Abstract
Introduction
In persons with multiple sclerosis (pwMS), little evidence exist on the effects of Alemtuzumab on physiological, physical, and cognitive function along with patient-reported outcomes, despite these domains are being rated as highly important. Therefore, our purpose was to perform a prospective observational study to examine these outlined outcomes during the first two years of Alemtuzumab treatment in pwMS.
Methods
In n = 17 relapsing–remitting pwMS, physiological function [body composition; bone mineral content; muscle strength; aerobic capacity], physical function [6-min walk test (6MWT, primary outcome); timed 25 ft walk test (T25FWT); six spot step test (SSST); 9-step stair ascend (9SSA); timed up and go test (TUG); 5 × sit to stand test (5STS)], cognitive function [selective reminding test (SRT); symbol digit modalities test (SDMT)], and patient-reported outcomes [multiple sclerosis impact scale-29 (MSIS29); 12-item multiple sclerosis walking scale (MSWS12); modified fatigue impact scale (MFIS); hospital anxiety and depression scale (HADS)] were assessed prior to Alemtuzumab treatment initiation as well as 3, 6, 12, and 24 months into the treatment.
Results
Improvements were observed at 24-month follow-up in T25FWT (+ 8%), SSST (+ 10%), SDMT (+ 5.2 points, 53% improved more than the clinical cut-off score) and SRT, whereas the primary outcome 6MWT, and all other remaining outcomes, remained stable throughout the Alemtuzumab treatment period.
Conclusion
The present findings suggest that Alemtuzumab treatment in relapsing–remitting pwMS can improve certain domains of physical function (short distance walking) and cognitive function (processing speed, memory), and furthermore stabilize physiological and physical function along with patient-reported outcomes.
Trial registration
Registered at clinicaltrials.gov: NCT03806387.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multiple Sclerosis (MS) is a chronic autoimmune neurodegenerative disease of the central nervous system (CNS), and the most common non-traumatic cause of disability in young people [1, 2]. Due to the pathology of MS (e.g., brain lesions and brain atrophy), a wide range of symptoms develops [3, 4], with approximately 40–70% of persons with MS (pwMS) reporting impairments in physical and/or cognitive function [5,6,7,8,9,10]. This is particularly evident for the 6-min walk test (6 MWT; reflecting walking endurance) [8] and for the symbol digit modalities test (SDMT; reflecting cognitive processing speed) [5, 6]. Importantly, both the 6 MWT and the SDMT are considered sentinel for impairments in physical and cognitive function in pwMS. While impairments in physical and cognitive function are present already at early disease stages [11, 12], rates of impairments increase substantially as the disease progresses [5,6,7,8, 13]. Moreover, pwMS perceive impairments in both physical and cognitive function among the most critical consequences of MS [14, 15]. Treatments that can positively impact (i.e., reduce impairments in) both physical and cognitive function are therefore warranted.
Disease-modifying drugs (DMDs) with varying mechanisms of action and routes of administration have been shown effective for relapsing–remitting MS (the most frequent disease course), specifically by reducing clinical relapses, brain lesions and brain atrophy [16,17,18] along with disability progression [assessed by the expanded disability status scale (EDSS)] [17, 19]. Furthermore, DMDs have also been shown to have some—yet more modest—stabilizing or even improving effects on objectively assessed cognitive [20] and physical function (most often assessed by the multiple sclerosis functional composite (MSFC)) [16], as well as on patient-reported outcomes (reflecting quality of life, depression, fatigue, physical function, and mental function) [21, 22]. Of note, this could be achieved indirectly, with DMDs reducing disease activity subsequently enabling patients to increase their daily physical activity levels and/or to engage more in exercise. Both physical activity and exercise are known to positively influence physical function and patient-reported outcomes [23, 24] along with body composition and bone health [25, 26]. Despite the importance from the perspective of both patients and clinicians, the existing studies that report on these domains are nevertheless few and heterogeneous in terms of their selection of outcome measures for cognitive function (perhaps with the exception of processing speed), physical function, and patient-reported outcomes.
Among the existing DMDs, Alemtuzumab is a humanized monoclonal antibody targeting CD52 cells, that depletes and repopulates B lymphocytes and T lymphocytes, causing sustained changes in the adaptive immunity [27,28,29]. Alemtuzumab has been shown to be among the most potent DMDs in reducing clinical relapses, brain lesions and brain atrophy for relapsing–remitting MS [18, 30,31,32,33,34]. However, current evidence on the potential stabilizing/improving effects of Alemtuzumab on objectively assessed physical and cognitive function as well as on patient-reported outcomes are sparse. Across previous studies (CARE-MS-1 and -2), it was reported that MSFC (a battery that combines the timed 25-foot walk (T25FWT), the 9-hole peg test (9HPT), and the paced auditory serial addition test (PASAT)) was slightly improved after a 24-month treatment period, mainly due to improvements in the 9HPT and the PASAT [30, 31, 35]. These positive effects on cognitive processing speed, were supported by Riepl and colleagues, as they also observed improvements (rey complex figure test and SDMT) after a 15-month treatment period [36]. Furthermore, patient-reported outcomes (short-form 36 physical and mental function (SF36); functional assessment of multiple sclerosis (FAMS)) were reported to improve after a 24-month treatment period [37]. Yet, no previous studies have comprehensively evaluated objectively assessed physical and cognitive function alongside patient-reported outcomes prospectively in pwMS following initiation of treatment with Alemtuzumab.
Altogether, the primary purpose of the present study is therefore to prospectively monitor changes (at 3, 6, 12, and 24 months) in multiple measures of (1) objectively assessed physiological outcomes related to physical function, (2) objectively assessed physical function (primary outcome: 6-min walk test (6MWT) at 24-month follow-up), (3) objectively assessed cognitive function, and (4) patient-reported outcomes during the first 2 years of treatment with Alemtuzumab in a well-characterised Danish cohort of relapsing–remitting pwMS.
Methods
The present study was registered in the database of the US National Library of Medicine (clinicaltrials.gov; NCT03806387), ethics approval was obtained from the ethics committee of the central Denmark region (record 1-10-72-223-16), and the study was conducted in accordance with the Declaration of Helsinki. All participants provided signed consent before entry. The Danish Data Protection Agency oversaw the study.
Study design and participants
The present prospective observational study investigated the effects of Alemtuzumab treatment across multiple functional domains in pwMS. Participants underwent testing prior to Alemtuzumab treatment (baseline) as well as 3, 6, 12 and 24 months after Alemtuzumab treatment initiation (Table 1). At both baseline and 12-month follow-up, the test session was performed prior to infusion of Alemtuzumab (corresponding to 1st and 2nd treatment). With the exception of an initial neurological screening, all test sessions were performed at Exercise Biology, Department of Public Health, Aarhus University, Denmark.
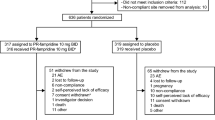
Participants were recruited from MS clinics across Denmark (Jutland, Funen, Zealand), with the neurologists or nurses confirming eligibility based on the patients’ medical records. Eligible and interested pwMS was referred to us, meaning that we worked independently of any treatment decisions. Participants had to fulfil the following inclusion criteria: age ranging from 18 to 65 years, planned to initiate Alemtuzumab treatment (according to national guidelines and the most recent SmPC; i.e., having high disease activity), EDSS ≤ 6.0, and signed consent to participate. Exclusion criteria: co-morbidities that prevent study participation (specifically dementia, serious cognitive disorders or other disorders affecting physical function). Of note, participants could withdraw from the study at any time and for any reason without prejudice to his or her future medical care. In case of serious adverse events, we were obliged to contact the relevant MS clinic, the regional ethical committee and to the study sponsor.
Body composition
Body composition was assessed by use of a Dual Energy X-ray Absorptiometry (DXA) scanner (GE Lunar DXA scan, GE Healthcare, Madison, WI, United States). The system’s software package (enCORE software v16.0) was used to determine whole body mass (kg), fat mass [absolute (kg), relative to whole body mass (%)], lean mass (absolute (kg), relative to whole body mass (%)) and bone mineral content (kg). In contrast to the remaining outcomes, DXA scans were not performed at 3- and 6-month follow-up, but only at baseline as well as at 12- and 24-month follow-up.
Neuromuscular function
As described in details elsewhere [38, 39], isometric muscle strength of the knee extensors (KE) at a fixed 70° knee joint angle was performed on the weaker leg (self-reported, most often being the affected side) using an isokinetic dynamometer (Humac Norm, CSMi, Stoughton, Massachusetts, USA) combined with muscle surface electromyography (emg; distal 1/3 of m. vastus lateralis) to evaluate neuromuscular activity (~ neural drive to muscles). Data were sampled at 1500 Hz (wireless TeleMyo Direct Transmission System and MyoResearch Software, Noraxon, Scottsdale, Arizona, USA) and subsequently low-pass filtered (6 Hz) and analysed using custommade software (MathWorks, MatLab 2017, Natick, MA, USA). In addition to low-pass filtering, emg data were furthermore full-wave rectified, resulting in a linear envelope, from which mean average voltage was calculated in a 250 ms interval preceding the time where the maximal KE muscle strength was determined to occur. Following two initial submaximal familiarization/warm-up trials (at approximately 50 and 80% of maximal effort), participants performed 3–5 maximal KE muscle contractions interspersed by 60-s rest periods. The trial with the highest KE muscle strength was selected for further analyses. Participants received strict instructions to contract as fast and forcefully as possible. Strong verbal encouragement along with visual feedback were provided during all trials. KE muscle strength was presented normalized to body mass (Nm kg−1). KE emg raw values (µV) was presented normalized to maximal KE muscle strength [40].
Isometric handgrip (HG) muscle strength was performed on the weaker hand (self-reported, most often being the affected side) using a hydraulic hand dynamometer with adjustable grip (SAEHAN, SH5001, Masan, Korea). The test was performed with the arm extended down the side of the body. Following 2 initial submaximal familiarization/warm-up trials (at approximately 50 and 80% of maximal effort), participants performed 3–5 maximal HG muscle contractions interspersed by 60 s rest periods. The trial with the highest HG muscle strength (N) was seleted for further analyses. Participants received strict instructions to contract as forcefully as possible for at least 3 s.
Aerobic capacity
As described in details elsewhere [41], aerobic capacity (~ maximal oxygen uptake; VO2max) was assessed using an incremental exercise test until exhaustion on a stationary bicycle ergometer (SRM, Jülich, Germany). The test was conducted at a self-chosen cadence between 55 and 95 revolutions per minute with an initial 5-min warm up at 40 W, followed by increments of 10 W/min (women) or 15 W/min (men) until voluntary exhaustion. The rate of oxygen uptake (VO2), carbon dioxide release (VCO2), and respiratory exchange ratio (RER) was determined continuously by an online respiratory gas exchange analyser (Oxigraf O2CPX, Oxigraf Inc., Sunnyvale, CA, USA) and analysed using commercially available software (Indoor 8.00 software, Innovision ApS, Glamsbjerg, Denmark). Heart rate was monitored by a Polar watch (Polar A300, Oulu, Finland). Participants were verbally encouraged to continue the test as long as possible, and were asked to rate their perceived exhaustion (RPE) after voluntary exhaustion using the 6–20 Borg scale [42]. The highest recorded 30-s VO2 average obtained during the test was considered the VO2max. VO2max and was presented normalized to body mass (ml O2 min−1 kg−1).
Physical function
As described in details elsewhere [38, 43,44,45,46], six objective tests representing different physical tasks was used to comprehensively evaluate physical function. The 6-min walk test (6MWT; primary outcome) was assessed on a 30-m track, to evaluate walking endurance [43]. Participants were instructed to walk as far a distance as possible (presented in m). The timed 25-ft walk test (T25FWT) was assessed on a 25-feet track (corresponding to 7.62 m), to evaluate simple short distance walking involving horizontal propulsion/acceleration [43]. Participants were instructed to walk as fast as possible (presented in m s−1). The best of two trials was selected for further analysis. The six spot step test (SSST) was assessed on a specially designed 5-m track with five wooden blocks (placed 1 m apart in the x–y plane), to evaluate complex short distance walking involving coordination and dynamic balance [44]. Participants were instructed to walk as fast as possible (presented in s). The average of four trials (two with left foot only, two with right foot only) was used for further analysis. The 9-step stair ascend (9SSA) was assessed on an indoor standard flight of stairs (depth 29 cm, height 17 cm), to evaluate vertical walking propulsion/acceleration [38]. Participants were instructed to walk as fast as possible (presented in s). The best of two trials was selected for further analysis. The timed up and go test (TUG) was assessed on a specially designed 3-m track with 1 chair and 1 turning point/cone, to evaluate the more functional components of mobility and transfer from sit to stand [45]. Participants were instructed to rise from the chair, walk as fast as possible to the turning point and then return to sit down on the chair (presented in s). The best of two trials was selected for further analysis. The five times sit to stand test (5STS) was assessed using a chair without armrests, to evaluate muscle mechanical function of the lower extremities (of relevance to walking) [46]. Participants were instructed to rise and sit down as fast as possible (presented in s). The best of two trials was selected for further analysis.
Cognitive function
As described in details elsewhere [41, 47], two objective tests representing different tasks were used to assess cognitive function. The selective reminding test (SRT) was used to assess verbal learning and memory consisting of both the long term storage test (SRT_LTS) and the consistent long term retrieval test (SRT_CLTR) [47]. The oral version of the SDMT was used to assess sustained attention and information processing speed [47]. The final part of the SRT will consist of the delayed recall test (SRT_D) [47]. The tests were performed in that order, yet alternating between three different versions of SDMT and SRT across the test sessions. The latter was done to avoid the well-known learning effect when repeating these cognitive tests [48].
Patient-reported outcomes
Four different reliable and validated questionnaires were used to obtain patient-reported ratings of both disease severity and symptoms, i.e., entirely from the patients’ perspective. The multiple sclerosis impact scale-29 (MSIS29) [49] was applied to assess the physiological and psychological impact of MS. Each of the 29 items of the MSIS29 were scored 1–5, and then transformed into a total score ranging from 0 to 100 (higher scores, greater impact). The 12-item multiple sclerosis walking scale (MSWS12) [50] was used to assess the impact of MS on walking abilities and mobility. Each of the 12 items of the MSWS12 was scored 1–5, and then transformed into a total score ranging from 0 to 100 (higher scores, greater impact). The modified fatigue impact scale (MFIS) [51] was used to assess the physical, cognitive and psychosocial impact of fatigue. Each of the 21 items of the MFIS were scored 0–4 for each, providing a total score ranging from 0 to 84 (higher scores, greater fatigue impact). Finally, the hospital anxiety and depression scale (HADS) [52] was applied to assess anxiety and depression. Each of the 14 items of the HADS was scored 0–3, providing a total score for anxiety and depression, respectively, ranging from 0 to 21 (higher scores, greater anxiety and/or depression).
Physical activity
To understand potential physical activity lifestyle changes and as described in details elsewhere [24], this was assessed objectively by use of thigh-worn accelerometry (Axivity AX3, Axivity Ltd, Newcastle, UK) for 7 consecutive days at home. The device was attached to the weaker/affected leg (mid-anterior thigh). Raw activity data were sampled at 100 Hz (± 8 g), downloaded using the OMGUI software (version 1.0.29). The data were subsequently exported to a ActiGraph as a raw binary file (gt3x) and processed into counts using the ActiLife software (version 6.4.11). Data reduction and aggregation was done using the custom-built software (Propero by Jan Christian Brønd, Odense, Denmark). Vector magnitude counts data were analysed in 30 s epochs over an 18-h time span starting at 6AM. Non-wear time was defined as time periods of ≥ 10 min consecutive zeros, and was excluded. Eight hours of accepted data had to be reached per day for a minimum of 4 days in order for the data to be valid and subsequently included. Ultimately, physical activity is presented as counts per minute (CPM). Following the 7 days of wearing the accelerometer, participants returned it by mail.
Statistics
We intended to base our sample size calculation on expected effects on the 6MWT. This was chosen as the primary outcome since it is among the most commonly used measures of walking capacity in pwMS, regarded as the golden standard [43], among the most impaired outcomes of physical function in pwMS [8], and rated as highly important by pwMS [14, 15]. While we were unable to identify any studies that examined the effects Alemtuzumab treatment on 6MWT, we assumed that the magnitude of the expected effects on 6MWT would be comparable to reported changes on MSFC from a previous study (mean effect size (change) in MSFC z-score of ~ 0.05 after 6 and 24 months of treatment) [30]. Therefore, an a priori sample size calculation for a repeated measure one-way ANOVA was performed, accounting for our design with one group and five repeated measures. A statistical power of 0.8, an alpha of 0.05 and an expected effect size of 0.05 rendered a required sample size of n = 49. Including an expected dropout of approximately 20% over 2 years, due to potential side effects and the natural dropouts occurring in scientific studies, a total sample size of n = 60 was deemed necessary.
Statistical analyses were performed using STATA (IC 14, StataCorp, College Station, TX, USA). An intention-to-treat linear mixed effects model (participant id set as a random effect, time points set as a fixed effect) was carried out, establishing change scores for all outcomes at follow-up time points, taking into account baseline levels. Hence, all participant data were included regardless of their compliance to the prospective study. Data at baseline are presented as mean ± SD for normally distributed data or as median [interquartile range (IQR)] for non-normally distributed data, whereas changes at follow-up time points relative to baseline are displayed as mean [95% confidence interval (CI)]. Normal distribution was tested by inspecting the standardized residuals (i.e., QQ-plots, plots of the standardized residuals against the fitted values) for each outcome. The level of statistical significance was set at p < 0.05 (“certain finding”) and p < 0.01 (“highly certain finding”) accompanied by interpretation of the confidence interval width (i.e., variability). We also evaluated the changes in 6MWT and SDMT in relation to established clinical cut-off change scores, as both the 6MWT and the SDMT are considered sentinel for impairments in physical and cognitive function, respectively. The cut-off score was 22 m for the 6MWT [53] and 4 points for the SDMT [54], from which pwMS were classified into the categories of improvers (positive changes at or beyond the cut-off scores), maintainers (changes not reaching the cut-off scores) or decliners (negative changes at or beyond the cut-off scores). Lastly, to understand whether the study participants were deemed to have impairments in physical and cognitive function at baseline, we used normative data obtained from healthy individuals for the 6MWT (n = 150, 51% females, mean age 35) [8] and the SDMT (n = 140, 56% females, mean age 46) [55] to calculate z-scores. Participants were classified as impaired if the individual z-scores were ≥ 1.5 standard deviation (SD) unit below the mean of published norms. Graphical presentations were made in GraphPad Prism 7.0 (GraphPad Software, La Jolla, CA, USA, www.graphpad.com).
Results
Descriptive and clinical data
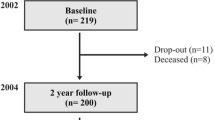
Demographic and clinical characteristics at baseline are summarized in Table 2. A total of n = 17 relapse-remitting MS patients (12 (71%) females, 35.8 years) with a mean EDSS of 3.0 were included in the present study. Participants mainly initiated Alemtuzumab treatment due to inadequate response to prior therapy. While no serious adverse events were registered during the 24-month study period, n = 1 participant were temporarily excluded from the study (around 12-month follow-up) due to suspected treatment-induced cardiac events (we were informed by the neurologist/MS clinic at which the participant was affiliated), yet later re-enrolled after thorough medical examinations as it was determined to have been relapses. After the 6-month follow-up test session, n = 2 participants dropped out due to personal reasons, neither related to the treatment nor the testing.
Body composition and physiological function
Body composition and physiological function at baseline and follow-up are summarized in Table 3. Except for transient increases in body mass and lean mass at 12-month follow-up (that had disappeared at 24 months) along with a trend towards a decrease in bone mineral content at 24 months follow-up, all body composition outcomes remained stable throughout the study period.
KE muscle strength (along with the corresponding neuromuscular activity; KE emg), HG muscle strength and VO2max also remained stable throughout the study period.
At all time points during VO2max testing, participants reached heart rate values that corresponded to 93 ± 3% of age-estimated maximal heart rate (208–0.7 × age), RER values = 1.21 ± 0.12 and Borg values = 18.0 ± 1.2 (data not shown).
Physical function
Physical function at baseline and follow-up are summarized in Table 3. In relation to the primary and first sentinel outcome, 6 MWT, n = 7/17 (41%) participants (including n = 1 that could not physically perform the test) were classified as impaired at baseline, based on having z-scores ≥ 1.5 SD unit below the mean of published norms.
While 6MWT remained stable throughout the study period, T25FWT and SSST improved at both 12- and 24-month follow-up (Fig. 1). According to the established clinical cut-off score for 6MWT, 331/3 % was categorized as improvers, 462/3 % as maintainers, and 20% as decliners. All other physical function outcomes remained stable throughout the study period.
Physical function. Delta changes in 6MWT (A), T25FWT (B) and SSST (C). Data are shown as mean [95%CI] changes from Baseline to 3 months, 6 months, 12 months and 24 months follow-up, respectively. Arrows denote direction of positive adaptations. Statistics: *denote p < 0.01, *denote p < 0.05. For 6MWT, dotted lines denote established clinical cut-off scores (22 m) [53]. 6MWT: 6-min walk test. T25FWT: timed 25-foot walk test. SSST: six spot step test. See Table 3 for baseline data and exact values along with data on remaining physical function outcomes
Cognitive function
Cognitive function at baseline and follow-up are summarized in Table 3 and Fig. 2. In relation to the second sentinel outcome, SDMT, n = 0/17 (0%) participants were classified as impaired at baseline, based on having z-scores ≥ 1.5 SD unit below the mean of published norms.
Cognitive function. Delta changes in SDMT (A), SRT_LTS (B), SRT_CLTR (C) and SRT_D (D). Data are shown as mean [95%CI] changes from Baseline to 3 months, 6 months, 12 months and 24 months follow-up, respectively. Blue arrows denote direction of positive adaptations. Statistical analysis: *denote p < 0.01, *denote p < 0.05. For SDMT, dotted lines denote established clinical cut-off scores (4 points) [54]. SDMT: symbol digit modalities test. SRT selective reminding test, LTS long term storage, CLTR consistent long term retrieval, D delayed. See Table 3 for baseline data and exact values
While most outcomes improved at 3- and 12-months follow-up, all cognitive function outcomes improved at 24-months follow-up. According to the established clinical cut-off score for SDMT, the mean improvement in SDMT were above this cut-off score, and 531/3 % was categorized as improvers, 331/3 % as maintainers, and 131/3 as decliners.
Patient-reported outcomes
Patient-reported outcomes at baseline and follow-up are summarized in Table 3. At baseline, n = 4/17 (24%) met the criteria for anxiety and n = 2/17 (12%) met the criteria for depression (HADS cut-off score for both outcomes: ≥ 8 [52]), n = 8/17 (47%) met the criteria for having high levels of fatigue (MFIS total cut-off score: ≥ 38 [56]), n = 1/17 (6%) met the criteria for having high physical impact of MS and n = 10/17 (59%) met the criteria for having high psychological impact of MS (MSIS29 physical and psychological cut-off scores: ≥ 61 and ≥ 25, respectively [49, 57]).
MSIS29 (total, physiological, psychological), MSWS12, MFIS (total, physical, cognitive, psychosocial) and HADS (anxiety, depression) all remained stable throughout the study period.
Physical activity
Physical activity (baseline 776 ± 215 cpm) also remained stable throughout the study period (change scores: 3 months = 66 [− 78:210]; 6 months = 3 [− 131:137]; 12 months = 81 [− 62:223]; 24 months = 25 [− 115:166]).
Discussion
The present study prospectively assessed the changes in multiple measures of (1) physiological outcomes related to physical function, (2) objectively assessed physical function, (3) objectively assessed cognitive function, and (4) patient-reported outcomes during the first 2 years of Alemtuzumab treatment in relapsing–remitting pwMS. The primary outcome, 6MWT, remained stable throughout the Alemtuzumab treatment period, whereas improvements were observed at 24-month follow-up in T25FWT and SSST (reflecting simple and complex short distance walking, respectively) as well as in SDMT and SRT (reflecting cognitive processing speed and memory, respectively). The remaining outcomes including physiological adaptations (body composition, bone mineral content, KE and HG muscle strength, VO2max), physical function (9SSA, TUG, 5STS), and patient-reported outcomes (MSIS29, MSWS12, MFIS, HADS) were stable throughout the study period.
A recently published ‘real-world setting’ study presented data on the complete cohort of Danish pwMS (n = 209) that had initiated and received Alemtuzumab treatment between 2009 and 2019 [58]. Compared to that cohort and the specific time period of 2017–2019, the enrolled n = 17 participants of the present study appeared to be quite representative, based on gender (163/43 vs. 12/5 females/males (78 vs. 71% females); present vs. cohort study, respectively), age (35.8 vs. 37.0 years) and EDSS scores (3.0 vs. 3.4). We furthermore established that according to published norm-data, none of the n = 17 participants were classified as cognitively (SDMT) impaired, whereas 41% were classified as being physically (6 MWT) impaired. While recollecting the highly individual development and presentation of symptoms, some study findings are in support of this notion, with physical function becoming earlier affected and impaired compared to cognitive function [10], and with physical function (walking capacity in specific) being reported by pwMS to influence health more than cognitive function [14]. In addition, 47% met the criteria for having high levels of fatigue, which also influence health to a large extent [14], and 59% met the criteria for having high psychological impact of MS. This information must be kept in mind when interpreting the potential effects elicited by Alemtuzumab treatment on the different outcome measures of the present study (discussed and elaborated below). It may be speculated that outcomes already impaired at baseline may be particularly responsive to treatment.
To the best of our knowledge, no previous studies have examined the effects of Alemtuzumab treatment on measures of body composition or physiological function in pwMS. As for body composition, a transient increase in body and lean mass at 12-month follow-up were observed, that returned to baseline levels at 24-month follow-up. This is likely due to the Alemtuzumab treatment per se and/or transient lifestyle changes following the Alemtuzumab treatment initiation, but apparently not due to physical activity levels as these remained stable (3% increase) throughout the study period. Of note, the latter may serve as a somewhat positive study finding as physical activity has been shown to decline over a 24-month period, corresponding to -8% in free-living pwMS [59]. Whole body bone mineral content showed a trend towards a decline at 24-month follow-up (with some uncertainty in the 95%CI), corresponding to a ~ 0.5% decline per year. This appear to be slightly greater than that observed in a healthy population of comparable age and gender composition (~ 0.2% decline per year) [60]. It is well known that bone health is preferentially negatively affected by MS and increasing the risk of bone fracture(s) [61], but we can only speculate whether our bone health findings were caused by changes in lifestyle factors (but not physical activity levels), the Alemtuzumab treatment per se, and/or other underlying risk factors. All measures of physiological function (i.e., KE and HG muscle strength, KE neuromuscular activity, and aerobic capacity) remained stable across the treatment period. We are unaware of any longitudinal studies involving pwMS that have reported data on KE neuromuscular activity or aerobic capacity, yet one study did report data on KE and HG muscle strength, with approximately 1/3 of their study participants receiving DMDs (yet assumable not Alemtuzumab). In comparison to the present study findings at 24-month follow-up (KE muscle strength + 5%, HG muscle strength 0%), KE and HG muscle strength slightly deteriorated after 24 months in the identified study (− 2% and − 5%, respectively) [62]. This may indicate a somewhat positive impact of Alemtuzumab on KE muscle strength. Intuitively it makes sense that no substantial improvements were observed as this normally require a substantial stimulus, e.g., as evidenced from studies examining the effects of moderate-to-high intensity exercise [23, 63]. The fact that KE and HG muscle strength, and especially neuromuscular activity (obtained during maximal KE muscle strength testing) argued to be a proxy measure of CNS function, remained stable may suggest beneficial effects of Alemtuzumab. Normally, the ability to produce maximal motor output from the CNS to skeletal muscles deteriorates due to disease progression [64] as does muscle strength [65]. This was indirectly supported by the measures of physical function that are known to rely on maximal motor output / lower extremity muscle strength, i.e., 9SSA, TUG, and 5STS (discussed in detail below) [38, 66], as they also remained stable.
While most physical function outcomes (including the primary study outcome, 6MWT) remained stable throughout the 24-month, improvements were observed in T25FWT and SSST. In comparison to the present study findings, we are aware of longitudinal studies involving pwMS that have reported data on 6MWT and T25FWT, but not on SSST, 9SSA, TUG or 5STS. The participants of these studies have either received unspecified DMDs (yet assumable not Alemtuzumab), specified DMDs yet never Alemtuzumab, or no DMDs. After 12–24 months of follow-up, 6MWT has been reported to remain stable or deteriorate slightly (ranging from − 2 to − 7%) [62, 67]. In comparison, 6MWT changed by approximately -2.5% in the present study. This was paralleled by a somewhat equally distributed number of participants categorized as improvers/maintainers/decliners according to clinical cut-off scores. Hence, the findings on 6MWT do not strongly support that outcomes impaired at baseline are particularly responsive to treatment. Additionally, after 12–24 months of follow-up, T25FWT (or other simple short distance walk tests) has been reported to remain stable or deteriorate slightly (ranging from 0 to − 6%) [31, 62, 67,68,69]. In comparison, T25FWT improved by approximately 8% in the present study (n = 3/15 categorized as improvers based on the clinical cut-off score of 20% [70], n = 12/15 categorized as maintainers; data not shown), accompanied by SSST that improved by approximately 10%. These substantial improvements (with certainty in the 95% CI) strongly support that Alemtuzumab had beneficial effects on these two specific outcomes. As discussed in detail elsewhere [38, 44, 46], the measures of physical function that were included in the present study appear to be preferentially influenced by different physiological ‘systems’, such as muscle strength/power, muscle control/coordination, and aerobic capacity. In support of this notion, our findings on physiological function and physical function generally seems to be aligned, i.e., with stable 6MWT levels (relying preferentially on aerobic capacity and endurance) and VO2max along with stable levels of 9SSA/TUG/5STS (relying preferentially on muscle strength/power) and KE muscle strength. In contrast, SSST (and to some extent T25FWT) appear preferentially influenced by muscle control/coordination [44], although this was not assessed in the present study. Nevertheless, it may be speculated that Alemtuzumab can positively affect the ability to produce submaximal motor output from the CNS to one or more skeletal muscles, and thereby enhancing muscle control/coordination, as supported by the improvements in SSST as well as in T25FWT.
The observed improvements in cognitive function (processing speed = SDMT, memory = SRT) following 24 months of Alemtuzumab treatment verify the previously shown positive effects on processing speed [31, 36]. In the study by Riepl and colleagues including n = 21 relapsing–remitting pwMS [36], they reported a mean improvement in SDMT of 4.3 points following 15 months of Alemtuzumab treatment (i.e., approximately 3 months after 2nd treatment), thus exceeding the clinical cut-off score of 4 SDMT points [54]. A total of 57% (n = 12/21) of their participants improved ≥ 4 SDMT points. We observed a somewhat comparable mean improvement in SDMT of 5.2 points after 24 months of Alemtuzumab treatment (i.e. approximately 12 months after the 2nd treatment), also exceeding the clinical cut-off score. Moreover, 53% (n = 8/15) of our participants improved ≥ 4 SDMT points. As with 6MWT, the findings on SDMT do also not strongly support that impaired outcomes are particularly responsive to treatment. In the much larger study by Giovannoni and colleagues including n = 426 relapsing–remitting pwMS [31], they reported a significant improvement in PASAT following 24 months of Alemtuzumab treatment, thus supporting our findings. An important notion to consider is the extent of 24-month changes that could have been expected without Alemtuzumab treatment initiation. Healy and colleagues provided longitudinal data on a large cohort of pwMS (n = 680, mixed sample with some receiving unspecified DMDs and others not), and from those having a baseline SDMT score of approximately 54 (corresponding to our sample), scores remained unaffected or slightly declined over a 24-month period [71]. This information, along with the fact that we alternated between three different versions of SDMT (and SRT) to minimize the well-known learning effect in this test [48], suggest that our observed improvements in SDMT are robust. As for verbal memory, the observed minor improvements in the rey auditory verbal learning test by Riepl and colleagues did not reach statistical significance [36]. In contrast, we observed improvements in SRT (across all subscores; including long term storage, consistent long-term retrieval, and delayed recall). This discrepancy are difficult to explain, but may be due to the slight difference in administering as well as content of these tests of verbal memory, e.g., in SRT all words are recited during the first trial, while in the rey auditory verbal learning test all words are recited during each trial, and in the scoring hereof.
We included four different patient-reported outcomes (MSIS29, MSWS12, MFIS, and HADS) to help elucidate how Alemtuzumab would affect different domains including disease severity and symptoms, entirely from the patients’ perspective. To the best of our knowledge, we are the first to report data on these specific outcomes in pwMS receiving Alemtuzumab treatment. In the previously mentioned CARE-MS studies, health-related quality of life measures were applied, revealing statistically certain improvements, at or in the vicinity of clinical cut-off scores, after 24-month treatment [outcomes: SF36, FAMS, and the European quality of life 5 dimensions (EQ-5D)] [37]. In contrast, the patient-reported outcomes of the present study, MSIS29, MSWS12, MFIS, and HADS, all remained stable throughout the 24-month Alemtuzumab treatment period. From one point, these divergent findings may indicate that the present study findings are negative (or neutral). From another point, however, the outcomes of the present study do not readily reflect health-related quality of life. Beyond Alemtuzumab studies, previously reported 24-month longitudinal data involving ‘mixed participants in relation to DMDs’ have revealed stable MSIS29 scores [69, 72, 73], although with some minor numerical reductions (i.e., positive effect) in the MSIS29 psychological score [69] as well as some increments (i.e., negative effect) in the MSIS29 physiological score [73], but apparently not beyond the clinical cut-off score of 8 [49]. In contrast, previous 24-month longitudinal data have revealed consistent increments (i.e., negative effect) in the MSWS12 (ranging from + 1.5 points to + 5.0 points) [59, 73]. While these changes are also not beyond the clinical cut-off score of 8–10 [53, 74], the findings of the present study may indicate that Alemtuzumab positively influences and stabilizes MSWS12. As with MSIS29, previous 24-month longitudinal data have revealed stable MFIS total scores (along with the fatigue severity scale (FSS) scores) [59, 75], but also reductions (i.e., positive effect) in MFIS total scores [76] beyond the clinical cut-off score of 4 [77]. While we do observe a pattern of reductions in the MFIS total score, weakly supporting a beneficial role of Alemtuzumab treatment on the impact of MS fatigue, the 2-point reduction is well below this clinical cut-off score. Lastly, previous 24-month longitudinal data have revealed stable HADS scores (along with scores from other anxiety and depression measures) [59, 76]. This appear fully aligned with the present study observations on HADS scores.
Methodological considerations
A number of limitations must be taken into account when interpreting the findings of the present study. First and most critical, the small sample size (well below the estimated sample size of n = 60) reduced the power of the study and may specifically have increased the risk of type II errors. Despite this, our sample appeared representative of Danish pwMS receiving Alemtuzumab [58]. Second, no control group was used in the present study and thus also no randomization was carried out. While these aspects are preferable, this was deemed unethical as all enrolled pwMS started Alemtuzumab treatment due to inadequate response to prior therapy and had high disease activity at the time of enrolment. Third, due to the EU General Data Protection Regulation (GDPR), we were unable to include information about preceding/ongoing number of relapses or MRI activity (mean number of T2/Flair hyperintense lesions and/or gadolinium enhancing lesions). All involved MS patients were nevertheless highly active MS patients as stated above, which was a requirement for initiating Alemtuzumab according to national guidelines and the most recent SmPC at the time of the study. We speculate that the majority of MS patients benefitted from the treatment, e.g., by reducing clinical relapses, brain lesions and brain atrophy over the 2-year intervention period, as previously reported [18, 19, 30,31,32,33,34]. This would likely be associated with the stabilizing/improving effects observed across most of the outcomes of the present prospective observational study. Future studies should include both type of outcomes. Fourth, few available longitudinal studies could be identified and used for comparison. Moreover, those we did identify, had mixed participant samples with some receiving unspecified DMDs (yet assumed rarely to involve Alemtuzumab) and others not, as well as divergent disease profiles (e.g., lower/higher EDSS scores, time since diagnosis, and age; different gender proportions; including both relapsing–remitting and progressive pwMS). Altogether, this introduces variability and challenges the direct comparison.
Clinical implications and perspectives
The present study findings verify that Alemtuzumab treatment elicit improvements in cognitive function, particularly processing speed [36], at a level surpassing clinical cut-off scores. We also provide novel insight into physiological function, physical function, and patient-reported outcomes, with Alemtuzumab treatment eliciting improvements in simple and complex short distance walking. Also, compared to other 24-month longitudinal study findings reporting deterioration in many outcome measures, our findings may suggest potential stabilizing effects of Alemtuzumab on KE muscle strength and MSWS12. Due to the limitations of the present study (e.g., small sample size), future larger and more long-term studies should help expand our understanding further on the effects of Alemtuzumab treatment on such domains. In that context, it is relevant to longitudinally follow a group of pwMS receiving other types of DMDs (or not at all if deemed ethically), to understand the true effects of Alemtuzumab. Moreover, a combination of exercise and Alemtuzumab could potentially be very potent as this non-pharmacological and pharmacological treatment, respectively, supplement and reinforce each other across all the domains of the present study [23].
Despite our positive interpretation of the present study findings, attention must of course also be directed towards the several severe adverse effects that sometimes accompany Alemtuzumab treatment in pwMS [32,33,34]. All available information must therefore be taken into consideration when deciding on initiating Alemtuzumab treatment in relapsing–remitting pwMS, a process that should involve both physician and patient.
Conclusion
Alemtuzumab treatment for 2 years in relapsing–remitting pwMS elicits improvements in cognitive function, specifically in processing speed (SDMT) and memory (SRT), with the improvements in processing speed being clinically relevant. Moreover, improvements in some outcomes of physical function were also observed, specifically in short distance walking capacity relying on motor control (T25FWT, SSST). The primary outcome, the 6 MWT, along with all remaining outcomes were stable throughout the Alemtuzumab treatment period.
References
GBD_MS_Collaborators (2019) Global, regional, and national burden of neurological disorders, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 18(5):459–480
Reich DS, Lucchinetti CF, Calabresi PA (2018) Multiple sclerosis. N Engl J Med 378(2):169–180
Vollmer T et al (2016) Relationship between brain volume loss and cognitive outcomes among patients with multiple sclerosis: a systematic literature review. Neurol Sci 37(2):165–179
Rocca MA, Comi G, Filippi M (2017) The role of T1-weighted derived measures of neurodegeneration for assessing disability progression in multiple sclerosis. Front Neurol 8:433
Planche V et al (2016) Cognitive impairment in a population-based study of patients with multiple sclerosis: differences between late relapsing-remitting, secondary progressive and primary progressive multiple sclerosis. Eur J Neurol 23(2):282–289
Ruano L et al (2017) Age and disability drive cognitive impairment in multiple sclerosis across disease subtypes. Mult Scler 23(9):1258–1267
Larocca NG (2011) Impact of walking impairment in multiple sclerosis: perspectives of patients and care partners. Patient 4(3):189–201
Hvid LG et al (2020) Accelerated trajectories of walking capacity across the adult life span in persons with multiple sclerosis: an underrecognized challenge. Neurorehabil Neural Repair 34(4):360–369
DeLuca GC et al (2015) Cognitive impairment in multiple sclerosis: clinical, radiologic and pathologic insights. Brain Pathol 25(1):79–98
Kister I et al (2013) Natural history of multiple sclerosis symptoms. Int J MS Care 15(3):146–158
Thrue C et al (2020) Time matters: early-phase multiple sclerosis is accompanied by considerable impairments across multiple domains. Mult Scler 27:1352458520936231
Kalron A, Achiron A, Dvir Z (2011) Muscular and gait abnormalities in persons with early onset multiple sclerosis. J Neurol Phys Ther 35(4):164–169
Giovannoni G et al (2016) Brain health: time matters in multiple sclerosis. Mult Scler Relat Disord 9(Suppl 1):S5–S48
Green R et al (2017) Which symptoms contribute the most to patients’ perception of health in multiple sclerosis? Mult Scler J Exp Transl Clin 3(3):2055217317728301
Heesen C et al (2018) Perceptions on the value of bodily functions in multiple sclerosis. Acta Neurol Scand 137(3):356–362
McGinley MP, Goldschmidt CH, Rae-Grant AD (2021) Diagnosis and treatment of multiple sclerosis: a review. JAMA 325(8):765–779
Torkildsen Ø, Myhr KM, Bø L (2016) Disease-modifying treatments for multiple sclerosis - a review of approved medications. Eur J Neurol 23(Suppl 1):18–27
Favaretto A et al (2018) Effects of disease modifying therapies on brain and grey matter atrophy in relapsing remitting multiple sclerosis. Mult Scler Demyelinating Disord 3(1):1
Iaffaldano P et al (2021) Long-term disability trajectories in relapsing multiple sclerosis patients treated with early intensive or escalation treatment strategies. Ther Adv Neurol Disord 14:17562864211019574
Landmeyer NC et al (2020) Disease-modifying treatments and cognition in relapsing-remitting multiple sclerosis: a meta-analysis. Neurology 94(22):e2373–e2383
Lanzillo R et al (2020) A snapshot on patient-reported outcome measures of people with multiple sclerosis on first-line therapies in a real world setting. Neurol Sci 41(11):3235–3241
Nowinski CJ, Miller DM, Cella D (2017) Evolution of patient-reported outcomes and their role in multiple sclerosis clinical trials. Neurotherapeutics 14(4):934–944
Dalgas U et al (2019) Exercise as medicine in multiple sclerosis-time for a paradigm shift: preventive, symptomatic, and disease-modifying aspects and perspectives. Curr Neurol Neurosci Rep 19(11):88
Rooney S et al (2019) Physical activity is associated with neuromuscular and physical function in patients with multiple sclerosis independent of disease severity. Disabil Rehabil, p 1–8
Snook EMM, Mojtahedi C et al (2005) Physical activity and body composition among ambulatory individuals with multiple sclerosis. Intern J MS Care 7(4):137–142
Cleland BT et al (2020) Determinants of low bone mineral density in people with multiple sclerosis: role of physical activity. Mult Scler Relat Disord 38:101864
Cox AL et al (2005) Lymphocyte homeostasis following therapeutic lymphocyte depletion in multiple sclerosis. Eur J Immunol 35(11):3332–3342
Jones JL et al (2009) IL-21 drives secondary autoimmunity in patients with multiple sclerosis, following therapeutic lymphocyte depletion with alemtuzumab (Campath-1H). J Clin Invest 119(7):2052–2061
Thompson SA et al (2010) B-cell reconstitution and BAFF after alemtuzumab (Campath-1H) treatment of multiple sclerosis. J Clin Immunol 30(1):99–105
Coles AJ et al (2012) Alemtuzumab for patients with relapsing multiple sclerosis after disease-modifying therapy: a randomised controlled phase 3 trial. Lancet 380(9856):1829–1839
Giovannoni G et al (2016) Alemtuzumab improves preexisting disability in active relapsing-remitting MS patients. Neurology 87(19):1985–1992
Ziemssen T, Thomas K (2017) Alemtuzumab in the long-term treatment of relapsing-remitting multiple sclerosis: an update on the clinical trial evidence and data from the real world. Ther Adv Neurol Disord 10(10):343–359
Li H et al (2020) Comparative efficacy and acceptability of disease-modifying therapies in patients with relapsing-remitting multiple sclerosis: a systematic review and network meta-analysis. J Neurol 267(12):3489–3498
Liu Z et al (2021) Disease modifying therapies in relapsing-remitting multiple sclerosis: a systematic review and network meta-analysis. Autoimmun Rev 20(6):102826
Fernandez O (2014) Alemtuzumab in the treatment of multiple sclerosis. J Inflamm Res 7:19–27
Riepl E et al (2017) Alemtuzumab improves cognitive processing speed in active multiple sclerosis-a longitudinal observational study. Front Neurol 8:730
Arroyo González R et al (2017) Alemtuzumab improves quality-of-life outcomes compared with subcutaneous interferon beta-1a in patients with active relapsing-remitting multiple sclerosis. Mult Scler 23(10):1367–1376
Sieljacks PS et al (2020) Lower extremity muscle strength across the adult lifespan in multiple sclerosis: implications for walking and stair climbing capacity. Exp Gerontol 139:111025
Kjolhede T et al (2015) Neuromuscular adaptations to long-term progressive resistance training translates to improved functional capacity for people with multiple sclerosis and is maintained at follow-up. Mult Scler 21(5):599–611
Farina D et al (2010) Decoding the neural drive to muscles from the surface electromyogram. Clin Neurophysiol 121(10):1616–1623
Langeskov-Christensen M et al (2018) Aerobic capacity is not associated with most cognitive domains in patients with multiple sclerosis—a cross-sectional investigation. J Clin Med 7(9):272
Borg GA (1982) Psychophysical bases of perceived exertion. Med Sci Sports Exerc 14(5):377–381
Gijbels D et al (2012) Which walking capacity tests to use in multiple sclerosis? A multicentre study providing the basis for a core set. Mult Scler 18(3):364–371
Callesen J et al (2019) How much does balance and muscle strength impact walking in persons with multiple sclerosis? A cross-sectional study. Mult Scler Relat Disord 29:137–144
Podsiadlo D, Richardson S (1991) The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 39(2):142–148
Moller AB et al (2012) Validity and variability of the 5-repetition sit-to-stand test in patients with multiple sclerosis. Disabil Rehabil 34(26):2251–2258
Rao S (1990) A manual for the brief repeatable battery of neuropsychological tests in multiple sclerosis. Medical College of Wisconsin, Milwaukee
Roar M, Illes Z, Sejbaek T (2016) Practice effect in Symbol Digit Modalities Test in multiple sclerosis patients treated with natalizumab. Mult Scler Relat Disord 10:116–122
Hobart J et al (2001) The Multiple Sclerosis Impact Scale (MSIS-29): a new patient-based outcome measure. Brain 124(Pt 5):962–973
Hobart JC et al (2003) Measuring the impact of MS on walking ability: the 12-Item MS Walking Scale (MSWS-12). Neurology 60(1):31–36
Fisk JD et al (1994) Measuring the functional impact of fatigue: initial validation of the fatigue impact scale. Clin Infect Dis 18(Suppl 1):S79-83
Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 67(6):361–370
Baert I et al (2014) Responsiveness and clinically meaningful improvement, according to disability level, of five walking measures after rehabilitation in multiple sclerosis: a European multicenter study. Neurorehabil Neural Repair 28(7):621–631
Benedict RH et al (2017) Validity of the Symbol Digit Modalities Test as a cognition performance outcome measure for multiple sclerosis. Mult Scler 23(5):721–733
Boringa JB et al (2001) The brief repeatable battery of neuropsychological tests: normative values allow application in multiple sclerosis clinical practice. Mult Scler 7(4):263–267
Flachenecker P et al (2002) Fatigue in multiple sclerosis: a comparison of different rating scales and correlation to clinical parameters. Mult Scler 8(6):523–526
Boeschoten RE et al (2014) A computer-based screening method for distress in patients with multiple sclerosis: a feasibility study. JMIR Res Protoc 3(2):e29
Theodorsdottir A et al (2021) Alemtuzumab treatment in Denmark: a national study based on the Danish Multiple Sclerosis Registry. Mult Scler 27:13524585211003292
Motl RW, McAuley E, Sandroff BM (2013) Longitudinal change in physical activity and its correlates in relapsing-remitting multiple sclerosis. Phys Ther 93(8):1037–1048
Warming L, Hassager C, Christiansen C (2002) Changes in bone mineral density with age in men and women: a longitudinal study. Osteoporos Int 13(2):105–112
Gupta S et al (2014) Osteoporosis and multiple sclerosis: risk factors, pathophysiology, and therapeutic interventions. CNS Drugs 28(8):731–742
Paltamaa J et al (2008) Measuring deterioration in international classification of functioning domains of people with multiple sclerosis who are ambulatory. Phys Ther 88(2):176–190
Taul-Madsen L et al (2021) Is aerobic or resistance training the most effective exercise modality for improving lower extremity physical function and perceived fatigue in people with multiple sclerosis? A systematic review and meta-analysis. Arch Phys Med Rehabilit (In Press)
Mamoei S et al (2020) Neurophysiological impairments in multiple sclerosis-Central and peripheral motor pathways. Acta Neurol Scand 142:401–417
Jorgensen M et al (2017) Muscle strength and power in persons with multiple sclerosis—a systematic review and meta-analysis. J Neurol Sci 376:225–241
Ramari C et al (2020) The importance of lower-extremity muscle strength for lower-limb functional capacity in multiple sclerosis: systematic review. Ann Phys Rehabil Med 63(2):123–137
Filli L et al (2018) Profiling walking dysfunction in multiple sclerosis: characterisation, classification and progression over time. Sci Rep 8(1):4984
Kempen JC et al (2011) Community walking can be assessed using a 10-metre timed walk test. Mult Scler 17(8):980–990
Conradsson D et al (2018) Changes in disability in people with multiple sclerosis: a 10-year prospective study. J Neurol 265(1):119–126
Goldman MD et al (2013) Clinically meaningful performance benchmarks in MS: timed 25-foot walk and the real world. Neurology 81(21):1856–1863
Healy BC et al (2021) Trajectories of Symbol Digit Modalities Test performance in individuals with multiple sclerosis. Mult Scler 27(4):593–602
Costelloe L et al (2008) The longitudinal relationship between the patient-reported Multiple Sclerosis Impact Scale and the clinician-assessed Multiple Sclerosis Functional Composite. Mult Scler 14(2):255–258
Sonder JM et al (2014) Do patient and proxy agree? Long-term changes in multiple sclerosis physical impact and walking ability on patient-reported outcome scales. Mult Scler 20(12):1616–1623
Mehta L et al (2015) Identifying an important change estimate for the Multiple Sclerosis Walking Scale-12 (MSWS-12v1) for interpreting clinical trial results. Mult Scler J Exp Transl Clin 1:2055217315596993
Téllez N et al (2006) Fatigue in multiple sclerosis persists over time: a longitudinal study. J Neurol 253(11):1466–1470
Brown RF et al (2009) Longitudinal assessment of anxiety, depression, and fatigue in people with multiple sclerosis. Psychol Psychother 82(Pt 1):41–56
Rooney S et al (2019) Minimally important difference of the fatigue severity scale and modified fatigue impact scale in people with multiple sclerosis. Mult Scler Relat Disord 35:158–163
Acknowledgements
We thank the study participants for their participation in the present study, along with the neurologists and nurses at the Danish MS clinics involved in the present study.
Funding
Sanofi Genzyme funded the present investigator sponsored study (Grant given to UD), but were not involved in study design, execution, analyses, interpretation, writing or publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Lars G. Hvid has received travel grants and/or teaching honorary from Biogen and Sanofi Genzyme; Egon Stenager ES declare no conflict of interests; Ulrik Dalgas has received research support, travel grants and/or teaching honorary from Biogen, Merck Serono, Novartis, Bayer Schering and Sanofi Aventis as well as honoraria from serving on scientific meetings of Biogen and Sanofi Genzyme.
Conflicts of interest
This study was conducted in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments, and was approved by the ethics committee of the central Denmark region (record 1-10-72-223-16).
Rights and permissions
About this article
Cite this article
Hvid, L.G., Stenager, E. & Dalgas, U. Objectively assessed physiological, physical, and cognitive function along with patient-reported outcomes during the first 2 years of Alemtuzumab treatment in multiple sclerosis: a prospective observational study. J Neurol 269, 4895–4908 (2022). https://doi.org/10.1007/s00415-022-11134-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-022-11134-7