Abstract
Purpose
To assess the effectiveness of intra-arterial chemotherapy (IAC), intravenous chemotherapy (IVC), and their combination in the management of group D retinoblastoma.
Methods
This was a retrospective, interventional, comparative, and non-randomized clinical study, including all eyes with primarily treated group D retinoblastoma managed in a single institution from February 2010 to July 2016. Patient demographics, treatment modality (primary enucleation, intravenous chemotherapy, intra-arterial chemotherapy alone or intravenous, and intra-arterial chemotherapy), additional need for consolidation treatments or intravitreal melphalan (IVM) injections, and follow-up time were recorded. The main outcome measure was ocular survival rate after various treatment modalities.
Results
Of 87 eyes of 83 consecutive cases, 9 eyes (10.3%) were primarily enucleated, 37 (42.6%) eyes received IVC, 30 (34.5%) eyes had IAC, and 11 (12.6%) eyes were treated with IVC followed by IAC. After a mean 81.1 ± 75.2 weeks of follow-up, enucleation rates were 56.8% in the IVC group, 23.3% in the IAC group, and 36.6% in the IVC + IAC group (p = 0.021). There was no significant difference of ocular survival estimates among these 3 groups at 2 or 5 years (p = 0.998, p = 0.986). With logistic regression analysis, age; gender; disease laterality; administration of IVM, TTT, or cryotherapy; mean dose of IVM; follow-up time; and number of IAC or IVC cycles were not significantly related to the enucleation rate (p > 0.05 for all variables).
Conclusions
Our experience showed that in group D patients, primary IAC achieved ocular survival in 76.7% of eyes, and less need for local consolidation treatments, whereas following primary IVC ocular survival was 43.2%.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The International Classification of Retinoblastoma (ICRB) as originally described by Murphree [1] defines group D as eyes with diffuse vitreous or subretinal seeding and/or massive, nondiscrete endophytic, or exophytic disease. This massive and/or diffuse intraocular disseminated tumor may consist of fine or greasy vitreous seeding or avascular masses, which is now designated as vitreous clouds, and plaque-like subretinal seeding [1, 2]. There may be more than one quadrant of retinal detachment [1]. Because of all these features, group D retinoblastoma is the most difficult to treat among other groups if the aim is to preserve a functional eye. Moreover, embarking on the best treatment option in unilateral group D eyes, which constituted 29% of all unilateral cases in one large series, is even further complicated and requires solid data and expertise [3]. Currently, there is no controversy in the treatment of group A, B, and C eyes. Group A tumors are treated with transpupillary thermotherapy (TTT) if they are posterior to the equator or with cryotherapy if they are anterior to the equator. For group B and C eyes, either intravenous chemotherapy (IVC) or intra-arterial chemotherapy (IAC) results in an almost 100% ocular survival rate [4, 5]. On the end of the spectrum, there are eyes with group E tumors, which are more advanced and 24 to 50% of which may harbor high-risk features, including post-laminar tumor invasion, massive choroidal invasion, or extrascleral extension [6, 7]. Again, the treatment decision here is often straightforward as the majority of group E eyes are still primarily enucleated in most centers worldwide. However, early results of a recent study on a small number of patients showed that in short term, 48% of eyes with group E tumors were salvaged with IAC [3].
Several studies have already evaluated the management of group D eyes with various modalities including primary IVC, first-line IAC, and the combination of IAC and IVC with the addition of intravitreal chemotherapy, and other focal treatments as consolidation therapies [8,9,10,11]. In this study, we retrospectively analyzed the outcomes of current treatment approaches specifically directed to group D eyes at a major referral center, in order to determine from which modality the children benefited the most in terms of ocular survival and least adverse effects.
Methods
This was a retrospective, interventional, comparative, and non-randomized single-center clinical study on patients with primarily treated group D retinoblastoma in at least one eye, who were diagnosed and managed at our institution between February 2010 and July 2016. Patients previously treated elsewhere were excluded from further analyses. The treatment decisions were made on a case-to-case basis. The study adhered to the tenets of the Declaration of Helsinki, as amended in 2008. The study was approved by the ethical committee of Hacettepe University (number: GO 16/204–06).
Collected demographic data included patient age at presentation, gender, and laterality of the tumor. Retrieved clinical data included presence, extent, and types of vitreous seeding (dust, sphere, and cloud), subretinal seeding, and associated retinal detachment [2]. The tumors were classified according to Los Angeles version of the ICRB [1].
B-mode ultrasonography was performed on each eye at every examination. In compliance with the protocols of our institution, cranial and orbital magnetic resonance imaging studies were performed once at initial diagnosis in all patients with bilateral tumors, and in patients with group D and E eyes, and only if extraocular disease was suspected thereafter. Ophthalmological examinations were carried out under general anesthesia 2 to 4 weeks apart. All available wide-angle contact fundus camera (RetCam, Clarity Medical Systems, Pleasanton, CA) and ultrasonographic recordings were also reviewed.
Initially, all bilateral cases, tumors associated with total retinal detachment and patients under the age of 6 months were primarily treated with IVC. Standard intravenous (systemic) chemotherapy included vincristine (0.05 mg/kg), etoposide (5 mg/kg), and carboplatin (18–20 mg/kg) given in 6 cycles, each 3 to 4 weeks apart via a central venous line. For patients below the age of 6 months, 50% of the standard dose was prescribed. The decision to switch to IAC was made if less than 20% reduction in tumor size was obtained or if progression was observed after 4 cycles of IVC. For IAC, melphalan (5–7.5 mg) and/or topotecan (1 mg) were used. Focal consolidation treatments in the form of cryotherapy and/or TTT, depending on the location of the tumor, were delivered between IAC or IVC cycles to consolidate non-calcified tumor remnants and type II tumor responses. Beginning from 2012, intravitreal melphalan (IVM) injections with a dose ranging from 25 to 45 μg were used to control intravitreal and subretinal seeding until all visible seeds became calcified or disappeared. These injections were repeated at 2-week intervals between IVC or IAC cycles. Mean follow-up time was defined as the time from initial diagnosis until the last visit or the time of enucleation (if performed), whichever occurred first. Mean follow-up time after last treatment was defined as the time from the last treatment (IAC, IVC, or consolidation) until the time of last visit even if enucleation had been performed in the meantime. If a patient was treated with only IVC or only IAC in the first 3 months after diagnosis, then this patient was classified under either primary IVC or primary IAC groups. If a patient had received both modalities any time within the first 3 months following diagnosis, then it was considered a combination therapy. Pathology reports were reviewed to assess the presence of histopathological high-risk factors [6]. At our institution, we recommend 2–4 cycles of systemic chemotherapy if these high-risk factors are documented on the enucleation specimens. We did not report on visual acuity in this study because most patients were preverbal and very few reliable Snellen measurements were available.
Statistical analyses were performed with SPSS version 21.0 (IBM Corp, Armonk, NY) and included descriptive statistics, chi-square test for comparison of frequencies, and ANOVA for that of means among treatment modalities. After computing kurtosis and skewness, parametric analyses were performed for data with normal distribution. Logistic regression analysis was used to determine the factors leading to enucleation. After chi-square test and ANOVA, pairwise comparisons were applied where p values were lower than 0.05. Kaplan-Meier curves were generated to assess ocular survival at 2 and 5 years in the whole cohort, and Mantel-Cox test was used to compare ocular survival rates among IVC, IAC, and IVC + IAC groups. All p values less than 0.05 were considered statistically significant. The main outcome measure was ocular survival rate after various treatment modalities.
Results
Between February 2010 and July 2016, 336 patients with retinoblastoma were treated at our ocular oncology service. The study involved 87 eyes of 83 consecutive patients with group D retinoblastoma, which constituted 24.7% of all retinoblastoma patients. Of 83 patients, 38 (45.8%) were female and 45 (54.2%) were male. At presentation, 30 patients (36.1%) had bilateral disease with at least one eye having group D retinoblastoma and 4 patients (4.8%) had bilateral group D retinoblastoma. Mean age at diagnosis was 19.2 months (range: 1–144 months) (Table 1). Nine eyes (10.3%) were primarily enucleated shortly after the diagnosis. Reasons for enucleation were parents’ request, strictly unilateral tumors in older patients, and no future potential for any useful vision. Only one (11.1%) of these eyes displayed a histopathological high-risk factor, which was massive choroidal invasion.
At our institution, we started to offer IAC in 2010, until when, all patients with group B, C, and D tumors were treated uniformly with IVC. During the period subject to this study, we were able to diversify the treatment of retinoblastoma. Initially, all bilateral cases, regardless of the group of the fellow eye, eyes with total retinal detachment and patients younger than 6 months of age were managed with primary IVC. Later, as we gained experience with IAC, more bilateral cases and tumors associated with total retinal detachment were managed with this modality and the age limit was lowered to 4 months. Seventy-eight eyes (89.7%) were primarily treated conservatively and pertaining data are summarized in Tables 2 and 3. There were 3 treatment groups; 37 (42.6%) eyes received IVC, 30 (34.5%) eyes had IAC, and 11 (12.6%) eyes were first treated with IVC followed by IAC. The reasons for switching to IAC after IVC were either to implement the “bridge therapy” [12] in one infant younger than 3 months of age and incomplete tumor regression after IVC with 4 cycles of chemotherapy given in 3 months. Patients with documented progression despite 4 cycles of IVC were offered enucleation. The mean number of IAC was 2.4 (range: 1–11) and the mean number of IVC cycles was 6.3 (range: 1–16). Among the treatment groups, IAC patients had the highest mean age (25.2 months), which was statistically significant (p = 0.001) and IVC patients had the youngest age (7.2 months, p = 0.005), compared to IVC + IAC group. Highest bilaterality rate was observed in the IVC group (65.7%, p < 0.001). Also, there was a tendency to treat patients with multifocal tumors with IVC although this did not reach statistical significance (p = 0.094).
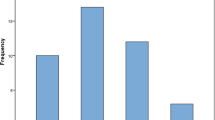
As for local consolidation treatments, 19 eyes (21.8%) received TTT and 13 eyes (14.9%) had cryotherapy. Intravitreal melphalan was given to 31 eyes (35.6%) with a mean number of 2.3 (range: 1–5) injections and a mean dose of 31.5 μg (range: 25–45 μg) per injection. Mean number of injections and dose of IVM were statistically similar in all groups. However, more eyes in the IVC group received overall consolidation treatments and more frequently than other groups (66.7%, p = 0.018). When enucleation rates were compared according to presence of IVM treatment, no statistically significant difference was found between eyes that received IVM and those that did not (42.9 vs. 54.8%, p = 0.284). This was also recognized in each treatment subgroup (p = 0.315 for IVC, p = 0.208 for IAC, and p = 0.554 for IVC + IAC, respectively). Mean follow-up time was 81.1 ± 75.2 weeks (median: 58 weeks) and 41 eyes (47.1%) were finally enucleated. Kaplan-Meier estimates revealed overall 67.3 and 20.0% eye survival rates at 2 and 5 years, respectively (Fig. 1). Even though chi-square test showed higher enucleation rate in the IVC group compared to others (56.8%, p = 0.021), using Mantel-Cox test in both 2-year and 5-year Kaplan-Meier curves separately, statistically, similar eye survival rates were encountered among IVC, IAC, and IVC + IAC groups (p = 0.998, p = 0.986). Eight patients (9.1%) had orbital recurrence of the disease (Table 4). Although six of these were in the IVC group, the frequency for orbital recurrence was similar among all groups without any difference attaining statistical significance (p = 0.552). Five (62.5%) of those also had IVM injections (range: 1–5 injections). In four eyes (50%), the tumor was totally obscuring the optic nerve head at the time of enucleation. Histopathological high-risk factors were present in five (62.5%) eyes. Retrospectively, none of these patients had any evidence of extraocular extension or optic nerve thickening on MRI scans at initial evaluation. Mean time from enucleation to orbital recurrence was 8.9 months. All patients with orbital recurrence received additional 6 cycles of high-dose IVC followed by fractionated 4500 cGy external beam radiation therapy. Three patients underwent orbital exenteration. Logistic regression analysis of age; gender; laterality of the disease; administration of IVM, TTT, or cryotherapy; mean dose of IVM; follow-up time; number of IAC or IVC cycles; and enucleation rate revealed no significant relation between enucleation rate with any of the listed variables (p > 0.05 for all variables).
In the IVC group, the most common severe complications that we encountered were widespread chorioretinal atrophy (five patients), and vitreous hemorrhage (three patients). The latter occurred following IVM and resolved spontaneously within 12 weeks in all cases. Patients who developed large areas of chorioretinal atropy in the IVC group received chemotherapy ranging between 6 to 10 cycles and had to be treated later with IAC (1–4 cycles). In all these eyes previously treated with IVC, we observed that chorioretinal atrophy rapidly developed following the first IAC. In the IAC group, there were permanent frontal alopecia in two patients, widespread chorioretinal atrophy in three eyes (after 1, 2, and 2 cycles respectively), vitreous hemorrhage following IVM in four eyes, and arrested ocular growth in two eyes. In the IVC + IAC group, two eyes developed extensive chorioretinal atrophy (after 2 IVC + 1 IAC and 1 IVC + 3 IAC cycles, respectively). One child developed bone metastases after the third IAC and was subsequently treated with systemic chemotherapy. There was no prior or concurrent orbital recurrence in this patient. There has been no recorded death in the whole cohort of group D patients up to the writing of this report.
Discussion
The optimum management of group D eyes continues to be controversial but the current trend evolves more in favor of conservative modalities. A recent international survey involving 1807 group D eyes revealed the divided opinion among experts, whose first choice was systemic chemotherapy in 53% of cases and primary enucleation for 27% of eyes [13].
Systemic chemotherapy was the treatment paradigm for almost two decades before the advent of IAC. For group D eyes, the best achieved globe salvage rate with IVC using 6 to 9-cycle regimens was 47%, which decreased to 30% if diffuse vitreous seeds were present [4]. Munier et al. [10] reported 57% ocular salvage rate at 5 years using 3 cycles of chemotherapy. A recent study on 104 eyes, primarily managed by IVC, documented that 95% of eyes required additional TTT and/or cryotherapy, 31% required IAC, and 6% required IVM [9]. All these resulted in 59% globe salvage rate at 5 years [9]. In our primary IVC cases, 66.7% of eyes needed additional local treatments. Berry et al. [14] observed that 53% of group D eyes managed with chemoreduction and consolidation therapies had recurrences or persistent active tumors. They were able to salvage an additional 35% of these eyes by implementing low-dose (36 Gy) intensity modulated radiotherapy [14]. In our IVC group, 64.5% of eyes continued to produce new tumors, and they were further treated with IAC, which salvaged only an additional 12.5% of these eyes. Our overall ocular survival rate in the primary IVC group was 43.2%.
IAC has recently become the standard first-line treatment of retinoblastoma, except for group A tumors in all major retinoblastoma sites worldwide [3, 5]. Several studies found 85 to 94% globe salvage rates using IAC for group D eyes, far more superior than that were achieved with IVC [3, 8, 10, 11, 15, 16]. Compared to IVC, IAC produced significantly better results in controlling vitreous seeds (25 vs. 74%), solid tumors (62 vs. 92%), and subretinal seeds (31 vs. 86%) [3]. Munier et al. [10] observed that faster and more extensive tumor control with less side effects was obtained with IAC. Compared to IVC, consolidation requirement was less, relapse was less frequent (24 vs. 52%), and recurrences occurred earlier with IAC [10]. We similarly observed that TTT and cryotherapy were significantly less necessary (p = 0.018) in our IAC group, and the ocular survival was 76.7% compared to 43.2% of our IVC group. While more successful in the primarily treated group D eyes, IAC also proved effective in previously failed group D eyes [16, 17]. Shields et al. [17] thwarted enucleation in 67% of six group D eyes unresponsive to IVC, and Abramson et al. [16] achieved globe preservation in 58.4% of previously treated eyes at 5 years. In our patients who had failed previous IVC and then receiving secondary IAC, the ocular survival rate was 60%.
Primary enucleation may still be preferred for selected group D eyes. We recommended primary enucleation for unilateral group D tumors presenting at older age and for eyes without any prospect for a useful vision. Similarly, in a small subset of eyes, another circumferential justification for enucleation may come from the fact that histopathological high-risk features may be present in 13–17% of group D eyes [7, 18]. Some clinical features, including old age, unifocal foveal tumor, subretinal seeds, exophytic growth pattern, and obscuration of the disc by the tumor were identified be in associated with high-risk features [18, 19]. These eyes may warrant early consideration for enucleation. There are conflicting reports regarding the effects of conservative treatments on high-risk features and the subsequent development of orbital recurrence. Berry et al. [20] suggested that enucleation after failed 6 cycles of IVC was safe in terms of orbital recurrence compared to primary enucleation in group D eyes. In contrast, Zhao et al. [21] found that IVC before enucleation might cause pathological downstaging in group D tumors and might mask some high-risk features. In our series, 75% of orbital recurrences developing after conservative treatments were in the IVC group and 50% of this particular IVC group had histopathological high-risk features, although there was no statistically significant difference between other groups. We found that persistent vitreous seeding and obscuration of the optic disc by the tumor were the most common clinical signs, and these should have alerted us for advising earlier enucleation rather than insisting on conservative modalities. We believe that microscopic invasion must always be suspected when the tumor covers the optic nerve head even if it looks clinically inactive. Orbital MRI has a sensitivity of 60% in detecting massive choroidal and post-laminar invasion [7], and in our patients, it was only in the final stage that MRI was suggestive of optic nerve involvement.
Ocular side effects of IVC are few if any and most often transient. We have observed chorioretinal atrophy emerging after administration of IAC in the failed IVC group, which was disturbing, since this had an adverse impact on the visual acuity and some children developed esotropia. Following IAC, significant retinal pigment epithelial changes were documented in 47% of eyes [22], and severe chorioretinal atrophy developed in 16.2% of eyes [23]. We may speculate that IAC might have additive toxicity to the already subclinically compromised choriocapillaris and retinal pigment epithelia in certain eyes, but further observation are needed to draw any meaningful conclusion. A study reporting on 14 patients similar to ours, receiving secondary IAC after IVC did not mention this devastating complication [17].
This study has the inherent limitations due to its retrospective nature and relatively small number of patients in each treatment subgroups. Our overall 2-year and particularly the 5-year ocular survival rates (67 and 20%, respectively) are disappointing compared to more favorable results in the literature. This may partly be explained by our low primary enucleation rate, which is due to cultural elements prevailing in the population we serve dictating avoidance of enucleation until the last limit. We should have enucleated more eyes initially instead of insisting on IVC or IAC, which would unlikely produce favorable results. Still, however, this retrospective review of our experience with group D eyes allowed us to modify our approach in the way that we currently offer IAC as the first-line treatment for the majority of cases except for infants younger than 4 months of age, along with the more liberal use of intravitreal chemotherapy (results reported elsewhere). We observed that with primary IAC, we were able to achieve 76.7% globe salvage rate, with less need for consolidation treatments and less side effects.
References
Murphree LA (2005) Intraocular retinoblastoma: the case for a new group classification. Ophthalmol Clin N Am 18:41–53
Munier FL (2014) Classification and management of seeds in retinoblastoma. Ellsworth Lecture Ghent August 24th 2013. Ophthalmic Genet 35:193–207
Shields CL, Jorge R, Say EAT, Magrath G, Alset A, Caywood E et al (2016) Unilateral retinoblastoma managed with intravenous chemotherapy versus intra-arterial chemotherapy. Outcomes based on international classification of retinoblastoma. Asia Pac J Ophthalmol 5:97–103
Shields CL, Mashayekhi A, Au AK, Czyz C, Leahey A, Meadows AT, Shields JA (2006) The International Classification of Retinoblastoma predicts chemoreduction success. Ophthalmology 113:2276–2280
Abramson DH, Marr BP, Brodie SE, Dunkel I, Palioura S, Gobin YP (2012) Ophthalmic artery chemosurgery for less advanced intraocular retinoblastoma: five-year review. PLoS One 7:e34120. https://doi.org/10.1371/journal.pone.0034120.t003
Eagle RC (2009) High-risk features and tumor differentiation in retinoblastoma: a retrospective histopathologic study. Arch Pathol Lab Med 133:1203–1209
Kaliki S, Shields CL, Rojanaporn D, Al-Dahmash S, McLaughlin JP, Shields JA et al (2013) High-risk retinoblastoma based on international classification of retinoblastoma: analysis of 519 enucleated eyes. Ophthalmology 120:997–1003
Abramson DH, Daniels AB, Marr BP, Francis JH, Brodie SE, Dunkel IJ et al (2016) Intra-arterial chemotherapy (ophthalmic artery chemosurgery) for group D retinoblastoma. PLoS One 11:e0146582. https://doi.org/10.1371/journal.pone.0146582
Fabian ID, Stacey AW, Johnson KP, Onadim Z, Chowdhury T, Duncan C et al (2017) Primary intravenous chemotherapy for group D retinoblastoma: a 13-year retrospective analysis. Br J Ophthalmol 101:82–88
Munier FL, Mosiman P, Puccinelli F, Gaillard MC, Stathopoulos C, Houghton S et al (2017) First-line intra-arterial versus intravenous chemotherapy in unilateral sporadic group D retinoblastoma: evidence of better visual outcomes, ocular survival and shorter time to success with intra-arterial delivery from retrospective review of 20 years of treatment. Br J Ophthalmol 101:1086–1093
Shields CL, Manjandavida FP, Lally SE, Pieretti G, Arepalli SA, Caywood EH et al (2014) Intra-arterial chemotherapy for retinoblastoma in 70 eyes: outcomes based on the international classification of retinoblastoma. Ophthalmology 121:1453–1460
Gobin YP, Dunkel IJ, Marr BP, Francis JH, Brodie SE, Abramson DH (2012) Combined, sequential intranevous and intra-arterial chemotherapy (bridge chemotherapy) for young infants with retinoblastoma. PLoS One 7:e44322. https://doi.org/10.1371/journal.pone.0044322
Scelfo C, Francis JH, Khetan V, Jenkins T, Marr B, Abramson DH et al (2017) An international survey of classification and treatment choices for group D retinoblastoma. Int J Ophthalmol 10:961–967
Berry JL, Jubran R, Kim JW, Wong K, Bababeygy SR, Almarzouki H et al (2013) Long-term outcomes of group D eyes in bilateral retinoblastoma patients treated with chemoreduction and low-dose IMRT salvage. Pediatr Blood Cancer 60:668–693
Abramson DH, Fabius AWM, Issa R, Francis JH, Marr BP, Dunkel IJ et al (2015) Advanced unilateral retinoblastoma: the impact of ophthalmic artery chemosurgery on enucleation rate and patient survival at MSKCC. PLoS One 10:e0145436. https://doi.org/10.1371/journal.pone.0145436
Abramson DH, Fabius AWM, Francis JH, Marr BP, Dunkel IJ, Francis JH, Brodie SE et al (2017) Ophthalmic artery chemosurgery for eyes with advanced retinoblastoma. Ophthalmic Genet 38:16–21
Shields CL, Kaliki S, Al-Dahmash S, Rojanaporn D, Leahey A, Griffin G et al (2013) Management of advanced retinoblastoma with intravenous chemotherapy then intra-arterial chemotherapy as alternative to enucleation. Retina 33:2103–2109
Fabian ID, Stacey AW, Chowdhury T, Duncan C, Karaa EK, Scheimberg I et al (2017) High-risk histopathology features in primary and secondary enucleated international intraocular retinoblastoma group D eyes. Ophthalmology 124:851–858
Kashyap S, Meel R, Pushker N, Sen S, Bakshi S, Sreenivas V et al (2012) Clinical predictors of high risk histopathology in retinoblastoma. Pediatr Blood Cancer 58:356–361
Berry JL, Kogachi K, Aziz HA, McGovern K, Zolfaghari E, Murphree LA et al (2017) Risk of metastasis and orbital recurrence in advanced retinoblastoma eyes treated with systemic chemoreduction versus primary enucleation. Pediatr Blood Cancer 64. https://doi.org/10.1002/pbc.26270
Zhao J, Dimaras H, Massey C, Xu X, Huang D, Li B et al (2011) Pre-enucleation chemotherapy for eyes severely affected by retinoblastoma masks risk of tumor extension and increases death from metastasis. J Clin Oncol 29:854–851
Muen WJ, Kingston JE, Robertson F, Brew S, Sagoo MS, Reddy MA (2012) Efficacy and complications of super-selective intra-ophthalmic artery melphalan for the treatment of refractory retinoblastoma. Ophthalmology 119:611–616
Bertelli E, Leonini S, Galimberti D, Moretti S, Tinturini E, Hadjistillanou T et al (2016) Hemodynamic and anatomic variations require an adaptable approach during intra-arterial chemotherapy for intraocular retinoblastoma: alternative routes, strategies, and follow-up. Am J Neuroradiol 37:1289–1295
Funding
This work was supported by the Hacettepe University Scientific Research Coordination Unit. Project No.: 13751.
The sponsor had no role in the design or conduct of this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (name the institution/committee) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Statement of informed consent
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Kiratli, H., Koç, İ., Inam, O. et al. Retrospective analysis of primarily treated group D retinoblastoma. Graefes Arch Clin Exp Ophthalmol 256, 2225–2231 (2018). https://doi.org/10.1007/s00417-018-4051-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-018-4051-4