Abstract
Purpose
Prior research in animal models has suggested that retinal macrophages play an important role in age-related macular degeneration (AMD), but studies have insufficiently characterized the distribution of retinal macrophages in various stages of human AMD.
Methods
In this case series, we analyzed H&E, periodic acid-Schiff, and CD163 and CD68 immunostained slides from 56 formaldehyde-fixed, paraffin-embedded autopsy eyes of patients over age 75: 11 age-matched, normal eyes, and 45 AMD eyes.
Results
Qualitative analysis of the macula and retinal periphery revealed that all eyes contained a significant number of CD163+ cells but a negligible number of CD68+ cells. In normal eyes and eyes with thin or infrequent basal laminar deposits, CD163+ cells were restricted to the inner retina. In contrast, in AMD eyes with thick basal deposits, choroidal neovascular membranes, and geographic atrophy, qualitatively there was a marked increase in the number and size of the CD163+ cells in the outer retina, sub-retinal, and sub-retinal pigment epithelium space in the macula.
Conclusions
The changes in number and localization of retinal CD163+ cells in eyes with intermediate-severe AMD support a key role for macrophages in the pathogenesis and progression of the disease. A larger, quantitative study evaluating the distribution of macrophage subpopulations in postmortem AMD eyes is warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Studies in animal models of neovascular age-related macular degeneration (AMD) [1–3] and human AMD case series [4–6] showed that retinal macrophages play an important role in AMD. Herein, we report that the retinas of human eyes with AMD contain a significantly larger number of infiltrating macrophages than previously demonstrated. Importantly, we observed a striking change in the number, morphology, and retinal localization of macrophages in eyes with intermediate and severe AMD as compared to normal or early AMD eyes. These observations suggest that retinal macrophages are centrally implicated in AMD genesis and progression.
Materials and methods
Autopsy eyes of patients over age 75 (average age 85.3, range 76–98) were evaluated in this study. The population was predominantly female (64%) and Caucasian (69%). The most common comorbidities were hypertension (36%) and diabetes mellitus (18%). The average post-mortem interval to tissue fixation was 28.1 h (range 6.5–70.3).
Autopsy eyes were enucleated and fixed in 3.7% neutral-buffered formaldehyde. The diagnosis of AMD was made postmortem due to the absence of ophthalmic clinical history in most cases. Following the removal of the superior calotte, postmortem fundus examination and color photography were performed, then the eyes were embedded in paraffin, and sectioned at 5 μm. The use of autopsy eyes for research was approved by the Institutional Review Board of the Duke University. Hematoxylin and eosin (H&E), periodic-acid Schiff (PAS), and immunostained macular sections were evaluated for the presence of AMD and graded using the AMD grading system by Sarks [7]. Eyes with other detectable macular pathology and eyes with glaucoma were excluded. The best foveal sections were selected for immunohistochemical (IHC) studies [8].
The IHC detection of CD68 and CD163 was performed using Leica Bond-MAX or Leica Bond-III automated stainers (Leica Microsystems Inc., Buffalo Grove, IL, USA), a 20 min antigen retrieval with Novocastra Bond Epitope Retrieval 2 solution (Leica Microsystems) at 100 °C and pH 6.0, ready-to-use CD68 (clone 514H12) antibodies or 1:200 dilution CD163 (clone 10D6) antibodies (Leica Microsystems), and the Novocastra Bond Polymer Refine Red Detection system (Leica Microsystems) [9]. Negative controls employed a commercially available cocktail of mouse IgG1, IgG2b, IgG3 and IgM (Leica Microsystems). Human tonsil sections were used as positive controls.
Photomicrographs were acquired using a Vanox AHSB3 microscope (Olympus America, Center Valley, PA) and a D800 Nikon camera connected by a 2.5× MM-SLR adapter (Martin Microscope Co., Easley, SC). DigiCamControl software (www.digicamcontrol.com) was used to acquire images.
Results
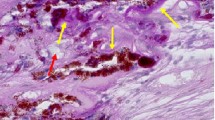
We identified 11 normal eyes from 11 age-matched control subjects (Sarks group I) and 45 eyes with AMD of various severities from 45 patients over age 75: eight eyes from group II, seven eyes from group III, eight eyes from group IV, 15 eyes from group V (eight eyes with geographic atrophy and seven eyes with CNV), and 7 eyes from group VI. The diagnosis was made postmortem due to the absence of ophthalmic clinical history in most cases. Postmortem fundus examination and color photography were performed. Qualitative analysis of both macula (defined by the retinal area with >1 ganglion cell layer) and retinal periphery revealed that all normal AMD eyes (group I) contained a large number of CD163+ cells. The number of CD68+ cells was nearly negligible in normal, control eyes (Figs. 1 and 2g). In control eyes and AMD eyes with isolated basal laminar deposits (group II; N = 8) or thin, continuous sub-retinal pigment epithelium (RPE) deposits (group III; N = 7), CD163+ cells were restricted to the inner retina (above the outer plexiform layer) of both macula and retinal periphery, and no CD163+ cells were present in the outer retina or sub-RPE. In these eyes (Fig. 2a–c), CD163+ cells in the nerve fiber layer and ganglion cell layer had a dendritic, microglioid phenotype with a small soma and long processes (inset in Fig. 2a). In the inner plexiform layer and inner nuclear layer, some of the CD163+ cells had a dendritic morphology, and others were characterized by a more rounded conformation (Fig. 2a). In contrast, in AMD eyes with thick, continuous sub-RPE deposits (group IV; N = 8), we detected a notable presence of CD163+ cells in the outer retina, sub-retinal and sub-RPE space in the macula. Qualitatively, there was an apparent increase in the number and size of CD163+ cells with higher disease severity (Fig. 2d–f). CD163+ cells had an activated morphology with large soma and short processes [4, 5], a phenotype that was especially prominent in severe AMD cases with geographic atrophy (N = 8), choroidal neovascularization (N = ,7) and disciform scar (N = 7) (inset in Fig. 2e). In AMD eyes with geographic atrophy, melanin-filled cells at the edges of areas of RPE atrophy expressed the marker CD163 (inset in Fig. 2e). In eyes with CNV and disciform scar (Fig. 2f), there were numerous CD163+ cells concentrated in the area of the fibrotic scar and throughout all retinal layers. In eyes from groups IV-VI, we noted a qualitative increase in the number of CD163+ cells in the outer retina in the periphery to the ora serrata. Many normal and AMD eyes exhibited subretinal CD163+ cells adjacent to the ora serrata. There was a complete absence of cellular staining in the negative controls (inset in Fig. 2h).
Eyes stained with hematoxylin and eosin illustrating histopathology in normal eyes and AMD eyes with various disease severities according to the Sarks classification system [7]. a Normal, age-matched control eye with normal RPE and absence of basal deposits (group I). b AMD eye with a few discrete, discontinuous sub-RPE basal laminar deposits, and mild RPE irregularity (group II). c AMD eye with thin, eosinophilic and finely granular, continuous basal deposits, and irregular RPE (consistent with group III); inset depicts the continuous sub-RPE basal deposits. d AMD eye with thick, continuous basal deposits, irregular RPE with indistinct cell borders and photoreceptors with foci of retraction, distortion, and occasional degeneration (group IV). e AMD eye with thick deposits, areas of RPE loss (geographic atrophy), RPE hyperplasia at the edges of atrophy, and photoreceptor loss (group V). f AMD eye with a disciform scar, RPE, and photoreceptor loss (group VI). Scale bar = 100 μm; insets are enlarged 4-fold. Please note that the white line in panels a and b is a break between two separate images, which were obtained due to the presence of a postmortem sensory retinal detachment
Immunohistochemical localization of CD163+ and CD68+ cells in normal, age-matched control eyes and eyes with AMD of various severity grades. CD163+ and CD68+ cells were detected using a red alkaline phosphatase polymer system. The tissue was counterstained with hematoxylin and the nuclei are blue. CD163+ cells are present solely in the inner retina in normal, age-matched eyes (a) and AMD eyes groups II and III (b, c), but were present in the outer retina and subretinal space in eyes with thick subretinal deposits in AMD group IV (d), geographic atrophy in group V (e), and disciform scar in group VI (f). In contrast, a negligible number of CD68+ cells were detected in the retina of control, age-matched eyes (g) and only a small number were in eyes with severe AMD (h group VI, disciform scar, same eye as in f). Insets in a: In normal eyes, CD163+ cells in the nerve fiber layer and ganglion cell layer had a dendritic, microglioid phenotype with a small soma and long processes. In the inner plexiform layer and inner nuclear layer, some of the CD163+ cells had a dendritic morphology and others were characterized by a more rounded, epithelioid conformation. Insets in d and f In eyes from groups IV-VI, CD163+ cells in the outer retina and subretinal space had a rounded morphology with large cell bodies and small processes. Insets in e In eyes with geographic atrophy (group V), the CD163+ cells had a larger soma and shorter processes, consistent with an activated macrophage morphology. The edges of geographic atrophy expressed the marker CD163 in cells filled with melanin granules. Inset in h In the negative controls, there was a complete absence of cellular staining with red chromogen. Scale bar = 100 μm; insets in a-f are enlarged fourfold and the inset in h is at the same magnification as images a-h. Arrow heads: CD163+ macrophages in the outer retina; arrows: subretinal CD163+ cells; *: sub-RPE CD163+ cells. The white line in panels a, b, d and g is the break between two separate photomicrographs taken due to postmortem sensory retinal detachment separating photoreceptors from RPE
Discussion
AMD-related changes in animal models were associated with retinal infiltration by bone marrow-derived macrophages early in the degenerative process [1, 2]. Despite a significant body of work devoted to this subject from the original ultrastructural observations to later immunohistochemical studies [10–13], the retinal distribution and relative contribution of macrophage subpopulations to the pathobiology of human AMD have not been adequately investigated. This is largely due to the fact that identification of retinal macrophages in human AMD is difficult. Most monocytic cells cannot be recognized within the retina in sections stained with H&E due to the high cellularity and heterogeneity of retinal cell types. Although RPE cells can be highly metaplastic and have been shown to express macrophage markers such as CD68 at the edges of geographic atrophy [8], pigment-laden macrophages may also closely resemble hypertrophied or migrating RPE cells at the edges of atrophy areas if immunohistochemical markers of macrophages are not employed. Indeed, retinal macrophages have been reported in a small number of human AMD cases [4–6]. Earlier studies found subpopulations of CD68+ cells in the normal aged retina, albeit in small numbers present in both retinal sections and flat mounts [13, 14]. In agreement with prior studies, we found nearly no CD68+ cells in the retina of normal eyes and eyes with early AMD, and a small number of CD68+ retinal macrophages in advanced AMD. Nonetheless, based on the report of Bronkhorst and coworkers in eyes with uveal melanoma, expression of CD163 and CD68 by macrophages may not be mutually exclusive in the intraocular microenvironment [15].
The newer macrophage marker CD163, a haptoglobin-hemoglobin scavenger [16] that predominantly labels bone marrow-derived macrophages [17], and access to a large collection of autopsy eyes allowed the identification of an abundance of infiltrating CD163+ cells in postmortem retinas of AMD patients. CD163+ cells with a resting morphology were present in the inner retina of all eyes studied. CD163+ cells accumulated over areas of geographic atrophy and some of these enlarged cells engulfed pigment. In eyes with CNV and disciform scars, we also noted a qualitative increase in intraretinal CD163+ cells and an abundance of subretinal and sub-RPE CD163+ cells. The significance of the peripheral CD163+ cells is unclear, but it is interesting to note that the pattern of infiltration in the retinal periphery in various AMD stages and controls appeared to parallel the pattern present in the macula, with an increase in the number of cells in the outer retina in intermediate-severe stages of AMD.
Cherepanoff and colleagues recently described the distribution of retinal CD163+ cells, CD163+ choroidal macrophages, and subretinal epithelioid CD163+ cells in the ora serrata region of six normal human adult eyes from four donors [9]. This distribution was consistent with our findings in normal control cases. Cao et al. [6] analyzed a total of ten AMD eyes (five with exudative AMD and five with atrophic AMD) and eight control eyes and found a very mild CD163+ cells infiltration in the CNV lesions, but no CD163+ cells in eyes with geographic atrophy or normal control eyes. The significant disparity between this work and ours is likely due to differences in IHC staining techniques and to the stated low availability of AMD cases in the prior study [6]. Cao and collaborators employed a citrate buffer retrieval technique [6] as opposed to the Novocastra Bond Epitope Retrieval. We found a great variability in CD163 staining of macrophages depending on technique, with optimum staining being achieved only when we used Leica Bond automated stainers, antibodies, and a polymer detection system.
Our observation that there is a qualitative increase in retinal CD163+ cells in eyes with thick, continuous basal deposits and advanced AMD supports a key role for macrophages in the pathogenesis and progression of AMD. A larger quantitative study evaluating the distribution and role of macrophage subpopulations in postmortem AMD eyes is warranted to confirm these qualitative observations.
References
Caicedo A, Espinosa-Heidmann DG, Hamasaki D, Pina Y, Cousins SW (2005) Photoreceptor synapses degenerate early in experimental choroidal neovascularization. J Comp Neurol 483:263–277
Caicedo A, Espinosa-Heidmann DG, Pina Y, Hernandez EP, Cousins SW (2005) Blood-derived macrophages infiltrate the retina and activate Muller glial cells under experimental choroidal neovascularization. Exp Eye Res 81:38–47
Grossniklaus HE, Ling JX, Wallace TM, Dithmar S, Lawson DH, Cohen C, Elner VM, Elner SG, Sternberg P Jr (2002) Macrophage and retinal pigment epithelium expression of angiogenic cytokines in choroidal neovascularization. Mol Vis 8:119–126
Penfold PL, Gyory JF, Hunyor AB, Billson FA (1995) Exudative macular degeneration and intravitreal triamcinolone. A pilot study. Aust N Z J Ophthalmol 23:293–298
Gupta N, Brown KE, Milam AH (2003) Activated microglia in human retinitis pigmentosa, late-onset retinal degeneration, and age-related macular degeneration. Exp Eye Res 76:463–471
Cao X, Shen D, Patel MM, Tuo J, Johnson TM, Olsen TW, Chan CC (2011) Macrophage polarization in the maculae of age-related macular degeneration: a pilot study. Pathol Int 61:528–535
Sarks SH (1976) Ageing and degeneration in the macular region: a clinico-pathological study. Br J Ophthalmol 60:324–341
Cherepanoff S, McMenamin P, Gillies MC, Kettle E, Sarks SH (2010) Bruch’s membrane and choroidal macrophages in early and advanced age-related macular degeneration. Br J Ophthalmol 94:918–925
Cherepanoff S, Hasic E, McMenamin P, Gillies M (2013) CD163+ and CD68+ cells in the adult human eye. Invest Ophthalmol Vis Sci 54(15):2048
Killingsworth MC, Sarks JP, Sarks SH (1990) Macrophages related to Bruch’s membrane in age-related macular degeneration. Eye (Lond) 4(Pt 4):613–621
Oh H, Takagi H, Takagi C, Suzuma K, Otani A, Ishida K, Matsumura M, Ogura Y, Honda Y (1999) The potential angiogenic role of macrophages in the formation of choroidal neovascular membranes. Invest Ophthalmol Vis Sci 40:1891–1898
Skeie JM, Mullins RF (2009) Macrophages in neovascular age-related macular degeneration: friends or foes? Eye (Lond) 23:747–755
Yang P, Das PK, Kijlstra A (2000) Localization and characterization of immunocompetent cells in the human retina. Ocul Immunol Inflamm 8:149–157
Penfold PL, Madigan MC, Provis JM (1991) Antibodies to human leucocyte antigens indicate subpopulations of microglia in human retina. Vis Neurosci 7:383–388
Bronkhorst IH, Ly LV, Jordanova ES, Vrolijk J, Versluis M, Luyten GP, Jager MJ (2011) Detection of M2-macrophages in uveal melanoma and relation with survival. Invest Ophthalmol Vis Sci 52:643–650
Kristiansen M, Graversen JH, Jacobsen C, Sonne O, Hoffman HJ, Law SK, Moestrup SK (2001) Identification of the haemoglobin scavenger receptor. Nature 409:198–201
Badylak SF, Valentin JE, Ravindra AK, McCabe GP, Stewart-Akers AM (2008) Macrophage phenotype as a determinant of biologic scaffold remodeling. Tissue Eng A 14:1835–1842
Conflict of interest
All authors certify that they have NO affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Financial disclosure
None to report
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lad, E.M., Cousins, S.W., Van Arnam, J.S. et al. Abundance of infiltrating CD163+ cells in the retina of postmortem eyes with dry and neovascular age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol 253, 1941–1945 (2015). https://doi.org/10.1007/s00417-015-3094-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-015-3094-z