Abstract
This study aimed to determine the etiologic distribution of dizziness and vertigo in a referral-based dizziness clinic in South Korea. We analyzed the diagnoses of 21,166 consecutive dizzy patients (12,691 women, mean age = 57.9 ± 15.7, age range = 3–97) seen from 2003 to 2019 using a registry and medical records. Overall, dizziness and vertigo were more common in women (60.0%, CI 0.59–0.61) than in men without a difference in age (57.7 ± 15.5 vs. 58.1 ± 16.1, p = 0.094). Benign paroxysmal positional vertigo (BPPV, 24.1%) was the most common cause of dizziness/vertigo, followed by psychiatric or persistent postural perceptual dizziness (20.8%), vascular disorders (12.9%), vestibular migraine (10.2%), Meniere’s disease (7.2%), and vestibular neuritis (5.4%). These six disorders comprised more than 80% of all disorders. The etiology could not be determined in 5.0%, and more than one etiology was found in 14.1%. Vestibular migraine was the most common disorder in children and adolescents (< 19 years), psychiatric or persistent postural perceptual dizziness (26.3%) in the adults (19–64 years), and BPPV (28.2%) in the elderly (≥ 65 years). This etiologic distribution is similar to that reported in another country, and indicates no significant differences in the proportion of diseases causing dizziness and vertigo across different ethnic groups. This study provides valuable information to establish healthcare policy for dizziness and vertigo.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dizziness is one of the most common symptoms leading to a hospital visit with a lifetime prevalence of 17–30% [1,2,3]. According to the Healthcare Bigdata Hub (health insurance review and assessment service in South Korea), the number of patients and medical expenditures due to dizziness (ICD10 code R42: dizziness and giddiness and H81: disorders of vestibular function) are increasing rapidly. Compared to those in 2014, for example, the number of patients with dizziness (1,935,723, 3.7% of total population) had increased by 19.4% along with an 80% increase of the medical expenditure (217 million USD, about 112 USD per each patient with dizziness/vertigo) in 2018 in South Korea. Since dizziness and vertigo are caused by various disorders including peripheral or central vestibular diseases, psychiatric disorders, and systemic illnesses, it would be important to identify the underlying causes and their proportion according to age and sex not only for diagnosing and treating individual patient but also for establishing public health strategy. The etiologic distribution of dizziness/vertigo has been reported in Germany [4, 5]. Etiologic distribution, however, may be dissimilar among different ethnic groups and can be dependent upon the clinical settings (acute vs. referral-based) or the physicians in charge (otolaryngologists vs. neurologists vs. others).
This study aimed to determine the etiologic distribution of dizziness/vertigo according to age and sex in Koreans by analyzing the diagnoses of 21,166 consecutive patients with dizziness/vertigo in a referral-based dizziness clinic run by neurologists in South Korea.
Methods
Subjects
This study was based on 21,166 consecutive patients who had been managed at the dizziness clinic of Seoul National University Bundang Hospital, Seongnam, South Korea, from 2003 to 2019. The data on diagnoses and clinical information were acquired using electronic medical records and a dizziness registry embedded in the medical records.
Diagnosis
Diagnostic terms were unified and entered into the registry that consisted of the main and sub-categories. The main category included the disorders responsible for dizziness/vertigo according to the International Classification of Vestibular Disorders (ICVD-I) layer 3 and the disorders adopted in the previous study [4, 6], while the sub-category included the specific diagnosis or subtypes of the diseases.
All diagnoses were made by the senior author (JSK) according to widely accepted diagnostic criteria for each vestibular disorder or the ICVD criteria when available [7,8,9,10,11,12,13,14,15,16,17,18,19]. When the criteria were available, we also included the patients with probable diagnosis [7, 13, 14]. We revised the registry whenever new diagnoses were made or added for each patient but did not re-classify the previous diagnoses according the newly developed diagnostic criteria. Vestibular neuritis (VN) was diagnosed according to the criteria previously proposed by the authors [19]. The diagnoses of vascular vertigo were made when the patients developed dizziness/vertigo in association with imaging evidences of vascular lesions (hypoperfusion, infarction, and hemorrhages) that may explain the dizziness/vertigo, and when other causes could not be found. When the vascular lesions were negative on brain imaging, additional central symptoms and signs were counted in addition to multiple vascular risk factors, again when other causes could not be found. When a patient had more than one disease, each diagnosis was counted. Thus, 24,619 diagnoses were extracted from 21,166 patients.
Statistical analyses
Student’s t test was used to compare continuous variables (age) between women and men, and the Brown–Forsythe test among the disease groups. Games–Howell test was performed for post hoc analyses. Chi-square test was adopted to compare the nominal variables (sex) between the disease groups, and the proportion of diseases between the first and the last 5 years of the study period. The one-sample proportion test determined the sex ratio in each disease in comparison to that in general population. All the tests were performed using R (version 3.3.3, https://www.r-project.org/) and p < 0.05 was considered significant.
Standard protocol approvals
All experiments followed the tenets of the Declaration of Helsinki and this study was approved by the Institutional Review Board of Seoul National University Bundang Hospital (IRB No. B-1907/553-001).
Results
Demographic characteristics
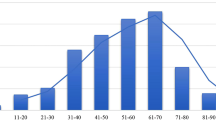
The patients included 8,474 (40.0%) men and 12,693 (60.0%) women with a women-to-man ratio of 1.5:1. This female predominance was maintained across all age groups with the highest ratio of 1.68:1 in the 6th decade (Supplementary figure). The mean age of the patients was 57.9 ± 15.7 (Fig. 1, median = 60.0, age range = 3–97) without a difference between women and men (57.7 ± 15.5 vs. 58.1 ± 16.1, p = 0.094).
Age distribution and sex ratio in general and age distribution by the disease. The age at diagnosis differs significantly among the diseases (Brown–Forsythe test, p < 0.001). The female predominance is maintained across all age groups (men:women = 1:1.5). The dotted line indicates the mean number of population in each age from 2015 to 2018 (KOSIS; KOrean Statistical Information Service). BPPV benign paroxysmal positional vertigo, MD Meniere’s disease, PPPD psychogenic/persistent postural perceptual dizziness, VM vestibular migraine, VN vestibular neuritis
Etiologic distribution: general
The underlying diseases and disorders are presented in ‘Table 1’ according to their proportion. Benign paroxysmal positional vertigo (BPPV, 24.2%) was the most common diagnosis, followed by psychogenic/persistent postural perceptual dizziness (PPPD, 20.8%), vascular vertigo (12.9%, Supplementary Table 1), vestibular migraine (10.2%), Meniere’s disease (7.2%), and vestibular neuritis (5.4%). These six diseases accounted for more than 80% of total diagnoses. Especially, BPPV and psychogenic/PPPD comprised nearly half of the diagnoses. The diseases with less than 1% proportion were categorized into ‘Other miscellaneous causes’ (Supplementary Table 2). A single diagnosis was assigned to 85.8% of the patients while two or more diagnoses were made in 14.2% of the patients. In contrast, no definite cause was found in 5% of the patients. Comorbid vestibular disorders were found 22.6% of the patients with psychogenic/PPPD, and the most common diseases include BPPV in 29.1%, vestibular migraine in 18.8%, vascular disorders in 12.4%, Meniere’ disease in 11.9%, and VN in 7.5%.
The relative proportion of each disorder had changed significantly over the study period (Chi-square test, p < 0.001). Especially, the proportions of BPPV, vascular vertigo, and vestibular neuritis had decreased while those of psychogenic/PPPD, vestibular migraine, and Meniere’s disease had increased from the first 5 to the last 5 years of the study period (Fig. 2).
Proportion of each disorder during the first and last 5 years of the study period. The proportion of disorders responsible for dizziness/vertigo had changed significantly over the study period (Chi-square test, p < 0.001). Especially, the proportions of benign paroxysmal positional vertigo (BPPV), vascular vertigo, and vestibular neuritis (VN) had decreased while those of psychogenic/persistent postural perceptual dizziness (PPPD), vestibular migraine (VM) and Meniere’s disease (MD) had increased from the first five to the last 5 years of the study period
Etiologic distribution according to sex
The sex ratio was different significantly among the disorders (Fig. 3, Chi-square test, p < 0.001). Vestibular migraine, BPPV, psychogenic/PPPD, neoplasm, and Meniere’s disease were more prevalent in women with the highest proportion of women at 81% in vestibular migraine. In contrast, vestibular neuritis, degenerative disorders, bilateral vestibulopathy, vascular vertigo, and cardiac/autonomic disorders were more commonly diagnosed in men with the highest proportion of men at 59% in cardiac/autonomic disorders. When compared with general population (women = 50.1%, men = 49.9%), the female predominance was statistically significant for vestibular migraine (women = 80.9%, p < 0.001), BPPV (women = 71.2%, p < 0.001), psychogenic/PPPD (women = 64.1%, p < 0.001), and Meniere’s disease (women = 58.5%, p < 0.001). In contrast, vascular vertigo showed a male predominance (men = 58.2%, p < 0.001). The sex ratio in VN (men = 51.0%, p = 0.5398) did not show a significant difference compared to the general population.
Sex distribution by the disease. The sex ratio was different significantly among the disorders (Chi-square test, p < 0.001). A female predominance was observed in vestibular migraine, BPPV, psychogenic/PPPD, neoplastic, and Meniere’s disease while a male predominance was found in degenerative disorders, bilateral vestibulopathy, vascular vertigo, and cardiac/autonomic disorders. In contrast, vestibular neuritis occurred equally in both women and men. BPPV benign paroxysmal positional vertigo, PPPD persistent postural perceptual dizziness
Etiologic distribution according to age at diagnosis
The age at diagnosis was different among the disorders (Fig. 1, Brown–Forsythe test, p < 0.001). The patients with vestibular migraine was youngest (49.5 ± 16.4) while those with bilateral vestibulopathy was oldest (67.9 ± 13.3).
The mean age of the patients with dizziness/vertigo was higher than that of general population of South Korea (KOSIS; KOrean Statistical Information Service, population census, 2015–2018) (Fig. 1). The proportion of the elderly (≥ 65 old) was 13.7% in the general population while it was 37.7% in patients with dizziness/vertigo. The patients with BPPV (61.7 ± 12.7) and vascular disorders (65.1 ± 12.5) were older when diagnosed while psychogenic/PPPD (52.7 ± 14.9) and vestibular migraine (49.5 ± 16.4) were more commonly observed in younger patients (Fig. 1). Thus, vestibular migraine was the most common cause in children and adolescents (< 19 years, 35.0%) while BPPV (28.2%) was the most common disease in the elderly (≥ 65, Table 2). In the adults (19–64 age), psychogenic/PPPD (26.3%) was the most common (Table 2).
Estimation of the number of hospital visits due to dizziness/vertigo
We estimated the number of hospital visits due to dizziness/vertigo in South Korea in 2050 using the data from the KOSIS and the Healthcare Bigdata Hub (health insurance review and assessment service in South Korea). The general population in 2050 is expected to decrease by approximately 8% (47,744,500) with an increase in the proportion of elderly compared to that in 2019. Since the data showed no changes in the number of hospital visits due to dizziness/vertigo (H81 and R42) per capita in each age group of general population from 2010 to 2019, we estimated the numbers using the data reported in 2019. The number of hospital visits due to dizziness/vertigo was 2,055,122 in 2019 and was estimated at 2,891,761 in 2050, an increase of 40% over the years. This corresponds to 3,974 visits per 100,000 of general population in 2019 and 6057 in 2050, an increase of 52% over the years.
Discussion
Our study showed various causes of dizziness/vertigo in a referral-based dizziness clinic in South Korea, but only six disorders accounted for more than 80% of all diseases. Especially, BPPV and psychogenic/PPPD were most common and comprised nearly a half of the diagnoses.
Dizziness/vertigo is one of the most common symptoms across all age groups, but the prevalence typically increases with aging. This increase in the prevalence of dizziness/vertigo with aging is well explained by an age-related decline in the labyrinthine hair cell density in mice [20], and a decrease in the otolithic function in the elderly [21, 22]. Age-related changes in hormones, various extrinsic factors, and increased oxidative stress may lead to apoptosis of the inner ear hair cells [23,24,25]. Our data also clearly show higher prevalence of dizziness/vertigo in the aged population in both men and women. According to the World Population Ageing 2019, proportion of the people aged 65 or over is rapidly increasing from 6% in 2019 to 16% by 2050 [26]. This aging trend is steeper and more serious in South Korea, from 15% in 2019 to 39% in 2050, than in other countries according to the data from KOSIS. In this study, we also predicted that the number of hospital visits due to dizziness/vertigo would increase by 52% per 100,000 population from 2019 to 2050 in South Korea, which necessitates urgent establishment of health care policies for dizziness/vertigo.
The relative proportion of each disorder causing dizziness/vertigo differed among different age groups. While vestibular migraine and psychogenic/PPPD were more common in younger population (< 65 years), BPPV and vascular vertigo were more prevalent in the aged group (≥ 65 years). These findings are consistent with those reported previously for each disorder in other ethnic backgrounds [3, 5]. In this study, the mean age at diagnosis was 50–60 years in most disorders. These findings are also in line with those reported previously for each disorder: BPPV [27, 28], psychogenic/PPPD [29], vestibular migraine [30], Meniere’s disease [31], VN [32], and vascular vertigo [33,34,35].
It is well known that dizziness/vertigo is more prevalent in women than in men [5, 36]. Indeed, we found a female predominance across all age groups with the highest ratio of 1.68:1 in the 6h decade (Supplementary figure). This applies to most of the highly prevalent disorders including vestibular migraine, BPPV, psychogenic/PPPD, and Meniere’s disease. In contrast, vascular vertigo showed a male predominance while VN occurred equally in women and men. These findings are also in line with the findings reported for each disorder; BPPV [27], psychogenic/PPPD [29], vestibular migraine [30] and Meniere’s disease [31], and VN [32]. In our study, only vascular dizziness/vertigo showed a male preponderance among the six major diseases. The sex ratio has been controversial in previous case series on vascular vertigo [35], but male gender is one of the known risk factors for stroke [37, 38].
The etiologic distribution observed in this study is similar to that reported in Germany [4]. This indicates no significant differences in the proportion of diseases causing dizziness and vertigo across different ethnic groups. However, some disorders require further consideration. Compared to the proportions reported in Germany, those of bilateral vestibulopathy (5.1% vs. 1.4%) and vestibular paroxysmia (3.9% vs. 0.5%) were relatively lower in our study [4]. The reason for this discrepancy is unknown, but the patients with bilateral vestibulopathy in association with other disorders (secondary) were more likely classified into the underlying disorders in our study [39]. Given the establishment of the diagnostic criteria for vestibular paroxysmia only recently, and increasing diagnoses of this disorder over the recent years in this study, the recognition of this disorder appears to be delayed in South Korea [11, 40, 41]. Otherwise, the patients with vestibular paroxysmia and bilateral vestibulopathy might have been managed by the ENT doctors more often than by neurologists.
PPPD and psychogenic dizziness were the second most common cause of dizziness and vertigo in our study. In contrast to the previous study performed in Germany [4], we did not separate these two disorders in calculating the proportion. This was mostly due to the frequent association and overlap of PPPD with psychiatric disorders, and rather recent recognition of PPPD in this country [9, 42].
Limitation
This study has several limitations. First of all, this study was conducted in a referral-based hospital mostly run by neurologists. Thus, the selection and referral biases would have been inevitable, and the results cannot be generalized to other primary clinics or referral-based clinic mostly run by ENT doctors. Unfortunately, the discrepancy between the diagnoses made by the referring doctors and those finally made after evaluation at the specialized dizziness clinic could not be determined in this study, and should be sought in future studies. Second, this study was retrospective in nature even though the data had been collected prospectively. Thus, there would have been uncontrollable variables. For example, the data in this study had been collected over about 16 years (from 2003 to 2019). The diagnostic criteria of each disorder or the settings of the clinic thus may have been changed during this period. Since we did not reclassify the diagnoses according to the newly developed guidelines, these may have influenced the results of this study. Indeed, the relative proportions of psychogenic/PPPD and vestibular migraine had increased during the last 5 years compared to those during the first 5 years of the study period, which may have been related to establishment of ICVD diagnostic criteria for these disorders. Moreover, errors or biases may have been inevitable since the diagnoses were mostly made by the senior author and it was not verified by another specialist. Again, this should be clarified in future studies adopting another study design. In patients with co-morbid vestibular disorders, the possibility of including only the principal diagnosis could not be excluded either.
References
Murdin L, Schilder AG (2015) Epidemiology of balance symptoms and disorders in the community: a systematic review. Otol Neurotol 36(3):387–392. https://doi.org/10.1097/MAO.0000000000000691
Kroenke K, Price RK (1993) Symptoms in the community. Prevalence, classification, and psychiatric comorbidity. Arch Intern Med 153(21):2474–2480
Neuhauser HK, von Brevern M, Radtke A, Lezius F, Feldmann M, Ziese T, Lempert T (2005) Epidemiology of vestibular vertigo: a neurotologic survey of the general population. Neurology 65(6):898–904. https://doi.org/10.1212/01.wnl.0000175987.59991.3d
Strupp M, Brandt T (2008) Diagnosis and treatment of vertigo and dizziness. Dtsch Arztebl Int 105(10):173–180. https://doi.org/10.3238/arztebl.2008.0173
Kruschinski C, Kersting M, Breull A, Kochen MM, Koschack J, Hummers-Pradier E (2008) Frequency of dizziness-related diagnoses and prescriptions in a general practice database. Z Evid Fortbild Qual Gesundhwes 102(5):313–319. https://doi.org/10.1016/j.zefq.2008.05.001
Bisdorff AR, Staab JP, Newman-Toker DE (2015) Overview of the international classification of vestibular disorders. Neurol Clin 33(3):541–550, vii. https://doi.org/10.1016/j.ncl.2015.04.010
Lopez-Escamez JA, Carey J, Chung WH, Goebel JA, Magnusson M, Mandala M, Newman-Toker DE, Strupp M, Suzuki M, Trabalzini F, Bisdorff A, Classification Committee of the Barany S, Japan Society for Equilibrium R, European Academy of O, Neurotology, Equilibrium Committee of the American Academy of O-H, Neck S, Korean Balance S (2015) Diagnostic criteria for Meniere's disease. J Vestib Res 25(1):1–7. https://doi.org/10.3233/VES-15054
Kim HA, Bisdorff A, Bronstein AM, Lempert T, Rossi-Izquierdo M, Staab JP, Strupp M, Kim JS (2019) Hemodynamic orthostatic dizziness/vertigo: diagnostic criteria. J Vestib Res 29(2–3):45–56. https://doi.org/10.3233/VES-190655
Staab JP, Eckhardt-Henn A, Horii A, Jacob R, Strupp M, Brandt T, Bronstein A (2017) Diagnostic criteria for persistent postural-perceptual dizziness (PPPD): consensus document of the committee for the Classification of Vestibular Disorders of the Barany Society. J Vestib Res 27(4):191–208. https://doi.org/10.3233/VES-170622
Strupp M, Kim JS, Murofushi T, Straumann D, Jen JC, Rosengren SM, Della Santina CC, Kingma H (2017) Bilateral vestibulopathy: diagnostic criteria consensus document of the Classification Committee of the Barany Society. J Vestib Res 27(4):177–189. https://doi.org/10.3233/VES-170619
Strupp M, Lopez-Escamez JA, Kim JS, Straumann D, Jen JC, Carey J, Bisdorff A, Brandt T (2016) Vestibular paroxysmia: diagnostic criteria. J Vestib Res 26(5–6):409–415. https://doi.org/10.3233/VES-160589
von Brevern M, Bertholon P, Brandt T, Fife T, Imai T, Nuti D, Newman-Toker D (2015) Benign paroxysmal positional vertigo: diagnostic criteria. J Vestib Res 25(3–4):105–117. https://doi.org/10.3233/VES-150553
Lempert T, Olesen J, Furman J, Waterston J, Seemungal B, Carey J, Bisdorff A, Versino M, Evers S, Newman-Toker D (2012) Vestibular migraine: diagnostic criteria. J Vestib Res 22(4):167–172. https://doi.org/10.3233/VES-2012-0453
Goebel JA (2016) 2015 equilibrium Committee Amendment to the 1995 AAO-HNS guidelines for the definition of Meniere's disease. Otolaryngol Head Neck Surg 154(3):403–404. https://doi.org/10.1177/0194599816628524
Brandt T, Dieterich M (1994) Vestibular paroxysmia: vascular compression of the eighth nerve? Lancet 343(8900):798–799. https://doi.org/10.1016/s0140-6736(94)91879-1
Brandt T (1996) Phobic postural vertigo. Neurology 46(6):1515–1519. https://doi.org/10.1212/wnl.46.6.1515
Dieterich M, Staab JP, Brandt T (2016) Functional (psychogenic) dizziness. Handb Clin Neurol 139:447–468. https://doi.org/10.1016/B978-0-12-801772-2.00037-0
Kim S, Oh YM, Koo JW, Kim JS (2011) Bilateral vestibulopathy: clinical characteristics and diagnostic criteria. Otol Neurotol 32(5):812–817. https://doi.org/10.1097/MAO.0b013e31821a3b7d
Jeong SH, Kim HJ, Kim JS (2013) Vestibular neuritis. Semin Neurol 33(3):185–194. https://doi.org/10.1055/s-0033-1354598
Shiga A, Nakagawa T, Nakayama M, Endo T, Iguchi F, Kim TS, Naito Y, Ito J (2005) Aging effects on vestibulo-ocular responses in C57BL/6 mice: comparison with alteration in auditory function. Audiol Neurootol 10(2):97–104. https://doi.org/10.1159/000083365
Chang CM, Young YH, Cheng PW (2012) Age-related changes in ocular vestibular-evoked myogenic potentials via galvanic vestibular stimulation and bone-conducted vibration modes. Acta Otolaryngol 132(12):1295–1300. https://doi.org/10.3109/00016489.2012.708437
Kim HJ, Lee JH, Kim JS (2014) Ocular vestibular evoked myogenic potentials to head tap and cervical vestibular evoked myogenic potentials to air-conducted sounds in isolated internuclear ophthalmoplegia. Clin Neurophysiol 125(5):1042–1047. https://doi.org/10.1016/j.clinph.2013.10.013
Iwasaki S, Yamasoba T (2015) Dizziness and imbalance in the elderly: age-related decline in the vestibular system. Aging Dis 6(1):38–47. https://doi.org/10.14336/AD.2014.0128
Yamasoba T, Lin FR, Someya S, Kashio A, Sakamoto T, Kondo K (2013) Current concepts in age-related hearing loss: epidemiology and mechanistic pathways. Hear Res 303:30–38. https://doi.org/10.1016/j.heares.2013.01.021
Cheng AG, Cunningham LL, Rubel EW (2005) Mechanisms of hair cell death and protection. Curr Opin Otolaryngol Head Neck Surg 13(6):343–348. https://doi.org/10.1097/01.moo.0000186799.45377.63
UN (2020) World Population Ageing 2019. vol ST/ESA/SER.A/444
Baloh RW, Honrubia V, Jacobson K (1987) Benign positional vertigo: clinical and oculographic features in 240 cases. Neurology 37(3):371–378. https://doi.org/10.1212/wnl.37.3.371
Kim HJ, Kim JS (2017) The patterns of recurrences in idiopathic benign paroxysmal positional vertigo and self-treatment evaluation. Front Neurol 8:690. https://doi.org/10.3389/fneur.2017.00690
Staab JP, Ruckenstein MJ (2007) Expanding the differential diagnosis of chronic dizziness. Arch Otolaryngol Head Neck Surg 133(2):170–176. https://doi.org/10.1001/archotol.133.2.170
Formeister EJ, Rizk HG, Kohn MA, Sharon JD (2018) The epidemiology of vestibular migraine: a population-based survey study. Otol Neurotol 39(8):1037–1044. https://doi.org/10.1097/MAO.0000000000001900
Ballester M, Liard P, Vibert D, Hausler R (2002) Meniere's disease in the elderly. Otol Neurotol 23(1):73–78. https://doi.org/10.1097/00129492-200201000-00017
Brandt T (2003) Vestibular neuritis. In: Vertigo. Springer, New York, pp 67–81. doi:10.1007/978-1-4757-3801-8
Grad A, Baloh RW (1989) Vertigo of vascular origin. Clinical and electronystagmographic features in 84 cases. Arch Neurol 46(3):281–284. https://doi.org/10.1001/archneur.1989.00520390047014
Choi JH, Park MG, Choi SY, Park KP, Baik SK, Kim JS, Choi KD (2017) Acute transient vestibular syndrome: prevalence of stroke and efficacy of bedside evaluation. Stroke 48(3):556–562. https://doi.org/10.1161/STROKEAHA.116.015507
Kattah JC, Talkad AV, Wang DZ, Hsieh YH, Newman-Toker DE (2009) HINTS to diagnose stroke in the acute vestibular syndrome: three-step bedside oculomotor examination more sensitive than early MRI diffusion-weighted imaging. Stroke 40(11):3504–3510. https://doi.org/10.1161/STROKEAHA.109.551234
Bisdorff A, Bosser G, Gueguen R, Perrin P (2013) The epidemiology of vertigo, dizziness, and unsteadiness and its links to co-morbidities. Front Neurol 4:29. https://doi.org/10.3389/fneur.2013.00029
Kerber KA, Brown DL, Lisabeth LD, Smith MA, Morgenstern LB (2006) Stroke among patients with dizziness, vertigo, and imbalance in the emergency department: a population-based study. Stroke 37(10):2484–2487. https://doi.org/10.1161/01.STR.0000240329.48263.0d
Kuroda R, Nakada T, Ojima T, Serizawa M, Imai N, Yagi N, Tasaki A, Aoki M, Oiwa T, Ogane T, Mochizuki K, Kobari M, Miyajima H (2017) The TriAGe+ score for vertigo or dizziness: a diagnostic model for stroke in the emergency department. J Stroke Cerebrovasc Dis 26(5):1144–1153. https://doi.org/10.1016/j.jstrokecerebrovasdis.2017.01.009
Choi SY, Kee HJ, Park JH, Kim HJ, Kim JS (2014) Combined peripheral and central vestibulopathy. J Vestib Res 24(5–6):443–451. https://doi.org/10.3233/VES-140524
Brandt T, Strupp M, Dieterich M (2016) Vestibular paroxysmia: a treatable neurovascular cross-compression syndrome. J Neurol 263(Suppl 1):S90–96. https://doi.org/10.1007/s00415-015-7973-3
Jannetta PJ, Moller MB, Moller AR (1984) Disabling positional vertigo. N Engl J Med 310(26):1700–1705. https://doi.org/10.1056/NEJM198406283102604
Wuehr M, Brandt T, Schniepp R (2017) Distracting attention in phobic postural vertigo normalizes leg muscle activity and balance. Neurology 88(3):284–288. https://doi.org/10.1212/WNL.0000000000003516
Acknowledgements
This study was supported by a grant of Seoul National University Bundang Hospital (06-2019-272). The authors thank the Medical Research Collaborating Center at Seoul National University Bundang Hospital for statistical analyses.
Author information
Authors and Affiliations
Contributions
Dr. H-J Kim acquired and analyzed the data, and drafted the manuscript. Ms. J-O Lee and Dr. J-Y Choi interpreted the data. Dr. J-S. Kim conducted the design and conceptualization of the study, interpretation of the data, and revising the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
Dr. H-J Kim, Ms. J-O Lee, and Dr. J-Y Choi report no disclosures. Dr. J-S Kim serves as an Associate Editor of Frontiers in Neuro-otology and on the editorial boards of the Journal of Clinical Neurology, Frontiers in Neuro-ophthalmology, Journal of Neuro-ophthalmology, and Journal of Vestibular Research. The other authors have nothing to disclose.
Ethical standards
This study followed the tenets of the Declaration of Helsinki and was performed according to the guidelines of Institutional Review Board of Seoul National University Bundang Hospital (IRB no. B-1907-553-001).
Electronic supplementary material
Below is the link to the electronic supplementary material.

415_2020_9831_MOESM1_ESM.png
Supplementary file1 The female predominance was maintained across all age groups, and peaked in the sixth decade (PNG 131 kb)
Rights and permissions
About this article
Cite this article
Kim, HJ., Lee, JO., Choi, JY. et al. Etiologic distribution of dizziness and vertigo in a referral-based dizziness clinic in South Korea. J Neurol 267, 2252–2259 (2020). https://doi.org/10.1007/s00415-020-09831-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-020-09831-2