Abstract
Purpose
The study aimed to evaluate cytokines in tears as potential biomarkers in non-infectious uveitis.
Methods
Tear samples were obtained using Schirmer strips from 50 patients enrolled in a randomised controlled study of simvastatin in non-infectious uveitis and from a control group of 30 healthy participants. The concentrations of IL-6, IL-8, IL-10, and IFN-γ in tears were measured at the study’s baseline and again after 8 weeks of treatment using commercial enzyme-linked immunosorbent assay kits.
Results
The concentrations of tears IL-6 and IL-10 were increased in patients with non-infectious uveitis in comparison with the healthy participants. Longer disease duration was associated with elevated levels of IL-6. The concentrations of the studied cytokines in tears did not correlate with the extent of eye inflammation at baseline. No link between the changes in cytokine levels and changes in clinical parameters during treatment was observed. Baseline IL-10 concentrations independently predicted the development of the clinical response to treatment at weeks 4 and 8.
Conclusion
Although elevated in non-infectious uveitis patients, tear cytokine levels do not correlate with eye inflammation and are not sensitive to change after treatment. However, the level of IL-10 may be a predictive biomarker of response to the treatment of uveitis.
Trial registration
NCT04183387
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Non-infectious uveitis is a significant health problem that contributes up to 10% of cases of total blindness [1] and has a socioeconomic impact at least as pronounced as that of diabetic retinopathy [2].
Given the methods for assessing uveitis activity are primarily subjective and lack discrimination and reliability, there is a need for biomarkers reflecting changes in the extent of eye inflammation in patients with uveitis [3]. Finding predictive biomarkers of uveitis would allow identification of patients who are less likely to respond to conventional treatments and who would benefit from early, aggressive treatment.
It is known that cytokines play a substantial role in inflammation in general and in local eye inflammation in non-infectious uveitis. In many studies, eye inflammation has been associated with an increase in pro-inflammatory cytokines in the serum and aqueous humour [4, 5]. Thus, cytokines might be potential biomarkers for non-infectious uveitis. However, the poor acceptability of cytokines in the aqueous humour limits this approach. Compared with the aqueous humour or vitreous samples, tear samples are more conveniently collected and so tear cytokines may be feasible biomarkers for uveitis. There is a lack of studies evaluating tear cytokines as biomarkers of eye inflammation or as predictive biomarkers of response to treatment in non-infectious uveitis patients.
The aims of the present study were to (a) compare the pro-inflammatory and anti-inflammatory cytokine levels in the tears of non-infectious uveitis patients and healthy participants; (b) evaluate clinical and demographic factors associated with the concentrations of cytokines in tears; (c) report changes in the cytokine levels of tears following uveitis treatment; and d) evaluate the possibility of using tear cytokines to predict clinical responses to uveitis treatment.
Methods
Healthy subjects
A group of 30 healthy medical students was used for this study. The exclusion criterion was any inflammatory disease of the eye.
Patients
The patients with uveitis were from the study evaluating the effects of simvastatin on eye inflammation in patients receiving conventional treatment. The conventional treatment consisted of local (one or both of eye drops and periorbital injections) and systemic corticosteroids, prescribed at the physician’s discretion. The study was registered on the Clinicaltrials.gov database (NCT04183387).
Details of the study protocol and the clinical results of the study are reported elsewhere [6]. Briefly, in this open-label study, 50 patients with acute non-infectious uveitis were randomised to receive, for 2 months, either conventional treatment alone or conventional treatment plus 40 mg/day of simvastatin. The clinical parameters used were slit-lamp anterior chamber cells, anterior chamber flare, vitreous haze grade, intraocular pressure, and estimation of best-corrected visual acuity in logMAR format. In the case of bilateral uveitis, the most affected eye was selected for the assessments.
The response to treatment was defined as follows:
-
(1)
≤ 0.5 + anterior chamber cells, ≤ 0.5 + vitreous haze, and no active retinal/choroidal lesions; and
-
(2)
≤ 10 mg of oral prednisone daily and ≤ 2 drops of prednisolone acetate 1% (or equivalent) a day.
The study was approved by the Independent Ethics Committee of Municipal City Hospital No. 1, Novosibirsk, and was conducted in accordance with the Declaration of Helsinki; all subjects provided written informed consent.
Tear sample collection
The tear samples were collected as previously described. The investigator, with gloves, placed a Schirmer strip over the lid margin at the junction of the lateral and middle thirds of the lower eyelids; it was kept in place for 5 min while subjects closed their eyes without an anaesthetic. The Schirmer strips were removed with gloves and tear volume was recorded in millimetres. Each Schirmer strip was placed into a sterile 2-mL centrifuge tube, stored on ice for between 20 min and 1 h, and then stored at minus 20 °C until processed [7].
Tear extraction from Schirmer strips
The method described previously was used to extract tears from the Schirmer strips [7]. In brief, a standard curve was first developed to calculate millimetres of wetting from the volume of tears collected. A known volume of phosphate-buffered saline (PBS) was placed on a Schirmer strip and wetting in millimetres was recorded after 1 min. This process was repeated a total of 3 times for each volume tested, and a standard curve for volume to Schirmer strip reading was generated.
Tubes containing a strip with a tear sample were warmed to ambient temperature and were incubated with an assay buffer (200 μL) for 3 h. Before discarding the Schirmer strips, residual liquid was removed and combined with the stored extraction buffer.
Detection of cytokines using an enzyme-linked immunosorbent assay
The multiple-antigen detection method developed by Wakefield et al. [8] was used to detect cytokines in the samples. Following this method, 110 μL of the diluted tears was placed on an antigen-capture enzyme-linked immunosorbent assay (ELISA) plate, where specific antigen from the sample were captured while other cytokines and chemokines remained in the solution. After incubation, assuming that approximately 5 μL of sample volume would be lost during transfer, the samples (105 μL) were retrieved from the ELISA plate and placed on the next antigen-capture ELISA plate. The ELISA analyses were performed using commercial ELISA kits (IL-6, IL-8, IL-10, TNFα, and IFN-γ ELISA-Best, Vector-Best, Russia). Based on the manufacturer’s instructions, the detection limits for IL-6, IL-8, IL-10, TNFα, and IFN-γ were 0.5, 2, 2.5, 2, and 5 pg/mL. Concentrations below these thresholds were considered non-detects. The concentrations of the detected cytokines in tear samples were then calculated based on the volume of tears in the sample and the volume of added assay buffer (200 μL) used for the cytokine extraction.
Statistical analysis
As is often the case for immunological data, cytokine values featured a substantial proportion of non-detects. For a given cytokine, concentrations below the reporting threshold were considered non-detectable and therefore left-censored. Tobit regression, a recommended statistical approach for left-censored data [9], was performed for each cytokine separately. This method allows adjustment for the effects of potential confounders such as age and sex. Summary statistics and regression equations for the left-censored data were computed using maximum likelihood estimation (MLE) [10]. Using MLE allows data to be analysed with up to 80% of censored values [11]. Using R package censReg version 0.5-26 [12], both the Student t test and censored regressions with and without potential confounders were performed to test the differences in cytokine levels between the control group and the patients. Multiple Tobit regression models were used to evaluate factors associated with baseline concentrations of cytokines in tears.
The changes before and after treatment were assessed using paired Student’s t test. The correlations between changes in tear cytokines and changes in clinical parameters were assessed using Spearman correlation test. The differences in baseline tear cytokine concentrations between patients who responded and who did not respond to treatment were assessed using both the Student t test as well as adjusted and non-adjusted censored regression models.
When adjusting for confounders, the usual rule of thumb of ten was not adhered to because it mostly concerns logistic regression analysis; in linear regression, the number of participants for one confounder may be significantly lower [13].
All statistical analyses were performed using the R software (version 3.5.1).
Results
Baseline demographic and clinical characteristics of the patients are presented in Table 1. Most patients had anterior uveitis. Almost half of the patients were HLA-B27-positive. More than 50% of patients had a diagnosis of underlying systemic disease, primarily ankylosing spondylitis. The mean age of the control group was 20.7 (1.2) years; 17 (57%) were male and 13 (43%) were female. The patients did not receive any systemic treatment at the time of baseline tear collection. There were no instances of decreased tear production in either the patient or control group.
Overall, baseline percentages of censored values for IL-6, IL-8, IL-10, TNFα, and IFN-γ were 51.25%, 1.25%, 73.75%, 97.5%, and 100%, respectively. The percentages of censored values on the last visit for IL-6, IL-8, IL-10, TNFα, and IFN-γ were 36%, 0%, 80%, 94%, and 96%. Therefore, data from TNFα and IFN-γ were excluded from all further analyses.
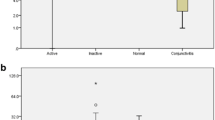
Table 2 presents a comparison of tear cytokine concentrations between the patients with uveitis and the healthy participants. Uveitis patients showed a sevenfold increase in concentration for IL-6, a twofold increase for tear IL-8, and a fivefold increase for IL-10 using both the Student t test and Tobit regression modelling adjusting for left-censoring. However, after adjustment for demographics, only the differences in IL-6 and IL-10 concentrations remained statistically significant.
Neither demographic characteristics nor signs of ocular inflammation were linked with tear cytokine concentrations. Among the chosen predictor variables, only the duration of uveitis was associated with higher concentrations of IL-6 and IL-8 at baseline. The β-coefficients 49 and 235 indicated that every year spent with uveitis was associated with a 49-pg/mL average increase in the concentration of IL-6 and a 235-pg/mL average increase in IL-8 (Table 3).
The treatment of uveitis did not result in significant changes in IL-6, IL-8, and IL-10 concentrations. After stratification for simvastatin use, the patient control group showed a significant decrease in IL-6 levels (Table 4). No correlations were found between changes in cytokine concentrations and changes in clinical measures (Table 5).
Table 6 presents the differences in baseline tear cytokine levels between patients who responded and those who did not respond to the treatment. The responders at week 4 and week 8 showed fourfold and ninefold higher baseline concentrations of IL-10 in the tear samples. These associations remained after adjustments for left-censoring and clinical covariates (Table 6).
Discussion
This study found increased concentrations of IL-6 and IL-10 in the tears of patients with uveitis compared with healthy control subjects. Increases in IL-6 levels were associated with longer disease duration. No link between changes in tear cytokine concentrations and changes in eye inflammation during the treatment was found. The baseline IL-10 was a significant and independent predictor of clinical response to treatment.
Most studies evaluating cytokines in uveitis have sampled from one or both of the aqueous humour and serum. Carreno et al., in a cross-sectional study investigating tear cytokines in uveitis, measured the levels of 21 molecules using multiplex bead-based assays [14]. This study’s observations match some of those made by Carreno et al. While the percentages of IL-8 and IL-10 detects were similar in both studies, this study detected IL-6 in more samples (50% compared with 20%). In both studies, TNFα and IFN-γ were not detected in almost 100% of the tear samples. Similar to Careno et al., we found a significant increase in tear IL-8 levels in uveitis patients in comparison with healthy control subjects using non-adjusted models, but this was not confirmed in models adjusted for age and sex. In contrast with Careno et al., this study used statistical techniques accounting for censoring and was able to perform further analyses on IL-10.
This study and that of Carreno et al. may differ in findings because almost half of the patients in the latter study received immunomodulatory agents at the time of the assessment, while patients in this study were treatment-free at the baseline.
The results of this study also concur with the findings of Türkçüoğlu et al., showing no association between pro-inflammatory cytokine IL-2 concentrations in tears and disease activity in patients with Bechet disease [15]. In another study, several cytokines in the tears of paediatric patients with non-infectious uveitis were found [16]. The detected cytokines differed from those in this study; this can be explained by the differences in cytokine profiles in adult patients with non-infectious uveitis and paediatric patients with non-infectious uveitis [17].
The findings indicate that duration of chronic eye inflammation rather than intensity is associated with higher pro-inflammatory tear cytokine levels. Therefore, IL-6 and IL-8 concentrations may be biomarkers of the cumulative burden of eye inflammation. On the other hand, IL-6 contributes to the transition from acute to chronic inflammation by changing the nature of leucocyte infiltrate and by stimulating T and B cells [18]; it may, therefore, be a marker of uveitis chronicity. The absence of changes in cytokine concentrations after treatment and the lack of association between changes in clinical parameters indicate that the tear cytokines studied may not be useful as disease activity biomarkers. These findings accord with the results of Carreno et al. who did not find any difference in tear cytokines between patients with active and non-active uveitis [14]. This can also be explained by the underdiagnosis of inflammation in patients with uveitis described by clinical information as inactive.
Numerous studies have assessed cytokine levels in the serum and aqueous humour of patients with uveitis. Similar to this study, higher IL-6 concentrations were found in the vitreous fluid of chronic uveitis patients than in that of patients without uveitis [19]. In addition, targeting IL-6 seems to be a promising strategy for the treatment of autoimmune uveitis [20]. In one study, serum IL-8 levels were higher in patients with non-infectious uveitis and associated with disease activity [21]. A study demonstrated that serum and aqueous humour IL-10 concentrations were increased in uveitis patients [22]. This study’s findings suggest that tear IL-6 and IL-10 levels may parallel the concentrations of these cytokines in the aqueous humour and serum.
TNFα plays an important role in the pathogenesis of uveitis, as evidenced by the efficacy of the anti-TNF blockade. Increased TNFα concentrations were found in both the serum and aqueous humour of patients with uveitis [23]––but were rarely detected in tear samples––in both this study and that of Carreno et al.—indicating that tear TNFα levels do not reflect the concentrations within the eye.
In another previous study, IFN-γ concentrations were found to be higher in the aqueous humour and serum of uveitis patients. Moreover, elevated serum IFN-gamma levels seemed to predispose the patient to a more serious loss of vision [22]. The low frequency of IFN-γ detection in this study indicates there might be no link between the concentration of IFN-γ in tears and the intraocular levels.
Also, matching this study’s findings, another study observed no changes in IL-6 and IL-10 levels in the aqueous humour during treatment of uveitis with the anti-TNF blocker adalimumab [24]. This suggests that cytokines have low sensitivity to change and therefore might not be a useful biomarker of changes in uveitis activity.
This study found the IL-10 level in tears could potentially predict responses to simvastatin treatment. This finding can be explained by the immunoregulatory effects of statins: statins were shown to induce immune tolerance [25], while IL-10 is necessary for the development of induced immune tolerance in experimental uveitis [26]. Therefore, it can be speculated that statins can exhibit anti-inflammatory effects and induce immunological tolerance in the presence of increased concentrations of IL-10 in patients with uveitis.
The main limitation of this study is the low number of cytokines studied.
The strength of this study was its longitudinal design and the use of statistical methods accounting for censoring inherent in the measurement of cytokine concentrations in biological fluids. The baseline evaluation of treatment-free patients allowed the exclusion of a potentially substantial confounder, the influence of immunosuppressive treatment on cytokine production.
Conclusion
The cytokines studied in tears do not appear to be potential biomarkers of disease activity in non-infectious uveitis and are not sensitive to change. The level of IL-10 in tears has potential utility as a predictive biomarker of response to treatment.
References
Suttorp-Schulten MS, Rothova A (1996) The possible impact of uveitis in blindness: a literature survey. Br J Ophthalmol 80(9):844–848
de Smet MD, Taylor SR, Bodaghi B, Miserocchi E, Murray PI, Pleyer U, Zierhut M, Barisani-Asenbauer T, LeHoang P, Lightman S (2011) Understanding uveitis: the impact of research on visual outcomes. Prog Retin Eye Res 30(6):452–470. https://doi.org/10.1016/j.preteyeres.2011.06.005
Denniston AK, Keane PA, Srivastava SK (2017) Biomarkers and surrogate endpoints in uveitis: the impact of quantitative imaging. Invest Ophthalmol Vis Sci 58(6):BIO131–BIO140. https://doi.org/10.1167/iovs.17-21788
Valentincic NV, de Groot-Mijnes JD, Kraut A, Korosec P, Hawlina M, Rothova A (2011) Intraocular and serum cytokine profiles in patients with intermediate uveitis. Mol Vis 17:2003–2010
Takase H, Futagami Y, Yoshida T, Kamoi K, Sugita S, Imai Y, Mochizuki M (2006) Cytokine profile in aqueous humor and sera of patients with infectious or noninfectious uveitis. Invest Ophthalmol Vis Sci 47(4):1557–1561. https://doi.org/10.1167/iovs.05-0836
Shirinsky IV, Biryukova AA, Shirinsky VS (2017) Simvastatin as an adjunct to conventional therapy of non-infectious uveitis: a randomized, open-label pilot study. Curr Eye Res 42(12):1713–1718. https://doi.org/10.1080/02713683.2017.1355468
VanDerMeid KR, Su SP, Krenzer KL, Ward KW, Zhang JZ (2011) A method to extract cytokines and matrix metalloproteinases from Schirmer strips and analyze using Luminex. Mol Vis 17:1056–1063
Wakefield D, McCluskey P, Roche N, Rossio JL (1995) Aqueous humor cytokine profile in patients with chronic uveitis. Ocul Immunol Inflamm 3(3):203–208. https://doi.org/10.3109/09273949509069113
Ballenberger N, Lluis A, von Mutius E, Illi S, Schaub B (2012) Novel statistical approaches for non-normal censored immunological data: analysis of cytokine and gene expression data. PLoS One 7(10):e46423. https://doi.org/10.1371/journal.pone.0046423
Helsel DR (2005) Nondetects and data analysis: statistics for censored environmental data. Statistics in practice. Wiley-Interscience, Hoboken
Huynh T, Ramachandran G, Banerjee S, Monteiro J, Stenzel M, Sandler DP, Engel LS, Kwok RK, Blair A, Stewart PA (2014) Comparison of methods for analyzing left-censored occupational exposure data. Ann Occup Hyg 58(9):1126–1142. https://doi.org/10.1093/annhyg/meu067
Henningsen A (2017) censReg: censored regression (Tobit) models. https://CRAN.R-project.org/package=censReg. Accessed 11 Dec 2019
Austin PC, Steyerberg EW (2015) The number of subjects per variable required in linear regression analyses. J Clin Epidemiol 68(6):627–636. https://doi.org/10.1016/j.jclinepi.2014.12.014
Carreno E, Portero A, Herreras JM, Garcia-Vazquez C, Whitcup SM, Stern ME, Calonge M, Enriquez-de-Salamanca A (2017) Cytokine and chemokine tear levels in patients with uveitis. Acta Ophthalmol 95(5):e405–e414. https://doi.org/10.1111/aos.13292
Turkcuoglu P, Arat YO, Kan E, Kan EK, Chaudhry IA, Koca S, Celiker U, Ilhan N (2016) Association of disease activity with serum and tear IL-2 levels in Behcet disease. Ocul Immunol Inflamm 24(3):313–318
Angeles-Han ST, Yeh S, Patel P, Duong D, Jenkins K, Rouster-Stevens KA, Altaye M, Fall N, Thornton S, Prahalad S, Holland GN (2018) Discovery of tear biomarkers in children with chronic non-infectious anterior uveitis: a pilot study. J Ophthalmic Inflamm Infect 8(1):17
Sijssens KM, Rijkers GT, Rothova A, Stilma JS, de Boer JH (2008) Distinct cytokine patterns in the aqueous humor of children, adolescents and adults with uveitis. Ocul Immunol Inflamm 16(5):211–216
Gabay C (2006) Interleukin-6 and chronic inflammation. Arthritis Res Ther 8(Suppl 2):S3
Yoshimura T, Sonoda KH, Ohguro N, Ohsugi Y, Ishibashi T, Cua DJ, Kobayashi T, Yoshida H, Yoshimura A (2009) Involvement of Th17 cells and the effect of anti-IL-6 therapy in autoimmune uveitis. Rheumatology (Oxford) 48(4):347–354. https://doi.org/10.1093/rheumatology/ken489
Mesquida M, Molins B, Llorenc V, de la Maza MS, Adan A (2017) Targeting interleukin-6 in autoimmune uveitis. Autoimmun Rev 16(10):1079–1089. https://doi.org/10.1016/j.autrev.2017.08.002
Klok AM, Luyendijk L, Zaal MJ, Rothova A, Hack CE, Kijlstra A (1998) Elevated serum IL-8 levels are associated with disease activity in idiopathic intermediate uveitis. Br J Ophthalmol 82(8):871–874
Lacomba MS, Martin CM, Chamond RR, Galera JM, Omar M, Estevez EC (2000) Aqueous and serum interferon gamma, interleukin (IL) 2, IL-4, and IL-10 in patients with uveitis. Arch Ophthalmol 118(6):768–772
Santos Lacomba M, Marcos Martin C, Gallardo Galera JM, Gomez Vidal MA, Collantes Estevez E, Ramirez Chamond R, Omar M (2001) Aqueous humor and serum tumor necrosis factor-alpha in clinical uveitis. Ophthalmic Res 33(5):251–255. https://doi.org/10.1159/000055677
Hernandez Garfella ML, Palomares Fort P, Roman Ivorra JA, Cervera Taulet E (2015) Aqueous humor levels of different interleukins 1-beta, 2, 6 and 10, tumor necrosis factor-alpha and vascular endothelial growth factor in uveitis treated with adalimumab. J Ophthalmic Vis Res 10(1):49–54. https://doi.org/10.4103/2008-322X.156110
Lee KJ, Moon JY, Choi HK, Kim HO, Hur GY, Jung KH, Lee SY, Kim JH, Shin C, Shim JJ, In KH, Yoo SH, Kang KH (2010) Immune regulatory effects of simvastatin on regulatory T cell-mediated tumour immune tolerance. Clin Exp Immunol 161(2):298–305
Rizzo LV, Morawetz RA, Miller-Rivero NE, Choi R, Wiggert B, Chan CC, Morse HC 3rd, Nussenblatt RB, Caspi RR (1999) IL-4 and IL-10 are both required for the induction of oral tolerance. J Immunol 162(5):2613–2622
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and data collection were performed by Anastasia Biruukova and Natalia Kalinovskaya; analyses were performed by Ivan Shirinsky and Valery Shirinsky. The first draft of the manuscript was written by Ivan Shirinsky, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the LEC attached to Municipal City Hospital No. 1, Novosibirsk, and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article received support from the mentorship team
Rights and permissions
About this article
Cite this article
Shirinsky, I.V., Biryukova, A.A., Kalinovskaya, N.Y. et al. Tear cytokines as potential biomarkers in non-infectious uveitis: post hoc analysis of a randomised clinical trial. Graefes Arch Clin Exp Ophthalmol 258, 1813–1819 (2020). https://doi.org/10.1007/s00417-020-04707-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-020-04707-7