Abstract
Purpose
Diabetic macular edema (DME) is a major cause of vision loss. Diabetes patients with mild macular edema and good visual acuity are often observed carefully so that treatment can be instituted when central vision is threatened. Optimal frequency of monitoring of these patients is unknown. Our study aimed to gather more information to determine a safe interval for monitoring of patients with eyes that were not undergoing active treatment for DME and to correlate outcomes with clinical risk factors.
Methods
Study population: Ninety-seven eyes with optical coherence tomography (OCT) evidence of DME of 97 patients with diabetes. Study procedures: Retrospective review of medical records and macular OCT scans at a 6–12-month interval. Primary outcomes: Change in visual acuity and change in central subfield thickness (CSFT) between the initial and follow-up OCT scans.
Results
There was no significant change from median baseline visual acuity 6/9 (inter-quartile range 6/6–6/12) or from median baseline CSFT (290 μm, inter-quartile range 270–312 μm) over a median duration of 8 months (inter-quartile range 7–10 months). The numbers of eyes where CSFT had increased ≥ 25 μm, reduced ≥ 25 μm, or remained unchanged were 16 (16%), 6 (6%), and 74 (76%), respectively. Patients with hemoglobin A1c ≥ 8.5% were 5.7 times more likely to develop central subfield thickening (95% CI 1.1–30.1, P = 0.038).
Conclusions
Majority of eyes with DME on OCT had stable CSFT without treatment over a median duration of 8 months. Hemoglobin A1c may be useful for risk stratification.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Diabetic macular edema (DME) is the major cause of central vision loss in people with diabetes [1,2,3]. Monitoring of patients prior to treatment for DME is becoming an increasing issue for medical retina specialists. There are some patients with DME who may qualify as center-involved or “treatment-warranted” where a decision is made to defer treatment on the basis of the perception that the burdens and risks of treatment are not yet justified by the disease severity. The optimal frequency of re-evaluation for patients with DME during periods in which clinicians and patients feel that treatment is not preferred has not been determined. This study was performed in a major hospital ophthalmology clinic offering intensive treatment of diabetic retinopathy (DR) and DME with all currently available modalities. In order to gather more information to determine a safe interval for monitoring of patients, we performed a retrospective study of eyes that were not undergoing active treatment for DME. Some of these eyes were treatment naïve and some had previously been treated. We investigated outcomes in terms of visual acuity and central subfield thickness (CSFT) on optical coherence tomography (OCT). We correlated these outcomes with clinical risk factors in order to develop hypotheses for further investigation for risk stratification in this population.
Methods
This is a retrospective study involving the review of macular OCT scans and medical records of patients from The Royal Melbourne Hospital. The study was approved by The Royal Melbourne Hospital Human Research Ethics Committee. Patients were at least 18 years of age, diagnosed with type 1 or type 2 diabetes, and had more than one macular OCT scans in the hospital database. All OCT scans were performed and analyzed on the Spectralis OCT platform (Heidelberg Engineering, Heidelberg, Germany). Data collection occurred between February and May 2017. A search within the database was conducted using the following diagnoses: “DME”, “DMO”, “CSME”, “CSMO”, “diabetic macular oedema”, and “diabetic retinopathy”. Bilateral 6 mm by 6 mm macular OCT scans of each patient were assessed for the presence of DME.
Study population
In this study, DME was defined as the presence of macular cystoid edema or macular thickening on OCT in a person with diabetes, where clinical and OCT examination did not suggest another cause of edema, such as epiretinal membrane, retinal vein occlusion, neovascular age-related macular degeneration, pseudophakic cystoid macular edema, or uveitic cystoid macular edema.
Eyes would be considered for inclusion if features of DME were evident on an OCT scan and there existed a follow-up scan obtained within a 6- to 12-month window of the initial scan, and where no treatment for DME, DR or cataract had been performed in this window. When multiple such pairs of OCT scans existed for a patient, the first pair from a chronological standpoint that satisfied these criteria was selected.
Eyes were not included or excluded on the basis of baseline visual acuity, severity of DR, central subfield thickness, location, or severity of DME on OCT. Eyes were excluded if macular laser treatment had been performed within 12 months prior to the initial scan, if periocular or intravitreal steroids had been used within 4 months prior to the initial scan or if vascular endothelial growth factor (VEGF) antagonists had been used within 2 months prior to the initial scan. Eyes that underwent cataract surgery within 6 months prior to the initial scan were excluded.
Patients selected based on OCT scans were further assessed against the medical and ophthalmic criteria through a review of medical records. Patients were excluded on the basis of pregnancy, hematological malignancies, use of systemic corticosteroids or VEGF antagonists, and retinitis pigmentosa. Eyes were excluded for any of the following diagnoses: uveitis, non-glaucomatous optic neuropathy, retinal vein occlusion, retinal arteriolar occlusion, neovascular age-related macular degeneration, or other maculopathy.
Study procedures
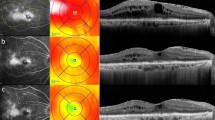
Macular OCT scans were assessed both quantitatively and qualitatively by trained ophthalmologists. Qualitative information of retinal structural changes including presence or absence of microaneurysm, lipid exudate, small hyper-reflective particle, laser, cystoid edema, vitreo-macular adhesion was recorded. Quantitative data included central subfield thickness as well as total macular volume. The thickness map was manually centered on the fovea in cases of misalignment.
Medical and ophthalmic data at baseline and in the inter-scan period were collected from medical records. These included age, gender, type of diabetes, duration of diabetes, body mass index, hemoglobin A1c (HbA1c), hemoglobin, blood pressure, low density lipoprotein, total cholesterol, triacylglyceride, use of insulin, diabetes medications, anti-hypertensive medications, lipid-lowering agents, heart failure, non-ocular complications of diabetes, visual acuity, severity of DR, lens status, glaucoma, treatment of glaucoma, past history of focal/grid laser, pan-retinal photocoagulation, intravitreal VEGF antagonists, intravitreal corticosteroids, and pars plana vitrectomy. When both eyes of a patient were eligible, one eye was randomly selected for statistical analysis using a computer random number generator.
Statistical analysis
The primary outcomes of interest were the change in visual acuity and the change in CSFT between the initial and follow-up OCT scans. Snellen scores for visual acuities were converted to logarithm of the minimum angle of resolution (LogMAR) for analysis. A change in LogMAR visual acuity of ≥ 0.08 (4 ETDRS letters) was considered a meaningful change in visual acuity. CSFT was deemed unchanged if it was within 25 μm of the baseline thickness. The Wilcoxon signed-rank test was used to assess whether there were significant inter-scan differences in visual acuity, macular volume, and CSFT.
Eyes were subdivided into three pre-specified groups according to the changes in CSFT from baseline, namely increased (≥ 25 μm), unchanged (within 25 μm of baseline), or decreased (≤− 25 μm). Kruskal-Wallis test and one-way ANOVA were performed to assess the values of medical and ophthalmic variables in predicting the direction of change in CSFT. The Chi-square test was used for categorical variables.
Multivariable logistic regression was conducted to determine the contribution of individual variables. Odds ratios were computed from the multiple regression. In order to better understand the results of the multivariable analysis, tests of multicollinearity between the independent variables were performed and stratification analyses were conducted to detect effect modification. A P value of less than 0.05 was considered to indicate statistical significance. P values and confidence intervals were two-sided. SPSS Statistics 23.0 (Armonk, NY: IBM Corp) was used for all statistical analyses.
Results
Patient characteristics
OCT scans of 543 patients were assessed for the presence of DME. A total of 140 eyes of 97 patients met the inclusion criteria. Among the 43 patients where both eyes were eligible, one eye was randomly chosen for analysis. Baseline characteristics of the studied patients and eyes are summarized in Table 1. The median inter-scan interval was 8 months, with an inter-quartile range (IQR) of 7 to 10 months. The median LogMAR visual acuity at baseline was 0.18 (IQR 0, 0.3; Snellen equivalent 6/9, IQR 6/6, 6/12). The median CSFT on OCT at baseline was 290 μm (IQR 270 μm, 312 μm). Sixteen eyes (17%) were documented to have clinically significant macular edema (CSME) at the baseline visits. The majority of eyes (98%) had some degree of diabetic retinopathy. Thirty-seven eyes (38%) of the 97 eyes had been previously treated for diabetic eye diseases. Focal/grid laser was the most common treatment.
Visual acuity and OCT outcomes
Over a median inter-scan period of 8 months, there were no statistically significant changes in the cohort’s visual acuity, CSFT, or macular volume (Table 2). Stratification on the basis of previous treatment showed an absence of statistically significant changes in CSFT in both treatment naïve eyes and previously treated eyes.
The change in visual acuity plotted against the change in CSFT over the follow-up period is shown in Fig. 1. Of the 90 eyes with complete visual acuity data, the numbers of eyes with unchanged (change < 0.08 LogMAR, equivalent to < 4 ETDRS letters), deteriorated, and improved visual acuities were 34 (38%), 24 (27%), and 32 (36%), respectively. The percentages of eyes maintaining, losing, and gaining vision were similar between treatment naïve eyes and previously treated eyes. Additionally, there was no significant difference in the change in visual acuity between treatment naïve eyes and non-treatment naïve eyes.
Scatter plot demonstrating the distribution of change in visual acuity against the change in CSFT on OCT from baseline. The dotted lines represent the upper and lower limits of stable visual acuity (− 0.08 to 0.08 LogMAR, equivalent to − 4 to 4 ETDRS letters), and the upper and lower limits of stable CSFT (− 25 μm to 25 μm). Abbreviations: CSFT, central subfield thickness; ETDRS, Early Treatment Diabetic Retinopathy Study; LogMAR, logarithm of the minimum angle of resolution; OCT, optical coherence tomography
Three eyes in the study were treated with intravitreal bevacizumab 9 months, 10 months, and 42 months prior to the initial visits, respectively. One eye that received intravitreal bevacizumab 9 months prior to the baseline visit lost the equivalent of 1 ETDRS letter in visual acuity, with increase in CSFT from 295 to 311 μm over a period of 9 months. Another eye had intravitreal bevacizumab 10 months before the baseline visit showed a slight reduction in CSFT from 298 to 286 μm with unchanged visual acuity (0.3 LogMAR on both visits) over 6 months of observation. Three eyes received intravitreal triamcinolone, 24 months, 7 months, and 40 months prior to the initial visits. The CSFT of the eye that received intravitreal triamcinolone 7 months prior to the baseline visit decreased from 281 to 277 μm, and the visual acuity of this eye improved 9 ETDRS letters (0.18 LogMAR) over 9 months. Data on the eyes that received intravitreal bevacizumab 42 months, and intravitreal triamcinolone 24 months and 40 months prior to the initial visits were not shown as the treatment was too distant to have meaningful impact on visual acuity or CSFT during the study period.
Of the 90 eyes with complete visual acuity data, the 12 eyes (13%) that had lost more than the equivalent of 9 ETDRS letters (0.18 LogMAR) during the study interval were further analyzed. Four of these eyes had OCT evidence of worsening DME, which upon evaluation of the clinical records was believed to have resulted in the decrease in visual acuity (Table 3). Of these four eyes, three were treated and one was not, since it had maintained excellent visual acuity. Visual recovery was achieved in all three eyes that had been treated. Seven of the 12 eyes that had loss of equivalent of 9 ETDRS letters (0.18 LogMAR) were naïve to intravitreal anti-VEGF and steroid. None of the other eyes had received an intravitreal injection in our hospital, and furthermore had no record of having received treatment elsewhere.
Factors associated with change in CSFT
The numbers of eyes with increased (≥ 25 μm), unchanged (within 25 μm of baseline), or decreased (≤− 25 μm) central subfield thicknesses were 16 (16%), 74 (76%), and 6 (6%), respectively. The three groups were compared with respect to baseline ophthalmic and medical factors. There was strong evidence that baseline CSFT was associated with change in CSFT (P = 0.001, Table 4 left panel). Post hoc pairwise analysis suggested that the difference between the decreased and unchanged groups was responsible for the overall significance. The baseline CSFT of the decreased CSFT group was significantly thicker. With respect to the duration of diabetes, we found in pairwise comparisons that there were differences between the decreased CSFT group and the increased CSFT group, and between the decreased CSFT group and the unchanged CSFT group (P = 0.002, Table 4 right panel). Patients whose maculae demonstrated a reduction in CSFT had a shorter history of diabetes.
In analyzing the relationship with HbA1c, we combined the decreased CSFT group and the unchanged CSFT group, since we only had HbA1c data for 2 eyes with decreased CSFT. HbA1c of the increased CSFT group was significantly higher than the combined unchanged and decreased CSFT group (P = 0.01, Fig. 2a). A receiver operating characteristic (ROC) analysis was conducted to determine the value of HbA1c that best predicted an increase of CSFT on OCT. The area under the ROC curve was 0.75 (95% CI 0.59–0.90, P = 0.005). An HbA1c of 8.5% may be used as a cut-off to indicate the risk of central subfield thickening on OCT, with 71.4% sensitivity and 64.3% specificity (Fig. 2b). No significant association was found between CSFT and any of the other demographic, medical, or ophthalmic factors listed in the methods section of this report.
a Boxplot showing the distribution of hemoglobin A1c in the increased CSFT group (≥ 25 μm) and the combined stable and decreased CSFT group (< 25 μm from baseline) (mean: solid line, 25th to 75th percentiles: extremes of the box, 10th to 90th percentiles: whiskers, outliers: circles). b Receiver operating characteristic curve for predicting central subfield thickening on OCT. In the study cohort, the AUC for the use of HbA1c to predict an increase in CSFT for ≥ 25 μm on OCT was 0.75 (95% CI 0.59–0.90, P = 0.005). The optimal cut-off was HbA1c of 8.5%, which had a sensitivity of 71.4% for predicting a CSFT increase of ≥ 25 μm on OCT and a specificity of 64.3%. Abbreviations: AUC, area under the curve; CSFT, central subfield thickness; OCT, optical coherence tomography
Due to the small number of eyes in the decreased CSFT group, it was combined with the unchanged CSFT group for multivariable analysis. A binomial logistic regression was conducted to ascertain the relative effects of age in addition to the factors that had been found to be significant in univariable analyses: HbA1c, duration of diabetes, and baseline CSFT. Tests for multicollinearity demonstrated a lack of collinearity between the independent variables. HbA1c was modeled as a categorical variable using 8.5% as the cut-off as derived from the ROC analysis. Of the four factors, only HbA1c had a significant correlation with the change in CSFT. The regression model suggested that patients with HbA1c of 8.5% or greater were 5.7 times more likely to have an increase in CSFT of at least 25 μm on OCT over the study period (95% CI 1.1–30.1, P = 0.038, Nagelkerke R2 = 0.33).
Further analyses were performed in order to better understand the results of the multivariable analysis. Stratifications were performed to assess for effect modification, which was demonstrated between HbA1c and baseline CSFT. In eyes with baseline CSFT of 290 μm or greater, HbA1c of 8.5% or higher was associated with an increased risk of central subfield thickening of 25 μm or greater (RR 9.23, 95% CI 1.25–68.11, P = 0.008, Table 5), whereas it appeared not to influence eyes with baseline CSFT of less than 290 μm. Effect modification was not found in other pairs of variables included in the multivariable analysis.
In this study, we have included eyes of patients who received intravitreal anti-VEGF in their contralateral eyes during the study period. Of the 97 eyes included in our study, a total of 16 received intravitreal anti-VEGF injections in their non-study eyes: 11 received intravitreal bevacizumab; 3 had intravitreal bevacizumab at the time of cataract surgery; 1 received intravitreal bevacizumab and triamcinolone at the time of cataract surgery; 1 received intravitreal aflibercept. There was no statistically significant difference in the change in CSFT between the eyes with contralateral intravitreal anti-VEGF use during the study period and those without contralateral intravitreal anti-VEGF use (P = 0.58). Therefore, it was unlikely that the inclusion of patients who received intravitreal anti-VEGF in the contralateral eyes would affect the overall trend of CSFT in our study.
Discussion
Our study looked to determine retrospectively the natural history of DME in untreated eyes. In some cases, the DME was not treated due to lack of center involvement or since it was not associated with significant symptoms. In others cases, patients were on the waiting list for cataract surgery combined with intra-operative DME treatment or opted to be treated only in the contralateral eye which had more severe disease. It should be stressed that this occurred in an environment where the default position was for all center-involved DME to be proactively treated. As a result, there was a spectrum of severity of DME included in the study. Eyes were included in the study based on the presence of morphological characteristics of DME on OCT imaging. An eye was deemed to have DME if retinal thickening from intra-retinal cysts, fluid or lipid exudates typical of DME was present on OCT without indicators of an alternative etiology. Eyes were included into the study irrespective of the location or severity of DME on OCT, and independent of evidence of DME from clinical examination.
Four previous natural history studies of OCT changes in DME have focused on the rate of DME progression to reach various binary outcomes. A retrospective study showed that over a period of 14 months, 48 of the 153 eyes (31%) with subclinical DME (defined as an abnormal thickness profile on OCT without clinical evidence of CSME) progressed to CSME that, in the opinion of the treating clinicians, required treatment [4]. In a Diabetic Retinopathy Clinical Research Network (DRCR.net) study, the probability of an eye developing a significantly increased CSFT (an increase of at least 50 μm from baseline on Stratus OCT) or judged by clinicians to warrant treatment for DME by 1 year and by 2 years were 27% and 38%, respectively [5]. In one European study, 5 out of 48 eyes (10%) with baseline subclinical DME (defined as CSFT between 260 and 290 μm in women and between 275 and 305 μm in men on Cirrus OCT) developed CSME after 12 months [6]. Another European study reported that 6 out of 32 eyes (19%) with subclinical DME (defined as center point thickness between 225 and 299 μm on Stratus OCT without foveal edema on slit-lamp exam) at baseline progressed to CSME over the course of 24 months, while only 20 out of 316 eyes (6%) without subclinical DME at baseline progressed to CSME, suggesting that subclinical DME is a predictive factor of progression to CSME [7]. Despite the different definitions for subclinical DME used, these studies have unanimously demonstrated that DME tends to progress slowly.
Our outcome measures were defined on the basis of change in OCT and visual acuity parameters, rather than by binary outcomes such as progression to CSME or by reaching a certain threshold of retinal thickening. Since all our patients were assessed with a spectral domain machine with greater resolution and better inter-test reliability, we elected to use a pre-specified change of at least 25 μm in the central subfield as the threshold. Previous work has demonstrated that changes of 12 μm or greater in CSFT on spectral domain OCT represent real changes [8]. In our study, 25 μm was greater than half of the IQR of the cohort’s baseline CSFT. Other studies that have assessed absolute magnitude of CSFT change used 37 μm [4] or 50 μm [5] when using the time-domain Stratus OCT (Carl Zeiss Meditec., Dublin, California, USA) as the threshold of significance.
Our data suggested that there was no significant overall change in the median CSFT on OCT over a median duration of 8 months, and thus provided additional confirmation that DME tends to progress slowly. A significant proportion of eyes (76%) had stable central subfield thicknesses with changes of less than 25 μm from baseline over the study period. Furthermore, greater baseline CSFT was not a risk factor for worsening of CSFT. In fact, eyes with greater CSFT were more likely to demonstrate a spontaneous reduction in CSFT.
Over a period of 6 to 12 months, 27% of the 90 eyes with visual acuity data had losses equivalent of at least 4 ETDRS letters (0.08 LogMAR), while 36% of the eyes improved by at least 4 ETDRS letters equivalent and 38% had changes of less than the equivalent of 4 ETDRS letters from baseline. In the previously mentioned DRCR.net study, 38% of the eyes that progressed from subclinical DME to clinically apparent macular edema or to requiring treatment lost 5 or more letters in less than 2 years [5]. In our study, 12 eyes (13%) had visual acuity loss that was equivalent of at least 9 ETDRS letters (0.18 LogMAR). Progression of DME accounted for visual decline in 4 out of the 12 eyes over a median duration of 8 months. Reassuringly, all 3 eyes that were treated demonstrated a return to baseline or better visual acuity (Table 3). One eye was left untreated and maintained visual acuity of 0.0 LogMAR (6/6 Snellen equivalent). While other studies have shown that eyes with baseline subclinical DME experienced a significant decrease in best-corrected visual acuity over a period of 2 years compared to those without [7], in our cohort, no eye suffered significant irreversible visual loss due to DME.
Major epidemiologic studies have shown that diabetes patients with higher glycosylated hemoglobin have an increased risk of developing DME and CSME [9,10,11]. Other studies have not shown a correlation [4, 12, 13]. Our study found that patients with higher HbA1c were more likely to develop increased CSFT. Patients with HbA1c measurements of 8.5% or greater were 5.7 times more likely to develop CSFT thickening of at least 25 μm over the study period. This effect was particularly pronounced in eyes with a baseline CSFT of 290 μm or greater. This may have value in determining frequency of follow up of patients with untreated DME.
Hikichi et al. found that patients with persistent CSME had significantly longer duration of type 2 diabetes as compared with those whose CSME spontaneously resolved [13]. In our study, a shorter history of diabetes was associated with spontaneous reduction in CSFT in univariable analysis. However, the effect of diabetes duration did not reach statistical significance in the multivariable analysis.
Our study was limited by the retrospective design as well as the sample size. Randomization was used to select eyes for statistical analysis to minimize data dependency issues that would have resulted from inclusion of both eyes of some patients. The study interval was restricted to 6 to 12 months. As such, discussion of the progression of DME outside of the 6 to 12 months time frame is beyond the scope of this study.
Conclusion
Our study suggested that the majority of eyes with DME identified on OCT had stable central subfield thicknesses in the absence of treatment over a median duration of 8 months. Approximately a quarter of the eyes experienced a meaningful decrease in visual acuity during this period. However, a 6- to 12-month follow-up interval seemed unlikely to miss the window for successful intervention for eyes with reduced visual acuity related to DME progression. A hemoglobin A1c of 8.5% or higher was associated with an increased risk of the development of thickening in the central subfield on OCT, particularly in patients with baseline CSFT of greater than or equal to 290 μm. Consideration of these risk factors may be of value in determining monitoring intervals.
Abbreviations
- CSFT:
-
Central subfield thickness
- CSME:
-
Clinically significant macular edema
- DME:
-
Diabetic macular edema
- DR:
-
Diabetic retinopathy
- DRCR:
-
Diabetic Retinopathy Clinical Research
- ETDRS:
-
Early Treatment Diabetic Retinopathy Study
- HbA1c:
-
Hemoglobin A1c
- LogMAR:
-
Logarithm of the minimum angle of resolution
- OCT:
-
Optical coherence tomography
- VA:
-
Visual acuity
- VEGF:
-
Vascular endothelial growth factor
References
Das A, McGuire PG, Rangasamy S (2015) Diabetic macular edema: pathophysiology and novel therapeutic targets. Ophthalmology. 122(7):1375–1394
Johnson MW (2009) Etiology and treatment of macular edema. Am J Ophthalmol 147(1):11–21.e1
Mitchell P, Wong TY (2014) Management paradigms for diabetic macular edema. Am J Ophthalmol 157(3):505–13.e8
Browning DJ, Fraser CM (2008) The predictive value of patient and eye characteristics on the course of subclinical diabetic macular edema. Am J Ophthalmol 145(1):149–54. e3
Diabetic Retinopathy Clinical Research Network, Bressler NM, Miller KM, Beck RW, Bressler SB, Glassman AR et al (2012) Observational study of subclinical diabetic macular edema. Eye (Lond) 26(6):833–840
Tejerina AN, Vujosevic S, Varano M, Egan C, Sivaprasad S, Menon G et al (2015) One-year progression of diabetic subclinical macular edema in eyes with mild nonproliferative diabetic retinopathy: location of the increase in retinal thickness. Ophthalmic Res 54(3):118–123
Pires I, Santos AR, Nunes S, Lobo C, Cunha-Vaz J (2013) Subclinical macular edema as a predictor of progression to clinically significant macular edema in type 2 diabetes. Ophthalmologica. 230(4):201–206
Fiore T, Androudi S, Iaccheri B, Lupidi M, Fabrizio G, Fruttini D et al (2013) Repeatability and reproducibility of retinal thickness measurements in diabetic patients with spectral domain optical coherence tomography. Curr Eye Res 38(6):674–679
Klein R, Klein BEK, Moss SE, Cruickshanks KJ (1995) The Wisconsin epidemiologic study of diabetic retinopathy XV. Ophthalmology. 102(1):7–16
Klein R, Klein BEK, Moss SE, Davis MD, DeMets DL (1984) The Wisconsin epidemiologic study of diabetic retinopathy. Ophthalmology 91(12):1464–1474
Yau JW, Rogers SL, Kawasaki R, Lamoureux EL, Kowalski JW, Bek T et al (2012) Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care 35(3):556–564
Chew EY, Davis MD, Danis RP, Lovato JF, Perdue LH, Greven C et al (2014) The effects of medical management on the progression of diabetic retinopathy in persons with type 2 diabetes. Ophthalmology. 121(12):2443–2451
Hikichi T, Fujio N, Akiba J, Azuma Y, Takahashi M, Yoshida A (1997) Association between the short term natural history of diabetic macular edema and the Vitreomacular relationship in type II diabetes mellitus. Ophthalmology. 104(3):473–478
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human participants and/or animals
All procedures performed in studies involving human participants were in accordance with the ethical standards of the National Statement on Ethical Conduct in Research 2007, The Melbourne Health Quality Assurance/Negligible Risk Research Project, and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
This article does not contain any studies with animals performed by any of the authors.
No informed consent was sought from patients in this study as only patient records that were accessible to medical professionals were obtained and collected for this study in a non-identifiable manner. In addition, no patient contact was required for this study, and outcomes for patients were not affected by the study due to its retrospective nature.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, H., Tan, M.H., Pomerleau, D. et al. Optical coherence tomography analysis of patients with untreated diabetic macular edema. Graefes Arch Clin Exp Ophthalmol 258, 653–661 (2020). https://doi.org/10.1007/s00417-019-04549-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-019-04549-y