Abstract
Purpose
To compare the lamina cribrosa (LC) depth of the optic nerve head in normal and glaucomatous eyes over a wide range of axial length (AXL).
Methods
A total of 402 eyes, including 210 normal and 192 glaucomatous eyes, were imaged by spectral domain optical coherence tomography. Normal and glaucomatous eyes were each divided into three subgroups according to the level of AXL; long (> 26 mm), mid-level (23–26 mm), and short (< 23 mm). Visual field mean deviation (VF MD), LC thickness, and LC depth were compared between normal and glaucomatous eyes in each of the AXL subgroups. These parameters were also compared between normal and glaucomatous eyes in the three AXL subgroups. Factors associated with LC depth in each AXL subgroup were evaluated by univariate and multivariate regression analyses.
Results
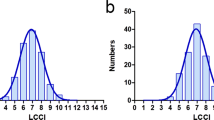
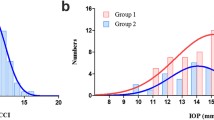
A comparison of the three AXL subgroups in normal eyes showed that the LC was thinnest in the long AXL subgroup (short; 189.7 ± 24.1 μm, mid-level; 179.9 ± 34.3 μm, long; 149.2 ± 36.2 μm, p < 0.001), but LC depth did not differ significantly in the three subgroups (short; 527.1 ± 144.4 μm, mid-level; 578.2 ± 163.5 μm, long; 594.4 ± 187.5 μm, p = 0.144). In glaucomatous eyes, glaucoma severity assessed by VF MD did not differ significantly among the three AXL subgroups (short; -6.99 ± 8.50 dB, mid-level; -6.40 ± 7.64 dB, long; -4.61 ± 5.22 dB, p = 0.168). However, LC depth was greater in the long than in the short AXL subgroup (679.5 ± 192.7 μm and 555.9 ± 134.1 μm, respectively, p = 0.004), although neither subgroup differed significantly in LC depth from the mid-level AXL subgroup (611.8 ± 162.3 μm, p = 0.385, p = 0.090). LC thickness was significantly different between normal and glaucomatous eyes (p < 0.001). LC depth was not different between normal and glaucomatous eyes in both short and mid-level AXL subgroups (p = 0.297, 0.222), but differed in the long AXL subgroup (p = 0.022). The presence of glaucoma was associated with greater LC depth only in the long AXL subgroup (p = 0.012).
Conclusions
LC depth may vary according to the level of AXL in glaucomatous eyes with a similar level of glaucoma severity, with the greatest LC depth found in eyes with long AXL. Those findings suggest that glaucomatous optic disc cupping would manifest differently according to the level of AXL.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Glaucomatous structural changes are characterized by optic disc excavation and loss of the neuroretinal rim. Posterior displacement of the lamina cribrosa (LC) of the optic nerve head (ONH) is one of the components of optic disc excavation [1]. The LC of the ONH has been proposed as a primary site for glaucoma pathogenesis [2–4]. In primates, elevation of intraocular pressure (IOP) was shown to result in the posterior displacement of the LC; in humans, IOP lowering treatment was shown to reverse this displacement [5, 6]. Hence, posterior displacement of the LC is a key feature of glaucomatous ONH changes. Histologic evaluation showed that the LC was thinner in highly myopic eyes [7, 8], suggesting that axial elongation of the eyeball can induce thinning of the LC. Thinner LC may be more vulnerable to glaucomatous damage at a similar level of IOP, and a thin LC may be predictive of glaucoma progression [9–11]. If this were the case, a thinner LC would be further displaced posteriorly than a thicker LC at a similar level of IOP. Thus, if axial elongation of the eyeball affects LC thickness and LC thickness is associated with the degree of LC posterior displacement, glaucomatous eyes of different axial lengths (AXLs) may show different amounts of posterior displacement of the LC.
The LC is covered with prelaminar neuroretinal tissue. Therefore, its complete features are rarely visible on routine ophthalmoscopic examination. Optical coherence tomography (OCT) provides high-resolution cross-sectional images of the ONH, enabling in vivo visualization of structural details of LC [12–17] to be evaluated in normal and glaucomatous eyes [18–20].
Since different-sized AXL may show different amounts of posterior displacement of the LC (like the negative correlation between AXL length and LC thickness), the current study compares LC depths over a wide range of AXL between glaucomatous and normal eyes.
Methods
Participants
All study participants were examined between March 2011 and August 2014 at the glaucoma clinic of Asan Medical Center, Seoul, Korea. The medical records of eligible glaucoma patients were retrospectively reviewed. All normal subjects were volunteers, employees of Asan Medical Center, Seoul, Korea, or family members of employees. All procedures conformed to the Declaration of Helsinki, and normal subjects provided written informed consent. The study protocol was approved by the Institutional Review Board of the Asan Medical Center at the University of Ulsan, Seoul, Korea.
Initial evaluation consisted of a complete ophthalmologic examination, including recording of medical, ocular, and family history; visual acuity (VA) testing; the Humphrey field analyzer (HFA) Swedish Interactive Threshold Algorithm (SITA) 24-2 test (Carl Zeiss Meditec, Dublin, CA); multiple IOP measurements using Goldmann applanation tonometry (GAT); stereoscopic optic nerve photography; AXL measurement (IOL Master; Carl Zeiss Meditec); and spectral domain (SD) OCT (Spectralis, Heidelberg Engineering, Dossenheim, Germany) imaging. Baseline IOP measurement was performed before IOP-lowering treatment. Only reliable HFA test results with a false-positive error < 15 %, a false-negative error < 15 %, and a fixation loss < 20 % were included. To minimize the learning effect, data from the second HFA tests were analyzed.
For inclusion in the study, both glaucoma patients and normal subjects had to have a best-corrected visual acuity of 20/30 or better, and a normal anterior chamber and open-angle on slit-lamp and gonioscopic examinations. Subjects with any other ophthalmic diseases that could result in HFA defects, and those with a history of diabetes mellitus, intraocular surgery or laser surgery, were excluded.
Glaucomatous eyes had to have a glaucomatous optic disc and a glaucomatous visual field (VF). Eyes with glaucomatous VF defects were defined as those with a glaucoma hemifield test result outside normal limits or a pattern standard deviation outside 95 % of normal limits. In addition, these eyes had to have a cluster of three points with probabilities of < 5 % on the pattern deviation map in at least one hemifield, including at least one point with a probability of < 1 %, or a cluster of two points with a probability of < 1 %. Glaucomatous VF defects had to be confirmed on at least two VF examinations
Normal eyes had IOPs less than 22 mmHg, with no history of IOP elevation, and were normal by VF examination. Eyes in the normal and glaucomatous groups were divided into three AXL subgroups: long (> 26 mm), mid-level (23–26 mm), and short (< 23 mm), for a total of six subgroups. If both eyes of any subject were eligible, one eye was randomly selected.
LC assessment by SD OCT imaging
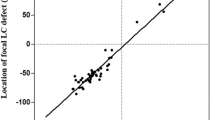
Imaging was performed using Spectralis OCT enhanced depth imaging (EDI) mode integrated within the machine. The image acquisition procedure has been described in detail [9, 21]. Briefly, the entire ONH was scanned using a 6-mm length line (512 A-scans) at intervals of 50 μm. In this study, an average of 35 horizontal B-scans was produced in EDI mode. From these B-scans, five frames (superior, mid-superior, center, mid-inferior, and inferior) that passed through the ONH were selected (Fig. 1). LC depth, defined as the distance between the line connecting both ends of Bruch’s membrane and the anterior border of the LC, was estimated. LC thickness was defined as the distance between the anterior and posterior borders of the LC, with these borders defined by the highly reflective structures below the optic cup. Both LC depth and LC thickness were estimated in each B-scan, with the distance from the reference line connecting the two termini of Bruch’s membrane to the level of the anterior border of the LC measured at the maximally depressed point and at 100 and 200 microns from the maximally depressed point in a temporal direction. Only the temporally adjacent points were selected because the maximally depressed point was often close to the central vessel trunk, the shadow of which obscured the LC. In addition, the full-thickness LC was often not clearly discernible at the temporal periphery. Images were analyzed by two experienced examiners (IKH, DJ) who were blinded to clinical information, including AXL. LC depth obtained by two examiners was averaged and considered in the analysis. The mean of 15 values (three points in each of five frames) was used for analysis.
Five frames (superior, mid-superior, center, mid-inferior, and inferior) that passed through the optic nerve head were selected from the images obtained by Spectralis optical coherence tomograpy (right). Lamina cribrosa (LC) depth, defined as the distance between the line connecting both ends of Bruch’s membrane and the anterior border of the LC, was estimated. LC thickness was defined as the distance between the anterior and posterior borders of the LC. Both LC thickness and depth were estimated in each frame, with the distance from the reference line connecting the two termini of Bruch’s membrane to the level of the anterior border of the LC measured at the maximally depressed point and at 100 and 200 microns from the maximally depressed point in a temporal direction (left)
Analysis
The Wilk–Shapiro test was used to test the distribution of numerical data. Normally distributed data were compared between normal and glaucomatous eyes in each of the three AXL subgroups using unpaired t-tests. Parameters among the three AXL subgroups in the normal and glaucoma groups were each compared by ANOVA with Bonferroni post-hoc corrections. Factors associated with LC depth in each of the three AXL subgroups were assessed by univariate and multivariate regression analyses. Variables with a probability ≤ 0.20 in univariate analyses were included in the multivariate analysis. A p value < 0.05 was considered statistically significant. All statistical analyses were performed using SPSS software (version 21.0; SPSS Inc., Chicago, IL, USA).
Results
Overall, 402 eyes of 402 subjects were analyzed, including 210 normal and 192 glaucomatous eyes. All patients were East Asians (Koreans), and the mean age of the two groups did not differ significantly (46.8 ± 12.7 vs. 48.7 ± 14.6 years, p = 0.278). Overall, the AXL was longer, the LC was thinner, and LC depth was greater in the glaucoma than in the normal group. As expected, average VF MD was worse and the RNFL was thinner in the glaucoma group (Table 1).
In both the normal and glaucomatous groups, subjects with long AXL were younger than subjects with mid-range and short AXL. A comparison of the three AXL subgroups within the normal group showed that both the LC (short AXL group; 189.7 ± 24.1 μm, mid-range AXL group; 179.9 ± 34.3 μm, long AXL group; 149.2 ± 36.2 μm, p < 0.001) and RNFL (short AXL group; 104.1 ± 8.2 μm, mid-range AXL group; 99.8 ± 8.5 μm, long AXL group; 94.8 ± 8.3 μm, p < 0.001) were thinnest in the long AXL subgroup. However, LC depth did not differ significantly in these three subgroups (short AXL group; 527.1 ± 144.4 μm, mid-range AXL group; 578.2 ± 163.5 μm, long AXL group; 594.4 ± 187.5 μm, p = 0.144). Comparisons of glaucoma severity, as assessed by both RNFL thickness and VF MD, in glaucomatous eyes, showed no significant differences among the three AXL subgroups (VF MD, short AXL group; -6.99 ± 8.50 dB, mid-range AXL group; -6.40 ± 7.64 dB, long AXL group; -4.61 ± 5.22 dB, p = 0.168), although both thinner (short AXL group; 148.6 ± 32.5 μm, mid-range AXL group; 130.5 ± 20.1 μm, long AXL group; 118.3 ± 23.3 μm, p < 0.001) and deeper LC features were found in the long AXL subgroup (short AXL group; 555.9 ± 134.1 μm, long AXL group; 679.5 ± 192.7 μm, p < 0.001, Table 2). LC depth was not different between normal and glaucomatous eyes in both short and mid-level AXL subgroups (p = 0.297, 0.222), but differed in the long AXL subgroup (p = 0.022).
When factors associated with LC depth were assessed in both normal and glaucomatous eyes with short AXL, none of the analyzed factors, including the presence of glaucoma, was significantly associated with LC depth. In the combined (normal and glaucomatous eyes) mid-level AXL subgroups, younger age [beta coefficient -4.213 (95 % confidence interval, -6.333, -1.629), p = 0.001], and a thinner LC [-1.054(-1.767, -0.200), p = 0.010] were associated with greater LC depth. In the combined (normal and glaucomatous eyes) long AXL subgroups, all analyzed variables, such as age [-2.447(-6.333, -0.715), p = 0.118], LC thickness [-0.783(-2.001, -0.369), p = 0.174], VF MD [-7.313(-16.091, 0.694), p = 0.064], RNFL thickness [-2.145(-4.535, -0.028), p = 0.045)], AXL [25.414(-11.341, 67.441), p = 0.197], and presence of glaucoma [85.641(10.11, 167.435), p = 0.031], had p values less than 0.2 in univariate analyses. Multivariate analysis that included these factors showed that the presence of glaucoma was significantly associated with greater LC depth [100.190(20.812, 167.325), p = 0.012, Table 3].
Discussion
According to our results, glaucomatous eyes were more myopic, showing longer AXL than normal eyes at similar age levels, with an approximate difference in length of 1.2 mm. Myopia was shown to be a risk factor for glaucoma development [22, 23]. Hence, our result was in agreement with that of previous reports. Recent publications reported that myopic glaucoma is prevalent in East Asian countries, especially in younger subjects [24, 25]. Our glaucoma patients were relatively young (mean age, 48.7 years), which may have contributed to the result that glaucomatous eyes were more myopic than normal eyes.
Overall, this study found that LC depth was greater in glaucomatous than in normal eyes, suggesting that glaucomatous eyes had greater optic disc excavation. Glaucomatous eyes also had longer AXL, which may have contributed to their greater LC depth because LC depth tended to increase as the eyeball became longer. Despite our finding that LC depth was greater in glaucomatous than in normal eyes overall, different outcomes were observed in the AXL subgroups. LC depth differed significantly in normal and glaucomatous eyes with long AXL, but not in those with short and mid-level AXL. That is, eyes with short and mid-level AXL did not show significant posterior displacement of the LC compared with normal eyes of similar AXL. Glaucoma severity, as assessed by VF MD and RNFL thickness, did not differ among the three AXL subgroups, indicating that glaucoma severity did not confound these results. Hence, posterior displacement of the LC in glaucomatous eyes with short AXL was lower than in eyes with long AXL at similar levels of glaucoma severity. Factor analysis showed similar results; none of the analyzed factors, including the presence of glaucoma, were associated with LC depth in eyes with short AXL. By contrast, LC depth was strongly associated with the presence of glaucoma in eyes with long AXL. Interestingly, LC thicknesses differed significantly between glaucomatous and normal eyes in all three AXL subgroups. Summarizing those results, LC thicknesses were lower in glaucomatous than in normal eyes regardless of AXL, but LC depth tended to be greater in glaucomatous eyes with relatively longer AXL, and to be lower in glaucomatous eyes with short AXL. This may be due to the thinner sclera in eyes with long AXL, enabling greater deformation of the LC. In contrast, at a similar level of glaucoma severity, LC depth was significantly lower in eyes with short than with long AXL. In as much as glaucoma severity was not greater in the long AXL subgroup, glaucomatous damage in the short AXL subgroup seemed to progress without further posterior displacement of the LC.
The study has a few limitations. The first is the measurement of LC depth. Although the EDI technique for imaging LC features (e.g., thickness) is being actively used in numerous publications, LC measurements remain difficult in certain cases. For example, the posterior border of the LC is harder to discern than the LC anterior border on images obtained by SD OCT EDI, which is key for accurate measurements of LC thickness. Although the measurement of LC depth seems to be plainer than that of LC thickness, it too may be problematic. Most studies set the reference point for LC depth as Bruch’s membrane opening (BMO) [11, 26]. Since myopic optic discs have experienced peripapillary changes, including posterior bowing of the BMO, or peripapillary atrophy (PPA) in the absence of BM [27, 28], LC depth may vary according to the position of the BMO or the presence of BM. Furthermore, use of BMO as a set point will result in LC depth that includes choroidal thickness, and subsequently, some eyes with a thin choroidal layer have a relatively small LC depth when using BMO as a reference point. However, if the set point is the choroid-scleral interface, the LC depth will be greater. That is, the reference point for measuring LC depth may require adjustment, depending on the shape of the optic disc and peripapillary atrophy or choroidal thickness. Another limitation of the study design is the use of only five cross sections, which supposedly represent the entire lamina cribrosa.
In conclusion, this study showed that LC depth may vary according to the level of AXL in glaucomatous eyes with a similar level of glaucoma severity. Glaucomatous eyes with long AXL had the greatest LC depth. Glaucomatous eyes with shorter AXL had LC depth similar to that of normal eyes with the same level of AXL. These observations suggest that glaucomatous optic disc cupping would differ depending on the level of AXL. Further, clinicians should consider the level of AXL when categorizing the amount of glaucomatous optic disc cupping, so as not to overestimate the severity of the disease.
References
Lee KM, Kim TW, Weinreb RN, Lee EJ, Girard MJ, Mari JM (2014) Anterior lamina cribrosa insertion in primary open-angle glaucoma patients and healthy subjects. PLoS One 9, e114935
Quigley HA, Addicks EM, Green WR, Maumenee AE (1981) Optic nerve damage in human glaucoma. II. The site of injury and susceptibility to damage. Arch Ophthalmol 99:635–649
Quigley HA, Anderson DR (1977) Distribution of axonal transport blockade by acute intraocular pressure elevation in the primate optic nerve head. Invest Ophthalmol Vis Sci 16:640–644
Radius RL, Anderson DR (1981) Rapid axonal transport in primate optic nerve. Distribution of pressure-induced interruption. Arch Ophthalmol 99:650–654
Strouthidis NG, Fortune B, Yang H, Sigal IA, Burgoyne CF (2011) Longitudinal change detected by spectral domain optical coherence tomography in the optic nerve head and peripapillary retina in experimental glaucoma. Invest Ophthalmol Vis Sci 52:1206–1219
Lee EJ, Kim TW, Weinreb RN (2012) Reversal of lamina cribrosa displacement and thickness after trabeculectomy in glaucoma. Ophthalmology 119:1359–1366
Jonas JB, Berenshtein E, Holbach L (2004) Lamina cribrosa thickness and spatial relationships between intraocular space and cerebrospinal fluid space in highly myopic eyes. Invest Ophthalmol Vis Sci 45:2660–2665
Jonas JB, Xu L (2014) Histological changes of high axial myopia. Eye (Lond) 28:113–117
Kim S, Sung KR, Lee JR et al (2013) Evaluation of lamina cribrosa in pseudoexfoliation syndrome using spectral-domain optical coherence tomography enhanced depth imaging. Ophthalmology 120:1798–1803
Park HY, Jeon SH, Park CK (2012) Enhanced depth imaging detects lamina cribrosa thickness differences in normal tension glaucoma and primary open-angle glaucoma. Ophthalmology 119:10–20
Lee EJ, Kim TW, Kim M, Kim H (2015) Influence of Lamina Cribrosa Thickness and Depth on the Rate of Progressive Retinal Nerve Fiber Layer Thinning. Ophthalmology 122:721–729
Srinivasan VJ, Adler DC, Chen Y et al (2008) Ultrahigh-speed optical coherence tomography for three-dimensional and en face imaging of the retina and optic nerve head. Invest Ophthalmol Vis Sci 49:5103–5110
Inoue R, Hangai M, Kotera Y et al (2009) Three-dimensional high-speed optical coherence tomography imaging of lamina cribrosa in glaucoma. Ophthalmology 116:214–222
Kagemann L, Ishikawa H, Wollstein G et al (2008) Ultrahigh-resolution spectral domain optical coherence tomography imaging of the lamina cribrosa. Ophthalmic Surg Lasers Imaging 39(suppl):S126–S131
Strouthidis NG, Grimm J, Williams GA et al (2010) A comparison of optic nerve head morphology viewed by spectral domain optical coherence tomography and by serial histology. Invest Ophthalmol Vis Sci 51:1464–1474
Girard MJ, Strouthidis NG, Ethier CR, Mari JM (2011) Shadow removal and contrast enhancement in optical coherence tomography images of the human optic nerve head. Invest Ophthalmol Vis Sci 52:7738–7748
Kim TW, Kagemann L, Girard MJ, Strouthidis NG, Sung KR, Leung CK et al (2013) Imaging of the lamina cribrosa in glaucoma: perspectives of pathogenesis and clinical applications. Curr Eye Res 38:903–909
Lee EJ, Kim TW, Weinreb RN et al (2011) Visualization of the lamina cribrosa using enhanced depth imaging spectral-domain optical coherence tomography. Am J Ophthalmol 152:87–95
Park SC, De Moraes CG, Teng CC et al (2012) Enhanced depth imaging optical coherence tomography of deep optic nerve complex structures in glaucoma. Ophthalmology 119:3–9
Wang B, Nevins JE, Nadler Z, Wollstein G, Ishikawa H, Bilonick RA et al (2013) In-Vivo Lamina Cribrosa Microarchitecture in Healthy and Glaucomatous Eyes as Assessed by Optical Coherence Tomography. Invest Ophthalmol Vis Sci 54:8270–8274
Chung HS, Sung KR, Lee KS, Lee JR, Kim S (2014) Relationship between the lamina cribrosa, outer retina, and choroidal thickness as assessed using spectral domain optical coherence tomography. Korean J Ophthalmol 28:234–240
Marcus MW, de Vries MM, JunoyMontolio FG et al (2011) Myopia as a risk factor for open-angle glaucoma: a systematic review and meta-analysis. Ophthalmology 118:1989–1994
Wong TY, Foster PJ, Hee J et al (2000) Prevalence and risk factors for refractive errors in adult Chinese in Singapore. Invest Ophthalmol Vis Sci 41:2486–2494
Chon B, Qiu M, Lin SC (2013) Myopia and glaucoma in the South Korean population. Invest Ophthalmol Vis Sci 54:6570–6577
Lee JY, Sung KR, Han S, Na JH (2015) Effect of myopia on the progression of primary open angle glaucoma. Invest Ophthalmol Vis Sci 56:1775–1781
Park SC, Brumm J, Furlanetto RL, Netto CF, Liu Y, Tello C, Liebmann JM, Ritch R (2015) Lamina Cribrosa Depth in Different Stages of Glaucoma. Invest Ophthalmol Vis Sci 56:2059–2064
Kim M, Kim TW, Weinreb RN, Lee EJ (2013) Differentiation of parapapillary atrophy using spectral-domain optical coherence tomography. Ophthalmology 120:1790–1797
Na JH, Moon BG, Sung KR, Lee Y, Kook MS (2010) Characterization of peripapillaryatrophy using spectral domain optical coherence tomography. Korean J Ophthalmol 24:353–359
Acknowledgments
This study was supported by a grant (2013-0513) from the Asan Medical Center, Seoul, Korea, grant (2013-500) from the Asan Institute for Life Sciences, Asan Medical Center, Seoul, Korea, and the Basic Science Research Program through the National Research Foundation of Korea (NRF), which is funded by the Ministry of Education, Science, and Technology (NRF-2014R1A1A3A04051089).
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements) in the subject matter or materials discussed in this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yun, SC., Hahn, I.K., Sung, K.R. et al. Lamina cribrosa depth according to the level of axial length in normal and glaucomatous eyes. Graefes Arch Clin Exp Ophthalmol 253, 2247–2253 (2015). https://doi.org/10.1007/s00417-015-3131-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-015-3131-y