).
Spectral domain optical coherence tomography (SD-OCT) pre-operative scan is on the top, showing a large IV-stage full-thickness macular hole (FTMH); successful FTMH surgery leads to the closure of the hole (middle). OCT scan after 10 years of follow-up is shown on the bottom with evident retinal pigmented epithelium (RPE) disruption
Mean BCVA (LogMAR) was 0.72 (range 0.55–0.89; median 0.5) (20/100 Snellen equivalent) pre-operatively, 0.20 (range 0.03–0.37; median 0.1) (20/32, 3 lines of improvement using ETDRS letter scores) post-operatively and 0.18 (range 0.06–0.30; median 0.2) (20/30, 3–4 lines of improvement using ETDRS letter scores) at the last follow-up. Differences in BCVA between pre-operative and post-operative and pre-operative and last follow-up visit were statistically significant (t test, p value < 0.001).
Mean retinal sensitivity (dB) was 10.60 ± 1.64 (95% CI 9.50 to 11.70) pre-operatively, 14.06 ± 2.85 (95% CI 12.15 to 15.98) post-operatively and 18.00 ± 1.92 (95% CI 16.71 to 19.29) at the last follow-up with a highly statistically significant difference between pre-operative and post-operative (t test, p value = 0.002), pre-operative and last follow-up (t test, p value < 0.001), post-operative and last follow-up data (t test, p value < 0.001) (Fig. 2).
Pre-operative absolute scotomas were 5.00 ± 4.71 (95% CI 1.83 to 8.17); in the early post-operative period decreased to 2.18 ± 2.60 (95% CI 0.43 to 3.95) and at last follow-up were 0.55 ± 0.93 (95% CI -0.08 to 1.17). Pre-operative relative scotomas were 9.82 ± 5.60 (95% CI 6.06 to 13.58), in the early post-operative period decreased to 6.91 ± 5.72 (95% CI 3.07 to 10.75) and at last follow-up were 2.91 ± 2.84 (95% CI 1.00 to 4.82). A statistically significant difference in the number of absolute scotomas was found between pre- and post-operative (t test, p value = 0.03), post-operative and last follow-up (t test, p value = 0.015) and pre-operative and last follow-up microperimetry (t test, p value = 0.004). A statistically significant difference in the number of relative scotomas was found between pre- and post-operative (t test, p value = 0.045), post-operative and last follow-up (t test, p value = 0.006) and pre-operative and last follow-up microperimetry (t test, p value = 0.001).
Fixation stability within 2 degree values (dB) was respectively 92.73 ± 10.44 (95% CI 85.71 to 99.74) pre-operatively, 97.64 ± 5.63 (95% CI 93.86 to 101.42) post-operatively and 99.36 ± 1.03 (95% CI 98.67 to 100.05) at the last follow-up. Fixation stability difference within 2 degrees (%) was statistically significant between pre-operative and post-operative (t test, p value = 0.01) and pre-operative and last follow-up data (t test, p value = 0.05); there was no statistical significance comparing post-operative and last follow-up fixation stability data.
No statistically significant difference was found between mean defect (dB) and fixation stability within 4 degree (%) parameters during the follow-up period. Mean values and standard deviation microperimetry data are summarized in Table 1.
Non-parametric Wilcoxon test performed between subjects with integrity and interruption of IS/OS layer after surgery showed no statistically significative differences in BCVA 0.20 and 0.23 (20/32 and 20/33), respectively (Wilcoxon test, p value = 0.72).
OCTA parameters of the operated eye showed no statistical significance compared with the fellow eye (Fig. 3). Data are shown in Table 2.
Optical coherence tomography angiography (OCTA), vessel density (VD) and SD-OCT comparison between the operated eye (left of the figure) and fellow eye (right of the figure). No statistically significant difference in analysed OCTA parameters was found. The IS/OS layer is continuous in both the eyes on OCT scan
Discussion
Vitrectomy associated to ILM peeling, nowadays, is considered the conventional surgical technique treating MH [9]. Many recent studies have shown that ILM peeling is a procedure that can cause traumatic effects and progressive modifications to underlying inner retinal layers shortly after the surgery [19]. Iatrogenic retinal repercussions are described as dissociated optic nerve fibre layer (DONFL), swelling of the arcuate nerve fibre layer (SANFL) and a reduction in papillo-foveal distance [20]. On the other hand, it has been demonstrated that functional changes appeared to be reversible and did not compromise final visual recovery; in addition, it has been validated that this technique increases primary anatomical closure [1, 20]. ILM removal is associated with a higher success rate in large size MH rather than < 400 μm holes [20]. Recently, new surgical procedures to treat large MH have been developed, like the inverted ILM flap technique [21] or amniotic membrane apposition over the hole [22], usually spent for bigger dimension MHs (> 700 μm). Our study considered large holes according to IVTS classification with 424.64 ± 71.07 μm mean diameter, representing the suitable candidates for vitrectomy associated to ILM peeling technique.
OCT technology permits all retinal layers assessment and several authors evaluated retinal changes in MH surgery [23,24,25,26,27]. Qualitative studies of the outer retinal layers were doubtless more instructive than studies reporting only retinal thickness. Besides ILM peeling associated retinal traumatic effects, more recent analysis focused on prognostic retinal defects. Patients showing OCT restoration of the photoreceptor IS/OS junction after MH surgery presented a good post-operative BCVA, while the functional outcome was poorer in those cases without IS/OS line [24]. We previously showed that pre-operative RPE layer integrity may be indicative of good photoreceptor restoration and visual recovery in patients with surgically closed MHs [25]. In recent times, different authors found out more: an intact external limiting membrane (ELM) seemed necessary for IS/OS line restoration [26]; post-operative VA was better when both IS/OS and ELM lines were restored rather than only IS/OS layer [27]. We have confirmed in our study IS/OS and ELM lines tight interconnection in the recovery progress. In long-term post-operative time, all eyes with IS/OS junction defect (6 eyes, 43%) had an ELM defect too. We noted slightly better visual acuity in eyes with restored IS/OS junction line, compared with eyes with IS/OS junction defect, which was 0.20 and 0.23, respectively, but these findings were not statistically significant.
OCTA features permitted a new approach in retinal microvasculature understanding. Recently has been shown [28] that the deep capillary plexus had a wheel-like pattern with denser vascular network in early-stage MHs, compared with poorer microvasculature of larger late-stage ones. Demirel et al. [28] evaluated OCTA characteristics after surgical MH repair compared with fellow eye and healthy controls. Surgical eyes revealed lower flow indexes, higher FAZ areas and lower vascular densities than those of the healthy eyes and the eyes of the control group. Unfortunately, our patients underwent surgery prior to this technology advent and our OCTA results could necessarily focus on the last follow-up testing. We compared treated eye vessel density and volume parameters with the fellow eye ones. Outcomes presented a modest quantitative reduction in VD of operated eyes statistically not significant suggesting a retinal microvasculature organization similar to the unaffected eye long time after successful MH closure. It is possible that in long-term retinal recovery, vessel density architecture could reorganize itself. This could conceivably explain why our results did not match with recent literature considering, in one hand, the lack of long-term OCTA studies after MH surgery, and, in the other, that the absence of pre-surgical comparison represents a limitation in our data.
The anatomic success of IMH surgery is considered when the MH is closed, even if it not commonly corresponds with the functional goal [29]. The operation is considered a functional success if there is a ≥ 2 Snellen line (equivalent ≥ 0.3 LogMAR units) improvement [30]. Many studies have shown that after macular surgery, the BCVA improves [31].
In our study, all the MHs were closed after surgery without relapsing cases after the long-term follow-up. BCVA improved significantly post-surgery (p value < 0.001) but without significant value between post-operative visit and long-term follow-up (p value = 0.34).
Microperimetry provides an accurate and repeatable examination of the retinal sensitivity in selected retinal areas; moreover, it tended to be more sensitive than VA in detecting macular dysfunction [15, 29]. For this reason, to assess the functional success of the surgery, we used microperimetry measuring retinal sensitivity and the fixation behaviour. We found that post-operative retinal mean sensitivity improved significantly (p value = 0.002), consistent with BCVA attitude. In addition, the mean sensitivity between post-operative exam and the long-term follow-up presented further significant gain (p value < 0.001). To estimate retinal sensitivity, we also compared patient scotomas before and after the treatment and at the long-term follow-up. In accordance with mean sensitivity, number of relative and absolute scotomas significantly decreased both post-operatively and comparing post-operative test and the long-term follow-up (p value = 0.03 and p value = 0.015 for absolute scotomas, respectively; p value = 0.045 and p value = 0.006 for relative scotomas, respectively). The fixation stability within 2 degrees presented quantitative improvement in post-operative data, displaying a significant gain right after surgery (p value = 0.01) and positive correlation comparing pre-operative and last follow-up (p value = 0.05). The distribution of fixation points presented an augmented accuracy in the long-term follow-up intensifying the point concentration through the centre of fixation area. Our data suggests an extended retinal readjustment after an anatomical successful MH surgery, improving retinal sensitivity and fixation stability over the years.
The limitations of the current study include a limited number of patients enrolled and the lack of OCTA pre-surgical imaging. The long-term follow-up in this case represents an adversity in the maintenance of patient cohort mostly for the increasing amount of patients lost to follow-up over time. In our case, 5 of 19 (26%) patients were excluded: four patients were lost to follow-up and one eye suffered from retinal detachment few years after macular surgery. Therefore, further studies using bigger sample of patients and possibly a direct comparison between pre-operative and long-term follow-up OCTA would add information to advance our understanding of retinal changes associated with MH surgical repair.
Using MP-1, Richter-Mueksch et al. [15] demonstrated fewer improvement of fixation stability in patients who underwent recent macular pucker surgery, suggesting that a longer time is needed for better visual function recovery. In the UK multicentre database study, 48.6% eyes showed BCVA improvement at 12 weeks after MH surgery and 58.3% at 52 weeks [31], confirming retinal functional enhancement in time. Our study corroborates this finding adding further information thanks to microperimetry and relevant long-term follow-up. Mean retinal sensitivity improvement in the long-term follow-up (at least 9 years), conversely to no statistical increase of BCVA compared with post-operative control, suggests protracted retinal functional recovery and reorganization after surgery without evident visual improvement.
Photoreceptor regeneration and readjustment combined to interneuron synaptic plasticity are a gradual and maybe constant phenomenon, expressed as a functional recovery, gross and easy to be objectified initially, subtle and refined after time.
Conclusions
In summary, we demonstrated that in successfully closed MHs, retinal sensitivity measured by microperimetry significatively increases after a long follow-up period even when BCVA remains stable or raises slightly. Vessel density tends to be quantitatively similar to fellow eye several years after surgery.
References
Parravano M, Giansanti F, Eandi CM, Yap YC, Rizzo S, Virgili G (2015) Vitrectomy for idiopathic macular hole. Cochrane Database Syst Rev 12(5):CD009080. https://doi.org/10.1002/14651858.CD009080.pub2
Gass JD (1995) M. Reappraisal of biomicroscopic classification of stages of development of a macular hole. Am J Ophthalmol 119(6):752–759. https://doi.org/10.1016/S0002-9394(14)72781-3
la Cour M, Friis J (2002) Macular holes: classification, epidemiology, natural history and treatment. Acta Ophthalmol Scand 80(6):579–587. https://doi.org/10.1034/j.1600-0420.2002.800605.x
Duker JS, Kaiser PK, Binder S, De Smet MD, Gaudric A, Reichel E, Sadda SR, Sebag J, Spaide RF, Stalmans P (2013) The International Vitreomacular Traction Study Group Classification of vitreomacular adhesion, traction, and macular hole. Ophthalmology 120(12):2611–2619. https://doi.org/10.1016/j.ophtha.2013.07.042
Heegaard S (1997) Morphology of the vitreoretinal border region. Acta Ophthalmol Scand Suppl (222):1–31
Sebag J, Wang MY, Nguyen D, Sadun AA (2009) Vitreopapillary adhesion in macular diseases. Trans Am Ophthalmol Soc 107:35–44
Tognetto D, Michelone L, Fanni D, Ravalico G (2007) Idiopathic macular hole. Expert Rev Ophthalmol (2):285–298. https://doi.org/10.1586/17469899.2.2.285
Christensen UC, Krøyer K, Sander B, Jorgensen TM, Larsen M, La Cour M (2010) Macular morphology and visual acuity after macular hole surgery with or without internal limiting membrane peeling. Br J Ophthalmol 94(1):41–47. https://doi.org/10.1136/bjo.2009.159582
Ezra E, Gregor ZJ (2004) Surgery for idiopathic full-thickness macular hole: two-year results of a randomized clinical trial comparing natural history, Vitrectomy, and Vitrectomy plus autologous serum: Moorfields Macular Hole Study Group report no. 1. Arch Ophthalmol 122(2):224–236
Eckardt C, Eckardt U, Groos S, Luciano L, Reale E (1997) Removal of the internal limiting membrane in macular holes. Clinical and morphological findings. Ophthalmologe 94(8):545–551
Tognetto D, Grandin R, Sanguinetti G, Minutola D, Di Nicola M, Di Mascio R, Ravalico G (2006) Internal limiting membrane removal during macular hole surgery. Results of a multicenter retrospective study. Ophthalmology 113(8):1401–1410. https://doi.org/10.1016/j.ophtha.2006.02.061
Miglior S (2003) Microperimetry and glaucoma. Acta Ophthalmol Scand 236:19. https://doi.org/10.1034/j.1600-0420.80.s236.9.x
Marmor MF, Choi SS, Zawadzki RJ, Werner JS (2008) Visual insignificance of the foveal pit: reassessment of foveal hypoplasia as fovea plana. Arch Ophthalmol 126(7):907–913. https://doi.org/10.1001/archopht.126.7.907
Chen WC, Wang Y, Li XX (2012) Morphologic and functional evaluation before and after successful macular hole surgery using spectral-domain optical coherence tomography combined with microperimetry. Retina 32(9):1733–1742. https://doi.org/10.1097/IAE.0b013e318242b81a
Richter-Mueksch S, Vécsei-Marlovits PV, Sacu SG, Kiss CG, Weingessel B, Schmidt-Erfurth U (2007) Functional macular mapping in patients with vitreomacular pathologic features before and after surgery. Am J Ophthalmol 144(1):23–31. https://doi.org/10.1016/j.ajo.2007.03.045
Spaide RF, Klancnik JM, Cooney MJ (2015) Retinal vascular layers imaged by fluorescein angiography and optical coherence tomography angiography. JAMA Ophthalmol 123(3):e24. https://doi.org/10.1001/jamaophthalmol.2014.3616
Rizzo S, Savastano A, Bacherini D, Savastano MC (2017) Vascular features of full-thickness macular hole by OCT angiography. Ophthalmic Surg Lasers Imaging Retina 48(1):62–68. https://doi.org/10.3928/23258160-20161219-09
Wong EN, Mackey DA, Morgan WH, Chen FK (2016) Inter-device comparison of retinal sensitivity measurements: the CenterVue MAIA and the Nidek MP-1. Clin Exp Ophthalmol 44(1):15–23. https://doi.org/10.1111/ceo.12629
Karacorlu M, Karacorlu S, Ozdemir H (2003) Iatrogenic punctate chorioretinopathy after internal limiting membrane peeling. Am J Ophthalmol 135(2):178–182. https://doi.org/10.1016/S0002-9394(02)01925-6
Morescalchi F, Costagliola C, Gambicorti E, Duse S, Romano MR, Semeraro F (2017) Controversies over the role of internal limiting membrane peeling during vitrectomy in macular hole surgery. Surv Ophthalmol 62(1):58–69. https://doi.org/10.1016/j.survophthal.2016.07.003
Michalewska Z, Michalewski J, Adelman RA, Nawrocki J (2010) Inverted internal limiting membrane flap technique for large macular holes. Ophthalmology 117(10):2018–2025. https://doi.org/10.1016/j.ophtha.2010.02.011
Rizzo S, Caporossi T, Tartaro R, Finocchio L, Franco F, Barca F, Giansanti F (2018) A human amniotic membrane plug to promote retinal breaks repair and recurrent macular hole closure. Retina. https://doi.org/10.1097/iae.0000000000002320
Ko TH, Witkin AJ, Fujimoto JG, Chan A, Rogers AH, Baumal CR, Schuman JS, Drexler W, Reichel E, Duker JS (2006) Ultrahigh-resolution optical coherence tomography of surgically closed macular holes. Arch Ophthalmol 124(6):827–836. https://doi.org/10.1001/archopht.124.6.827
Morawski K, Jȩdrychowska-Jamborska J, Kubicka-Trzaska A, Romanowska-Dixon B (2016) The analysis of spontaneous closure mechanisms and regeneration of retinal layers of a full-thickness macular hole: relationship with visual acuity improvement. Retina 36(11):2132–2139. https://doi.org/10.1097/IAE.0000000000001074
Reibaldi M, Avitabile T, Longo A, Uva MG, Bonfiglio V, Russo A, Toro MD, Stella S, Giovannini A, Viti F, Nicolai M, Saitta A, Cennamo G, Gagliano C, Mariotti C (2014) Correlation of preoperative retinal pigment epithelium status with foveal microstructure in repaired macular holes. Ophthalmologica. 232(4):194–199
Landa G, Gentile RC, Garcia PMT, Muldoon TO, Rosen RB (2012) External limiting membrane and visual outcome in macular hole repair: spectral domain OCT analysis. Eye 26(1):61–69. https://doi.org/10.1038/eye.2011.237
Ruiz-Moreno JM, Lugo F, Montero JA, Piñero DP (2012) Restoration of macular structure as the determining factor for macular hole surgery outcome. Graefes Arch Clin Exp Ophthalmol 250(10):1409–1414. https://doi.org/10.1007/s00417-012-1963-2
Demirel S, Deǧirmenci MFK, Bilici S, Yanik Ö, Batloǧlu F, Özmert E, Alp N (2017) The recovery of microvascular status evaluated by optical coherence tomography angiography in patients after successful macular hole surgery. Ophthalmic Res 59(1):53–57. https://doi.org/10.1159/000484092
Ueda-Consolvo T, Otsuka M, Hayashi Y, Ishida M, Hayashi A (2015) Microperimetric biofeedback training improved visual acuity after successful macular hole surgery. J Ophthalmol 2015:572942. https://doi.org/10.1155/2015/572942
Bonnabel A, Bron AM, Isaico R, Dugas B, Nicot F, Creuzot-Garcher C (2013) Long-term anatomical and functional outcomes of idiopathic macular hole surgery. The yield of spectral-domain OCT combined with microperimetry. Graefes Arch Clin Exp Ophthalmol 251(11):2505–2511. https://doi.org/10.1007/s00417-013-2339-y
Kaźmierczak K, Stafiej J, Stachura J, Zuchowski P, Malukiewicz G (2018) Long-term anatomic and functional outcomes after macular hole surgery. J Ophthalmol 2018:3082194. https://doi.org/10.1155/2018/3082194
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nicolai, M., Franceschi, A., De Turris, S. et al. Long-term improvement of retinal sensitivity after macular hole surgery over at least 9-year-old follow-up: a case series. Graefes Arch Clin Exp Ophthalmol 258, 1655–1662 (2020). https://doi.org/10.1007/s00417-020-04719-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-020-04719-3