Abstract
Purpose
To compare the antibiotic susceptibilities and visual acuity (VA) outcomes in endophthalmitis caused by methicillin-resistant (MRSA) versus methicillin-sensitive S. aureus (MSSA).
Methods
The records of 34 cases of S. aureus endophthalmitis at The New York Eye and Ear Infirmary from Jan 1997 to June 2011 were reviewed. Antibiotic susceptibility profiles over time and VA at presentation and at 3, 6, and ≥12 months were recorded. S. aureus isolates were grouped based on oxacillin resistance.
Results
Of the 34 cases, 15 (44 %) were MRSA and 19 (56 %) MSSA. Median presenting VA was hand motions (logMAR 4.0) in both the MRSA and MSSA groups. There was no statistically significant difference in VA between the MRSA and MSSA groups at 3, 6, or ≥12 months. No MRSA isolates were resistant to vancomycin or gentamicin. While over 85 % of MRSA isolates tested for fourth-generation fluoroquinolones were resistant, just 10 % MSSA isolates tested were resistant. There was a trend suggesting an increase in the proportion of MRSA isolates compared to MSSA isolates over the course of the study period.
Conclusions
There was no statistical difference in short- or long-term VA outcomes between the MRSA and MSSA groups at any time point. Resistance to fourth-generation fluoroquinolones was present in over 85 % of MRSA isolates, but just 10 % of MSSA isolates. An increasing proportion of MRSA amongst S. aureus isolates was noted over the course of the study period.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Staphylococcus aureus is a significant cause of acute endophthalmitis, encountered most commonly following cataract surgery at a rate of 0.04 % [1, 2]. S. aureus endophthalmitis can also follow trauma, intravitreal injections [3–5], other ocular surgeries, and septicemia [6, 7]. S. aureus possesses virulence factors that give it the ability to adhere to and invade host tissues, combat the immune system, and resist a variety of antibiotics [8–10]. These factors may be transferred from one organism to another, at which time genes coding for resistance mechanisms to antibiotics such as methicillin and the fourth-generation fluoroquinolones commonly used for post-cataract surgery endophthalmitis prophylaxis may also be conferred upon the receiving organism [11]. Evidence to support this theory can be found in reports of methicillin-resistant S. aureus (MRSA) strains with increased virulence, as has been reported in cases of pneumonia, necrotizing fasciitis, and bacteremia [12–15]. However, while trends towards a worse outcome in cases of MRSA endophthalmitis compared to methicillin-sensitive S. aureus (MSSA) endophthalmitis have been shown, limited sample size and follow-up have prevented this relationship from being firmly established. Such a trend, should it be confirmed, could be due to either inadequate antibiotic prophylaxis due to differences in antibiotic susceptibilities of MRSA as compared to MSSA, or could be due to MRSA possessing more advantageous pathogenesis traits than MSSA. The aim of the current study is to help provide answers to several outstanding questions on this topic: Is there a difference in visual acuity outcomes between cases of MRSA and MSSA endophthalmitis? Is there a difference in the sources of cases of MRSA and MSSA endophthalmitis? What are the resistance patterns of MRSA and MSSA isolates, particularly to commonly used antibiotics such as fourth generation fluoroquinolones and vancomycin? Is MRSA endophthalmitis on the rise? To answer these questions, cases of endophthalmitis from the New York Eye and Ear infirmary over a 13-year period were examined with regard to long-term visual acuity outcome, the source of endophthalmitis, and antibiotic sensitivity.
Materials and methods
A search of the New York Eye and Ear Infirmary Microbiology Department database and corresponding medical records identified 98 cases of patients with S. aureus endophthalmitis between January 1, 1997, and June 1, 2011. Cases were included in the analysis only if visual acuity follow-up was available, since the primary aim of this study was to correlate antibiotic susceptibility (MSSA versus MRSA) with visual outcome. The secondary aim of the study was to report on the antibiotic susceptibility profiles of S. aureus isolates, and other parameters such the source of endophthalmitis and the treatment method employed.
Treatments were either “tap and inject”, specifically, aspiration of a vitreous sample followed by intravitreal antibiotic injection (antibiotic chosen by provider, but usually consisting of vancomycin and ceftazidime with occasional inclusion of dexamethasone), or pars plana vitrectomy (PPV) followed by intravitreal delivery of antibiotic. There was no standardized therapeutic algorithm, and therapy was at the discretion of the treating physician.
Intraocular specimens from each patient were obtained from either vitreous needle aspiration during a tap-and-inject procedure or through pars plana vitrectomy (PPV). Vitreous samples were plated on thioglycolate, blood, chocolate, anaerobic blood, and Sabouraud agar and were incubated at 37 ° C. All isolates were incubated for at least 18 to 24 hours in a carbon dioxide incubator. Cultures were observed daily for up to 7 days for visible growth. Vitek automated microbial identification and susceptibility testing system (bioMérieux, Inc, Durham, NC, USA) or disc diffusion testing were used to determine and compare susceptibility patterns. Interpretations of culture results were in accordance with guidelines from the Clinical Laboratory Standards Institute (Wayne, PA, USA). Isolates were determined to be MRSA vs MSSA based on their resistance (MRSA) or sensitivity (MSSA) to oxacillin according to the CLSI standards at the time of isolation.
To establish S. aureus as the causative organism, growth of the organism had to be present on two or more culture media, or semiconfluent growth on one or more solid media. Cases with polymicrobial growth were excluded from the analysis.
Data collected included source of endophthalmitis, gender, age, and time from inciting event to initial presentation when available. Visual acuity (VA) was recorded at presentation, as well as 3 months, 6 months, and ≥12 months after treatment. For statistical analysis, Snellen VA was converted into logMAR units to allow for statistical comparison. VA outcomes were compared between MRSA and MSSA cohorts at each time point and within each cohort between presentation and each subsequent time-point. Treatment choice (PPV vs tap and inject) was also compared between the MRSA and MSSA groups.
Statistical analysis was performed using Graph Pad Prism software (Graph Pad Software, Inc, La Jolla, CA, USA). Student t-test was used for analyzing variables with Gaussian distribution. Sampling distribution was analyzed using chi-square test.
To report on the rates of MRSA and MSSA endophthalmitis throughout the duration of the study period, all cases of S. aureus endophthalmitis were included, not only those cases for which clinical follow-up was available.
Results
Thirty-four patients with S. aureus endophthalmitis for whom long-term visual acuity was available were identified. Of these 34 cases, 15 (44 %) were caused by MRSA and 19 (56 %) were caused by MSSA. Demographics of the two cohorts were similar (Table 1) with respect to gender and age. Men and women were distributed similarly in both the MRSA and the MSSA group (six men and nine women in the MRSA group, eight men and 11 women in the MSSA group; p = 1.00). Also, there was no difference in age between the two groups, with a mean age of 70 years in the MRSA group and of 69 years in the MSSA group (p = 0.75).
At presentation, the available median logMAR visual acuity in both the MSSA (available in 18 of 19 cases) and the MRSA group (available in 14 of 15 cases) was 4.0, representing hand motions (n = 14). Initial Snellen visual acuity ranged from 20/400 to LP in the MRSA group and from 20/400 to NLP in the MSSA group. Mean logMAR visual acuity was used for statistical analysis and was found not be significantly different between the MRSA and MSSA groups at presentation (p = 0.38). There was no statistically significant difference in mean visual acuity between the MRSA and MSSA groups at any subsequent time point either. At 3 months, 6 months, and 12 months, the p-values were 0.18, 0.28, and 0.38 respectively (Fig. 1).
Overall, most endophthalmitis cases caused by S. aureus (18 of 34 cases or 53 %) were associated with cataract surgery. Of these, ten (56 %) were caused by MRSA, and eight (44 %) were caused by MSSA. Four cases occurred following an intravitreal injection (12 %), one case of which was MRSA and three of which were MSSA. Two cases (6 %) were endogenous, both of which were MSSA. Another two cases were bleb-associated (one MRSA, one MSSA), two cases resulted from trauma (one MSSA, one MRSA), two cases occurred after vitrectomy (one MSSA, one MRSA), two cases occurred following a penetrating keratoplasty (one MSSA, one MRSA), one MRSA case occurred following shortly after a trabeculectomy, and one case occurred following traumatic dehiscence of a corneal graft that had been transplanted 2 years earlier. There was no statistically significant difference in the etiologies of endophthalmitis between the MRSA and MSSA cohorts (PA and PB values >0.17).
Susceptibilities were not available for all antibiotics for every strain because antibiotics included in the routine test battery changed over the timeframe of this study. With regard to fluoroquinolone susceptibility, no strain was tested for susceptibility to all generations of this class of antibiotic. Early isolates were tested only for levofloxacin, and ciprofloxacin ± ofloxacin, while later strains were tested for levofloxacin, gatifloxacin, and moxifloxacin but not ciprofloxacin or ofloxacin. Percentages reflect the available data. Raw numbers are given in parentheses.
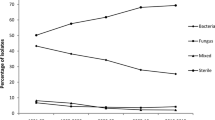
Overall, there was a trend toward an increase in the number of MRSA endophthalmitis cases per year over the course of the study period (Fig. 2). There was also a trend toward a lower rate of of MSSA endophthalmitis per year.
All S. aureus isolates, both MRSA and MSSA, were sensitive to vancomycin, gentamicin, trimethoprim–sulfamethoxazole, linezolid, and chloramphenicol (Table 2 and Table 3).
Of the MRSA strains tested for resistance to ciprofloxacin, only one strain (1/6, 17 %) was resistant. Seventy-one percent of MRSA isolates (10/14) were resistant to levofloxacin. The four MRSA strains that were sensitive were obtained prior to 2004 and were also sensitive to ciprofloxacin. All MRSA strains isolated after 2004 were resistant to levofloxacin, and were also tested for susceptibility to moxifloxacin and gatifloxacin. Of these strains, 88 % (7/8) were resistant to moxifloxacin and 89 % (8/9) were resistant to gatifloxacin.
Of the isolates in the MSSA group, all tested isolates were sensitive to moxifloxacin and all but one were sensitive to gatifloxacin. Of the isolates tested, 13 % (1/8) were resistant to ciprofloxacin and 12 % (2/13) were resistant to levofloxacin.
With regard to treatment, the MRSA group contained three patients (20 %) who underwent tap and inject and 12 patients (80 %) who initially underwent a pars plana vitrectomy. The MSSA group contained a similar distribution, with three patients (16 %) receiving a tap and inject and 16 (84 %) having undergone a PPV (p = 0.75).
Discussion
To date, the current study has the largest sample size and longest follow-up of any study comparing the visual acuity outcomes of MRSA and MSSA endophthalmitis. Of the 34 cases of S. aureus endophthalmitis for which long-term clinical follow-up was available, 15 (44 %) were MRSA. This percentage is similar to the one found in a study by Major et al [1], which identified 13 of 32 (41 %) isolates as MRSA. This appears to confirm a significant rise of MRSA compared to earlier studies such as the Endophthalmitis Vitrectomy Study, where only 6/29 (21 %) of S. aureus isolates were resistant to methicillin [16]. This however, is not unexpected, given the overall rise of the incidence of MRSA in the United States [17].
The primary aims of this study were (1) to determine if a difference between the final visual acuity of MRSA and MSSA endophthalmitis exists, and (2) to report on the microbiological characteristics of the included isolates.
MRSA has been shown in other disease processes such as pneumonia and necrotizing fasciitis to be more virulent than its MSSA counterparts, and a trend towards this appeared to emerge in a previous analysis of endophthalmitis [1]. However, in our larger cohort with longer follow-up, we observed no such trend and no statistically significant difference between the two groups at any time point. Although this is the largest study of its kind to date, the number of eyes analyzed in each group at 12 months of follow-up is relatively modest. This study may not have the power to detect subtle differences in visual acuity between the two groups at any given time point. Another potential limitation is that given the retrospective nature of this study, the treatment was at the discretion of each physician, and no standardized treatment algorithm was employed. As such, while there was no statistical difference between the rates of pars plana vitrectomy and “tap and inject” procedures between the two groups, physicians may have responded differently to the presence of different signs and symptoms that were not analyzed in this study, such as presenting visual acuity, the rapidity of onset, or the presence of certain infectious signs. It is likely, however, that in appropriate patients, the treatment modality was selected according to conclusions drawn from the Endophthalmitis Vitrectomy Study (EVS) [18].
With regard to antibiotic susceptibilities, the main limitation is that not every isolate was tested for every antibiotic listed in Table 2. Earlier isolates were tested only for early-generation fluoroquinolones, and showed a high level of sensitivity. More recent isolates were tested for sensitivity to fourth-generation fluoroquinolones, and showed a high rate of resistance. No strain was sensitive to a fourth-generation fluoroquinolone yet resistant to an earlier generation. The high incidence of MRSA resistance to latest-generation fluoroquinolones is alarming, especially given that the majority of cataract surgeons utilize fluoroquinolones as their primary antibiotic prophylaxis following cataract surgery [19]. While the use of intracameral cefuroxime has been suggested as a replacement for or adjunct to topical post-operative antibiotics, it is unclear from our study whether this would help to combat S. aureus, as no MRSA isolates and only one MSSA isolate were tested for sensitivity to cefuroxime [20].
An additional question that was addressed in the current study was whether a difference exists in the etiologies of endophthalmitis between the MRSA and MSSA cohorts. The data obtained in this study did not demonstrate any statistical difference between the two groups, as cataract surgery was the predominant etiology in both cohorts and was followed by relatively few cases from other etiologies, including intravitreal injections, trauma, endogenous, bleb-associated, corneal surgery, and incisional glaucoma surgery.
In conclusion, the relative incidence of MRSA endophthalmitis as compared to MSSA appears to be increasing. While MRSA remains sensitive to vancomycin, its sensitivity to fourth-generation fluoroquinolones appears to have dropped below 15 %, leading us to question popular choices of post-cataract surgery antibiotic prophylaxis. No difference in visual acuity outcome was observed between the MRSA and MSSA cohorts at any time point.
References
Major JC Jr, Engelbert M, Flynn HW Jr, Miller D, Smiddy WE, Davis J (2010) Staphylococcus aureus endophthalmitis: antibiotic susceptibilities, methicillin resistance, and clinical outcomes. Am J Ophthalmol 149(2):278.e271–283.e271. doi:10.1016/j.ajo.2009.08.023
Miller JJ, Scott IU, Flynn HW Jr, Smiddy WE, Newton J, Miller D (2005) Acute-onset endophthalmitis after cataract surgery (2000-2004): incidence, clinical settings, and visual acuity outcomes after treatment. Am J Ophthalmol 139(6):983–987. doi:10.1016/j.ajo.2005.01.025
Artunay O, Yuzbasioglu E, Rasier R, Sengul A, Bahcecioglu H (2009) Incidence and management of acute endophthalmitis after intravitreal bevacizumab (Avastin) injection. Eye (London, England) 23(12):2187–2193. doi:10.1038/eye.2009.7
Lyall DA, Tey A, Foot B, Roxburgh ST, Virdi M, Robertson C, MacEwen CJ (2012) Post-intravitreal anti-VEGF endophthalmitis in the United Kingdom: incidence, features, risk factors, and outcomes. Eye (London) 26(12):1517–1526. doi:10.1038/eye.2012.199
Shah CP, Garg SJ, Vander JF, Brown GC, Kaiser RS, Haller JA (2011) Outcomes and risk factors associated with endophthalmitis after intravitreal injection of anti-vascular endothelial growth factor agents. Ophthalmology 118(10):2028–2034. doi:10.1016/j.ophtha.2011.02.034
Ho V, Ho LY, Ranchod TM, Drenser KA, Williams GA, Garretson BR (2011) Endogenous methicillin-resistant Staphylococcus aureus endophthalmitis. Retina 31(3):596–601. doi:10.1097/IAE.0b013e3181ecccf0
Melo GB, Bispo PJ, Yu MC, Pignatari AC, Hofling-Lima AL (2011) Microbial profile and antibiotic susceptibility of culture-positive bacterial endophthalmitis. Eye (London) 25(3):382–387. doi:10.1038/eye.2010.236, quiz 388
Chambers HF (2005) Community-associated MRSA--resistance and virulence converge. N Engl J Med 352(14):1485–1487. doi:10.1056/NEJMe058023
Heilmann C (2011) Adhesion mechanisms of staphylococci. Adv Exp Med Biol 715:105–123. doi:10.1007/978-94-007-0940-9_7
Watkins RR, David MZ, Salata RA (2012) Current concepts on the virulence mechanisms of meticillin-resistant Staphylococcus aureus. J Med Microbiol 61(Pt 9):1179–1193. doi:10.1099/jmm.0.043513-0
Malachowa N, DeLeo FR (2010) Mobile genetic elements of Staphylococcus aureus. Cell Mol Life Sci 67(18):3057–3071. doi:10.1007/s00018-010-0389-4
Gillet Y, Issartel B, Vanhems P, Fournet JC, Lina G, Bes M, Vandenesch F, Piemont Y, Brousse N, Floret D, Etienne J (2002) Association between Staphylococcus aureus strains carrying gene for Panton–Valentine leukocidin and highly lethal necrotising pneumonia in young immunocompetent patients. Lancet 359(9308):753–759. doi:10.1016/s0140-6736(02)07877-7
Gonzalez BE, Martinez-Aguilar G, Hulten KG, Hammerman WA, Coss-Bu J, Avalos-Mishaan A, Mason EO Jr, Kaplan SL (2005) Severe Staphylococcal sepsis in adolescents in the era of community-acquired methicillin-resistant Staphylococcus aureus. Pediatrics 115(3):642–648. doi:10.1542/peds.2004-2300
Miller LG, Perdreau-Remington F, Rieg G, Mehdi S, Perlroth J, Bayer AS, Tang AW, Phung TO, Spellberg B (2005) Necrotizing fasciitis caused by community-associated methicillin-resistant Staphylococcus aureus in Los Angeles. N Engl J Med 352(14):1445–1453. doi:10.1056/NEJMoa042683
Vandenesch F, Naimi T, Enright MC, Lina G, Nimmo GR, Heffernan H, Liassine N, Bes M, Greenland T, Reverdy ME, Etienne J (2003) Community-acquired methicillin-resistant Staphylococcus aureus carrying Panton–Valentine leukocidin genes: worldwide emergence. Emerg Infect Dis 9(8):978–984. doi:10.3201/eid0908.030089
Han DP, Wisniewski SR, Wilson LA, Barza M, Vine AK, Doft BH, Kelsey SF (1996) Spectrum and susceptibilities of microbiologic isolates in the Endophthalmitis Vitrectomy Study. Am J Ophthalmol 122(1):1–17
Calfee DP (2011) The epidemiology, treatment, and prevention of transmission of methicillin-resistant Staphylococcus aureus. J Infus Nurs 34(6):359–364. doi:10.1097/NAN.0b013e31823061d6
No Authors Listed (1996) Microbiologic factors and visual outcome in the endophthalmitis vitrectomy study. Am J Ophthalmol 122(6):830–846
Chang DF, Braga-Mele R, Henderson BA, Mamalis N, Vasavada A (2015) Antibiotic prophylaxis of postoperative endophthalmitis after cataract surgery: results of the 2014 ASCRS member survey. J Cataract Refract Surg 41(6):1300–1305. doi:10.1016/j.jcrs.2015.01.014
Barry P, Seal DV, Gettinby G, Lees F, Peterson M, Revie CW (2006) ESCRS study of prophylaxis of postoperative endophthalmitis after cataract surgery: preliminary report of principal results from a European multicenter study. J Cataract Refract Surg 32(3):407–410. doi:10.1016/j.jcrs.2006.02.021
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This research was supported by The Macula Foundation, Inc.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge, or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Huz, J.I., Mukkamala, K., Pagan, I.R. et al. Clinical outcomes and antibiotic susceptibilities of Staphylococcus aureus endophthalmitis. Graefes Arch Clin Exp Ophthalmol 255, 651–656 (2017). https://doi.org/10.1007/s00417-016-3504-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-016-3504-x