Abstract
Purpose
Corneal endothelial cell density and the integrity of the monolayer are essential for maintenance of a clear cornea. In 1992, Williams et al. introduced a method to estimate the endothelial cell density in histopathologic examination. It would enable an evaluation of the corneal host endothelium, even if preoperative measurement was not possible. The goal of this study is to evaluate the accuracy of the Williams equation in corneal buttons obtained from penetrating keratoplasties.
Methods
High power field (HPF) photographs and histological endothelial cell counts were made from the corneal endothelial cells of each corneal histopathological cross-section. We then compared the calculated endothelial cell density using the Williams equation with the preoperative measured endothelial cell density. A bivariate regression analysis of the histological HPF cell counts and the preoperative endothelial cell density count was also performed.
Results
The equation of Williams et al. overestimates the endothelial density in all of our patients. Linear regression showed a strong relation between the central histological HPF count and the preoperative endothelial cell density. The regression formula for the endothelial cell density is 59.66 + (272.447 × HPF count); p < 0.001, R 2 = 0.901.
Conclusion
This study confirms the relation between the corneal endothelial cell density, measured with specular microscopy, and the histopathological endothelial cell count in a HPF. However, the equation of Williams et al. provides an overestimation of the endothelial cell density. To proper utilize the histopathological endothelial cell count, a calibration of the equation coefficients in the local setting is necessary to prevent systematic errors.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Corneal endothelial cells are responsible for maintaining constant hydration of the cornea. They are essential for providing a clear cornea. The corneal endothelial cell density decreases with increasing age [1]. The density also decreases in many corneal diseases like Fuchs endothelial dystrophy [2], inflammatory disease of the anterior or posterior segment [3], and after penetrating keratoplasty [4]. Specular microscopy can provide endothelial cell density evaluation in vivo in the clinical setting [5]. In histopathologic evaluations, however, the endothelial cell density is usually only judged as normal or reduced.
In 1992, Williams et al. introduced a method to estimate the endothelial cell density in histopathologic examination. A strong correlation between specular microscopic cell density and cross-sectional high power field counts was found in corneal donor buttons that were not suitable for transplantation. The linear equation for cell density was (number of cells per high-power field × 145) + 668. The correlation was statistically significant (p < 0.01; r = 0.91) [6].
Having the ability to estimate the endothelial cell density from histopathologic examinations can add important information. The stage of the corneal disease can be better evaluated and recognized more reliably. This is especially true in patients where a clinical evaluation of the corneal endothelial cell density is not possible by specular microscopy due to corneal opacification. The host endothelium is a strong predictor of graft longevity [4]. Therefore, the calculated endothelial cell density might be of prognostic value for the corneal transplant.
Another possible application field for an estimation of endothelial cell density in histopathologic examination is in research. The impact of other corneal diseases, like different corneal dystrophies, keratoconus, corneal trauma, or corneal inflammatory diseases on the endothelial cell density could be further evaluated.
As far as we know, the equation of Williams et al. has never been tested in a clinical setting with corneal histological specimens from penetrating keratoplasties. The goal of this study was to evaluate the equation of Williams et al. in corneal buttons, which were obtained through a penetrating keratoplasty and where the preoperative endothelial cell density had been assessed. Additionally, we evaluated the relationship between the histological endothelial cell count and the preoperative endothelial cell density.
Material and methods
We assessed all charts of patients that underwent a penetrating keratoplasty in our institution since 2008, and in whom a preoperative measurement of the endothelial cell density was available (Topcon SP 3000P, Topcon Corporation, Japan; Noncon Robo SP 8000, Konan Medical, Japan). Informed consent was obtained from all suitable patients. Ethics committee approval was granted by the ethics committee of the Albert-Ludwigs-University of Freiburg. From all available histopathological slides, five central high power field (HPF) photographs with a 40× optical field were made from the center of the corneal button (Fig. 1), and one photograph from each peripheral area. The endothelial cells were counted in all photographs by a second examiner who was not aware of the preoperative endothelial cell density. A fixed frame model was used. Due to the composition of the photographs, cells could only touch the left or right margin. Cells that touched the right margin were excluded. The mean endothelial cell count of the center HPF and peripheral area HPF were adapted for the equation of Williams et al., since there was a difference in the visual field width (Williams et al. 490 μm, our field 260 μm). We then compared the calculated endothelial cell density for the Williams equation with the preoperative measured endothelial cell density.
In a second step, we performed a regression analysis of the HPF cell counts and the preoperative endothelial cell density. We also assessed the relation of the cell counts of the center HPF and the peripheral HPF. Statistical analysis was performed with IBM SPSS Statistics, IBM, USA.
Results
Twenty-four patients fulfilled the inclusion criteria. Fifteen penetrating keratoplasties were performed due to keratoconus, and nine due to recurrence on grounds of further progression of keratoconus in the peripheral host cornea. The equation of Williams et al. overestimates the corneal endothelial density in all our patients by up to 1,000 cells/mm2 when using the histological cell count of the central HPF. In almost all cases, the peripheral HPF also results in an overestimation of the endothelial cell density (Table 1, Fig. 2). The hypothesis of zero bias can safely be rejected. The p value from the paired t-test is <0.0001. The mean of the difference is 613.
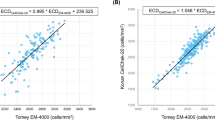
Our line of best fit in linear regression analysis was: endothelial cell density = 59.6 + (272.447 × HPF count). A strong relation between the central histological HPF count and the preoperative endothelial cell density could be demonstrated (p < 0.001, R 2 = 0.9, Fig. 3). The relation between the endothelial cell density with the peripheral HPF count was weaker; however, it was still statistically significant (p < 0.001, R 2 = 0.65). The equation of our line of best fit in linear regression analysis for the periphery was: endothelial cell density = 417.684 + (216.555 × peripheral HPF count); Fig. 4.
The relation between the central histological HPF count and the peripheral histological HPF count also was statistically significant (R 2 = 0.63).
Discussion
This study confirms the relation between the corneal endothelial cell density, measured with specular microscopy, and the histopathological endothelial cell count in a HPF, which was initially introduced by Williams et al. [6]. However, the original equation did not match our clinical endothelial cell density. One explanation might be the difference in the obtained material. Our study was performed with histopathologic slides, which were obtained by means of a penetrating keratoplasty, in contrast to donor corneas in Williams et al.’s investigation. Also the endothelial cell density was determined in different ways. Williams et al. performed measurements of the endothelial cell density ex vivo after the donor corneas were in organ culture. Our in-situ cell density measurements were entirely in vivo before the surgery was performed. Semiautomated noncontact specular microscopy is widely used in the clinical setting; however, the data quality may be reduced due to systematic errors [7, 8].
Tissue preparation for histopathologic examination may also be a reason for different cell counts due to different rates of shrinkage [9]. Since the histological cell count is based on fewer cells than the specular microscopy, any change in cell size has a much higher impact on sample errors or bias in histological counts. Another reason for different equations may be differences in the field of vision. Williams et al. were able to use 490 μm for their cell count, while we only had 260 μm. Nevertheless, our histological HPF counts showed a strong relationship with the endothelial cell density. A general limitation of our study is the study population. There are only very few patients with preoperative endothelial cell density measurements. Corneal opacities usually inhibit such measurements. We were only able to include patients with keratoconus or recurrence of keratoconus due to further progression of keratoconus in the peripheral host cornea. The reason for the one-sided patient selection is the successful preoperative measurement of the endothelial cell density. Patients with keratoconus or a recurrence usually have a clear cornea, which enables a measurement, whereas most other corneal diseases do not allow any measurement and otherwise healthy corneas usually do not undergo any form of penetrating keratoplasty. Most of our cases, especially those which underwent the first keratoplasty, cover only the higher range of cell densities. The small number of patients is a limiting factor. Since the number of suitable patients for this kind of study is small, a further evaluation of the method, for example by using an animal model, might be necessary.
Due to the strong relationship between the endothelial cell density and the histological central HPF count, the endothelial cell density can be quickly calculated. This provides additional information for the ophthalmic pathologist and the clinician in order to better evaluate the corneal endothelium. This might be especially useful in cases where no preoperative evaluation of the endothelium was possible due to corneal edema or scarring or other opacification. Since the autologous endothelium is a strong predictor of graft longevity [4], the calculated endothelial cell density might be of prognostic value for the corneal transplant. Another application is the systematic evaluation of the corneal endothelium in retrospective research. However, in order to prevent a systematic error there should be a calibration of the equation coefficients in the local setting, to adapt for different types of microscopes, cameras, or fixation and embedding techniques.
References
Møller-Pedersen T (1997) A comparative study of human corneal keratocyte and endothelial cell density during aging. Cornea 16:333–338
Olsen T (1980) On the significance of a low endothelial cell density in Fuchs’ endothelial dystrophy. A specular microscopic study. Acta Ophthalmol (Copenh) 58:111–116
Olsen T (1980) Changes in the corneal endothelium after acute anterior uveitis as seen with the specular microscope. Acta Ophthalmol (Copenh) 58:250–256
Böhringer D, Böhringer S, Poxleitner K et al (2010) Long-term graft survival in penetrating keratoplasty: the biexponential model of chronic endothelial cell loss revisited. Cornea 29:1113–1117. doi:10.1097/ICO.0b013e3181d21d07
Bourne WM, Kaufman HE (1976) Specular microscopy of human corneal endothelium in vivo. Am J Ophthalmol 81:319–323
Williams KK, Noe RL, Grossniklaus HE et al (1992) Correlation of histologic corneal endothelial cell counts with specular microscopic cell density. Arch Ophthalmol 110:1146–1149
Doughty MJ (2013) Evaluation of possible error sources in corneal endothelial morphometry with a semiautomated noncontact specular microscope. Cornea 32:1196–1203. doi:10.1097/ICO.0b013e318295e72a
Böhringer D, Hettich L, Maier PC, Reinhard T (2012) Data quality of unsupervised endothelial cell counting vs. reading centre analysis in multicentric clinical trials. Klin Monatsbl Augenheilkd 229:628–631. doi:10.1055/s-0031-1299508
Sun N, Shibata B, Hess JF, FitzGerald PG (2015) An alternative means of retaining ocular structure and improving immunoreactivity for light microscopy studies. Mol Vis 21:428–442
Acknowledgments
We thank Lisa Lacher for assistance with the statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this research.
Conflict of Interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge, or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Lang, S.J., Freysoldt, A., Böhringer, D. et al. Connection of histological corneal endothelial cell count with endothelial cell density before penetrating keratoplasty. Graefes Arch Clin Exp Ophthalmol 254, 1993–1997 (2016). https://doi.org/10.1007/s00417-016-3457-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-016-3457-0