Abstract
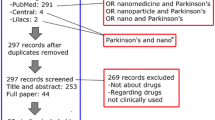
Although effective symptomatic treatments for Parkinson’s disease (PD) have been available for some time, efficient and well-controlled drug delivery to the brain has proven to be challenging. The emergence of nanotechnology has created new opportunities not only for improving the pharmacokinetics of conventional therapies but also for developing novel treatment approaches and disease modifying therapies. Several exciting strategies including drug carrier nanoparticles targeting specific intracellular pathways and structural reconformation of tangled proteins as well as introducing reprogramming genes have already shown promise and are likely to deliver more tailored approaches to the treatment of PD in the future. This paper reviews the role of nanoparticles in PD including a discussion of both their composition and functional capacity as well as their potential to deliver better therapeutic agents.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Current treatment strategies for Parkinson’s disease (PD) largely focus on relieving motor symptoms by increasing dopamine levels within the central nervous system (CNS) or by stimulating dopamine receptors. The most effective treatment is levodopa but its benefits are impacted by unpredictable absorption and extensive peripheral metabolism, leading to motor fluctuations [1].
Nanotechnology-based drug-delivery systems provide a promising avenue to overcome the pharmacokinetic limitations of conventional therapies, but also provide distinct benefits by virtue of their small size (1–100 nm). Nanoparticles can act as drug-delivery vehicles with the potential to directly manipulate biological targets (e.g. DNA, RNA, proteins) [2]. In particular, they can protect drug from degradation, provide sustained release, facilitate entry into the CNS and also deliver drug to specific cells to target particular intracellular pathways [3, 4].
In this review, we will focus on nanoparticles that may impact on future PD therapies. We will first describe the composition and structure of the various subtypes of nanoparticles that have been developed for PD, highlighting polymer-based, lipid-based and inorganic agents. We will then outline how nanoparticles may be applied in the future treatment of PD from a functional perspective.
Nanoparticle composition
Nanoparticles are classically divided by their structural composition. The advantages and disadvantages of each type are described in Table 1.
Polymeric nanoparticles
Polymeric nanoparticles can be composed of synthetic or naturally occurring polymers and are organised into a variety of structures, which have been shown to be biocompatible, biodegradable, and non-toxic [5]. The two most basic types are nanocapsules, where the drug is encapsulated in a polymeric vesicle, and nanospheres, where the drug is entrapped in a matrix of polymer or adsorbed onto its surface (Fig. 1). In either case, the drug is released as the polymer is degraded allowing flexibility in the rate of delivery, which can range from weeks to months [6].
More sophisticated polymeric structures exist in the form of polymeric micelles and dendrites (Fig. 1). Polymeric micelles are formed by amphiphilic polymers that self-assemble typically into a sphere with a hydrophobic core and hydrophilic shell [7]. They are particularly beneficial for encapsulating hydrophobic drugs. Dendrimers, on the other hand, are highly branched macromolecules formed by radially branched polymers in repeating units called ‘generations.’ Due to their well-defined chemical structure, they are uniform in size and can be very small (< 20 nm) [8]. Multiple binding sites on the terminal branches of these dendrimers provide additional functions and it has been shown that they can prevent ⍺-synuclein fibrillation and potentially remove fibrils in vitro [9,10,11].
The most common FDA-approved polymers to prepare nanoparticles are poly(lactic-co-glycolic acid) (PLGA), polylactic acid (PLA) and polyethylene glycol (PEG). Of the clinically approved nanoparticles, PEG is the most widely used polymer as it is used to coat nanoparticles as well as to stabilise proteins in more conventional therapies [12]. The earliest example of pegylation was used in Adagen® in 1990, which is PEG-adenosine deaminase for the treatment of severe combined immunodeficiency disease. Furthermore, Eligard®, a PLGA-encapsulated leuprorelin (a testosterone inhibiting drug), is commonly used for the controlled release of hormone therapy for the treatment of prostate cancer, allowing for subcutaneous injection every six months [13]. Unfortunately, there are few other examples of polymeric nanoparticles in clinical use with the majority of current trials being conducted in cancer therapies [14]. Despite the proof of concept in these clinical trials, polymeric nanoparticles have not progressed beyond preclinical studies in Parkinson’s disease.
Lipid-based nanoparticles
Lipid-based nanoparticles are biocompatible and due to their lipid nature and size can penetrate the CNS without any modification [15]. They may circumvent first-pass metabolism when absorbed via the lymphatic system [16]. Lipid vesicles made from a single layer of phospholipids (micelles) or a bilayer (liposomes) can encapsulate drugs and provide sustained protection from degradation in the circulation (Fig. 2) [17]. Endogenous extracellular vesicles (exosomes) naturally composed of phospholipid bilayers have been harvested and loaded with PD drugs with lower immunogenicity utilising natural cell-specific targeting mechanisms [18,19,20]. Other lipid-based nanostructures can also be made of solid lipid, liquid lipid (Nanoemulsions) or a mixture of the two (Nanostructured Lipid Carriers) [21,22,23,24]. These are shown in Fig. 2, with advantages and disadvantages listed in Table 1.
Liposomes comprise the majority of clinically available nanoparticles [14] with over 20 years of clinical use including agents such as liposomal amphotericin (AmBisome®) and doxorubicin (Doxil® or Caelyx®). Liposomal amphotericin improves the half-life of the drug as well as reducing nephrotoxicity by preventing the active drug from interacting with the renal distal tubules [25]. Liposomal doxorubicin, whilst improving the pharmacokinetic profile of doxorubicin, also reduces cardiotoxicity, myelosuppression and nausea and vomiting. This is because the liposome favours distribution away from sites that have tight capillary junctions, such as the heart and gastrointestinal tract, and into areas with fenestrated capillaries such as sites of inflammation or tumour growth [26]. Newer liposomal drugs are available, but there is limited clinical availability of the other types of lipid nanoparticles. Drug-loaded exosomes have made it has far as completing phase II studies in cancer therapeutics [27]. Despite the emerging clinical use of exosomes and the wide clinical usage of liposomes, research into lipid-based nanoparticles for PD is currently limited to preclinical studies.
Inorganic nanoparticles
Inorganic nanoparticles have attracted considerable attention as drug-delivery systems, as well as potential disease modifiers [28]. Current developments have evaluated gold [29], magnetic iron oxide [30], as well as the synthetic allotropes of carbon [31, 32], such as fullerene, graphene and carbon nanotubes for use in PD (Fig. 3). These structures are very small (< 25 nm) and have electrochemical properties that are size and shape dependent [33]. Importantly, some concerns have been raised about the use of carbon nanotubes due to some asbestos-like toxicity whereby they can induce the secretion of proinflammatory cytokines such as IL-1β from macrophages [34].
Iron oxide nanoparticles are the most widely FDA-approved inorganic nanoparticles, with examples such as iron carboxymaltose (Ferrinject®) for anaemia and others being used as imaging agents [14]. However, gold nanoparticles are emerging with Phase II clinical trials underway for multiple sclerosis, amyotrophic lateral sclerosis, and Parkinson’s disease, which will be discussed below [35,36,37].
Application to Parkinson’s Disease
To date, nanoparticles have been trialled around a number of different rationales including providing the sustained release of conventional PD therapies, evading the immune system and facilitating entry into the CNS [4]. They have also been modified with functional elements to further enhance entry across mucosal surfaces, to target particular cell types (e.g. dopaminergic neurons) or to only release the active drug in particular circumstances, such as within acidic intracellular organelle compartments (e.g. lysosomes) (Fig. 4; Table 2) [38]. Therefore, potential benefits of nanotherapies extend beyond simply improving the pharmacokinetic properties of conventional treatments to the delivery of novel therapies that could target particular intracellular pathways (e.g. oxidative stress, inflammation) or even specific genes [39].
Sustained release
The earliest research into nanoparticles for PD involved improving the release profile of dopamine and then other dopaminergic medications, such as levodopa, dopamine agonists and monoamine oxidase B inhibitors. The first formulations involved stereotactically implanting dopamine-loaded liposomes directly into the striatum of a rat model of PD [40]. These liposomes released dopamine for 40 days with levels that remained elevated for 25 days following implantation. Similarly, formulations of levodopa have been able to achieve sustained levels via peripheral administration of liposomes [41, 42], as well as polymer-based nanoparticles [43,44,45,46,47]. A progression of studies resulted in a PLGA-PLA nanosphere being developed in 2012 that allowed for a once weekly administration of subcutaneous levodopa, resulting in elevated plasma dopamine levels that were sustained for 20 days in 6-OHDA lesioned rats. This approach not only improved bradykinesia but also ameliorated dyskinesias [43]. In an effort to avoid subcutaneous administration, more recent research has focused on intranasal formulations of levodopa-loaded PLGA nanoparticles, which appear to offer motor benefits that can persist for at least a week following administration [44]. In the last few years, studies have also demonstrated lower neuronal cytotoxicity from nanoparticles compared with free levodopa forming a stepping stone into first in human clinical studies [47].
Most of the recent research into extending the release of conventional PD therapies has been with polymeric nanoparticles rather than liposomes, which make up the majority of clinically approved nanoparticles in other diseases. Polymeric nanoparticles offering extended release have been successfully demonstrated in preclinical models with apomorphine [48, 49], bromocriptine [50], ropinirole [51], rotigotine [52,53,54] and selegeline [55]. Notably, one PLGA-based microsphere loaded with rotigotine has demonstrated stable plasma and striatal levels for 14 days, leading to reduced dyskinesias in 6-OHDA lesioned rats [54]. However, toxicity was not extensively investigated in any of these studies. Given that safety cannot be extrapolated from the composition of nanoparticles alone and thus the efficacy, safety, biodistribution and pharmacokinetics of each nanoparticle need to be evaluated more thoroughly prior to human studies [56].
Immunoevasion
Another important property of nanoparticles is the ability to manipulate their surface which allows them to avoid the immune system. Coating nanoparticles with polyethylene glycol (PEG) can bestow a ‘stealth property’, which prolongs peripheral circulation [14]. This is achieved by steric hindrance suppressing opsonisation, reducing activation of the complement system and hence reducing clearance [57]. This approach has been used to improve the circulation times of dopamine [58,59,60], apomorphine [48, 61, 62], and rotigotine [52, 63, 64] in rodent models of PD only. PEG is used as an adjunct with other nanoparticles such as liposomes or as components of polymeric micelles rather than directly conjugated to PD drugs. Pegylated formulations of conventional PD therapies might be destined to follow the same fate as pegylated insulin, whose development was ceased despite completion of Phase III studies. This was reportedly due to the financial burden of investigating potential hepatotoxicity, which outweighed the potential financial returns in the context of competition from alternative basal insulins [65]. This does not mean that pegylation is not a viable strategy, as evidenced by the numerous pegylated therapies available in other conditions, but financial incentives might favour research into disease modifying therapies in PD rather than adding to the numerous symptomatic treatments that are currently available.
Mucosal entry
Intranasal drug delivery has the potential of circumventing first-pass metabolism and facilitating quick entry into the brain via olfactory and trigeminal nerve pathways [66]. Nanoparticles can optimise intranasal delivery via the use of mucoadhesive polymers, such as chitosan or by conjugating nanoparticles with ligands capable of binding to the nasoepithelial surface, such as lectins.
Chitosan is commonly used as the core polymer in nanoparticles [45] or as a coating [67] because it can easily adhere to mucous membranes for the purpose of enhancing absorption across the nasoepithelium. Chitosan has the added benefit that it can disrupt cellular tight junctions, allowing easier entry across the blood–brain barrier [68]. So far, chitosan nanoparticles have been used for intranasal formulations of bromocriptine [50], levodopa [45], pramipexole [69], selegeline [69], rotigotine [53] and ropinirole [67]. In general, these studies reported faster and increased absorption across the mucosa due to chitosan, which translated to clinical and biochemical benefits in rodent models of PD.
Conjugating nanoparticles with ligands capable of binding to the nasoepithelium can also enhance nasal absorption and have been used to deliver anti-PD drugs intranasally. For example, conjugation of the peptide odorranalectin has been utilised because it preferentially binds to L-fucose, a sugar moiety found on the olfactory epithelium [70]. In one study, fluorescence labelling was able to show that odorranalectin conjugation increased the uptake of urocortin-containing nanoparticles in the brain (sustained and continued to increase over 8 h) compared to those without odorranalectin [71]. Another similar approach has been through the use of wheat germ agglutinin (WGA), which binds to N-acetyl-D-glucosamine and sialic acid, molecules that are both abundant in the nasal cavity [72]. Indeed work in MPTP-lesioned mice demonstrated that WGA-grafted levodopa nanoparticles can cause a rapid and sustained improvement in locomotor activity following nasal delivery [47].
Another method of improving intranasal drug absorption has been the incorporation of nanoparticles into thermosensitive gels, which improve the intranasal residence time of the drug due to increased viscosity and hence absorption. In one example, rotigotine, which is poorly water-soluble, was encapsulated in a polymeric micelle so that it could be dissolved into a water-based thermosensitive gel. Indeed, this method nearly doubled entry into the brain compared to intravenously administered rotigotine [63].
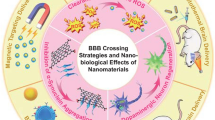
Blood–brain barrier entry
Clearly, one of the key obstacles in the treatment of PD lies with the blood–brain barrier (BBB), the tightly regulated interface between the CNS and the bloodstream. The BBB restricts passive transport to small and lipophilic drugs and almost no large molecules (> 1000 Daltons) and around 98% of all small molecules (< 500 Daltons) can get across it [73]. Furthermore, many molecules that are able to cross into the brain are quickly transported back to the bloodstream via efflux pumps [74]. Effective transport across the BBB may be facilitated by carriers (solute carriers), such as the large amino acid transporter (LAT1), receptor-mediated transport or adsorption-mediated transcytosis systems [75]. Importantly, nanoparticles can facilitate entry via each of these mechanisms.
Lipid-based vehicles can enter through the BBB unimpeded due to their small size and lipophilicity, as can some polymeric nanoparticles especially if they are under 100 nm. However, enhanced entry is usually achieved by functionalising the surface of nanoparticles with ligands known to target receptors on the BBB. For instance, lactoferrin (lf) is an iron-binding glycoprotein of the transferrin family reported to enhance transcytosis across the brain capillary endothelium through its interaction with lactoferrin-receptors, such as the low-density lipoprotein receptor-related protein (LRP) found on brain endothelial cells and neurons [76]. Lactoferrin-receptors appear to be increased in both dopaminergic neurons and respiratory epithelial cells [77, 78]. Thus, intranasally administered rotigotine-loaded nanoparticles conjugated with lactoferrin have shown increased concentration in the striatum over other areas in the brain such as the hippocampus [52, 64].
This approach has also been used to study a neuroprotective agent, urocortin, which is a corticotrophin-releasing factor-related peptide that has been shown to restore nigrostriatal function [79]. One study has demonstrated that urocortin-loaded Lf-conjugated PEG-PLGA nanoparticles were capable of increasing brain uptake by threefold, when compared to unconjugated nanoparticles [80]. Finally, it has also been demonstrated that lactoferrin conjugation can also improve the delivery of gene therapy to dopaminergic neurons, which are discussed in greater detail below [81].
An important synthetic peptide that is gaining clinical attention is angiopep, which is an efficient ligand to LRP and allows higher brain penetration than other brain-targeting peptides such as lactoferrin [82]. It has been used for the delivery of gene therapy to the CNS in preclinical studies of PD, but will be utilised in a Phase III study to delivery paclitaxel to brain or leptomeningeal metastases after successful open label Phase II study [83, 84].
Polysorbate-80 (PS80) is a surfactant that is well known for facilitating entry into the blood–brain barrier [85]. It is thought to act as an anchor for various lipoproteins that become attached to it in the circulation by adsorption. These lipoproteins, such as apolipoprotein B and/or E, then facilitate entry into the brain by receptor-mediated endocytosis. As an example, PS80-coated chitosan nanoparticles have been used to enhance the entry of ropinirole, which typically crosses the BBB poorly due to its hydrophilicity [51]. These PS80-coated nanoparticles exhibited higher concentrations in the brain and less accumulation in other organs, such as the liver, spleen, and kidney compared with uncoated nanoparticles. This suggests that PS80-coated nanoparticles not only improved CNS entry across the BBB but also reduced opsonisation by the mononuclear phagocytic system, allowing more effective drug delivery.
Another novel method of facilitating entry into the CNS has been by combining nanoparticles with MRI-guided focused ultrasound [86]. Nanoparticles can be complexed to microbubbles that when exposed to ultrasound are believed to exert a radial force on capillaries, leading to local openings of the blood–brain barrier. This approach has been used in two recent studies to deliver gene therapy encapsulated in liposomes specifically to striatal neurons [87, 88]. This will be discussed in greater detail in the section on gene therapy.
Cell-targeting
The conjugation of specific ligands on nanoparticles can be used to promote selective uptake into dopaminergic neurons. Indeed, the Rabies Virus Glycoprotein (RVG29) is thought to facilitate internalisation into neurons by specifically binding to the nicotinic acetylcholine receptor (nAchR), which is found on dopaminergic neurons, as well as the extracellular surface of the brain’s microvascular endothelial cells. Using this approach, studies have demonstrated that RVG29 can be conjugated with liposomes to deliver a dopamine derivative to the substantia nigra and striatum in PD rodents with a higher specificity than other neurons and in greater concentrations than was achieved with non-conjugated liposomes [60]. This technique of conjugating nanoparticles with ligands capable of being internalised within specific neurons offers advantages when looking to target pathogenic intracellular processes (see below).
There are currently no clinically approved targeted nanoparticles available for any diseases. There are phase II studies for cancer therapies, with one active phase II trial exploring anti-EGFR-immunoliposomes loaded with doxorubicin in patients with advanced triple negative EGFR positive breast cancer [89]. These immunoliposomes are constructed by covalently linking liposomes to Fab fragments of the monoclonal antibody cetuximab, which recognises the EGFR molecule on the tumour [90]. Clinical trials utilising targeted ligands have fallen short due to off-target toxicity, increased clearance by the increased immunological recognition of surface ligands, and because of the difficulties associated with upscaling product manufacture [91].
Triggered release
To combat off-target toxicity and adverse effects, nanoparticles can be modified to release drug in selective environments, such as inside intracellular organelles. This approach has been explored with apomorphine loaded into polymeric nanoparticles modified with phenylboronic acid. The boronate ester undergoes dynamic changes in acidic environments, so that the drug is protected from release in the circulation but is rapidly released when taken into the acidic environment of the endolysosomes within neurons [48]. This has been studied in animal models of PD, but not in human studies. A triggered release nanoparticle ThermoDox®, which is a thermosensitive liposome that releases doxorubicin in response to temperatures at 40 °C, is currently in a phase III study for the treatment of hepatocellular carcinoma in combination with radiofrequency ablation, which provides the external heat required for activation [91, 92].
Pathological targets
Anti-aggregation
Drugs that prevent ⍺-synuclein misfolding and/or aggregation have been an appealing approach to disease modification [93]. For example, epigallocatechin gallate (EGCG) has demonstrated good in vitro evidence for the inhibition of ⍺-synuclein aggregation but unfortunately failed in clinical trials of patients with Multiple System Atrophy due to a lack of efficacy and significant hepatoxicity [94]. Notwithstanding the in vivo evidence of anti-Parkinson’s effect in rodent models, it has been suggested that some of the limitations of EGCG included difficulties crossing the blood–brain barrier and poor internalisation into dopaminergic neurons [95]. In order to combat these issues, EGCG has been incorporated in multi-functional lipid micelles that facilitate receptor-mediated transcytosis across the BBB (using B6, a peptide with high affinity for the transferrin receptor), as well as ligands that target entry into dopaminergic neurons via the dopamine transporter (using mazindol, a drug that binds to the dopamine transporter DAT and promotes its internalisation) [96]. EGCG was grafted onto the surface of these nanoparticles utilising the reversible boronate ester bond that was discussed in the previous section, allowing for the release of EGCG only after the nanoparticle had been taken into the acidic environment of the endolysosomes within dopaminergic neurons. In the same study, these nanoparticles were labelled with superparamagnetic iron oxide nanocubes, which traced accumulation via magnetic resonance imaging. Results showed not only favourable pharmacokinetics compared to free EGCG but also increased accumulation, specifically within the substantia nigra, which correlated with improvements in both behavioural and biochemical markers of dopaminergic neuronal loss in these murine models of PD.
Other examples of anti-⍺-synuclein aggregation are reasonably diverse but aggregates of several to hundreds of gold atoms called ‘gold nanoclusters’ have been reported to inhibit ⍺-synuclein fibrillation, reverse dopaminergic neuronal loss and improve motor behaviour in MPTP-induced mice [97], whilst melatonin-loaded polymeric nanoparticles made from dopamine polymers (polydopamine) have demonstrated a cytoprotective effect and suppress ⍺-synuclein phosphorylation in vitro [98]. Furthermore, dendrimers as a class of nanoparticles are thought to possess anti-fibrillation properties per se due to their highly branched structure, which has been supported using some in vitro models of PD [9, 10].
Oxidative stress
There is active research into the pathophysiological pathways in PD, including drugs that target mitochondrial dysfunction, oxidative stress and inflammation. Although there may be good in vitro evidence with some of these drugs, many of them have failed to demonstrate disease modification in clinical studies [99]. However, it is possible that some of these studies have been limited by the pharmacokinetic properties of these drugs and there may be an opportunity to re-evaluate their benefit if they were combined with nanoparticles to circumvent these issues [100]. Indeed, recent examples of antioxidants that have demonstrated motor improvements in rodent models of PD when delivered via nanoparticles have included coenzyme Q10 [101], curcumin [102], acteoside [103] and puerarin [104, 105].
Gold nanoparticles have been proposed as a means for protecting dopaminergic neurons against oxidative stress. Recent studies investigating the preclinical efficacy of the gold nanoparticle CNM-Au8 have reported the enhanced survival of dopaminergic neurons when subjected to MPP + and 6-OHDA lesions, as well as improvements in paw placement in 6-OHDA-lesioned rats [106]. These findings have prompted clinical trials of CNM-Au8, such as the REPAIR-PD study, a Phase II single-centre, open label pilot assessing this therapy in PD patients within three years of diagnosis [35]. The study proposes that these orally administered gold nanoparticles will act as redox catalysts, increasing the production of ATP and offering protection against oxidative stress. The primary endpoint of this short clinical intervention will utilise magnetic resonance spectroscopy (31P-MRS) to evaluate the ratio of oxidised to reduced nicotinamide adenine dinucleotide (NAD + /NADH) with a lower ratio indicating increased oxidative stress.
Intracellular iron
Excess intracellular iron is a common characteristic in PD patients and is thought to be a precipitating factor in the development of the disease, possibly through oxidative stress and consequent necrosis [107]. This insight has prompted a number of clinical trials, some of which have shown a trend towards motor benefits using iron chelators [108]. However, the most effective iron chelator, deferoxamine (or desferrioxamine) (DFO) has a short half with low bioavailability as it is hydrophilic with poor penetrance of the BBB. To overcome this, DFO has been encapsulated within a PEG-PLGA polymeric micelle, coated with RVG29 to facilitate entry across the BBB and promote internalisation within dopaminergic neurons. Early results in MPTP-induced mice have demonstrated a reduction in striatal iron, a reduction in ⍺-synuclein levels, a reversal of dopaminergic neuronal loss and an improvement in motor deficits [109].
Gene therapy
Gene therapy involves transferring nucleic acid-based therapeutic agents such as plasmid DNA, short interfering RNA (siRNA), microRNA or RNA into cells to repair, replace or regulate genes. In PD, gene therapy has been investigated to promote the expression of neuroprotective genes, such as glial cell line-derived neurotrophic factor (GDNF) [81, 82, 87, 88] or to downregulate the expression of ⍺-synuclein [30, 110, 111]. Conventional viral vectors have faced challenges including some safety concerns, poor gene loading efficiency and immunogenicity with repeated administration. However, the biggest hurdle is that they require invasive intracranial administration due poor BBB penetration [112].
Nanoparticles can improve passage through the BBB via different methods, potentially allowing for the peripheral administration of gene therapy. Surface-modified dendrimers have been shown to improve penetration into the CNS by about fourfold compared with non-modified nanoparticles [81]. Peripheral intravenous administration of lactoferrin-modified dendrimers improved delivery of GDNF to the CNS over transferrin-modified and unmodified nanoparticles in PD rats. This resulted in improved locomotor activity, reduced dopaminergic neuronal loss and enhanced monoamine neurotransmitter levels [81]. The same group utilised a synthetic peptide called angiopep conjugated to a poly-L-lysine dendrimer to successfully deliver GDNF intravenously to the CNS of PD-induced rats resulting in improved locomotor activity and reduced dopaminergic neuronal loss [82]. A Phase III clinical trial is due to commence in 2021 studying the delivery of paclitaxel to brain and leptomeningeal metastases of brain cancer using angiopep-2 to target the CNS [84].
Another technique has been to combine nanoparticles with MRI-guided focused ultrasound (FUS) to achieve local disruption of the CNS. Intravenous administration of liposomes carrying GDNF has been shown improve penetration by fivefold when combined with FUS [87]. The combination of FUS with microbubbles complexed to liposomes carrying GDNF significantly improved behaviour of MPTP-induced mice and reduced dopaminergic neuronal loss when compared with liposomal delivery alone. In fact, liposomal delivery alone did not significantly improve behaviour over MPTP-induced controls [87]. Similar results were found when pegylated liposomes complexed with microbubbles were delivered intravenously to 6-OHDA lesioned rats. The combination increases the DNA-carrying capacity as well as BBB penetration, which would otherwise be traded off as increasing the size of the nanoparticle would reduce BBB penetration [88].
Inorganic nanoparticles present an alternative strategy to improve the loading efficiency of viral vectors due to their high surface area-to-volume ratio, and ability to be functionalised to target specific brain tissue [30, 110]. Examples have included gold nanoparticles and magnetic iron oxide nanoparticles, which both have been used to deploy plasmid DNA inhibiting SNCA to neurons with the aid of conjugating Nerve Growth Factor (NGF), which promotes neuronal uptake. In the study using magnetic iron oxide, nanoparticles also utilised a pH-sensitive and thermoresponsive polymer (N-isopropylacrylamide) to favour intracellular over extracellular release of the DNA [30]. This resulted in reduced ⍺-synuclein expression, dopaminergic neuronal loss and improvements in behaviour in MPTP-induced mice. Gold nanoparticles with chitosan coating and NGF showed biochemical and histological improvements with no obvious toxicity [110]. Further studies and modifications are required to establish safety and improve efficacy, but these studies serve as starting point for the use of inorganic nanoparticles for gene therapy in PD.
Exosomes present an obvious solution to the immunoreactivity of traditional viral vectors in gene therapy. Exosomes have endogenous surface markers that are not recognised by the immune system and thus are less likely to generate immune responses even with repeated administration [20]. One recent study packaged DNA-targeting SNCA expression into exosomes, which were transfected with RV29 [111]. This ligand enabled passage through the BBB and internalisation into neurons so that the exosomes could be intravenously administered. The DNA was packed in efficient structures called ‘mini-circles’, which are essentially bacterial plasmid DNA with excess DNA fragments removed to make them smaller, but still favouring transgene expression for long periods [113]. This method provided SNCA knockdown for at least 7 weeks after a single intravenous administration. Following a second dose, a behavioural improvement was demonstrated for up to 45 days in a synuclein mouse model. There were no increased inflammatory markers, but more studies are required to assess safety of these exosomes. The approach of using exosomes allowed for the more widespread knockdown of SNCA across the brain over more targeted delivery methods such as surgery or FUS [111]. However, exosomes are clearly at their infancy and require more research to improve harvesting, purification and scalability [19].
The possibilities of combining nanoparticles with gene therapy are growing. One suggested approach has been to implant exosome-secreting cells peripherally in situ and this has already been attempted subcutaneously in 6-OHDA-lesioned mice [114]. The cells automatically produced and packaged catalase mRNA into exosomes in vivo. The surface of these exosomes had ligands for BBB penetration and neuronal uptake where catalase could then be expressed by translation of the mRNA. The results of this study demonstrated that the implantation of designer cells could deliver mRNA-containing exosomes, resulting in the attenuation of neuroinflammation in 6-OHDA-induced mice opening up the potential for further studies and new therapeutic opportunities.
The Future
As our understanding of the pathogenic mechanisms of PD improves, nanoparticles could be designed to replace or repair specific pathological processes. This would involve multi-functionalised nanoparticles with the ability to protect drugs, proteins or nucleic acids from degradation in the peripheral circulation before providing targeted and triggered release in the brain. Various mechanisms of sensing the environment and triggered release are already being studied including using focused ultrasound, external heat or local pH. It is foreseeable that techniques to respond to local dopamine levels or deep brain stimulation cues are possible. However, despite the enormous potential demonstrated in preclinical studies, there is still a paucity of clinical translation for even the most basic applications of nanoparticles to PD therapy [14]. Obstacles have included limited scalability, cost and safety [56, 115]. Clearly, addressing these challenges is essential before the potential benefit of nanoparticles in the treatment of PD can be realised. Despite this, there are certainly many avenues that are worthy to pursue in order to bring these treatments from bench to bedside.
References
Jankovic J (2002) Levodopa strengths and weaknesses. Neurology 58(4 Suppl 1):S19-32
Roco MC (2003) Nanotechnology: convergence with modern biology and medicine. Curr Opin Biotechnol 14(3):337–346
Singh R, Lillard JW Jr (2009) Nanoparticle-based targeted drug delivery. Exp Mol Pathol 86(3):215–223
Saraiva C et al (2016) Nanoparticle-mediated brain drug delivery: Overcoming blood-brain barrier to treat neurodegenerative diseases. J Control Release 235:34–47
Jesus S et al (2019) Hazard assessment of polymeric nanobiomaterials for drug delivery: what can we learn from literature so far. Front Bioeng Biotechnol 7:261
Crucho CIC, Barros MT (2017) Polymeric nanoparticles: A study on the preparation variables and characterization methods. Mater Sci Eng C Mater Biol Appl 80:771–784
Elezaby RS et al (2017) Self-assembled amphiphilic core-shell nanocarriers in line with the modern strategies for brain delivery. J Control Release 261:43–61
Zhu Y, Liu C, Pang Z (2019) Dendrimer-based drug delivery systems for brain targeting. Biomolecules. https://doi.org/10.3390/biom9120790
Rekas A et al (2009) PAMAM dendrimers as potential agents against fibrillation of alpha-synuclein, a Parkinson’s disease-related protein. Macromol Biosci 9(3):230–238
Milowska K et al (2015) Carbosilane dendrimers inhibit alpha-synuclein fibrillation and prevent cells from rotenone-induced damage. Int J Pharm 484(1–2):268–275
Mignani S et al (2017) Can dendrimer based nanoparticles fight neurodegenerative diseases? Current situation versus other established approaches. Prog Polym Sci 64:23–51
Bobo D et al (2016) Nanoparticle-based medicines: a review of FDA-approved materials and clinical trials to date. Pharm Res 33(10):2373–2387
Tunn UW (2011) A 6-month depot formulation of leuprolide acetate is safe and effective in daily clinical practice: a non-interventional prospective study in 1273 patients. BMC Urol 11:15
Anselmo AC, Mitragotri S (2019) Nanoparticles in the clinic: An update. Bioeng Transl Med 4(3):e10143
Tapeinos C, Battaglini M, Ciofani G (2017) Advances in the design of solid lipid nanoparticles and nanostructured lipid carriers for targeting brain diseases. J Control Release 264:306–332
Ghasemiyeh P, Mohammadi-Sammani S (2018) Solid lipid nanoparticles and nanostructured lipid carriers as novel drug delivery systems: applications, advantages and disadvantages. Res Pharm Sci 13(4):288–303
Pattni BS, Chupin VV, Torchilin VP (2015) New developments in liposomal drug delivery. Chem Rev 115(19):10938–10966
Batrakova EV, Kim MS (2015) Using exosomes, naturally-equipped nanocarriers, for drug delivery. J Control Release 219:396–405
Yu H et al (2020) Potential roles of exosomes in parkinson’s disease: from pathogenesis, diagnosis, and treatment to prognosis. Front Cell Dev Biol 8:86
Luo S, Du L, Cui Y (2020) Potential therapeutic applications and developments of exosomes in parkinson’s disease. Mol Pharm 17(5):1447–1457
Saupe A et al (2005) Solid lipid nanoparticles (SLN) and nanostructured lipid carriers (NLC) – structural investigations on two different carrier systems. Biomed Mater Eng 15(5):393–402
Iqbal MA et al (2012) Nanostructured lipid carriers system: Recent advances in drug delivery. J Drug Target 20(10):813–830
Singh Y et al (2017) Nanoemulsion: concepts, development and applications in drug delivery. J Control Release 252:28–49
Sheth T et al (2020) Multiple nanoemulsions. Nature Rev Mater 5(3):214–228
Stone NR et al (2016) Liposomal amphotericin B (AmBisome((R))): a review of the pharmacokinetics, pharmacodynamics clinical experience and future directions. Drugs 76(4):485–500
Rafiyath SM et al (2012) Comparison of safety and toxicity of liposomal doxorubicin vs. conventional anthracyclines: a meta-analysis. Exp Hematol Oncol. https://doi.org/10.1186/2162-3619-1-10
Sun H et al (2020) Extracellular vesicles in the development of cancer therapeutics. Int J Mol Sci. https://doi.org/10.3390/ijms21176097
Chen S et al (2016) Inorganic nanomaterials as carriers for drug delivery. J Biomed Nanotechnol 12(1):1–27
Sardar R et al (2009) Gold nanoparticles: past, present, and future. Langmuir 25(24):13840–13851
Niu S et al (2017) Inhibition by multifunctional magnetic nanoparticles loaded with alpha-synuclein RNAi plasmid in a Parkinson’s Disease model. Theranostics 7(2):344–356
John AA et al (2015) Carbon nanotubes and graphene as emerging candidates in neuroregeneration and neurodrug delivery. Int J Nanomedicine 10:4267–4277
Maiti D et al (2018) Carbon-based nanomaterials for biomedical applications: a recent study. Front Pharmacol 9:1401
Suchomel P et al (2018) Simple size-controlled synthesis of Au nanoparticles and their size-dependent catalytic activity. Sci Rep 8(1):4589
Palomäki J et al (2011) Long, needle-like carbon nanotubes and asbestos activate the NLRP3 inflammasome through a similar mechanism. ACS Nano 5(9):6861–6870
31P-MRS imaging to assess the effects of cnm-au8 on impaired neuronal Redox state in Parkinson's Disease (REPAIR-PD). 2019; Available from: https://clinicaltrials.gov/ct2/show/NCT03815916
Therapeutic nanocatalysis to slow disease progression of amyotrophic lateral sclerosis (ALS) (RESCUE-ALS). 2019; Available from: https://clinicaltrials.gov/ct2/show/NCT04098406
31P-MRS imaging to assess the effects of CNM-Au8 on impaired neuronal redox state in multiple sclerosis (REPAIR-MS). 2019; Available from: https://clinicaltrials.gov/ct2/show/NCT03993171
Khan AR et al (2018) Recent progress of drug nanoformulations targeting to brain. J Control Release 291:37–64
Paul A, Yadav KS (2020) Parkinson’s disease: Current drug therapy and unraveling the prospects of nanoparticles. J Drug Delivery Sci Technol. https://doi.org/10.1016/j.jddst.2020.101790
During MJ et al (1992) Biochemical and behavioral recovery in a rodent model of Parkinson’s disease following stereotactic implantation of dopamine-containing liposomes. Exp Neurol 115(2):193–199
Di Stefano A et al (2004) Evaluation of rat striatal L-dopa and DA concentration after intraperitoneal administration of L-dopa prodrugs in liposomal formulations. J Control Release 99(2):293–300
Di Stefano A et al (2006) Maleic- and fumaric-diamides of (O, O-diacetyl)-L-Dopa-methylester as anti-Parkinson prodrugs in liposomal formulation. J Drug Target 14(9):652–661
Yang X et al (2012) Controlled-release levodopa methyl ester/benserazide-loaded nanoparticles ameliorate levodopa-induced dyskinesia in rats. Int J Nanomed 7:2077–2086
Gambaryan PY et al (2014) Increasing the efficiency of Parkinson’s Disease treatment using a poly(lactic-co-glycolic acid) (PLGA) based L-DOPA delivery system. Exp Neurobiol 23(3):246–252
Sharma S, Lohan S, Murthy RS (2014) Formulation and characterization of intranasal mucoadhesive nanoparticulates and thermo-reversible gel of levodopa for brain delivery. Drug Dev Ind Pharm 40(7):869–878
Li X et al (2019) Preparation of levodopa-loaded crystalsomes through thermally induced crystallization reverses functional deficits in Parkinsonian mice. Biomater Sci 7(4):1623–1631
Arisoy S et al (2020) In vitro and in vivo evaluation of levodopa-loaded nanoparticles for nose to brain delivery. Pharm Dev Technol 25(6):735–747
Tan JPK et al (2019) Effective encapsulation of apomorphine into biodegradable polymeric nanoparticles through a reversible chemical bond for delivery across the blood-brain barrier. Nanomedicine 17:236–245
Regnier-Delplace C et al (2013) PLGA microparticles with zero-order release of the labile anti-Parkinson drug apomorphine. Int J Pharm 443(1–2):68–79
Md S et al (2013) Bromocriptine loaded chitosan nanoparticles intended for direct nose to brain delivery: pharmacodynamic, pharmacokinetic and scintigraphy study in mice model. Eur J Pharm Sci 48(3):393–405
Ray S et al (2018) Polysorbate 80 coated crosslinked chitosan nanoparticles of ropinirole hydrochloride for brain targeting. J Drug Deliv Sci Technol 48:21–29
Bi C et al (2016) Intranasal delivery of rotigotine to the brain with lactoferrin-modified PEG-PLGA nanoparticles for Parkinson’s disease treatment. Int J Nanomed 11:6547–6559
Tzeyung AS et al (2019) Fabrication, optimization, and evaluation of rotigotine-loaded chitosan nanoparticles for nose-to-brain delivery. Pharmaceutics. https://doi.org/10.3390/pharmaceutics11010026
Wang A et al (2012) Preparation of rotigotine-loaded microspheres and their combination use with L-DOPA to modify dyskinesias in 6-OHDA-lesioned rats. Pharm Res 29(9):2367–2376
Bali NR, Salve PS (2019) Selegiline nanoparticle embedded transdermal film: An alternative approach for brain targeting in Parkinson’s disease. J Drug Delivery Sci Technol 54:101299
Hua S et al (2018) Current trends and challenges in the clinical translation of nanoparticulate nanomedicines: pathways for translational development and commercialization. Front Pharmacol 9:790
Knop K et al (2010) Poly(ethylene glycol) in drug delivery: pros and cons as well as potential alternatives. Angew Chem Int Ed Engl 49(36):6288–6308
Tang S et al (2019) Brain-targeted intranasal delivery of dopamine with borneol and lactoferrin co-modified nanoparticles for treating Parkinson’s disease. Drug Deliv 26(1):700–707
Kang Y-S et al (2016) Use of PEGylated immunoliposomes to deliver dopamine across the blood-brain barrier in a rat model of Parkinson’s disease. CNS Neurosci Ther 22(10):817–823
Qu M et al (2018a) A brain targeting functionalized liposomes of the dopamine derivative N-3,4-bis(pivaloyloxy)-dopamine for treatment of Parkinson’s disease. J Control Release 277:173–182
Wen CJ et al (2012) Theranostic liposomes loaded with quantum dots and apomorphine for brain targeting and bioimaging. Int J Nanomed 7:1599–1611
Liu KS et al (2012) Combined strategies of apomorphine diester prodrugs and nanostructured lipid carriers for efficient brain targeting. Nanotechnology 23(9):095103
Wang F et al (2020) Facile nose-to-brain delivery of rotigotine-loaded polymer micelles thermosensitive hydrogels: In vitro characterization and in vivo behavior study. Int J Pharm 577:119046
Yan X et al (2018) Lactoferrin-modified rotigotine nanoparticles for enhanced nose-to-brain delivery: LESA-MS/MS-based drug biodistribution, pharmacodynamics, and neuroprotective effects. Int J Nanomed 13:273–281
Riddle MC (2016) Lessons from Peglispro: IMAGINE how to improve drug development and affordability. Diabetes Care 39(4):499–501
Rehman S et al (2019) Intranasal delivery of mucoadhesive nanocarriers: a viable option for Parkinson’s disease treatment? Expert Opin Drug Deliv 16(12):1355–1366
Pardeshi CV, Belgamwar VS (2019) Improved brain pharmacokinetics following intranasal administration of N, N, N-trimethyl chitosan tailored mucoadhesive NLCs. Mater Technol 35(5):249–266
Trapani A et al (2011) Characterization and evaluation of chitosan nanoparticles for dopamine brain delivery. Int J Pharm 419(1–2):296–307
Raj R et al (2018) Pramipexole dihydrochloride loaded chitosan nanoparticles for nose to brain delivery: Development, characterization and in vivo anti-Parkinson activity. Int J Biol Macromol 109:27–35
Lundh B, Brockstedt U, Kristensson K (1989) Lectin-binding pattern of neuroepithelial and respiratory epithelial cells in the mouse nasal cavity. Histochem J 21(1):33–43
Wen Z et al (2011) Odorranalectin-conjugated nanoparticles: preparation, brain delivery and pharmacodynamic study on Parkinson’s disease following intranasal administration. J Control Release 151(2):131–138
Gao X et al (2006) Lectin-conjugated PEG-PLA nanoparticles: preparation and brain delivery after intranasal administration. Biomaterials 27(18):3482–3490
Gabathuler R (2010) Approaches to transport therapeutic drugs across the blood-brain barrier to treat brain diseases. Neurobiol Dis 37(1):48–57
Demeule M et al (2002) Drug transport to the brain: Key roles for the efflux pump P-glycoprotein in the blood-brain barrier. Vascul Pharmacol 38:339–348
Kageyama T et al (2000) The 4F2hc/LAT1 complex transports l-DOPA across the blood–brain barrier. Brain Res 879(1):115–121
Fillebeen C et al (1999) Receptor-mediated transcytosis of lactoferrin through the blood-brain barrier. J Biol Chem 274(11):7011–7017
Faucheux A et al (1995) Expression of lactogerrin receptors is increased in the mesencephalon of patients with Parkinson disease. Natl Acad Sci United States America 92(21):9603–9607
Suzuki YA, Lopez V, Lonnerdal B (2005) Mammalian lactoferrin receptors: structure and function. Cell Mol Life Sci 62(22):2560–2575
Abuirmeileh A et al (2007) The corticotrophin-releasing factor-like peptide urocortin reverses key deficits in two rodent models of Parkinson’s disease. Eur J Neurosci 26(2):417–423
Hu K et al (2011) Lactoferrin conjugated PEG-PLGA nanoparticles for brain delivery: preparation, characterization and efficacy in Parkinson’s disease. Int J Pharm 415(1–2):273–283
Huang R et al (2010) Gene therapy using lactoferrin-modified nanoparticles in a rotenone-induced chronic Parkinson model. J Neurol Sci 290(1–2):123–130
Huang R et al (2013) Angiopep-conjugated nanoparticles for targeted long-term gene therapy of Parkinson’s disease. Pharm Res 30(10):2549–2559
Tang SC et al (2016) ANG1005, a novel peptide-paclitaxel conjugate crosses the BBB and shows activity in patients with recurrent CNS metastasis from breast cancer, results from a phase II clinical study. Ann Oncol. https://doi.org/10.1093/annonc/mdw367.02
A randomized open-label, Multi-Center Pivotal Study of ANG1005 Compared With Physician’s Best Choice in HER2-Negative Breast Cancer Patients with Newly Diagnosed Leptomeningeal Carcinomatosis and Previously Treated Brain Metastases (ANGLeD). 2018 7 September, 2020; Available from: https://clinicaltrials.gov/ct2/show/NCT03613181
Wilson B et al (2008) Targeted delivery of tacrine into the brain with polysorbate 80-coated poly(n-butylcyanoacrylate) nanoparticles. Eur J Pharm Biopharm 70(1):75–84
Fisher DG, Price RJ (2019) Recent advances in the use of focused ultrasound for magnetic resonance image-guided therapeutic nanoparticle delivery to the central nervous system. Front Pharmacol 10:1348
Lin CY et al (2016) Non-invasive, neuron-specific gene therapy by focused ultrasound-induced blood-brain barrier opening in Parkinson’s disease mouse model. J Control Release 235:72–81
Yue P et al (2018) Ultrasound-triggered effects of the microbubbles coupled to GDNF plasmid-loaded PEGylated liposomes in a rat model of Parkinson’s disease. Front Neurosci 12:222
Anti-EGFR-immunoliposomes Loaded with Doxorubicin in Patients with Advanced Triple Negative EGFR Positive Breast Cancer. 2016; Available from: https://clinicaltrials.gov/ct2/show/NCT02833766
Mamot C et al (2005) Epidermal growth factor receptor-targeted immunoliposomes significantly enhance the efficacy of multiple anticancer drugs in vivo. Cancer Res 65(24):11631–11638
Wolfram J, Ferrari M (2019) Clinical cancer nanomedicine. Nano Today 25:85–98
Celsion corporation to continue following patients in Phase III OPTIMA Study for Overall Survival. 2020; Available from: https://investor.celsion.com/news-releases/news-release-details/celsion-corporation-continue-following-patients-phase-iii-optima
Elkouzi A et al (2019) Emerging therapies in Parkinson disease - repurposed drugs and new approaches. Nat Rev Neurol 15(4):204–223
Levin J et al (2019) Safety and efficacy of epigallocatechin gallate in multiple system atrophy (PROMESA): a randomised, double-blind, placebo-controlled trial. Lancet Neurol 18(8):724–735
Malar DS et al (2020) Neuroprotective properties of green tea (Camellia sinensis) in Parkinson’s disease: a review. Molecules. https://doi.org/10.3390/molecules25173926
Li Y et al (2018) “Cell-addictive” dual-target traceable nanodrug for Parkinson’s disease treatment via flotillins pathway. Theranostics 8(19):5469–5481
Gao G et al (2019) Gold nanoclusters for Parkinson’s disease treatment. Biomaterials 194:36–46
Srivastava AK, Roy Choudhury S, Karmakar S (2020) Melatonin/polydopamine nanostructures for collective neuroprotection-based Parkinson’s disease therapy. Biomater Sci 8(5):1345–1363
Parkinson Study Group Q.E.I. et al (2014) A randomized clinical trial of high-dosage coenzyme Q10 in early Parkinson disease: no evidence of benefit. JAMA Neurol 71(5): 543–52
Anand P et al (2007) Bioavailability of curcumin: problems and promises. Mol Pharm 4(6):807–818
Sikorska M et al (2014) Nanomicellar formulation of coenzyme Q10 (Ubisol-Q10) effectively blocks ongoing neurodegeneration in the mouse 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine model: potential use as an adjuvant treatment in Parkinson’s disease. Neurobiol Aging 35(10):2329–2346
Zhang N et al (2018) Localized delivery of curcumin into brain with polysorbate 80-modified cerasomes by ultrasound-targeted microbubble destruction for improved Parkinson’s disease therapy. Theranostics 8(8):2264–2277
Xue Y et al (2020) Neuroprotective effect of chitosan nanoparticle gene delivery system grafted with acteoside (ACT) in Parkinson’s disease models. J Mater Sci Technol 43:197–207
Chen T et al (2019) Nanoparticles Mediating the Sustained Puerarin Release Facilitate Improved Brain Delivery to Treat Parkinson’s Disease. ACS Appl Mater Interfaces 11(48):45276–45289
Xiong S et al (2019) Oral delivery of puerarin nanocrystals to improve brain accumulation and anti-parkinsonian efficacy. Mol Pharm 16(4):1444–1455
Ho KS, Hotchkin MT, Mortenson MT (2019) Gold nanocatalysis as a novel therapeutic for neuroprotection in Parkinson's disease. In Program no. 743.04. 2019 neuroscience meeting planner. Society for Neuroscience, Chicago, IL. https://www.abstractsonline.com/pp8/#!/7883/presentation/57120
Nunez MT, Chana-Cuevas P (2018) New perspectives in iron chelation therapy for the treatment of neurodegenerative diseases. Pharmaceuticals (Basel). https://doi.org/10.3390/ph11040109
Martin-Bastida A et al (2017) Brain iron chelation by deferiprone in a phase 2 randomised double-blinded placebo controlled clinical trial in Parkinson’s disease. Sci Rep 7(1):1398
You L et al (2018) Targeted brain delivery of rabies virus glycoprotein 29-modified deferoxamine-loaded nanoparticles reverses functional deficits in Parkinsonian mice. ACS Nano 12(5):4123–4139
Hu K et al (2018) Neuroprotective effect of gold nanoparticles composites in Parkinson’s disease model. Nanomedicine 14(4):1123–1136
Izco M et al (2019) Systemic exosomal delivery of shRNA minicircles prevents Parkinsonian pathology. Mol Ther 27(12):2111–2122
Mead BP et al (2016) Targeted gene transfer to the brain via the delivery of brain-penetrating DNA nanoparticles with focused ultrasound. J Control Release 223:109–117
Darquet AM et al (1997) A new DNA vehicle for nonviral gene delivery:supercoiled minicircle. Gene Therapy 4:1341–1349
Kojima R et al (2018) Designer exosomes produced by implanted cells intracerebrally deliver therapeutic cargo for Parkinson’s disease treatment. Nat Commun 9(1):1305
Accomasso L, Cristallini C, Giachino C (2018) Risk assessment and risk minimization in nanomedicine: a need for predictive, alternative, and 3Rs strategies. Front Pharmacol 9:228
Beloqui A et al (2016) Nanostructured lipid carriers: Promising drug delivery systems for future clinics. Nanomed Nanotechnol Biol Med 12(1):143–161
Allen TM, Cullis PR (2013) Liposomal drug delivery systems: from concept to clinical applications. Adv Drug Deliv Rev 65(1):36–48
Wang ZY et al (2019) Strategies for brain-targeting liposomal delivery of small hydrophobic molecules in the treatment of neurodegenerative diseases. Drug Discov Today 24(2):595–605
Ghosh P et al (2008) Gold nanoparticles in delivery applications. Adv Drug Deliv Rev 60(11):1307–1315
Suk JS et al (2016) PEGylation as a strategy for improving nanoparticle-based drug and gene delivery. Adv Drug Deliv Rev 99:28–51
Cao X et al (2016) Effects and molecular mechanism of chitosan-coated levodopa nanoliposomes on behavior of dyskinesia rats. Biol Res 49(1):32
Casettari L, Illum L (2014) Chitosan in nasal delivery systems for therapeutic drugs. J Control Release 190:189–200
Sridhar V et al (2018) Pharmacokinetics and pharmacodynamics of intranasally administered selegiline nanoparticles with improved brain delivery in Parkinson’s disease. Nanomedicine 14(8):2609–2618
Lopalco A et al (2018) Transferrin functionalized liposomes loading dopamine HCl: development and permeability studies across an in vitro model of human blood-brain barrier. Nanomaterials (Basel). https://doi.org/10.3390/nano8030178
Qu M et al (2018b) Dopamine-loaded blood exosomes targeted to brain for better treatment of Parkinson’s disease. J Control Release 287:156–166
Funding
SJGL is supported by an NHMRC Leadership Fellowship (#1195830), as well as funding to ForeFront, a collaborative research group at the Brain and Mind Centre University of Sydney, from NHMRC program (#1132524), Dementia Research Team (#1095127), CogSleep Centre of Research Excellence (#1152945) grants.
Author information
Authors and Affiliations
Contributions
JB was responsible for drafting and revision of the manuscript and JEJ for revision of the manuscript. SJGL was responsible for concept and revision of the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
There are no conflicts of interest.
Rights and permissions
About this article
Cite this article
Baskin, J., Jeon, J.E. & Lewis, S.J.G. Nanoparticles for drug delivery in Parkinson’s disease. J Neurol 268, 1981–1994 (2021). https://doi.org/10.1007/s00415-020-10291-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-020-10291-x