Abstract
Objectives
This study aimed to evaluate the safety and efficacy of mechanical thrombectomy (MT) in patients with acute basilar artery occlusion (BAO) based on the baseline Basilar Artery on Computed Tomography Angiography (BATMAN) score.
Methods
We selected patients from the BASILAR study and analyzed the effects and safety of standard medical therapy (SMT) and MT for patients with documented BATMAN scores. The patients were subgrouped according to their BATMAN score (0–3, 4–6, and 7–10). The primary outcome was a favorable functional outcome (modified Rankin Scale [mRS] ≤ 3) and mortality after 90 days.
Results
This study included 828 patients: 337 with poor BATMAN scores (0–3), 386 with moderate BATMAN scores (4–6), and 105 with good BATMAN scores (7–10). MT was associated with favorable functional outcomes in the poor (adjusted odds ratio [aOR], 11.96; 95% confidence interval [CI], 2.58–55.43; P = 0.002), moderate (aOR, 4.66; 95% CI, 2.11–10.28; P < .001), and good (aOR, 7.71; 95% CI, 2.20–27.02; P = 0.001) BATMAN score subgroups. MT was also associated with low mortality rates in the poor (aOR, 0.10; 95% CI, 0.04–0.27; P < 0.001) and moderate (aOR, 0.31; 95% CI, 0.16–0.57; P = 0.002) BATMAN score subgroups. The BATMAN score was significantly associated with favorable outcomes in both the SMT (aOR, 1.44; 95% CI, 1.08–1.93; P = 0.014) and MT (aOR, 1.31; 95% CI, 1.20–1.44; P < 0.001) groups.
Conclusion
Higher BATMAN scores were associated with improved prognosis and lower mortality rates after 3 months. MT was associated with improved outcomes in patients with low BATMAN scores despite their worse overall outcomes.
Unique identifier
ChiCTR1800014759, 2018/02/03.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Mechanical thrombectomy (MT) has become the first-line treatment for patients with acute ischemic stroke secondary to a large artery occlusion after the outcomes of several randomized clinical trials [1]. Acute basilar artery occlusion (BAO) is a rare but catastrophic condition that accounts for 1% of all strokes, and nearly 80% of patients with BAO die or survive with severe disabilities [2, 3]. Several recent clinical trials have not demonstrated the benefit of intervention [4, 5]. The anatomy and pathology of the posterior circulation differ from those of the anterior circulation; therefore, a possible reason is that we did not select the patients who could benefit from MT. Currently, there are no established criteria for identifying patients with BAO who may benefit from MT.
The scoring system used in earlier studies to evaluate the collateral circulation was mainly based on digital subtraction angiography (DSA) and derived from studies on the anterior circulation [6,7,8]. Currently, the diagnosis of BAO is mainly based on computed tomography angiography (CTA), which is noninvasive and easily accessible [9]. Alemseged et al. proposed the Basilar Artery on Computed Tomography Angiography (BATMAN) score, which is a semi-quantitative CTA-based 10-point scoring system that reflects the condition of the collateral circulation and the thrombus burden of acute BAO patients, for predicting the prognosis of acute BAO patients [10]. A few studies have validated the BATMAN score based on CTA and DSA for acute BAO patients and reported that it demonstrates good accuracy in predicting the prognosis of acute BAO patients [10,11,12]. However, these results were limited by the small samples used in the studies, and the optimal threshold of this score for differentiating patients likely to have a poor outcome has not been determined [11, 12].
The Endovascular Therapy for Acute Basilar Artery Occlusion Study (BASILAR) is a large multicenter registry of BAO patients. In our study, we aimed to analyze and compare the safety and efficacies of MT and standard medical treatment (SMT) based on subgroupings of BATMAN scores (0–2, 3–6, and 7–10). We also sought to explore the relationships between favorable outcomes and baseline BATMAN scores and the time metrics in patients who underwent MT.
Methods
Study population
We selected 828 participants of BASILAR, a nationwide prospective registry study involving 47 comprehensive stroke centers in China that evaluated the association between MT and the clinical outcomes of patients with acute BAO between January 2014 and May 2019 [13]. Signed informed consent was obtained from all patients or their legally authorized representatives. Patients evaluated with the BATMAN score based on CTA were included. BASILAR was registered in the Chinese Clinical Trial Registry (http://www.chictr.org.cn; ChiCTR1800014759), and the study protocol was approved by the ethics committee of the participating centers. The main inclusion criteria were age ≥ 18 years, estimated time presentation of BAO ≤ 24 h, BAO confirmed by CTA, magnetic resonance angiography (MRA), or DSA, treatment with intravenous recombinant tissue plasminogen activator within 4.5 h or intravenous urokinase within 6 h of the estimated time of BAO, and signed the informed consent. The main exclusion criteria were premorbid modified Rankin Scale (mRS) > 2, evidence of cerebral hemorrhage, a lack of follow-up information at 90 days or baseline critical data, current pregnancy or lactation, and/or a serious, advanced, or terminal illness.
Treatments
The patients were divided into SMT and MT groups based on their treatment. Patients in the SMT group were administered intravenous thrombolytics, antiplatelet drugs, anticoagulants, or their combination according to the guidelines for the management of acute ischemic stroke [14]. Patients in the MT group received SMT and underwent MT with aspiration or the use of a stent retriever device, balloon angioplasty, stenting, or a combination of the above approaches.
Variables and grading system
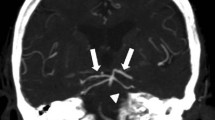
We collected patient data on the baseline characteristics, risk factors for stroke, imaging features, time metrics, process features, and prognosis for analysis. If the time of onset was unknown, the last known time of onset was considered. We used the BATMAN score to assess the collateral circulation and thrombotic burden in patients with BAO, which is a semi-quantitative scoring system based on CTA. In the BATMAN scoring system, 1 point was assigned to each of the proximal (from the proximal origin of the basilar artery to the anterior inferior cerebellar arteries), middle (from the anterior inferior cerebellar arteries to the superior cerebellar arteries), and distal (from the superior cerebellar arteries to its tip) segments of the basilar artery, the intracranial vertebral arteries, and the P1 segment of the posterior cerebral arteries; 2 points were assigned to each non-fetal posterior communicating artery (PCoA); 1 point was assigned if the diameter of the PCoA was < 1 mm; 3 points were assigned if fetal PCoA was present. We divided the patients into three subgroups based on the BATMAN score: 0–3, poor BATMAN score subgroup, 4–6, moderate BATMAN score subgroup; 7–10, good BATMAN score subgroup. Successful reperfusion was defined as a modified postprocedural thrombolysis in cerebral infarction (mTICI) score of 2b–3 at the end of the procedure. An independent core imaging laboratory evaluated the imaging data. Two experienced and trained investigators blinded to the clinical outcomes independently viewed the CTA images. In the case of inconsistent evaluations, a third investigator evaluated and confirmed the results.
Outcomes measurements
The primary efficacy outcome was a favorable outcome, with an mRS score ≤ 3 after 90 days. The secondary efficacy outcomes included functional independence, defined as an mRS score ≤ 2 after 90 days, and successful reperfusion. The safety outcomes included mortality within 90 days and symptomatic intracerebral hemorrhage (SICH) within 48 h, which was defined as a new intracranial hemorrhage confirmed on computed tomography or magnetic resonance imaging with a National Institutes of Health Stroke Scale (NIHSS) score ≥ 4 points or ≥ 2 points in one category before worsening. We evaluated the type of intracerebral hemorrhage using the Heidelberg Bleeding Classification [15]. We also compared the procedural-related complications and severe adverse events as outcome events.
Statistical analysis
The statistical analyses were performed using SPSS version 26.0 (IBM Corp., Armonk, NY, USA) and STATA version 16.0 (StataCorp LLC, TX, USA). Imputation was not needed, because patients with missing key data were excluded from the analysis. For univariate comparisons, the Kruskal–Wallis test or Mann–Whitney U test was applied to continuous variables, and the χ2 test or Fisher’s exact test was applied to categorical variables. The odds ratios (ORs) and 95% confidence intervals (CIs) for the clinical outcomes of MT were assessed using multivariable logistic regression, with adjustments for age, sex, baseline NIHSS score, history of stroke and diabetes, and occlusion sites. We used Spearman correlation to test the correlation between the BATMAN and pc-ASPECTS scores in both groups. By setting the BATMAN score as a continuous variable and other variables to the mean, we generated favorable outcome prediction curves for the treatment modalities.
Only patients who underwent MT were included. We applied multivariable logistic regression to assess the factors associated with favorable outcomes after 90 days by adjusting for variables with P < 0.1 from the univariate analysis. We analyzed the association between onset to puncture time (OPT) or puncture to recanalization time (PRT) and the favorable outcome using adjusted margin plots. In addition, we assessed the probability of a favorable outcome based on the continuous BATMAN score and time metrics. Statistical significance was set at P < 0.05. SigmaPlot version 14.0 (Systat Software, Inc., Chicago, IL, USA) to create the distribution surfaces representing the relationships between the probability of a favorable outcome and the continuous BATMAN score and time metrics and R2 to assess the models.
Results
According to the inclusion and exclusion criteria, we initially screened 1254 patients from 51 comprehensive stroke centers in China. Among them, 4 centers and 22 patients were excluded from participation in the registry, because not all pertinent data on consecutive patients were being recorded. Another 71 patients were excluded, because they had a BAO accompanied by anterior circulation LVO, 121 patients because of a chronic BAO, 187 patients because of missing critical baseline data, and 11 survivors because of lack of 90-day mRS scores. A total of 829 patients were included in the BASILAR study. One patient did not have the BATMAN score and was excluded from our analysis; thus, 828 patients were included in the subgroup analysis. There were 182 and 646 patients in the SMT and MT groups, respectively. The median age was 65 (interquartile range [IQR], 57–74) years; the median NIHSS score was 27 (IQR, 16–33); the median BATMAN score was 4 (IQR, 2–6). A total of 223 patients (26.9%) achieved favorable functional outcomes after 90 days. A total of 429 patients (51.8%) died within 90 days. The interobserver agreement for the grading of the BATMAN score on CTA images was good, with κ = 0.79.
Baseline characteristics
The baseline characteristics for the subgroups based on the BATMAN score and treatment modality are shown in Table 1 and Table I in the Online Resource. Among these three subgroups, the subgroup with good BATMAN scores comprised younger participants and had lower NIHSS scores, less frequent history of coronary heart disease, and a higher prevalence of middle basilar artery occlusion. Other variables were matched between the subgroups.
Outcomes of MT and SMT in subgroups based on the BATMAN score
Only the subgroups based on the BATMAN score were considered. There was a statistically significant difference in the primary efficacy outcomes (P < 0.001). There were also significant differences in the secondary efficacy and safety outcomes (Table 2).
We considered the effect of MT on the outcomes of the BATMAN score subgroups. For the favorable functional outcomes, the three subgroups of the MT group showed significantly better trends (3.0 vs 20.7% in the poor subgroup, P = 0.001; 12.8 vs 38.3% in the moderate subgroup, P < 0.001; 13.2 vs 47.8% in the good subgroup, P < 0.001). Similar results were obtained for functional independence (Table 2). The other outcomes are shown in Table 2. Figure 1 shows the distribution of the mRS score across different subgroups and treatment modalities.
Multivariable analysis (Table 3) showed that MT was associated with favorable functional outcomes in the poor (adjusted OR, 11.96; 95% CI, 2.58–55.43; P = 0.002), moderate (adjusted OR, 4.66; 95% CI, 2.11–10.28; P < 0.001), and good (adjusted OR, 7.71; 95% CI, 2.20–27.02; P = 0.001) BATMAN score subgroups. Similar results were obtained for functional independence (Table 3). The safety outcomes are presented in Table 3.
Outcomes of MT and SMT associated with the numeric BATMAN score
The BATMAN score was considered a continuous variable, and it was significantly associated with favorable outcomes in both the SMT (adjusted OR, 1.44; 95% CI, 1.08–1.93; P = 0.014) and MT (adjusted OR, 1.31; 95% CI, 1.20–1.44; P < 0.001) groups. There was no interaction between the treatment modalities (P = 0.591). Figure 2A shows the relationship between the BATMAN score and the predicted probabilities of favorable outcomes in both treatment groups. Mortality within 90 days decreased as the BATMAN score increased in both SMT (adjusted OR, 0.69; 95% CI, 0.56–0.86; P = 0.001) and MT (adjusted OR, 0.82; 95% CI, 0.75–0.89; P < 0.001) groups, as shown in Fig. 2B. There was no interaction between the treatment modalities (P = 0.102).
Probabilities of favorable outcomes and mortality stratified by treatment modality based on the Basilar Artery on Computed Tomography Angiography (BATMAN) score. A Probability of a favorable outcome increased and was higher in the MT group (mechanical thrombectomy plus standard medical therapy) than in the SMT group (standard medical therapy) with an increase in the BATMAN score. B Probability of death decreased more rapidly in the MT group than in the SMT group with an increase in the BATMAN score
Outcomes of MT associated with the numeric BATMAN score and time metrics
There were significant differences in the favorable outcomes (20.7% [BATMAN 0–3] vs 38.3% [BATMAN 4–7] vs 47.8%[BATMAN 7–10], P < 0.001), functional independence (17.3% [BATMAN 0–3] vs 32.5% [BATMAN 4–7] vs 43.3% [BATMAN 7–10], P < 0.001), and mortality (57.2% [BATMAN 0–3] vs 39.9% [BATMAN 4–7] vs 31.1% [BATMAN 7–10], P < 0.001) among the three MT subgroups. Details are provided in Table II in the Online Resource. The results of the multivariable logistic regression analyses are shown in Table III in the Online Resource.
Of the patients included, the onset to treatment time (OTT) was within 6 h in 586 (70.8%) patients, 6–12 h in 189 (22.8%) patients, and > 12 h in 53 (6.4%) patients. MT and favorable outcomes were associated when the OTT was within 6 h (10.3 vs 33.9%, P < 0.001) and 6–12 h (4.5 vs 22.1%, P = 0.007), but no significant differences were found when the OPT was > 12 h (16.7 vs 43.9%, P = 0.105). MT remained associated with favorable outcomes in 57 (6.9%) patients with wake-up stroke (0% vs 28.6%, P = 0.024). In patients with OTT > 12 h, the correlation between the BATMAN score and favorable outcomes was not significant (P = 0.307), but patients with high BATMAN score tended to have favorable outcomes when the OPT was > 12 h (P = 0.045).
The relationship between the time metrics and favorable functional outcomes is shown in Fig. 3A, B. Figure 3A shows a decline in favorable outcomes with an increase in OPT. However, after adjusting for confounding factors, OPT was not associated with favorable outcomes (P = 0.216). Shorter PRT was associated with an increased probability of favorable outcomes, and the logistic regression results were statistically significant (P < 0.001). The effects of the BATMAN score and time metrics on the probability of favorable outcomes are shown in Fig. 3C, D. There were no interactions between the BATMAN score, OPT (P = 0.131), and PRT (P = 0.895). For patients with a given BATMAN score, the change in OPT had little impact on favorable outcomes (Fig. 3C). However, the probability of a favorable outcome was approximately greater in patients with shorter PRT and higher BATMAN scores (Fig. 3D).
Impact of the time metrics and the Basilar Artery on Computed Tomography Angiography (BATMAN) score on favorable outcomes in patients who have undergone mechanical thrombectomy (MT). The curves show the decrease in the probability of favorable outcomes with increases in the onset to puncture time (A) and puncture to recanalization time (B). C Associations between the onset to puncture time and the BATMAN score and the probability of favorable outcomes in patients who have undergone MT. For patients with a given BATMAN score, the change in time had minimal impact on favorable outcomes (R2 = 0.991). D Associations between the puncture to recanalization time and BATMAN score and the probability of favorable outcomes in patients with MT. The probability of favorable outcomes was greater in patients with shorter puncture to recanalization and higher BATMAN scores (R2 = 0.966)
Discussion
To our knowledge, this multicenter cohort study is the first to evaluate the safety and efficacy of MT in patients with different BATMAN scores. This study also used the largest sample yet to assess the relationship between the BATMAN score and prognosis. Our study demonstrated that the baseline BATMAN score is a strong predictor of prognosis in patients with acute BAO who have or have not undergone MT.
Patients with good BATMAN scores had good outcomes after MT. Patients undergoing MT had lower mortality than those receiving SMT in the poor (89.4 vs 57.2%, P < 0.001) and moderate (67.9 vs 39.9%, P < 0.001) BATMAN score subgroups. However, this difference was not significant (47.4 vs 31.3%, P = 0.102) for the good subgroup. This is probably because patients with high BATMAN scores have a lower risk of death because of better collateral circulation, lower thrombotic burden, and lower NIHSS score (P < 0.001). In the poor and moderate subgroup, the probability of SICH was higher in the MT group than in the SMT group. SICH was correlated with a worse prognosis [16, 17], but the overall benefit of patients undergoing MT outweighed this partial risk.
The BATMAN score was first proposed by Alemseged et al., and the best cutoff value was 7; patients with a poor BATMAN score < 7 were considered unlikely to have good outcomes even with successful recanalization [10]. Yang et al. considered a BATMAN score > 3 as an independent predictor of favorable outcomes in patients who had undergone MT [11]. In our analysis, we found that MT was still beneficial to patients in the poor (0–3) and moderate (4–6) BATMAN score subgroups. This may be attributed to the larger sample of our study than in the two studies.
Collateral circulation status is predictive of the prognosis of patients with BAO [8, 9, 18,19,20]. Good collateral circulation can reduce the infarct volume of patients [21], prolong the time window [8,9,10,11,12,13,14,15,16,17,18,19,20,21,22], and facilitate more benefits of MT. Ischemia is always a function of time and cerebral hypoperfusion, which largely depends on the collateral status [18]. The PCoA probably provides the most important collateral circulation. Previous studies have confirmed that the presence of PCoA and its diameter are important prognostic factors [9, 10, 20]. When PCoA is present, blood flow from the internal carotid artery fills the PCAs or the distal segment of the basilar artery, maintaining patency of the branches of the posterior cerebral arteries and superior cerebellar arteries [10,11,12,13,14,15,16,17]. The thrombotic burden is also a predictor of clinical outcomes. Legrand et al. found that a lower thrombotic burden was associated with a 24-h recanalization and a 3-month outcome after intravenous thrombolysis [23]. For the basilar artery, increased thrombus length is also related to poor outcomes [24]. Longer thrombus in BAO is associated with increased blockage of perforating arteries and larger areas of ischemia in the brainstem. The brainstem lesions cannot be recovered even after revascularization, because there are artery anastomoses between the superficial brainstem arteries and not between the internal brainstem arteries [17, 24].
We found that the probability of a favorable outcome decreased with an increase in the OPT increased (Fig. 3A); however, multivariable analysis showed that OPT was not associated with favorable outcomes (P = 0.216). This suggests that the BATMAN score may be a more critical factor influencing the benefit of MT over OPT. In the anterior circulation, some studies [25, 26] have demonstrated the superiority of MT for carefully selected patients with effective time windows and a shift from the time window to the tissue window [27]. Several studies have found that OPT does not predict clinical outcomes in patients undergoing MT in the posterior circulation [18, 24, 28]. This may be due to the developed collateral network, reverse filling of the distal basilar artery, and plasma flow siding of the clot [17]. Nevertheless, we still need to achieve recanalization as soon as possible to prevent further thrombus growth from blocking the perforating arteries, especially when patients have lower BATMAN scores [22].
Our findings demonstrate that longer procedures were associated with a lower likelihood of a good prognosis. For every 10 min of prolongation, the likelihood of a good prognosis decreased by 7% (adjusted OR, 0.93; 95% CI, 0.89–0.96; P < 0.001). Some recent studies have shown that the prolongation of procedures decreased the rate of favorable outcomes and increased the rates of complications and SICH [29,30,31]. Spiotta and colleagues proposed a procedural duration of < 60 min and careful assessment before continuing a procedure lasting more than 60 min [29, 31]. However, procedural duration is affected by several factors, including etiology of stroke, lesion location, tortuosity of vessels, and interventionalist experience [32], it may depend on the situation of each patient [33].
Limitations
Our study had several limitations. First, it was an observational study, and certain biases were inevitable. However, we conducted a training for each center before the study started and our prospective data were collected from multiple centers to reduce the risk of bias. Second, the imaging data were obtained with different CTA equipment using different parameters, but we evaluated the imaging data in an independent core imaging laboratory, and three investigators who were blinded to the clinical outcomes independently assessed the CTA images.
Conclusion
In summary, a higher BATMAN score was associated with better prognoses and lower mortality rates after 3 months, and MT was associated with improved outcomes in patients with low BATMAN scores despite the worse overall outcomes. Furthermore, a shorter procedural duration was associated with a better prognosis. Our findings will require further validation.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Code availability
Not applicable.
References
Goyal M, Menon BK, van Zwam WH, Dippel DWJ, Mitchell PJ, Demchuk AM, Dávalos A, Majoie CBLM, van der Lugt A, de Miquel MA, Donnan GA, Roos YBWEM, Bonafe A, Jahan R, Diener H-C, van den Berg LA, Levy EI, Berkhemer OA, Pereira VM, Rempel J, Millán M, Davis SM, Roy D, Thornton J, Román LS, Ribó M, Beumer D, Stouch B, Brown S, Campbell BCV, van Oostenbrugge RJ, Saver JL, Hill MD, Jovin TG (2016) Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. The Lancet 387:1723–1731. https://doi.org/10.1016/s0140-6736(16)00163-x
Mattle HP, Arnold M, Lindsberg PJ, Schonewille WJ, Schroth G (2011) Basilar artery occlusion. The Lancet Neurol 10:1002–1014. https://doi.org/10.1016/s1474-4422(11)70229-0
Schonewille WJ, Wijman CAC, Michel P, Rueckert CM, Weimar C, Mattle HP, Engelter ST, Tanne D, Muir KW, Molina CA, Thijs V, Audebert H, Pfefferkorn T, Szabo K, Lindsberg PJ, de Freitas G, Kappelle LJ, Algra A (2009) Treatment and outcomes of acute basilar artery occlusion in the Basilar Artery International Cooperation Study (BASICS): a prospective registry study. The Lancet Neurol 8:724–730. https://doi.org/10.1016/s1474-4422(09)70173-5
Liu X, Dai Q, Ye R et al (2020) Endovascular treatment versus standard medical treatment for vertebrobasilar artery occlusion (BEST): an open-label, randomised controlled trial. The Lancet Neurology 19:115–122. https://doi.org/10.1016/s1474-4422(19)30395-3
Langezaal LCM, van der Hoeven E, Mont’Alverne FJA et al (2021) Endovascular therapy for stroke due to basilar-artery occlusion. N Engl J Med 384:1910–1920. https://doi.org/10.1056/NEJMoa2030297
Singer OC, Berkefeld J, Nolte CH et al (2015) Mechanical recanalization in basilar artery occlusion: the ENDOSTROKE study. Ann Neurol 77:415–424. https://doi.org/10.1002/ana.24336
Higashida RT, Furlan AJ, Roberts H, Tomsick T, Connors B, Barr J, Dillon W, Warach S, Broderick J, Tilley B, Sacks D (2003) Trial design and reporting standards for intra-arterial cerebral thrombolysis for acute ischemic stroke. Stroke 34:e109-137. https://doi.org/10.1161/01.Str.0000082721.62796.09
Kim BM, Baek JH, Heo JH, Nam HS, Kim YD, Yoo J, Kim DJ, Jeon P, Baik SK, Suh SH, Lee KY, Kwak HS, Roh HG, Lee YJ, Kim SH, Ryu CW, Ihn YK, Kim B, Jeon HJ, Kim JW, Byun JS, Suh S, Park JJ, Lee WJ, Roh J, Shin BS, Bang OY (2018) Collateral status affects the onset-to-reperfusion time window for good outcome. J Neurol Neurosurg Psychiatry 89:903–909. https://doi.org/10.1136/jnnp-2017-317627
van der Hoeven EJ, McVerry F, Vos JA, Algra A, Puetz V, Kappelle LJ, Schonewille WJ, Investigators Br (2016) Collateral flow predicts outcome after basilar artery occlusion: the posterior circulation collateral score. Int J Stroke 11:768–775. https://doi.org/10.1177/1747493016641951
Alemseged F, Shah DG, Diomedi M, Sallustio F, Bivard A, Sharma G, Mitchell PJ, Dowling RJ, Bush S, Yan B, Caltagirone C, Floris R, Parsons MW, Levi CR, Davis SM, Campbell BC (2017) The basilar artery on computed tomography angiography prognostic score for basilar artery occlusion. Stroke 48:631–637. https://doi.org/10.1161/STROKEAHA.116.015492
Yang H, Ma N, Liu L, Gao F, Mo D, Miao Z (2018) The basilar artery on computed tomography angiography score for acute basilar artery occlusion treated with mechanical thrombectomy. J Stroke Cerebrovasc Dis 27:1570–1574. https://doi.org/10.1016/j.jstrokecerebrovasdis.2018.01.007
Rentzos A, Karlsson JE, Lundqvist C, Rosengren L, Hellstrom M, Wikholm G (2018) Endovascular treatment of acute ischemic stroke in the posterior circulation. Interv Neuroradiol 24:405–411. https://doi.org/10.1177/1591019918762320
Zi W, Qiu Z, Wu D et al (2020) Assessment of endovascular treatment for acute basilar artery occlusion via a nationwide prospective registry. JAMA Neurol 77:561–573. https://doi.org/10.1001/jamaneurol.2020.0156
Powers WJ, Derdeyn CP, Biller J, Coffey CS, Hoh BL, Jauch EC, Johnston KC, Johnston SC, Khalessi AA, Kidwell CS, Meschia JF, Ovbiagele B, Yavagal DR, American Heart Association Stroke C (2015) 2015 American Heart Association/American Stroke Association focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: a guideline for healthcare professionals From the American Heart Association/American Stroke Association. Stroke 46:3020–3035. https://doi.org/10.1161/STR.0000000000000074
von Kummer R, Broderick JP, Campbell BC, Demchuk A, Goyal M, Hill MD, Treurniet KM, Majoie CB, Marquering HA, Mazya MV, San Roman L, Saver JL, Strbian D, Whiteley W, Hacke W (2015) The Heidelberg bleeding classification: classification of bleeding events after ischemic stroke and reperfusion therapy. Stroke 46:2981–2986. https://doi.org/10.1161/STROKEAHA.115.010049
Montalvo M, Mistry E, Chang AD et al (2019) Predicting symptomatic intracranial haemorrhage after mechanical thrombectomy: the TAG score. J Neurol Neurosurg Psychiatry 90:1370–1374. https://doi.org/10.1136/jnnp-2019-321184
Lindsberg PJ, Pekkola J, Strbian D, Sairanen T, Mattle HP, Schroth G (2015) Time window for recanalization in basilar artery occlusion: speculative synthesis. Neurology 85:1806–1815. https://doi.org/10.1212/wnl.0000000000002129
Kwak HS, Park JS (2020) Mechanical thrombectomy in basilar artery occlusion: clinical outcomes related to posterior circulation collateral score. Stroke 51:2045–2050. https://doi.org/10.1161/strokeaha.120.029861
Antunes Dias F, Castro-Afonso LH, ZanonZotin MC, Alessio-Alves FF, Martins Filho R, Camilo MR, Nakiri GS, Abud DG, Pontes-Neto OM (2019) Collateral scores and outcomes after endovascular treatment for basilar artery occlusion. Cerebrovasc Dis 47:285–290. https://doi.org/10.1159/000502083
Goyal N, Tsivgoulis G, Nickele C, Doss VT, Hoit D, Alexandrov AV, Arthur A, Elijovich L (2016) Posterior circulation CT angiography collaterals predict outcome of endovascular acute ischemic stroke therapy for basilar artery occlusion. J Neurointerv Surg 8:783–786. https://doi.org/10.1136/neurintsurg-2015-011883
Christensen S, Mlynash M, Kemp S, Yennu A, Heit JJ, Marks MP, Lansberg MG, Albers GW (2019) Persistent target mismatch profile >24 hours after stroke onset in DEFUSE 3. Stroke 50:754–757. https://doi.org/10.1161/strokeaha.118.023392
Alemseged F, Van der Hoeven E, Di Giuliano F et al (2019) Response to late-window endovascular revascularization is associated with collateral status in basilar artery occlusion. Stroke. https://doi.org/10.1161/STROKEAHA.118.023361
Legrand L, Naggara O, Turc G, Mellerio C, Roca P, Calvet D, Labeyrie MA, Baron JC, Mas JL, Meder JF, Touze E, Oppenheim C (2013) Clot burden score on admission T2*-MRI predicts recanalization in acute stroke. Stroke 44:1878–1884. https://doi.org/10.1161/STROKEAHA.113.001026
Gilberti N, Gamba M, Premi E, Costa A, Vergani V, Delrio I, Spezi R, Mardighian D, Frigerio M, Gasparotti R, Padovani A, Magoni M (2016) Endovascular mechanical thrombectomy in basilar artery occlusion: variables affecting recanalization and outcome. J Neurol 263:707–713. https://doi.org/10.1007/s00415-016-8047-x
Jovin TG, Saver JL, Ribo M et al (2017) Diffusion-weighted imaging or computerized tomography perfusion assessment with clinical mismatch in the triage of wake up and late presenting strokes undergoing neurointervention with Trevo (DAWN) trial methods. Int J Stroke 12:641–652. https://doi.org/10.1177/1747493017710341
Albers GW, Lansberg MG, Kemp S, Tsai JP, Lavori P, Christensen S, Mlynash M, Kim S, Hamilton S, Yeatts SD, Palesch Y, Bammer R, Broderick J, Marks MP (2017) A multicenter randomized controlled trial of endovascular therapy following imaging evaluation for ischemic stroke (DEFUSE 3). Int J Stroke 12:896–905. https://doi.org/10.1177/1747493017701147
Desai SM, Haussen DC, Aghaebrahim A, Al-Bayati AR, Santos R, Nogueira RG, Jovin TG, Jadhav AP (2018) Thrombectomy 24 hours after stroke: beyond DAWN. J Neurointerv Surg 10:1039–1042. https://doi.org/10.1136/neurintsurg-2018-013923
Bouslama M, Haussen DC, Aghaebrahim A, Grossberg JA, Walker G, Rangaraju S, Horev A, Frankel MR, Nogueira RG, Jovin TG, Jadhav AP (2017) Predictors of good outcome after endovascular therapy for vertebrobasilar occlusion stroke. Stroke 48:3252–3257. https://doi.org/10.1161/STROKEAHA.117.018270
Spiotta AM, Vargas J, Turner R, Chaudry MI, Battenhouse H, Turk AS (2014) The golden hour of stroke intervention: effect of thrombectomy procedural time in acute ischemic stroke on outcome. J Neurointerv Surg 6:511–516. https://doi.org/10.1136/neurintsurg-2013-010726
Hassan AE, Shariff U, Saver JL, Goyal M, Liebeskind D, Jahan R, Qureshi AI (2019) Impact of procedural time on clinical and angiographic outcomes in patients with acute ischemic stroke receiving endovascular treatment. J Neurointerv Surg 11:984–988. https://doi.org/10.1136/neurintsurg-2018-014576
Alawieh A, Vargas J, Fargen KM, Langley EF, Starke RM, De Leacy R, Chatterjee R, Rai A, Dumont T, Kan P, McCarthy D, Nascimento FA, Singh J, Vilella L, Turk A, Spiotta AM (2019) Impact of procedure time on outcomes of thrombectomy for stroke. J Am Coll Cardiol 73:879–890. https://doi.org/10.1016/j.jacc.2018.11.052
Gupta R, Horev A, Nguyen T et al (2013) Higher volume endovascular stroke centers have faster times to treatment, higher reperfusion rates and higher rates of good clinical outcomes. J Neurointerv Surg 5:294–297. https://doi.org/10.1136/neurintsurg-2011-010245
Sang H, Li F, Yuan J et al (2021) Values of Baseline posterior circulation acute stroke prognosis early computed tomography score for treatment decision of acute basilar artery occlusion. Stroke 52:811–820. https://doi.org/10.1161/strokeaha.120.031371
Acknowledgements
We would like to thank Editage (www.editage.cn) for English language editing.
Funding
This study was funded by the National Natural Science Foundation of China (no. 82071323), Chongqing Natural Science Foundation (no. cstc2020jcyj-msxmX0926), Chongqing Science and Health Joint Project (no. 2019ZDXM002), the Army Medical University Clinical Medical Research Talent Training Program (nos. 2018XLC3039, 2019XLC2008, and 2019XLC3016), and Medical and Health Planning Project of Xiamen (no. 3502z20209036).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethical approval
Approval was obtained from the ethics committee of the participating centers. The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Consent to participate
Informed consent was obtained from all individual participants included in the study or their legally authorized representatives.
Consent to publication
All included patients gave their consent for publication of the collected data.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Song, K., Li, F., Shi, M. et al. Basilar artery on computed tomography angiography score and clinical outcomes in acute basilar artery occlusion. J Neurol 269, 3810–3820 (2022). https://doi.org/10.1007/s00415-022-11013-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-022-11013-1